Abstract
Closed reduction with external fixation (CREF) and percutaneous pinning (CRPP) are commonly used surgical interventions to treat distal radius fractures. However, there is no consensus regarding the optimal management of these types of fractures. Therefore, this study aimed to compare these treatments’ clinical and radiological outcomes in two subgroups of distal radius fractures. The patients who were ≥ 18 and were referred for the diagnosis of type I and III (Fernandez) distal radius fractures were treated with one of these two methods, which have been evaluated through a retrospective analysis of the medical records. A total of 244 patients were divided into CREF treatment (n = 122) and control treatment (n = 122). These patients’ radiological, clinical, functional, and incidence rates of complications (over-distraction, radial neuropathy, and deep or superficial infection) were compared to analyze each method’s positive and negative aspects. This study showed that patients in the PP group reported significantly less pain than those in the EF group (P-value < 0.05). The PP group scored lower in the specific and general activities categories, significantly reducing Patient-Rated Wrist Evaluation (PRWE). Although the CREF group had greater radius shortening, the difference was not statistically significant. Notably, the CREF group exhibited a significantly higher incidence of complications. Percutaneous pinning proved to be a more effective method for treating distal radius type I and III fractures. Compared to those treated with external fixation, patients experienced fewer post-treatment complications, lower pain levels, and less difficulty in daily activities.
Similar content being viewed by others
Introduction
One of the most common fractures is seen in 0.36% of trauma-related visits to emergency departments and 1.8% of upper extremity traumas1. This fracture type is significantly higher in pediatrics (high-energy traumas such as sports-related injuries)2,3 and geriatrics with lower bone density (low-energy traumas such as falling)4,5. Many social and personal implications, such as a remarkable financial burden, absence from work and school, decreased independence, and long-term disabilities, accompany these fractures6. There is no consensus regarding the optimal therapeutic strategies for this type of fracture, including surgical and non-surgical methods7. However, before this decision, it is important to consider pain management, immobilization, and evaluation for open fractures or neurovascular injuries, which should be ruled out by orthopedic or, if necessary, vascular surgeons8. Considering the fracture type, the patient’s preference, available devices, expertise, and the anatomy of the fracture location are crucial in selecting the surgery type9. Many studies have underscored the closed reduction and internal fixation (CRIF) method as the most efficient surgical method8. Others declared external fixation with volar locking plates a significantly more efficient technique that improved short-term recovery10. However, closed reduction is mainly used to treat these fractures. The fixation of the fracture must also be selected appropriately since this can affect the outcome of the limb’s function and the treatment’s recovery time and costs11. There is no clear and well-illustrated comparison between fixation methods, and different and sometimes reverse outcomes have been declared12.
Although multiple randomized trials and observational studies have explored the outcomes of various distal radius fracture fixation methods13,14, few have directly compared closed reduction with external fixation (CREF) versus closed reduction with percutaneous pinning (CRPP) specifically for Fernandez type I and III fractures15. Moreover, the existing literature shows heterogeneous conclusions regarding functional recovery, complication rates, and radiographic parameters, often due to differences in fracture classification, patient selection, or surgical technique10,12,14,15,16,17,18,19. As such, there remains a gap in the consensus over the preferred approach for specific fracture types in routine clinical settings12,16,19. This study addresses this knowledge gap by conducting a large retrospective comparative analysis focused exclusively on Fernandez type I and III fractures. We strive to evaluate the clinical and radiological outcomes, complication profiles, and patient-reported function between these two frequently used surgical methods, thereby helping refine decision-making in distal radius fracture management.
Materials and methods
A retrospective comparative cohort study analyzing patient files was conducted at Imam Khomeini and Golestan hospitals in Ahvaz. The study included patients aged 18–60 years with distal radius type I and III Fernandez injuries (Table 1), who were treated with either external fixators or closed reduction using percutaneous pinning and casting more than 6 months before the start of the study. Patients with significant comorbidities, associated neurological or vascular injuries, osteoporosis, fractures in the contralateral upper limb, multiple traumas, pregnancy or uncertainty regarding their pregnancy, and open-angle fractures were excluded from the study (Table 2). A total of 244 eligible patients were analyzed in two groups. The first group consisted of patients who underwent CRPP under C-ARM in the operating room. The second group included patients who underwent CREF under C-ARM in the operating room. Demographic information, such as age, gender, and cause of injury, was extracted and recorded from hospital records.
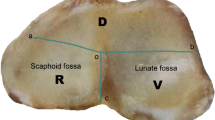
An independent orthopedic surgeon conducted the clinical evaluation and improved patients’ functional status without knowing the treatment type. The clinical assessment utilized the DASH score (Disability of Arm, Shoulder, and Hand) and the PRWE score (Patient-Rated Wrist Evaluation) questionnaires (Supplementary file 1)20. Additionally, plain anterior-posterior and lateral X-rays were requested for radiological assessment, and patients were asked to bring their post-operative X-rays. The wrist X-ray evaluation classified the radiologic outcome as acceptable if the shortening of the radius was less than 5 mm and the volar tilt was zero degrees; otherwise, the result was deemed unacceptable. Surgery-related complications, including over-distraction, superficial radial nerve injury, and deep or superficial surgical site infection, were examined and documented during the evaluation (Fig. 1).
Statistical analysis
The data were analyzed using SPSS software version 22, with a significance level of less than 0.05. This study reported the results using descriptive statistics, including mean, standard deviation (SD), frequency, and percentage. Additionally, an independent t-test or a Mann-Whitney test was utilized based on the distribution of quantitative variables. For qualitative variables, the chi-square test was employed to compare the averages of the investigated variables between the two groups.
Ethical declaration
The project received approval from the Ahvaz Jundishapur University of Medical Sciences (AJUMS) ethics committee (IR.AJUMS.REC.1395.168). Informed consent was obtained from the participants, who could withdraw from the study at any time. All study steps were designed and conducted under the confidentiality policy of the Ahvaz Jundishapur University of Medical Sciences (AJUMS).
Results
The main demographic features of both groups of participants, such as their ages, genders, mechanisms of injury, and the involved side, were extracted from their files (Table 3).
There was no significant difference in the average age between the CRPP and CREF groups. Additionally, the age-related factor did not notably impact the outcomes for either group. In both groups, the number of male patients exceeded that of female patients; however, there was no significant difference in gender distribution between the two groups. The follow-up period for patients in the CRPP group ranged from 26 to 56 months, and from 23 to 58 months for those in the CREF group. There was no significant difference in the average follow-up time between the two groups at their last examinations.
The group of patients receiving CRPP treatment had lower pain scores and better outcomes in specific and general activities than those in the CREF group. Furthermore, patients in the CRPP group reported fewer difficulties in their daily activities. The CRPP group’s total PRWE score was significantly lower than that of the CREF group, and the functional improvement in the CRPP group was approximately 50% greater than that of the CREF group, with a notable difference observed. In the final follow-up, patients in both groups were assessed using the DASH scoring criteria. The total DASH score was significantly lower in the CRPP group than in the CREF group (Table 4). The DASH questionnaire consists of 30 questions, each with five qualitative responses, scored from 1 to 5. The total score is calculated, with a lower score indicating better function.
The patients’ radiological results were thoroughly analyzed, specifically regarding the extent of radiation shortening and volar tilt. The results revealed that the CREF group had a higher average radius shortening than the CRPP group. However, no statistically significant difference existed between these two groups. Additionally, while the volar angle was higher in the CRPP group, there was no significant difference between the two groups.
The CREF group exhibited a higher incidence of complications, and this difference was statistically significant. Radial superficial nerve damage was the most common complication among those treated with plaster pins, while superficial infections were more frequent in the external fixative group. Both groups experienced straightforward conditions and required only regular dressings without oral antibiotic treatment. No deep-seated infections occurred, which would have necessitated the removal of fixation devices or pins in either group. Two patients in the external fixative group experienced neuroma pain in the area of the injury due to nerve damage, as diagnosed by their surgeon. Fortunately, both patients achieved satisfactory outcomes.
Discussion
Restoration of function and range of motion, while imposing minimal complications, is the primary purpose of DRF treatment21, mainly achieved after restoring anatomical alignment and articular congruity after the intervention10,17. The main pillars of the initial steps of DRF management are control of pain and immobilization of the joint22,23. Closed reduction with external fixation (CREF) and closed reduction with fixation using percutaneous pin (CRPP) are two commonly used fixation methods for these fractures11,16. The external fixator, widely used for DRF, has benefits such as lower surgery time, less surgery-related trauma, and a more straightforward procedure24,25,26,27. They are also effective in treating soft tissue loss or internal fixation due to concomitant traumas or risk of infection in the surgical site28. However, some studies concluded that there was no remarkable superiority in the outcome of EFs in comparison with locking plates18 or others, which emphasized a higher risk of surgery site infection, loss of grip strength, traction of the pins, restricted finger movement, or radial nerve injury with EFs treatment10. On the other hand, although the favorable efficacy and appropriate outcomes of the CRPP method as a treatment for DRF have been shown in several studies11,19, others have concluded there was a lack of superiority of CRPP over other options16. There has yet to be a consensus among previous publications9.
Distal radius fractures have a wide range of clinical presentations. However, the crucial point in managing these patients is having a holistic and systemic approach and not missing probably more vital injuries29,30. Therefore, indicators of severe injuries that might change the therapeutic strategy, such as any sign of open fracture, hints of compartment syndrome, or neurovascular injuries, should be investigated in the physical exam31. By evaluating radial height and inclination, articular step-off, and dorsal angulation in the patient’s Xray, these fractures are categorized (Smith’s, Colle’s, Torus/Buckle, Greenstick, and Die-punch) and considering clinical and personal features (bone quality, injury mechanism, patient’s age, occupation, and financial status and surgeon’s skills) the treatment plans are determined12,32,33,34. Non-surgical management of DRFs is considered appropriate when specific radiographic criteria are met. Radial length shortening should be less than 5 mm, and changes in radial inclination should not exceed 5 degrees. An articular step-off must be less than 2 mm to minimize joint incongruity, and dorsal angulation should be less than 5 degrees or within 20 degrees of the contralateral distal radius. These parameters are essential for assessing fracture alignment and determining suitability for conservative treatment35.
The strategy selected for the fixation of bones has always been controversial in DRF treatment10,17. External fixators (EF) and percutaneous pins (PP) are standard methods evaluated in the current study for treating type I and III distal fractures of the radius. The study aimed to determine a preferred therapeutic technique for these types of fractures based on a statistical analysis of patients’ PRWE and DASH scores, their history of pain and difficulty experienced, and the incidence of complications, including over-distraction, radial nerve damage, and infection. The results indicated that patients treated with CRPP had significantly better pain scores, general and specific functional scores, lower difficulty in their daily activities, and superior radiological indices. These results are inconsistent with those of a study by Hutchison et al., which compared the outcomes and complication rates in treatments using EF, pins, and casts. Although their study was similar to ours, the overall functional outcomes for both groups were excellent, with no significant differences. In their study, EF performed better in maintaining radial length13. They also found no difference between the two groups regarding major complications, even though the rate of minor complications was higher in the EF group. This finding is not consistent with our study’s results. The inconsistency between these two studies might be attributed to differences in the studied patients. Participants in Hutchison’s study had unstable DRFs, while we did not place limits on our patients regarding the specific severity of the fracture. Another study by Jafari et al. compared two methods of external fixation. The overall outcomes of both fixator groups were acceptable, and their results showed more favorable statistics than those in our study. The discrepancy between the two studies appears to stem from the differences in study participants. This outcome contrasts with our study, which did not focus on the specific severity of the distal radius fractures, whereas Jafari et al.’s study included only unstable fractures14.
Despite the presence of the mentioned positive aspects of EF, there are serious concerns about their complications, such as malunion, acute carpal tunnel syndrome, stiffness in wrists and fingers, over-distraction, and infection as the most prevalent complication of EFs in the distal radius, with an incidence rate of up to 37%36,37,38,39,40. Previous studies have reported superficial radial nerve injury as a complication of percutaneous pin fixation, which more commonly occurs during the removal of the pins41. However, our recent study shows that the complication rates mentioned were lower than in most previous studies and lower in the CRPP than in CREF. Our findings showed that the incidence of infection is lower at 13.93%, but it is still more common in the group treated with CREF. We did not observe the two types of complications reported in previous studies: superficial and deep-seated. The latter requires the removal of the fixation or pins. Our study found that complications were significantly higher in the group treated with external fixation compared to the pin and gypsum method. These findings offer valuable insights for medical professionals treating patients with radial nerve damage.
This study was performed in two tertiary referral centers for orthopedic surgeries, and a wide range of epidemiologic features were included in the participants. However, since it was a retrospective evaluation, there was a significant variety among the patients regarding the time that had passed since their surgeries. Moreover, it was only possible to examine some eligible cases due to the need for more consistency in recording the patients’ information and the percentage of eligible participants living far from these two centers. The other limitation factor was the difference between surgeons, anesthesiologists, and the setting of the operation. It might have caused minor bias in the result, even though most basic characteristics were similar between the two groups of surgeons. It is highly recommended that future authors investigate the pros and cons of these methods in a prospective study with a single surgical and anesthesia team and a unified surgical setting.
Conclusion
This study compared two common surgical treatments for distal radius fractures. The study results showed superior general and specific functional outcomes in the CRPP group compared to CREF. Moreover, the difference in the complication rate and pain experienced by these two groups of patients was statistically significant in favor of the CRPP. The overall rate of complications in both groups was lower than most of the previously reported rates.
Data availability
The data that supports this study’s findings are available from the corresponding author, AH, upon reasonable request.
Abbreviations
- AJUMS:
-
Ahvaz Jundishapur University of Medical Sciences
- C-ARM:
-
C-arm X-ray machine
- CREF:
-
Closed reduction with external fixation
- CRIF:
-
Closed reduction and internal fixation
- CRPP:
-
Closed reduction and percutaneous pinning
- DASH:
-
Disability of arm, shoulder, and hand
- DRF:
-
Distal radius fracture
- EF:
-
External fixator
- IRB:
-
Institutional review board
- PP:
-
Percutaneous pinning
- PRWE:
-
Patient-rated wrist evaluation
- SD:
-
Standard deviation
- SPSS:
-
Statistical package for the social sciences
References
Chinta, S. R. et al. Epidemiology of distal radius fractures: elucidating mechanisms, comorbidities, and fracture classification using the National trauma data bank. Injury 55 (2), 111217 (2024).
Cooper, C. et al. Epidemiology of childhood fractures in Britain: a study using the general practice research database**. J. Bone Miner. Res. 19 (12), 1976–1981 (2004).
Ward, W. T. & Rihn, J. A. The impact of trauma in an urban pediatric orthopaedic practice. JBJS 88 (12), 2759–2764 (2006).
Luokkala, T. et al. Distal radius fractures in the elderly population. EFORT Open. Rev. 5 (6), 361–370 (2020).
Flinkkilä, T. et al. Epidemiology and seasonal variation of distal radius fractures in Oulu, Finland. Osteoporos. Int. 22 (8), 2307–2312 (2011).
Neiman, R. Focal dome osteotomy for the treatment of diaphyseal malunion of the lower extremity. Medicina 58 (2), 308 (2022).
Haslhofer, D. J. et al. Comparison of surgical and conservative therapy in older patients with distal radius fracture: a prospective randomized clinic al trial. J. Orthop. Traumatol. 25 (1), 46 (2024).
Corsino, C. B., Reeves, R. A. & Sieg, R. N. Distal Radius Fractures (StatPearls [Internet], 2023).
Shapiro, L. M. & Kamal, R. N. Distal radius fracture clinical practice guidelines-updates and clinical implications. J. Hand Surg. Am. 46 (9), 807–811 (2021).
Ermutlu C, Mert M, Kovalak E, Kanay E, Obut A, Öztürkmen Y. Management of Distal Radius Fractures: Comparison of Three Methods. Cureus 12(8):e9875. https://doi.org/10.7759/cureus.9875 . PMID: 32963915; PMCID: PMC7500733.
Özkan, S. et al. Distal radius fractures: evaluation of closed reduction and percutaneous Kirschner wire pinning. J. Hand Microsurg. 10 (3), 134–138 (2018).
Chhabra, A. B. & Yildirim, B. Adult distal radius fracture management. JAAOS-J. Am. Acad. Orthop. Surg. 29 (22), e1105–e1116 (2021).
Hutchinson, D., Strenz, G. & Cautilli, R. Pins and plaster vs external fixation in the treatment of unstable distal radial fractures: a randomized prospective study. J. Hand Surg. 20 (3), 365–372 (1995).
Jafari, D. et al. Treatment outcomes of applying external fixator on distal radius fractures: a randomized clinical trial to compare between two directions of force exertion in parallel to radius shaft and perpendicular to the distal radius articular surface. BMC Musculoskelet. Disord. 24 (1), 283 (2023).
Kleinlugtenbelt, Y. V. et al. Classification systems for distal radius fractures: does the reliability improve using additional computed tomography? Acta Orthop. 88 (6), 681–687 (2017).
Søsborg-Würtz, H. et al. Closed reduction of distal radius fractures: a systematic review and meta-analysis. EFORT Open. Reviews. 3 (4), 114–120 (2018).
Talmaç, M. A. et al. Comparison of Three Surgical Methods in the Treatment of Intraarticular Comminuted Distal Radius Fractures: Volar Locking Plate, non-bridging External Fixator, and Bridging External Fixator30p. 224–232 (Eklem Hastaliklari ve Cerrahisi = Joint Diseases & Related Surgery, 2019). 3.
Wang, D., Shan, L. & Zhou, J. L. Locking plate versus external fixation for type C distal radius fractures: a meta-analysis of randomized controlled trials. Chin. J. Traumatol. 21 (02), 113–117 (2018).
Zhao, B. et al. A novel retractor-assisted closed reduction combined with percutaneous pinning fixation for the treatment of elderly distal radius fractures: a retrospective cohort study. J. Orthop. Surg, Res. 16 (1), 409 (2021).
Changulani, M. et al. Outcome evaluation measures for wrist and hand: which one to choose? Int. Orthop. 32 (1), 1–6 (2008).
Trumble, T. E. et al. Intra-articular fractures of the distal aspect of the radius. Instr. Course Lect. 48, 465–480 (1999).
Tseng, P. T. et al. Hematoma block or procedural sedation and analgesia, which is the most effective method of anesthesia in reduction of displaced distal radius fracture? J. Orthop. Surg. Res. 13 (1), 62 (2018).
Yim, G. H. & Hardwicke, J. T. The evolution and interpretation of the Gustilo and Anderson classification. J. Bone Joint Surg. Am. 100 (24), e152 (2018).
Daumillare, A. et al. Volar locking plate fixation of distal radius fractures: isokinetic assessment of the influence of an ulnar styloid process fracture on pronation-supination strength. Hand Surg. Rehabilitation. 39 (1), 23–29 (2020).
Costantino, C. et al. Isokinetic strength test and functional outcomes in proximal humeral fractures treated with a locking plate. J. Orthop. Sci. 19 (5), 776–785 (2014).
Verdano, M. A. et al. Strength recovery after proximal humeral fractures treated with locking plate. Musculoskelet. Surg. 98 (1), 61–69 (2014).
Hammer OL, Clementsen S, Hast J, Šaltytė Benth J, Madsen JE, Randsborg PH. Volar Locking Plates Versus Augmented External Fixation of Intra-Articular Distal Radial Fractures: Functional Results from a Randomized Controlled Trial.J Bone Joint Surg Am. 101(4):311–321 (2019).
Taylor, K. F. et al. Restoring volar Tilt in AO type C2 fractures of the distal radius with unilateral external fixation. J. Hand Surg. Am. 42 (7), 511–516 (2017).
Mauck, B. M. & Swigler, C. W. Evidence-based review of distal radius fractures. Orthop. Clin. North. Am. 49 (2), 211–222 (2018).
Rodríguez-Merchán EC. Pediatric fractures of the forearm. Clin Orthop Relat Res 432:65–72. PMID: 15738805. (2005).
Walenkamp, M. M. et al. The unstable distal radius fracture-how do we define it? A systematic review. J. Wrist Surg. 4 (4), 307–316 (2015).
Medoff, R. J. Essential radiographic evaluation for distal radius fractures. Hand Clin. 21 (3), 279–288 (2005).
Caldwell, R. A., Shorten, P. L. & Morrell, N. T. Common upper extremity fracture eponyms: a look into what they really mean. J. Hand Surg. Am. 44 (4), 331–334 (2019).
Bell, J. A. et al. The pitfalls of difficult distal radius fractures and provisional reduction. Orthop. Clin. North. Am. 55 (1), 113–122 (2024).
Hsu, H., Fahrenkopf, M. P. & Nallamothu, S. V. Wrist Fracture, in StatPearls. StatPearls Publishing Copyright © 2023, StatPearls Publishing LLC.: Treasure Island (FL). (2023).
Anderson, J. T., Lucas, G. L. & Buhr, B. R. Complications of treating distal radius fractures with external fixation: a community experience. Iowa Orthop. J. 24, 53–59 (2004).
Hayes, A. J., Duffy, P. J. & McQueen, M. M. Bridging and non-bridging external fixation in the treatment of unstable fractures of the distal radius: a retrospective study of 588 patients. Acta Orthop. 79 (4), 540–547 (2008).
Cooney, W.P. External fixation of distal radial fractures. Clin. Orthop. Relat. Res. 180, 44–49 (1983).
Papadonikolakis, A. et al. The effect of increasing distraction on digital motion after external fixation of the wrist. J. Hand Surg. Am. 30 (4), 773–779 (2005).
Kaempffe FA, Walker KM. External fixation for distal radius fractures: effect of distraction on outcome. Clin Orthop Relat Res.380:220–225. (2000)
Karantana, A., Handoll, H. H. & Sabouni, A. Percutaneous pinning for treating distal radial fractures in adults. Cochrane Database Syst. Rev., 2(2): Cd006080. (2020).
Funding
The authors declared that this study has not received financial support from any organization.
Author information
Authors and Affiliations
Contributions
PE, AH, and RN contributed to the study’s design, data collection, and supervision. SM and MF evaluated the patients’ clinical and radiologic outcomes. BH, HT, and MM wrote the initial draft of the manuscript and designed the graphs and tables. NS, MG, and AH contributed to the data analysis, the paper’s revision, and the writing of the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board
The project was approved by the Ahvaz Jundishapur University of Medical Sciences (AJUMS) ethics committee (IR.AJUMS.REC.1395.168). Informed consent was obtained from the participants. Patients were able to withdraw from the study whenever they intended. All study steps were designed and performed based on the confidentiality policy of the Ahvaz Jundishapur University of Medical Sciences (AJUMS).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nazari, R., Mousavi, S., Fakoor, M. et al. Comparative analysis of closed reduction with external fixation versus closed reduction with percutaneous pinning for distal radius fractures. Sci Rep 15, 19147 (2025). https://doi.org/10.1038/s41598-025-04001-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04001-8