Abstract
This ex-vivo study compares the adaptation, porosity, and sealing performance of ProRoot MTA, NeoPutty, and Biodentine in standardized, simulated furcation perforations created in extracted mandibular molars using clinical evaluation and high-resolution micro-computed tomography (micro-CT). Thirty-six mandibular molars with furcation perforations were randomly assigned to three groups (n = 12). Clinical evaluation assessed adaptation, porosity, and overfilling, while micro-computed tomography (micro-CT) provided quantitative data on voids and gaps. Statistical analysis used chi-square, Kruskal–Wallis, and Mann–Whitney U tests. NeoPutty and ProRoot MTA showed superior adaptation compared to Biodentine (p < 0.05). Biodentine showed higher porosity (28.44%) than ProRoot MTA (0%) and NeoPutty (8.3%) (p < 0.001). Biodentine also had the highest void volume (1.05 mm3) and gap volume (1.37 mm3), while ProRoot MTA recorded the lowest void volume (0.59 mm3), and NeoPutty had the smallest gap volume (0.85 mm3). No significant differences were observed in overfilling rates. Overall, ProRoot MTA exhibited the most consistent sealing ability, whereas NeoPutty emerged as a viable alternative due to its favorable handling and reliable adaptation. Biodentine, by contrast, showed the poorest performance in terms of structural integrity and sealing capacity. Within the limitations of this study, these findings support the use of ProRoot MTA or NeoPutty for furcation perforation repair, while suggesting more cautious use of Biodentine in such applications.
Similar content being viewed by others
Introduction
Furcation perforations are pathological connections between the root canal system and the surrounding periodontium. They can be caused by extensive caries, resorption processes, or iatrogenic factors during endodontic treatment1. These perforations compromise the tooth’s integrity and often lead to periodontal inflammation due to bacterial colonization of the perforation site. If left untreated, furcation perforations worsen over time2. Due to their proximity to critical periodontal structures and the increased risk of contamination from the oral environment, they pose a significant challenge to successful endodontic treatment1,2.
The prognosis of teeth with furcation perforations is strongly influenced by several factors, including the size and location of the perforation, the time elapsed until repair, and the type of material used for sealing3. Larger perforations and those located close to the bone crest pose a greater risk of bacterial infiltration and contamination with fluid from the gingival sulcus, leading to compromised healing outcomes4. In addition, untreated perforations can lead to a series of complications, which increase the likelihood of tooth extraction, such as persistent inflammation, damage to the periodontal attachment, epithelial tissue overgrowth, ongoing bone deterioration, and extensive bone resorption2. It has been reported as the second leading cause of endodontic failures following obturation, accounting for 9.6% of cases5.
An effective repair material should provide an adequate seal with minimal setting time, be biocompatible, non-toxic, non-carcinogenic, affordable, bacteriostatic, readily available, easy to handle, and capable of promoting osteogenesis and cementogenesis6. Additionally, it should function effectively as a barrier or matrix between the root canal filling and surrounding tissues, guaranteeing a hermetic seal5,7,8. This can be accomplished by reducing the formation of gaps between the dentin walls and the material and minimizing voids within the material itself to decrease bacterial microleakage8,9.
Recent advances in calcium silicate-based cements such as mineral trioxide aggregate (MTA) and Biodentine (Septodont, Saint Maur des Fosse’s, France)10 have revolutionized the treatment of furcation perforations. These highly biocompatible materials promote complex tissue regeneration and provide a hermetic seal that prevents bacterial recontamination11. MTA, introduced in the 1990s, became the gold standard due to its ability to induce cementogenesis and its excellent sealing properties6. However, its disadvantages include long setting times6, complex handling, and possible discoloration due to the inclusion of bismuth oxide12,13.
In response to these limitations, second-generation calcium silicate-based cements such as Biodentine have been developed, offering shorter setting times and improved handling properties14. Biodentine, which incorporates zirconium oxide as a radiopacifier instead of bismuth oxide, has been shown to avoid staining while maintaining similar mechanical properties to dentin15. More recently, pre-mixed putty-like repaired materials such as NeoPutty (Avalon Biomed, Houston, Texas, USA) have come onto the market, eliminating mixing variability and facilitating application. These materials have demonstrated satisfying outcomes in several clinical situations besides furcation perforations such as root resorptions, vital pulp therapies, and microsurgeries8,16,17.
The evaluation of calcium silicate-based materials for furcal perforation repair remains limited, as many of the currently available data are based on isolated case reports with variable clinical outcomes. These reports often lack standardized protocols and include uncontrolled variables that may influence the success of the repair beyond the properties of the materials themselves8.
Although furcation perforation repair has been previously explored through microleakage testing, such investigations have not addressed critical structural parameters such as internal adaptation, gap formation, and porosity18. Prior assessments have relied on two-dimensional techniques, such as fluid filtration or dye penetration, which provide indirect and limited information about the internal sealing quality of the materials. These methods do not allow for a spatial evaluation of voids or the interface between the material and dentinal walls18.
Advanced imaging techniques such as micro-computed tomography (micro-CT) are frequently used to investigate the efficacy of these materials in sealing furcation perforations19. This technique enables a thorough examination of marginal adaptation, porosity, and the integration of the material into the surrounding dentin.
In a recent study8, micro-CT imaging was used to evaluate the adaptation of three calcium silicate-based cements in simulated furcation perforations of mandibular molars. However, the study’s methodology involved assessments conducted by the same operator, which limited the potential for blinded results. The absence of a blinded assessment introduces potential bias, as the operator may unconsciously favor one material over the others during testing.
In addition to the previously mentioned study, there is a noticeable lack of research focused on assessing gaps and voids in cases of furcal perforation using micro-CT analysis. Given this gap in the literature, the current study aims to evaluate and compare the marginal adaptation, porosity, and sealing performance of three calcium silicate-based cements in repairing simulated furcation perforations in mandibular molars using clinical assessment and micro-CT imaging.
Materials and methods
Sample size calculation
The present study is reported according to the Preferred Reporting Items for Laboratory studies in Endodontology (PRILE) 2021 guidelines20. The research protocol was approved by the Rey Juan Carlos institutional ethics committee (Madrid, Spain) under registration no. 1,301,202,302,823. The study was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all subjects and/or their legal guardians.
The sample size calculation was based on the percentage values of gaps and voids reported in a previous study8. The results indicated that a minimum of eight samples would be required in each group to achieve a power of 95%, given an alpha error of 0.05. Twelve samples per group were included to enhance the robustness and reliability of the study findings.
Sample selection and grouping
An initial sample of 125 extracted inferior mandibular molars were collected for this ex-vivo study.
After assessing eligibility based on inclusion and exclusion criteria, only 36 extracted mandibular molars were selected. All included teeth had intact furcation areas and were free of root caries, previous endodontic treatment, or visible cracks. Exclusion criteria included teeth with root fractures, carious lesions involving the furcation area, previous endodontic treatment, or any structural damage that could compromise standardization of the perforation site.
The teeth were randomly assigned to three experimental groups (n = 12 per group), each assigned to one of three commercially available calcium silicate-based cements: ProRoot MTA (Dentsply Maillefer, Ballaigues, Switzerland), NeoPutty (Avalon Biomed, Houston, TX, USA), and Biodentine (Septodont, Saint-Maur-des-Fossés, France).
Before the experimental procedures, the samples were standardized using Cone Beam Computed Tomography (CBCT) to measure the distance from the chamber floor to the furcation, ensuring consistent anatomical conditions across the samples. This step aimed to create a more homogeneous sample set and decrease the chances of furcation perforations having greater depth and a higher presence of material. The samples were grouped in sets of three based on similar volume, and then the three matched samples were randomly assigned to one of the three calcium silicate-based materials.
Furcation perforation standardization and placement of sealing material
The molars were first immersed in a 4.25% sodium hypochlorite solution for 15 min to eliminate organic matter from the root surfaces. They were then thoroughly rinsed with a saline solution to remove residual sodium hypochlorite. A coronal access cavity was prepared using a round bur (801LG.FG.016, Meisinger, Neuss, Germany), ensuring the bottom of the pulp chamber remained untouched. Subsequently, standardized furcal perforations were created in the center of the pulp chamber floor using the same round bur (with a diameter of 1.6 mm and an active part length of 1.6 mm) under constant irrigation to prevent overheating. All furcation perforations were created by a single experienced operator using a standardized technique to ensure uniformity across all specimens.
The crown was sectioned 4 mm above the cementoenamel junction, and the roots were sectioned 4 mm below the furcation area using a lance bur (859 LF.FG.014, Komet, Lemgo, Germany). Each tooth was mounted in heavy-body silicone, leaving a gap between the specimen and the mold. A sterile cotton pellet moistened with saline solution was placed under the furcation perforation to simulate the moisture present in the periodontal ligament under clinical conditions.
The furcation perforations were sealed using the calcium silicate-based materials: ProRoot MTA, NeoPutty, and Biodentine.
ProRoot MTA was mixed according to the manufacturer’s guidelines by combining the powder with sterile water at a 3:1 ratio. A spatula blended the mixture on a glass slab until it reached a putty-like consistency. Similarly, Biodentine was prepared by mixing the liquid with the powder in the capsule and blending them in a triturator for 30 s, following the manufacturer’s directions. NeoPutty, a premixed calcium silicate-based material, was used immediately without additional preparation.
Each material was loaded into an amalgam carrier, applied to the perforation site, and compacted with an inverted size 30 paper point (ProTaper Gold F3 paper point, Dentsply Sirona, York, PA, USA), which has a base diameter of 1.2 mm. This provided a broad and consistent surface to ensure proper fit against the cavity walls. After application, the samples were kept in a 100% humidity chamber at 37 °C for a week to mimic oral conditions during the setting process.
Qualitative and quantitative evaluation
After sealing, radiographs were taken to assess the adaptation of the repair materials. Each sample was examined under a dental microscope (OPMI PICO, Carl Zeiss, Göttingen, Germany) at 10x magnification, and images were captured. Each clinical photograph was paired with its corresponding radiograph and compiled into a PowerPoint presentation, and each specimen was assigned a random letter (uppercase/lowercase).
A table cross-referencing the letters with specific samples was created and made available only to one operator (M.R.C.) to ensure that the other three operators involved in the evaluation (J.M.C., N.N., and D.R.F.) remained blinded. These operators were calibrated and unaware of the material of the samples. A PDF file containing clinical and radiographic images of each specimen and the corresponding assigned letter was provided to the three operators, who were asked to complete a questionnaire evaluating four clinical parameters: adaptation of the material to the cavity, presence of porosity, overfilling, and overall adequacy of the sealing. Responses were assessed as either “yes” or “no.” This double-blind approach helped to reduce bias and enhance the quality of the assessment.
Micro-CT scans were performed using a Phoenix V|tome|x S240 system (General Electric, Boston, MA, USA) with an isotropic resolution of 20 μm. Scanning was conducted at 155 kV and 190 mA, utilizing a 0.2-mm-thick aluminum filter and completing a full 360° rotation around the vertical axis, resulting in approximately 1300 images per tooth after reconstruction with Phoenix Datos|x 3D software (General Electric, Boston, MA, USA), which included ring artifact correction of 5, beam hardening correction of 50%, and smoothing of 8. Each scan took about 60 min.
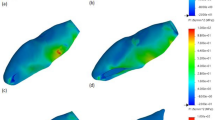
The volumetric data (mm3) were subsequently analyzed using a combination of ImageJ (National Institutes of Health, Bethesda, MD) for quantitative analysis, 3D Slicer (http://www.slicer.org) for image binarization, and Meshmixer (Autodesk Inc.) for generating three-dimensional models to visualize the perforations. For each sample, the data associated with the calcium-silicate-based materials within the cavities, as well as the voids and gaps between the dentin wall and the repair material, were calculated by creating binary images (by subtracting the filled perforation from the total volume) and assessing porosity through segmentation to identify regions of lower density (Fig. 1).
Gaps are dark voids between the dentin wall and the repair material, indicating inadequate adaptation or sealing. Conversely, voids refer to dark spaces within the repair material, suggesting internal porosity or incomplete filling. These factors were measured quantitatively to evaluate the integrity and sealing performance of the materials examined.
Although micro-CT was the primary tool for quantitative analysis, radiographs and photographs were included to simulate routine clinical evaluation. These methods allowed for blinded visual assessment of surface adaptation, overfilling, and porosity, enhancing the clinical relevance of the findings and enabling comparison with standard diagnostic practices.
Statistical analysis
The statistical analysis was conducted using SPSS (Statistical Package for the Social Sciences 21.0; IBM Corp, Armonk, NY). The qualitative data, including adaptation, overfilling, porosity, and overall quality of obturation, were analyzed using the chi-square test. In contrast, the quantitative data from the micro-CT scans, such as voids and porosity, were first assessed for normality using the Shapiro-Wilk test. Since the data did not follow a normal distribution, the Kruskal-Wallis test was employed to compare the three experimental groups, followed by the Mann-Whitney U test for pairwise comparisons, with an appropriate adjustment for multiple comparisons. The statistical significance level was set at p < 0.05.
Results
Qualitative analysis
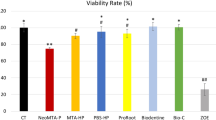
Results from the qualitative analysis are shown in Table 1. The qualitative analysis of furcal perforation repair using various calcium silicate-based cements focused on four key aspects: adaptation, overfilling, porosity, and overall obturation quality.
Before testing the materials’ sealing ability, the volumes of the initial perforation were compared between groups to verify homogeneity among the samples. The analysis confirmed that no statistically significant differences were observed in the initial perforation volumes across the groups, validating the comparability of the results obtained after treatment.
ProRoot MTA and NeoPutty demonstrated 100% adaptation to the cavity, while Biodentine achieved only 66.7%. This difference was statistically significant (p < 0.05) when comparing Biodentine with ProRoot MTA and NeoPutty. No significant differences were observed between ProRoot MTA and NeoPutty.
The proportion of cases showing porosity in the material was significantly higher with Biodentine (50%) compared to NeoPutty (8.3%) and ProRoot MTA (0%). The difference between Biodentine and the other two materials was statistically significant (p < 0.05), while no significant difference was found between NeoPutty and ProRoot MTA.
The best qualitative results regarding overfilling were obtained with ProRoot MTA (25%), followed by NeoPutty and Biodentine (33.3%). However, this difference was not statistically significant.
ProRoot MTA demonstrated the highest performance, with 100% of cases achieving proper obturation. NeoPutty followed with 91.7%, while Biodentine recorded the lowest success rate at 66.7%. Significant differences were noted when comparing NeoPutty to Biodentine® and ProRoot MTA to Biodentine (p < 0.05).
Quantitative evaluation
Table 2 presents the results of a quantitative evaluation conducted with micro-CT imaging. The evaluation focused on voids, gaps, and porosity within the material (Figs. 2 and 3).
Representative 3D sagittal images illustrating pre (A, C, E), and post perforation repair with (B) NeoPutty; (D) Biodentine; (F) ProRoot. All perforations were created using the same standardized protocol and bur size; apparent differences in perforation size are due to variations in image orientation, magnification, and rendering angle.
NeoPutty had the highest percentage of voids (4.20%), whereas ProRoot MTA had the lowest (1.28%). Biodentine exhibited an average void volume of 1.05 mm3 (2.38%), which was higher than NeoPutty (0.70 mm3, 1.65%) and ProRoot MTA (0.59 mm3, 1.29%). These differences highlight the superior material density of ProRoot MTA and NeoPutty compared to Biodentine.
Gaps, referring to the spaces between the dentinal wall and the sealing material, were largest in ProRoot MTA (6.48%), followed by Biodentine (2.40%), and smallest in NeoPutty (1.03%). In terms of gap volume, Biodentine had the highest value (1.37 mm3), followed by NeoPutty (0.85 mm3) and ProRoot MTA (0.29 mm3).
Biodentine exhibited the highest porosity at 28.44%, whereas NeoPutty demonstrated no measurable porosity at 0.0%. The differences between Biodentine and ProRoot MTA and between Biodentine and NeoPutty were statistically significant (p < 0.001); however, no significant differences were observed between ProRoot MTA and NeoPutty.
Discussion
The present study evaluated the sealing ability of three calcium silicate-based cements—ProRoot MTA, NeoPutty, and Biodentine—to repair furcal perforations in mandibular molars. Both qualitative (adaptation, overfilling, porosity, and obturation quality) and quantitative micro-CT assessments (voids, gaps, and porosity) were employed to compare these materials. The findings indicate significant differences in material performance, especially regarding adaptation, porosity, and obturation quality, which are critical factors for the success of furcation perforation repairs.
To the authors’ knowledge, this is the first study to perform a qualitative clinical assessment of calcium silicate-based cement adaptation in furcal perforations. Since micro-CT imaging cannot be performed in vivo, this study provides a controlled experimental setting that closely replicates real clinical situations. Indeed, micro-CT is a highly reliable technique commonly employed to evaluate 3D microstructures in ex vivo models21. Its precision in image analysis arises from its ability to distinguish the dentinal wall, furcal repair materials, and empty spaces using various grayscale thresholds.
These results are consistent with a recent study8 that used micro-CT imaging to evaluate the adaptation of three calcium silicate-based cements [i.e., Endosequence BC RRM-Fast Set Condensable Putty (Brasseler USA, Savannah, GA, USA), ProRoot MTA, and Biodentine] in simulated furcation perforations of mandibular molars, emphasizing the superior sealing ability and biocompatibility of calcium silicate-based cements, particularly MTA8. Among the materials tested, the Endosequence BC putty exhibited the lowest gap volume, suggesting superior adaptation to the dentinal walls. However, this previous study relied on assessments conducted by a single, non-blinded operator, which introduced a potential source of bias and limited the objectivity of the results. In contrast, the present study employed blinded clinical evaluations by multiple observers, combined with high-resolution micro-CT analysis, to provide a more rigorous and unbiased assessment of material performance.
Overall, the current findings indicate that both ProRoot MTA and NeoPutty achieved superior adaptation to the dentinal walls, significantly exceeding the performance of Biodentine. This variation in adaptation is linked to the materials’ handling characteristics. Specifically, NeoPutty, with its pre-mixed, putty-like texture, appears to offer enhanced ease of use and improved conformity to the irregularities of the perforation site. In contrast, Biodentine, while it sets relatively quickly22, demonstrated a statistically significant inability to adapt as well as the other two materials.
As shown in Table 1, one of the most critical findings of this study is the difference in porosity among the materials. Biodentine exhibited significantly higher porosity (28.44%) compared to both ProRoot MTA (0%) and NeoPutty (8.3%). This increased porosity in Biodentine could be attributed to its mixing process, which involves mechanical vibration and automatic agitation. These mixing methods may introduce air bubbles into the material, producing higher porosity. In contrast, NeoPutty comes in a pre-mixed formula that effectively minimizes the incorporation of air during handling, resulting in its lower porosity and improved overall performance.
Indeed, a key factor influencing the performance of calcium silicate-based cements is the mixing process23,24, which is eliminated in NeoPutty due to its pre-mixed formulation. This ensures consistent material properties and reduces operator-dependent variability. Previous studies highlighted this aspect, demonstrating that factors such as the powder-to-liquid ratio, temperature, and porosity can significantly affect the mechanical properties of cements23,24,25. As a result, any variables related to mixing (e.g., the powder-to-liquid ratio and the operator’s mixing technique) and material placement play a crucial role in the outcome23.
Furthermore, the porosity of endodontic sealers plays a crucial role in their effectiveness. Exposure to periradicular fluids can negatively impact the durability of the endodontic filling. Sealers with high porosity are more prone to microleakage, potentially causing periradicular fluids to infiltrate the root canal system. This infiltration can compromise the success of the root canal treatment, posing a risk to long-term clinical outcomes8,26.
Biodentine’s markedly higher porosity appears inconsistent with findings from a previous study27 comparing the porosity of Biodentine and ProRoot MTA against a pre-mixed cement, iRoot BP Plus (Innovative BioCeramix Inc., Vancouver, BC, Canada), and Ceramicrete. The study found no statistically significant differences in porosity among the materials tested. Nevertheless, despite the lack of significance, these earlier results indicated that Biodentine was more porous than ProRoot MTA, aligning with the current findings. Meanwhile, the pre-mixed calcium silicate-based cement exhibited the highest porosity. The differences observed in the current data might be attributed to using plastic molds instead of actual mandibular molars in that study and a small sample size per group (n = 4).
Furthermore, the results obtained in the current study do not align with those reported by Guerrero et al.19, who found significant differences in the porosity of Biodentine compared to White ProRoot MTA, with Biodentine demonstrating superior porosity properties in terms of both the number and volume of pores. However, it is important to note that their study did not use human molars, but rather 5 mm high silicone tubes, and the samples were not placed in a humidity chamber to simulate oral conditions. Additionally, the materials were let to set only 24 h, a detail that could influence the results. On the contrary, the present study demonstrated that ProRoot MTA and NeoPutty are effective materials for sealing furcal perforations, particularly in porosity control.
The current investigation also evaluated overfilling, which was observed across all groups, with ProRoot MTA exhibiting the lowest rate (25%), while NeoPutty and Biodentine both showed a higher overfilling rate of 33.3%. Overfilling can be particularly relevant in cases where the perforation site is close to critical anatomical structures, as it could cause inflammation, delayed healing, or potential interference with periradicular tissue regeneration. The presence of extruded material in crucial areas such as the furcal region may also jeopardize periodontal reattachment and raise the risk of treatment failure28. Interestingly, ProRoot MTA showed a lower overfilling rate, which may be attributed to its thicker consistency, allowing a more controlled application. On the contrary, NeoPutty, despite its pre-mixed formulation, may exhibit slightly lower viscosity, making it more prone to extrusion beyond the perforation site. Similarly, Biodentine presents a higher overfilling rate, probably due to its lower viscosity and faster setting time, which could make the materials harder to manipulate precisely before setting.
This study highlighted that pre-mixed calcium silicate-based cements achieved better gap reduction results regarding quantitative parameters. This is consistent with the findings of a recent study8, where Endosequence Fast Set Putty achieved significantly better outcomes. Both studies followed a similar clinical protocol, performing micro-CT assessments in extracted teeth. In this study, ProRoot MTA exhibited the highest gap percentage (6.48%), followed by Biodentine (2.40%) and NeoPutty, which showed the smallest gap percentage (1.03%).
However, when considering the absolute gap volume, Biodentine showed the highest value (1.37 mm3), followed by NeoPutty (0.85 mm3), with ProRoot MTA showing the lowest value (0.29 mm3). These findings indicate that despite having the highest gap percentage, ProRoot MTA had the smallest actual gap volume; this is probably explained by its higher adaptation and material density that compensate for its marginal gap presence. Conversely, Biodentine showed higher gap volume, supporting its lower adaptation performance, as observed in qualitative analyses. On the contrary, NeoPutty, with both a low gap percentage and moderate gap volume, demonstrated consistent adaptation, probably explained by its putty-like consistency, which allows for better flow and adaptation to the dentinal surface.
From a clinical perspective, these results highlight that adaptation and porosity are critical factors when choosing a repair material for furcation perforations. While all materials showed some voids and gaps, ProRoot MTA remains the most reliable, while NeoPutty offers a strong alternative. Indeed, NeoPutty emerged as the superior material in terms of both handling and porosity. Its pre-mixed nature eliminates the variability associated with on-site material mixing, which can introduce inconsistencies in performance, as seen with Biodentine, which requires careful handling due to its limitations8. .
Indeed, despite its shorter setting time, bioactivity, and ease of use in some clinical scenarios, Biodentine shows significantly higher porosity and lower adaptation rate, which limits its reliability for furcal perforation repair. This suggests that it might be better suited for other clinical applications, such as dentin replacement in non-load-bearing areas, where its shortcomings in adaptation and porosity are less critical29.
While the pre-mixed nature of NeoPutty offers significant clinical advantages in terms of ease of handling and reduced operator variability, it also introduces considerations regarding the setting reaction and long-term behavior. Unlike manually mixed materials, pre-mixed formulations may undergo a more gradual setting process that depends on environmental factors such as moisture and temperature. This could, in theory, influence the long-term maintenance of the favorable marginal adaptation and low porosity observed in the present study, which was limited to a one-week evaluation30. However, recent studies have demonstrated that NeoPutty maintains stable performance for at least six months in indirect pulp therapy, with success rates around 91.67%, comparable to Biodentine and superior to calcium hydroxide, although the differences were not statistically significant31,32. While the present study focused primarily on short-term adaptation and porosity, these external findings provide context supporting the clinical potential of NeoPutty beyond the one-week evaluation period.
Furthermore, although micro-CT can assess many parameters with high precision, the inclusion of qualitative assessments through clinical photographs and radiographs reflects routine diagnostic practice and enhances the applicability of the findings to real-world clinical scenarios.
The present results regarding NeoPutty’s favorable adaptation and low porosity are further supported by findings from Paulo et al.33, who reported that a comparable premixed calcium silicate-based material (TotalFill BC Putty, FKG, La Chaux-de-Fonds, Switzerland) exhibited significantly higher push-out bond strength than both Biodentine and MTA, regardless of blood contamination. This suggests that certain premixed formulations may combine ease of handling with reliable mechanical retention under clinically relevant conditions. However, as demonstrated by a previous study34, the interface with subsequent restorations requires careful consideration. Indeed, it was shown that the application of a hydrophobic resin bonding layer over a calcium silicate-based cement significantly enhanced shear bond strength and improved the morphology of the adhesive interface, resulting in thicker, more continuous hybrid layers and fewer defects. Clinicians should balance the immediate sealing properties highlighted in the present study with the long-term restorative challenges identified in these works.
While this study provides valuable results regarding the performance of different calcium silicate-based cements, several limitations should be acknowledged.
First of all, although adequate for detecting significant differences, the sample size could be expanded in future studies to increase the generalizability of the findings. Furthermore, although micro-CT is a powerful tool for evaluating internal and marginal integrity, it does not assess mechanical retention. Future studies should consider a multiparametric approach by combining microtensile bond strength (µTBS) or push-out bond strength testing to better correlate structural adaptation with mechanical performance, particularly for pre-mixed materials like NeoPutty. As highlighted in a previous study33, pre-mixed bioceramics can exhibit favorable bond strength properties, which should be considered alongside microstructural metrics.
Moreover, the ex vivo model employed does not replicate the full clinical environment. Notably, the effects of blood contamination, which may influence the setting behavior and interface of hydraulic calcium silicate cements, were not simulated. Studies such as Xavier et al.34 has shown that blood exposure can significantly alter material properties and compromise sealing ability, and this should be integrated into future research designs.
Additionally, this study did not investigate the interface between repair materials and restorative composites, which plays a crucial role in long-term sealing success. Previous studies35,36 indicate that the timing of restoration and compatibility can play a significant role in long-term outcomes in terms of adhesion and performance. Another shortcoming of this study is the absence of bacterial infiltration or biofilm challenge models. While NeoPutty exhibited the lowest porosity in our quantitative assessment, the extent to which this translates into superior resistance to microbial leakage remains unverified. Future studies should incorporate bacterial challenge protocols to determine whether lower porosity effectively reduces bacterial penetration, particularly in comparison to more porous materials such as Biodentine.
In terms of procedural limitations, although care was taken to control for extrusion, the open nature of the ex vivo model may have allowed minimal material overflow beyond the perforation site, which could influence sealing assessments and should be considered in the interpretation of results. Finally, the one-week evaluation period reflects only the short-term performance of these materials.
Long-term studies are necessary to assess the behavior of these cements under functional stresses, thermocycling, and bacterial challenge in order to predict their clinical durability more accurately. Moreover, although the present study focused primarily on internal adaptation, future research should also include targeted analysis of the external surface of the perforation, where the material interfaces with the periodontium. In addition, further in vivo investigations are essential to assess factors such as cytocompatibility, bioactivity, and tissue response.
In conclusion, this study’s findings suggest that NeoPutty is the most reliable material for furcal perforation repair, offering superior adaptation and the lowest porosity. ProRoot MTA remains a strong option, although its handling properties may present challenges in clinical settings. Biodentine, while advantageous in setting time, exhibits significant porosity and suboptimal adaptation, making it a less favorable choice for critical repair cases such as furcation perforations.
Data availability
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
References
Cardoso, M., Catré, D., Noites, R., Paulo, M. & Viegas, C. Animal models used in furcation perforation studies: A systematic review and comprehensive synthesis of model characteristics. Aust Endod J. 44, 273–280 (2018).
Silva, L. A. B. et al. Furcation perforation: periradicular tissue response to Biodentine as a repair material by histopathologic and indirect Immunofluorescence analyses. J. Endod. 43, 1137–1142 (2017).
Mente, J., Leo, M., Panagidis, D., Saure, D. & Pfefferle, T. Treatment outcome of mineral trioxide aggregate: repair of root perforations-long-term results. J. Endod. 40, 790–796 (2014).
Gorni, F. G., Andreano, A., Ambrogi, F., Brambilla, E. & Gagliani, M. Patient and clinical characteristics associated with primary healing of iatrogenic perforations after root Canal treatment: results of a Long-term Italian study. J. Endod. 42, 211–215 (2016).
Singh, P. et al. Sealing ability of mineral trioxide aggregate, calcium phosphate cement, and glass ionomer cement in the repair of furcation perforations. Acta Med. (Hradec Kralove). 56, 97–103 (2013).
Tawil, P. Z., Duggan, D. J. & Galicia, J. C. Mineral trioxide aggregate (MTA): its history, composition, and clinical applications. Compend Contin Educ. Dent. 36, 247–252 (2015). quiz 254.
Samuel, A., Asokan, S., Priya, G., Thomas, S. & P.R. & Evaluation of sealing ability of Biodentine™ and mineral trioxide aggregate in primary molars using scanning electron microscope: A randomized controlled in vitro trial. Contemp. Clin. Dent. 7, 322–325 (2016).
Toia, C. C., Teixeira, F. B., Cucco, C., Valera, M. C. & Cavalcanti, B. N. Volumetric evaluation of voids and gaps of different Calcium-Silicate based materials used in furcal perforations: A Micro-CT study. Dent J. (Basel) 10 (2022).
Siew, K., Lee, A. H. & Cheung, G. S. Treatment outcome of repaired root perforation: A systematic review and Meta-analysis. J. Endod. 41, 1795–1804 (2015).
Dawood, A. E., Parashos, P., Wong, R. H. K., Reynolds, E. C. & Manton, D. J. Calcium silicate-based cements: composition, properties, and clinical applications. J Investig Clin. Dent 8 (2017).
Nawal, R. R. et al. The influence of calcium silicate-based cement on osseous healing: A systematic review and meta-analysis. J. Conserv. Dent. 26, 122–133 (2023).
Marciano, M. A. et al. Assessment of color stability of white mineral trioxide aggregate Angelus and bismuth oxide in contact with tooth structure. J. Endod. 40, 1235–1240 (2014).
Ioannidis, K., Mistakidis, I., Beltes, P. & Karagiannis, V. Spectrophotometric analysis of coronal discolouration induced by grey and white MTA. Int. Endod J. 46, 137–144 (2013).
Torabinejad, M., Parirokh, M. & Dummer, P. M. H. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part II: other clinical applications and complications. Int. Endod J. 51, 284–317 (2018).
Madani, Z., Alvandifar, S. & Bizhani, A. Evaluation of tooth discoloration after treatment with mineral trioxide aggregate, calcium-enriched mixture, and Biodentine(®) in the presence and absence of blood. Dent. Res. J. (Isfahan). 16, 377–383 (2019).
Howait, M., Shaker, M., Aljuhani, H. & AlMohnna, M. External cervical resorption: A case report and brief review of the literature, and treatment algorithms. J. Contemp. Dent. Pract. 22, 298–303 (2021).
Moinzadeh, A. T., Aznar Portoles, C., Schembri Wismayer, P. & Camilleri, J. Bioactivity potential of endosequence BC RRM putty. J. Endod. 42, 615–621 (2016).
Koç, C., Aslan, B., Ulusoy, Z. & Oruçoğlu, H. Sealing ability of three different materials to repair furcation perforations using computerized fluid filtration method. J. Dent. Res. Dent. Clin. Dent. Prospects. 15, 183–187 (2021).
Guerrero, F. & Berástegui, E. Porosity analysis of MTA and Biodentine cements for use in endodontics by using micro-computed tomography. J. Clin. Exp. Dent. 10, e237–e240 (2018).
Nagendrababu, V. et al. PRILE 2021 guidelines for reporting laboratory studies in endodontology: A consensus-based development. Int. Endod J. 54, 1482–1490 (2021).
Huang, Y. et al. Evaluation of the sealing ability of different root Canal sealers: a combined SEM and micro-CT study. J. Appl. Oral Sci. 26, e20160584 (2018).
Bilvinaite, G., Drukteinis, S., Brukiene, V. & Rajasekharan, S. Immediate and Long-Term radiopacity and surface morphology of hydraulic calcium Silicate-Based materials. Materials (Basel) 15 (2022).
Ghasemi, N., Janani, M., Razi, T. & Atharmoghaddam, F. Effect of different mixing and placement methods on the quality of MTA apical plug in simulated apexification model. J. Clin. Exp. Dent. 9, e351–e355 (2017).
Basturk, F. B., Nekoofar, M. H., Gunday, M. & Dummer, P. M. Effect of varying water-to-powder ratios and ultrasonic placement on the compressive strength of mineral trioxide aggregate. J. Endod. 41, 531–534 (2015).
Sharifi, R., Araghid, A., Ghanem, S. & Fatahi, A. Effect of temperature on the setting time of mineral trioxide aggregate (MTA). J. Med. Life. 8, 88–91 (2015).
De Souza, E. T. et al. Tridimensional quantitative porosity characterization of three set calcium silicate-based repair cements for endodontic use. Microsc Res. Tech. 76, 1093–1098 (2013).
Souza, E. et al., Tridimensional Quantitative Porosity Characterization of Three Set Calcium Silicate-Based Repair Cements for Endodontic Use. Microscopy Res. Technique 76 (2013).
Asgary, S. & Fayazi, S. Endodontic surgery of a symptomatic overfilled MTA apical plug: A histological and clinical case report. Iran. Endod J. 12, 376–380 (2017).
Askerbeyli Örs, S., Aksel, H., Küçükkaya Eren, S. & Serper, A. Effect of perforation size and furcal lesion on stress distribution in mandibular molars: a finite element analysis. Int. Endod J. 52, 377–384 (2019).
Camilleri, J. Current Classification of Bioceramic Materials in Endodontics. in Bioceramic Materials in Clinical Endodontics (eds. Drukteinis, S. & Camilleri, J.) 1–6Springer International Publishing, Cham, (2021).
Acharya, S. & Gurunathan, D. Comparison of novel bioactive materials in indirect pulp therapy in deciduous teeth: an in vivo study. Pesquisa Brasileira Em Odontopediatria E Clínica Integrada 25 (2025).
Acharya, S. et al. Comparison of modified NeoPutty MTA®, Biodentine, and calcium hydroxide in indirect pulp therapy in deciduous teeth: an in vivo clinical study. Int. J. Clin. Pediatr. Dentistry. 17, 1025–1029 (2024).
Paulo, C. R. et al. Influence of blood contamination on Push-Out bond strength of three calcium Silicate-Based materials to root dentin. Appl. Sci. 11, 6849 (2021).
Xavier, M. T., Costa, A. L., Caramelo, F. J., Palma, P. J. & Ramos, J. C. Evaluation of the interfaces between restorative and regenerative biomaterials used in vital pulp therapy. Materials 14, 5055 (2021).
Palma, P. J. et al. Does delayed restoration improve shear bond strength of different restorative protocols to calcium Silicate-Based cements?? Materials 11, 2216 (2018).
Palma, P. J. et al. Effect of restorative timing on shear bond strength of composite resin/calcium silicate–based cements adhesive interfaces. Clin. Oral Invest. 25, 3131–3139 (2021).
Acknowledgements
The authors do not want to thank anyone in particular.
Author information
Authors and Affiliations
Contributions
Authorship Declaration: All authors contributed to the study’s conception and design. M.R: Investigation, Methodology, Data curation, Software. A.M.-D.: Investigation. J.M.C: Conceptualization, Methodology, Data curation, Investigation. N.N: Conceptualization, Investigation, Supervision. A.R.P: Writing- Reviewing and Editing, Conceptualization, Supervision. G.M.: Writing-Reviewing and Editing, Data curation J.A: Investigation, Supervision. D.R.-F.: Conceptualization, Investigation, Reviewing and Editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
José Aranguren and Alejandro R. Pérez are the opinion leaders of ZARC (Zarc4endo, Gijón, Asturias, Spain), and Juan Miraglia Cantarini is the opinion leader of Dentsply (Dentsply-Sirona, Baillagues, Switzerland). The other authors deny any conflicts of interest.
Ethics approval and consent to participate
The Rey Juan Carlos institutional ethics committee approved the study (protocol 1301202302823).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rojo-Carpintero, M., Martín-Díaz, A., Cantarini, J.M. et al. Marginal adaptation and porosity of calcium silicate-based cements in furcation perforations: a micro-CT comparative study. Sci Rep 15, 19244 (2025). https://doi.org/10.1038/s41598-025-03729-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-03729-7