Abstract
To assess whether transanal drainage tubes (TDT) protect against anastomotic leakage (AL) in patients without diverting stomas (DS) after laparoscopic anterior rectal resection (LAR). In the TDT group, after anastomosis of the sigmoid colon to the rectum, a 32F silicone tube was inserted through the anus with the tip of the tube exceeding the anastomosis by more than 5 cm. The tube was secured around the anus with a skin suture and a drainage bag was attached. It was left in place for 3–5 days postoperatively in the TDT group. In the No-TDT group, no transanal silicone tube drainage was used after the anastomosis. A total of 927 patients (620 in the no-TDT group and 307 in the TDT group) were included in the analysis, and a total of 50 (5.4%) patients were observed to develop AL. After using propensity score matching (PSM) to reduce baseline feature imbalances between the two groups, there were 287 patients in both groups, and the mean retention time of TDT was (4.7 ± 1.2) d. The incidence of AL in the TDT group was significantly lower than that in the no-TDT group (3.8% vs. 8.0%, with a the incidence of AL in the TDT group was significantly lower than that in the non-TDT group (3.8% vs. 8.0%, P = 0.034), but the incidence of AL classification was similar (P = 0.709). There were no significant differences between the two groups in terms of postoperative complications and postoperative recovery. Multivariate logistic regression analysis revealed that TDT was found to be an independent protective factor for postoperative AL (OR 0.437, 95% CI 0.207–0.923, P = 0.030). The elective use of TDT is a simple and effective protective measure for the prevention of AL in patients without stoma after LAR surgery, helping to reduce the probability of AL. This may be a potential alternative DS method for the appropriate population.
Similar content being viewed by others
Introduction
Laparoscopy-assisted rectal cancer is increasingly used as an alternative to open surgery for rectal cancer1,2. Meanwhile, the double-stapling technique (DST) continues to improve, and an increasing number of patients with rectal cancer have the opportunity to preserve their sphincter3. However, the thorny problem of anastomotic leakage (AL) still needs to be addressed. Although many high-quality studies have been devoted to reducing the incidence of AL after laparoscopic-assisted anterior rectal resection (LAR), the incidence remains as high as 6.1–12.3%3,4,5.
Since the first report of the preventive effect of a transanal drainage tube (TDT) on AL in 19976, several trials and meta-analyses have been dedicated to exploring the role of TDT in LAR4,6,7,8,9,10,11,12,13,14,15,16. It has been shown that the use of TDT can provide drainage, promote gastrointestinal motility, and reduce postoperative rectal resting pressure in patients compared with those who did not use TDT17. In many cases, TDT may be a safe and effective alternative to diverting stomas (DS)18. Nevertheless, the conclusions reached in later randomised controlled trials were the opposite7,8, and some studies were forced to terminate the study early for ethical reasons19. The most recent meta-analyses have reached different conclusions20,21. Therefore, the efficacy of TDT for preventing AL after rectal surgery remains unclear.
It is well known that DS repeatedly reduces the probability of AL and the reoperation rate and may even protect patients’ lives22. Therefore, even in randomised controlled trials, we cannot randomly choose whether to use DS or not, which causes a certain bias in the studies, and some of them were forced to be terminated early under the pressure of ethics and safety19. Meanwhile, clinicians have some subjectivity in the choice of using DS or TDT and may choose DS for a lower anastomotic position and tend to use TDT for a higher position23, as well as the small size of the populations included in the studies, which may have led to the inconsistent results of the studies above. Therefore, this study reports a large retrospective study conducted at the Chinese Center for the Diagnosis and Treatment of Colorectal Diseases that excluded patients with DS and used propensity-score matching (PSM) analysis to reduce bias in the selection of patients between the two groups. We aimed to assess whether TDT has a protective effect on AL in postoperative LAR patients without DS, and its impact on postoperative recovery and complications.
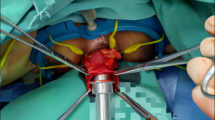
Illustration: A 32F silicone tube with more than three lateral holes in the tip was inserted through the anus under laparoscopic guidance, with the tip of the tube extending more than 5 cm beyond the anastomosis. The tube was secured around the anus using skin sutures and a drainage bag was attached. (Drawing by Wang).
Methods
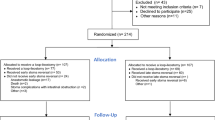
Patients and study design
Clinical data of patients with rectal cancer treated at the Zhangzhou Affiliated Hospital of Fujian Medical University between January 2018 and December 2023 were retrospectively collected.
Inclusion and exclusion criteria
The inclusion criteria: (1) the tumor was ≤ 15 cm from the anus and pathologically diagnosed as primary rectal cancer; (2) the anus was successfully saved, LAR surgery was performed, and end-to-end DST anastomosis was completed, the anastomosis is located 1–10 cm from the rectal dentate line; (3) DS was not performed in the first stage of surgery; (4) complete clinical information.
Exclusion criteria: (1) open surgery; (2) palliative surgery with preoperative combined distant metastases; (3) emergency surgery with preoperative combined acute bowel obstruction or bowel perforation, including failure to pass preoperative colonoscopy; (4) combined with organ resection from other sites; (5) other types of anastomosis-free surgery including abdominal perineal resection, Hartmann’s surgery, and transanal partial resection.
Treatment
All surgeries are performed by 2 lead surgeons in the same department, both of whom have extensive experience in colorectal surgery and are skilled in this procedure. Standard bowel preparations and oral antibiotics were administered preoperatively to prevent infection24. The surgical procedure was performed according to the principles of total mesorectal excision (TME), and all were laparoscopic-assisted25. The circular anastomosis was inserted transrectally, and end-to-end DST anastomosis was accomplished endoluminally. Airtightness was routinely assessed using transanal air insufflation26.
In the TDT group, after anastomosis of the sigmoid colon to the rectum, a 32F silicone tube was inserted through the anus under laparoscopic-assisted guidance, with its tip exceeding the anastomosis by more than 5 cm above the anastomosis. The tube was secured around the anus using skin sutures and a drainage bag was attached. The TDT group was left in place for 3–5 days postoperatively, unless accidental displacement or intolerance of early extraction occurred, and if AL occurred during this period, the TDT acted as a drain and prolonged the extraction time. If the TDT was removed ≤ 2 days postoperatively was considered to have been removed early or accidentally extubated, and the expected retention goal was not achieved. In the No-TDT group, transanal silicone tube drainage was not used after anastomosis. (Fig. 1).
Outcomes
The primary endpoint of this study was the occurrence of AL within 30 days after surgery in both groups. The secondary endpoints were anastomotic bleeding, bowel obstruction, bowel recovery, and length of hospital stay.The definition of AL was based on the guidelines issued by the International Rectal Cancer Study Group27, and was diagnosed when any of the following conditions were met: (1) abdominal pain, fever, or peritonitis manifested postoperatively, along with a bowel wall defect at the site of the anastomosis, and signs of spillage of the contrast agent on imaging; (2) fecal outflow from pelvic drainage tubes, vagina, or urethra drainage from pelvic drainage tube, vagina, urethra, and palpable anastomotic defect on rectal palpation; (3) intraoperative diagnosis of AL (interruption of bowel wall continuity and defect at the anastomotic site). Grade B is clinically significant and requires active therapeutic intervention but can be improved with conservative treatment.Grade C requires a second open abdominal surgery.
Statistical analysis
In retrospective observational research, it is an effective and commonly used method to balance the bias of the two groups to achieve an environment similar to that of a randomized controlled study using PSM analysis28. This method is well-suited for cohort studies, such as this study, where ethical and risk pressures exist19. In this study, matching was performed by 1:1 matching (caliper = 0.2) of the following variables: age, sex, body mass index (BMI), anemia, hypoproteinemia, diabetes, CEA, CA19-9, operation time, intraoperative bleeding, distance to anal verge (DTAV), neoadjuvant chemotherapy, and pT/N/TNM stage.
The characteristics of the two groups were compared before and after PSM. Categorical variables were analyzed using the chi-square test or Fisher’s test, and the rank-sum test was used for grade data. Continuous variables were compared using Student’s t-test (data are expressed as mean ± standard deviation). Logistic regression analysis was used to identify independent predictors of AL. Statistical significance was defined as P < 0.05. The above statistical analyses were performed using the SPSS version 26.0 (IBM) software.
Results
Finally, 927 consecutive patients who met the criteria for consecutive visits were included in the analysis, including 620 in the non-TDT group and 307 in the TDT group. Before PSM, eight patients in the TDT group were dislodged before planned extraction and were still included in the TDT group.
Patient characteristics
Before PSM, patients in the TDT group had a longer operative time compared to patients in the Non-TDT group (127.3 ± 39.5 vs. 116.8 ± 35.1, P < 0.001), and a significantly higher proportion of patients with DTAV 5–10 cm (63.2% vs. 35.0%, P < 0.001), which are significantly higher, apparently suggesting a possible relationship between these indicators and postoperative recovery and AL. (Table 1 before PSM).
After PSM, a new cohort was obtained, both groups contained 287 patients, including operative time. DTAV indicators were well-matched, and the basic patient-specific differences were not statistically significant (all P > 0.05), specifically higher comparability. 8 patients (2.8%) in the TDT group did not complete the TDT because they could not tolerate the early removal of the TDT. (Table 1, after PSM).
Primary endpoint
Before PSM, 50 cases of postoperative AL were observed in this cohort, with an overall incidence of 5.4%, including 26 grade C AL leading to reoperation and 24 grade A + B AL. The differences in postoperative AL and AL grades were not statistically significant.
After PSM, the average preservation time of TDT was 4.7 ± 1.2 days. In terms of the probability of AL, the TDT group had a significantly lower incidence than the non-TDT group (3.8% vs. 8.0%), and the difference was statistically significant (P = 0.034). However, the incidence of grade C AL was similar in terms of the AL grade (54.5% vs. 65.2%, P = 0.709) (Table 2).
Secondary endpoints
We further explored whether TDT had any effect on other postoperative complications or on postoperative recovery. There were no statistically significant differences in the probability of anastomotic bleeding, intestinal obstruction, time to anal evacuation/resumption of a normal diet, and postoperative hospital stay, either before or after PSM (P > 0.05) (Table 2).
Independent impact factors of AL
We further explored the independent impact factors of AL using logistic regression modeling. Before PSM, multivariate regression analysis showed that, carcinoembryonic antigen (CEA) level and operative time had an independent effect on postoperative AL. However, TDT did not have a protective effect on postoperative AL (odds ratio [OR] 0.519, 95% CI 0.259–1.037, P = 0.063) (Table 3).
As described previously, to reduce retrospective study selection bias, we balanced the unbalanced factors between the 2 groups of patients using the PSM method to improve comparability. After PSM, we explored the independent influence of AL. The results showed that CEA level (OR 2.327, 95% CI 1.139–4.754, P = 0.020) and operation time (OR 1.010, 95% CI 1.003–1.017, P = 0.007) still had independent influences on postoperative AL. TDT was found to be an independent protective factor for postoperative AL (OR 0.437, 95% CI 0.207–0.923, P = 0.030) (Table 4).
Discussion
This study included 927 patients with rectal cancer without DS to evaluate the effect of TDT on AL after LAR. After PSM 1:1 matching, the results showed that the proportion of AL in the TDT group was significantly lower than that of patients in the Non-TDT group, and the difference was statistically significant (3.8% vs. 8.0%, P = 0.034). Meanwhile, TDT was confirmed to be an independent protective factor for AL by multifactorial regression (OR 0.437, 95% CI 0.207–0.923, P = 0.030), but failed to reduce the rate of postoperative grade C AL.
AL is a frequent and serious complication of rectal sphincter preservation surgery, resulting in a huge economic burden and severely threatening the life of the patient3,29. Since TDT can elicit the rectal contents in a timely manner, thereby reducing the resting pressure in the intestinal lumen, theoretically, it has a protective effect on postoperative anastomosis, but it still cannot completely avoid postoperative AL as well as the serious complications that it may cause6,17. Several previous RCTs have aimed to confirm the efficacy of TDT, but the conclusions drawn remain inconsistent. Xiao et al. prospectively included 439 patients with a DTAV ≤ 15 cm, excluding neoadjuvant chemotherapy and DS patients. Patients were likely to use handsewn or double-staple techniques for anastomosis, but did not disclose that the TDT group used the caliber of silicone tubing; ultimately, AL was considered significantly lower in TDT patients (4.0% vs. 9.6%, P = 0.026)17. Tamura et al. in their prospective study included a relatively small sample size; only 161 patients with DTAV ≤ 15 cm were enrolled, and the TDT group used 20-24F silicone tubing with a smaller caliber and poorer drainage, with no difference in the AL rate between the two groups (10.1% vs. 14.1%, P = 0.445)8. Unlike the previous two RCT studies, Zhao et al. included 560 patients with DTAV ≤ 10 cm and also excluded preoperative neoadjuvant chemotherapy, the decision of whether to do DS in the study was made by the surgeon after the anastomosis, and 28F silicone tubing was used in the TDT group. Further subgroup analyses were done according to the presence or absence of DS, taking into account the possible effects of DS, but ultimately, it was concluded that TDT had no protective effect (OR 0.95, 95% CI 0.51–1.77, P = 0.87)7. In addition to the aforementioned reasons, such as inconsistent TDT retention times and different surgical approaches, including laparoscopic or open surgery, a combination of reasons may lead to inconsistent conclusions from different RCT studies.
Several newly published high-quality meta-analyses have shown a protective effect of TDT, especially among patients without DS, similar to the findings of the present study13,14. In a meta-analysis, Shiki et al. concluded that TDT reduced the incidence of AL in a subgroup of 955 patients without DS (OR 0.50, 95% CI 0.29–0.86, P = 0.012), but concluded that it was not protective if DS patients were included in the whole population14. This is also supported by another larger meta-analysis, which suggests that patients without DS may be the population with the greatest benefit from TDT13. Furthermore, a meta-analysis concluded that TDT has a greater role in reducing the chance of reoperation after the occurrence of AL, that is, preventing grade C AL, which brings certain clinical benefits15,16.
Unfortunately, no study has clearly shown the indications for its use in LAR. However, the use of TDT may influence the surgeon’s decision on the application of DS, which has been suggested to be applied in patients with high expected reoperation rates or mortality, and TDT has been considered a potential alternative to DS30. Although PSM was performed in this study to reduce confounders between the 2 groups, we have to recognise that there is still some selection bias when surgeons are choosing whether or not to use TDT. For example, in the non-DS population, patients with a DTAV of 5–10 cm were more likely to be selected for TDT (63.2% vs. 36.8%, P < 0.001) as patients with a DTAV of ≤ 5 cm required DS or even APR, whereas patients with a DTAV of ≥ 10 cm had a relatively low incidence of AL for which TDT was less commonly used. Alternatively, patients with longer operative times are more likely to be treated with TDT.In short, intraoperative use of TDT requires a simple and feasible method of anastomotic protection chosen by the surgeon on the basis of comprehensive post-anastomotic judgement when the anastomosis is deemed to be less than optimal and at the expense of not wanting to perform a DS. Finally, we advocate that silicone tubing used for TDT should be recommended to choose larger calibre silicone tubing, such as 32F, with multiple side holes at the tip to ensure drainage31.
This study had several limitations. First, as a retrospective study, although the sample size was sufficiently large, issues such as confounders and selection bias unavoidably existed; therefore, we utilized the PSM method to minimize between-group bias. Second, we excluded patients with incomplete information where the incidence of AL might have been overestimated or underestimated. Third, this study only included patients who underwent laparoscopic-assisted surgery, and further exploration is needed in patients who undergo open surgery. Finally, the depth of TDT placement may not be exactly the same in different patients, but it can be ensured to be > 5 cm above the anastomosis, and factors such as optimal TDT placement depth and placement time need to be further explored. However, to the best of our knowledge, in terms of sample size and exclusion of DS bias, our study, either before or after PSM, is the largest retrospective controlled study to explore the efficacy of TDT for the prevention of postoperative AL after LAR to date.
Conclusion
The elective use of TDT is a simple and effective protective measure for the prevention of AL in patients without a stoma after laparoscopic AR surgery, helping to reduce the probability of AL. It may be a potential alternative DS method among the appropriate population, but more studies are needed to clarify the indications for its clinical use.
Data availability
All data obtained or analyzed during this study are included in the article. Data analyzed during the study can be obtained from the corresponding author if necessary.
References
Fleshman, J. et al. Effect of laparoscopic-assisted resection vs open resection of stage ii or iii rectal cancer on pathologic outcomes: The ACOSOG Z6051 randomized clinical trial. JAMA 314(13), 1346–1355. https://doi.org/10.1001/jama.2015.10529 (2015).
van der Pas, M. H. G. M. et al. Laparoscopic versus open surgery for rectal cancer (COLOR II): short-term outcomes of a randomised, phase 3 trial. COLOR II. Lancet Oncol. 14(3), 210–218. https://doi.org/10.1016/s1470-2045(13)70016-0 (2013).
Kuroyanagi, H. et al. Laparoscopic-assisted anterior resection with double-stapling technique anastomosis: safe and feasible for lower rectal cancer?. Surg. Endosc. 23(10), 2197–2202. https://doi.org/10.1007/s00464-008-0260-y (2009).
Choy, K. T., Yang, T. W. W., Heriot, A., Warrier, S. K. & Kong, J. C. Does rectal tube/transanal stent placement after an anterior resection for rectal cancer reduce anastomotic leak? A systematic review and meta-analysis. Int. J. Colorectal Dis. 36(6), 1123–1132. https://doi.org/10.1007/s00384-021-03851-8 (2021).
Watanabe, T. et al. Prediction model for complications after low anterior resection based on data from 33,411 Japanese patients included in the National Clinical Database. Surgery 161(6), 1597–1608. https://doi.org/10.1016/j.surg.2016.12.011 (2017).
Klein, P., Immler, F., Sterk, P. & Schubert, F. Secure anastomoses of the large intestine (especially with transanal drainage. Zentralbl. Chir. 122(7), 528–532 (1997).
Zhao, S. et al. Transanal drainage tube use for preventing anastomotic leakage after laparoscopic low anterior resection in patients with rectal cancer: A randomized clinical trial. JAMA Surg. 156(12), 1151–1158. https://doi.org/10.1001/jamasurg.2021.4568 (2021).
Tamura, K. et al. Laparoscopic anterior resection with or without transanal tube for rectal cancer patients—A multicenter randomized controlled trial. Am. J. Surg. 222(3), 606–612. https://doi.org/10.1016/j.amjsurg.2020.12.054 (2021).
Shigeta, K. et al. A meta-analysis of the use of a transanal drainage tube to prevent anastomotic leakage after anterior resection by double-stapling technique for rectal cancer. Surg. Endosc. 30(2), 543–550. https://doi.org/10.1007/s00464-015-4237-3 (2016).
Chen, H., Cai, H. K. & Tang, Y. H. An updated meta-analysis of transanal drainage tube for prevention of anastomotic leak in anterior resection for rectal cancer. Surg. Oncol. 27(3), 333–340. https://doi.org/10.1016/j.suronc.2018.05.018 (2018).
Ha, G. W., Kim, H. J. & Lee, M. R. Transanal tube placement for prevention of anastomotic leakage following low anterior resection for rectal cancer: A systematic review and meta-analysis. Ann. Surg. Treat Res. 89(6), 313–318. https://doi.org/10.4174/astr.2015.89.6.313 (2015).
Yang, Y. et al. Prophylactic transanal decompression tube versus non-prophylactic transanal decompression tube for anastomotic leakage prevention in low anterior resection for rectal cancer: A meta-analysis. Surg. Endosc. 31(4), 1513–1523. https://doi.org/10.1007/s00464-016-5193-2 (2017).
Fujino, S., Yasui, M., Ohue, M. & Miyoshi, N. Efficacy of transanal drainage tube in preventing anastomotic leakage after surgery for rectal cancer: A meta-analysis. World J. Gastrointest. Surg. 15(6), 1202–1210. https://doi.org/10.4240/wjgs.v15.i6.1202 (2023).
Zhang, Y. X., Jin, T. & Yang, K. The role of transanal drainage tube in preventing the anastomotic leakage in rectal cancer surgery without a defunctioning stoma: A meta-analysis. Surgeon 21(4), e164–e172. https://doi.org/10.1016/j.surge.2022.11.002 (2023).
Xia, S. et al. Transanal drainage tube for the prevention of anastomotic leakage after rectal cancer surgery: A meta-analysis of randomized controlled trials. Meta Front. Oncol. 13, 1198549. https://doi.org/10.3389/fonc.2023.1198549 (2023).
Wang, W., Zhang, J., Cai, J., Zhao, X. & Wang, F. Transanal drainage tube for the prevention of anastomotic leakage in anterior resection for rectal cancer: A systematic review and meta-analysis. Expert Rev. Anticancer Ther. 23(4), 431–442. https://doi.org/10.1080/14737140.2023.2179991 (2023).
Xiao, L. et al. Can transanal tube placement after anterior resection for rectal carcinoma reduce anastomotic leakage rate? A single-institution prospective randomized study. World J. Surg. 35(6), 1367–1377. https://doi.org/10.1007/s00268-011-1053-3 (2011).
Carboni, F. et al. Transanal drainage tube: Alternative option to defunctioning stoma in rectal cancer surgery?. Transl. Gastroenterol. Hepatol. 5, 6. https://doi.org/10.21037/tgh.2019.10.16 (2020).
Bulow, S., Bulut, O., Christensen, I. J., Harling, H., Rectal Stent Study G. Transanal stent in anterior resection does not prevent anastomotic leakage. Colorectal Dis. 8(6), 494–496. https://doi.org/10.1111/j.1463-1318.2006.00994.x (2006).
Liu, Y. et al. Does transanal drainage tubes placement have an impact on the incidence of anastomotic leakage after rectal cancer surgery? A systematic review and meta-analysis. BMC Cancer 24(1), 263. https://doi.org/10.1186/s12885-024-11990-8 (2024).
Guo, C., Fu, Z., Qing, X. & Deng, M. Prophylactic transanal drainage tube placement for preventing anastomotic leakage after anterior resection for rectal cancer: A meta-analysis. Colorectal. Dis. 24(11), 1273–1284. https://doi.org/10.1111/codi.16231 (2022).
Garg, P. K., Goel, A., Sharma, S., Chishi, N. & Gaur, M. K. Protective diversion stoma in low anterior resection for rectal cancer: A meta-analysis of randomized controlled trials. Visc. Med. 35(3), 156–160. https://doi.org/10.1159/000497168 (2019).
Herrinton, L. J. et al. Conversations for providers caring for patients with rectal cancer: Comparison of long-term patient-centered outcomes for patients with low rectal cancer facing ostomy or sphincter-sparing surgery. CA Cancer J. Clin. 66(5), 387–397. https://doi.org/10.3322/caac.21345 (2016).
Lee, J. H., Ahn, B. K., Ryu, J. & Lee, K. H. Mechanical bowel preparation combined with oral antibiotics in colorectal cancer surgery: A nationwide population-based study. Int. J. Colorectal. Dis. 36(9), 1929–1935. https://doi.org/10.1007/s00384-021-03967-x (2021).
Heald, R. J., Husband, E. M. & Ryall, R. D. The mesorectum in rectal cancer surgery–the clue to pelvic recurrence?. Br. J. Surg. 69(10), 613–616. https://doi.org/10.1002/bjs.1800691019 (1982).
Kawada, K. et al. Risk factors for anastomotic leakage after laparoscopic low anterior resection with DST anastomosis. Surg. Endosc. 28(10), 2988–2995. https://doi.org/10.1007/s00464-014-3564-0 (2014).
Rahbari, N. N. et al. Definition and grading of anastomotic leakage following anterior resection of the rectum: A proposal by the International Study Group of Rectal Cancer. 38Surgery 147(3), 339–351. https://doi.org/10.1016/j.surg.2009.10.012 (2010).
D’Agostino, R. B. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat. med. 17(19), 2265–2281. https://doi.org/10.1002/(sici)1097-0258(19981015)17:19%3c2265::aid-sim918%3e3.0.co;2-b (1998).
Mukai, T., Maki, A., Shimizu, H. & Kim, H. The economic burdens of anastomotic leakage for patients undergoing colorectal surgery in Japan. Asian J. Surg. 46(10), 4323–4329. https://doi.org/10.1016/j.asjsur.2023.06.123 (2023).
Cho, S. H. et al. The usefulness of transanal tube for reducing anastomotic leak in mid rectal cancer: Compared to diverting stoma. Ann. Surg. Treat Res. 100(2), 100–108. https://doi.org/10.4174/astr.2021.100.2.100 (2021).
Luo, Y., Zhu, C. K., Wu, D. Q., Zhou, L. B. & Wang, C. S. Effect comparison of three different types of transanal drainage tubes after anterior resection for rectal cancer. BMC Surg. 20(1), 166. https://doi.org/10.1186/s12893-020-00811-x (2020).
Acknowledgements
The authors thank the foundation for their support.
Funding
This study was supported by the Natural Science Foundation of Fujian Province (Grant Number 2023J011819).
Author information
Authors and Affiliations
Contributions
Project development: GW, HT, YG, YH; Data collection or management: GW; Data analysis: GW; Manuscript writing: GW. All the authors have reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was reviewed and approved by the Medical Ethics Committee of Zhangzhou Affiliated Hospital of Fujian Medical University (Grant No. 2024LWB363). All methods were performed in accordance with relevant guidelines and regulations (Declaration of Helsinki). Informed consent was obtained from all subjects and/or their legal guardians (s) for this study.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, G., Tang, H., Huang, Y. et al. Efficacy of transanal drainage tubes in postoperative anastomotic leakage in patients with laparoscopic anterior rectal resection without diverting stoma. Sci Rep 15, 18834 (2025). https://doi.org/10.1038/s41598-025-03440-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03440-7