Abstract
The symptoms of coronavirus disease 2019 (COVID-19) range from severe lung disease to milder manifestations, such as cough and throat irritation. As a bisbenzylisoquinoline alkaloid, cepharanthine (CEP) has various pharmacological properties, such as antifibrotic, anti-inflammatory, antioxidant, and antiviral effects. However, its poor solubility and low bioavailability hinder subsequent drug development. Inclusion complex technology is a well-established drug delivery method that improves drug bioavailability. Therefore, in our study, we encapsulated CEP with β-cyclodextrin and formulated it into oral tablets. Oral tablets can be absorbed through sublingual and buccal mucosa, improving CEP bioavailability, facilitating convenient dosing, and thereby enhancing its therapeutic efficacy. The cepharanthine–β-cyclodextrin (CEP–β-CD) inclusion complex was prepared using the co-grinding method. It was characterized using scanning electron microscopy, X-ray diffraction, Fourier transform infrared spectroscopy, and differential scanning calorimetry to assess its physicochemical properties. Subsequently, the quality of the CEP–β-CD oral tablets was evaluated according to the relevant requirements of the 2020 edition of the Chinese Pharmacopoeia. Furthermore, the pharmacokinetic characteristics of the oral tablets were assessed in beagles. Finally, the anti-inflammatory effects of the CEP–β-CD oral tablets were evaluated in alveolar macrophage MH-S cells and a mouse pneumonia model. Our results suggest that the formulation of the CEP–β-CD inclusion complex into oral tablets is a promising preventive and therapeutic approach for lung injury caused by COVID-19.
Similar content being viewed by others
Introduction
Coronavirus disease 2019 (COVID-19), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a novel form of pneumonia that has profoundly influenced human society and posed significant challenges to global public health1. The term “Long COVID” was first coined in 2020 and is defined as the persistence of multisystem symptoms following seemingly “mild” SARS-CoV-2 infections2, primarily including cough, dyspnea, and respiratory distress3, which significantly impair patients’ quality of life. In 2022, 6.9% of American adults reported experiencing Long COVID, with the highest prevalence (8.9%) observed among individuals aged 35–49 years4. For lung injuries associated with Long COVID, current clinical practice involves the administration of antiviral drugs, such as remdesivir5, nirmatrelvir-ritonavir6, and molnupiravir7. However, the efficacy of these drugs remains modest, underscoring the need for more effective therapeutic strategies.
Cepharanthine (CEP), a bisbenzylisoquinoline alkaloid extracted from Stephania cepharantha HAYATA8, is primarily used in clinical settings to treat leucopenia in patients with cancer following radiotherapy or chemotherapy9. In addition, CEP has antitumor, antifibrotic, antibacterial, anti-inflammatory, antioxidant, antiviral, and other pharmacological effects10. Several studies have reported that CEP exerts its anti-inflammatory effects by reducing NLRP3 inflammasome activation11 and inhibiting the MAPK and NF-κB p65 signaling pathways12,13; moreover, it suppresses the production of inflammatory cytokines, such as TNF-α and IL-6, in lipopolysaccharide (LPS)-stimulated dendritic cells14. However, CEP development faces challenges such as poor solubility and low bioavailability. An absolute bioavailability of 5.65% ± 0.35% following oral administration has been reported in rats, accompanied by slow distribution and elimination, indicating its limited absorption15. Researchers have developed a self-emulsifying drug delivery system encapsulating CEP to enhance its oral bioavailability in rats. Nevertheless, optimizing such formulations is a complex, multistep process, limiting their clinical applicability16. Therefore, a simple, effective, and convenient CEP delivery method could enhance its bioavailability, potentially contributing to the prevention and treatment of lung injury caused by Long COVID.
Inclusion complexes are ultrasmall drug carriers that can improve drug bioavailability. Currently, the most common inclusion complex drug carrier is cyclodextrin (CD)17, a cyclic oligosaccharide with a truncated cone structure classified as “Generally Recognized as Safe” by the United States Food and Drug Administration. Its external surface contains numerous hydroxyl groups, which contribute to its high-water solubility. Conversely, the hydrogen and oxygen atoms within its glycosidic bonds make its cavity hydrophobic. Hydrophobic compounds can be encapsulated within CD, thereby enhancing their water solubility18. Compared with drug monomers, inclusion complexes formed between drugs and CD offer the following advantages: (1) improved drug solubility and bioavailability19, (2) enhanced physicochemical stability and prolonged drug shelf life20, and (3) reduced or eliminated unpleasant odors associated with drugs21.
In this study, an oral CEP–β-CD tablet was formulated using inclusion complex technology to enhance CEP bioavailability and potentially prevent and treat lung injuries associated with Long COVID. CEP was encapsulated within the hydrophobic cavity of β-CD to improve its water solubility. The administration route of the oral tablet was designed to increase CEP bioavailability through sublingual and buccal mucosa absorption, thereby augmenting its therapeutic efficacy. Various techniques were used to analyze the physicochemical properties of the CEP–β-CD inclusion complex, including Fourier transform infrared spectroscopy (FT-IR), scanning electron microscopy (SEM), differential scanning calorimetry (DSC), powder X-ray diffraction (XRD), encapsulation efficiency, and drug dissolution. Subsequently, quality control tests were conducted, encompassing weight variation, friability, hardness, and disintegration time. In addition, the pharmacokinetic properties of the oral tablets were evaluated in beagles. Finally, the anti-inflammatory effects of the CEP–β-CD oral tablets were assessed in alveolar macrophage MH-S cells and in a mouse model of pneumonia. These evaluations aimed to provide insights into the potential therapeutic benefits of this novel formulation in mitigating lung injury caused by Long COVID.
Materials and methods
Materials
CEP (purity 98%, 0200328–220301 C) was purchased from Chengdu Jianteng Technology Co; β-CD (A02847) was purchased from Beijing Enocai Technology Co., Ltd; Dextrin (950418) was purchased from Chengdu Lichun Chemical Factory; Talc (010115) was purchased from Beijing Yanjing Pharmaceutical Factory; Aspartame (A75648) was purchased from Beijing Innochem Technology Co., Ltd.; Carboxymethylstarchna (A20201201) was purchased from Shandong Liaocheng Ahua Pharmaceutical Co., Ltd.; Lipopolysaccharide (L6529) was purchased from Israel.
Cell lines and animals
The MH-S cell line (Catalog Number: STCC20007) was obtained from Wuhan Service Bio Technology Co., Ltd. The cells were cultured in RPMI-1640 medium supplemented with 10% fetal bovine serum, 100 U/mL penicillin, and streptomycin (all from Wuhan Servicebio Technology Co., Ltd.). The cells were maintained in a 5% CO2 atmosphere (Thermo, VIOS 160i) at 37 °C.
Twenty male C57BL/6J mice (20 ± 3 g, 8 weeks old) were purchased from Spebio Biotechnology Co., Ltd. (Beijing, China). In addition, four beagle dogs were acquired from Beijing Jinmuyang Laboratory Animal Breeding Co., Ltd. All mice and dogs were cared for according to the standard feeding guidelines for experimental animals. The animal study protocol was approved by the Institution of Animal Care and Use Committee, Academy of Military Medical Science (IACUC-DWZX-2024-P626, Beijing, China).
Phase solubility analysis
An appropriate amount of β-cyclodextrin is weighed out, dissolved in ultrapure water, and the volume is adjusted to 50 mL. Solutions with concentrations of 0.5, 10, 15, 20, 25, and 30 mM are prepared. A certain amount of CEP is added to each concentration solution, and the mixtures are sonicated for 30 min. The solutions are then placed in a constant temperature shaker for 24 h. They are filtered through a 0.45 μm filter. Appropriate amounts of the filtrate are taken and diluted to certain concentrations. A UV-Vis spectrophotometer is used to determine the CEP content in the supernatants at the corresponding wavelengths. The solubility curve of the CEP–β-CD inclusion complex is plotted, with β-CD concentration as the horizontal axis and CEP concentration as the vertical axis. The stability constant K, which represents the complexation constant of the CEP–β-CD inclusion complex, is a characteristic parameter for characterizing the strength of complexation. It is calculated according to the following formula22.
S0 is the solubility at zero cyclodextrin concentration.
Preparation and characterization of the CEP–β-CD inclusion complex
The CEP–β-CD inclusion complex was prepared by grinding, with the optimal formulation of a 1:1 mass ratio (CEP: β-CD). In particular, CEP was dissolved in absolute ethanol, whereas β-CD was dissolved in excess deionized water at 37 °C to form a suspension. These two solutions were mixed and co-ground in a mortar under light-protected conditions for 30 min. Subsequently, the mixture was placed in an oven and dried at 40 °C for 24 h to remove the solvents22.
Surface morphology
The CEP-β-CD inclusion complex surface morphology was examined using Field Emission SEM (Sigma 500, ZEISS, Germany). The samples were coated with gold using a magnetron sputtering device, and Bruker XFlash 6130 was used as the energy-dispersive X-ray spectroscopy system.
XRD
The prepared CEP-β-CD inclusion complex’s crystallinity was detected with XRD. The samples were scanned from 5° to 60° (2θ) at a speed of 2°/min using an X-ray powder diffractometer (Bruker D8 Advance, Bruker, Germany).
FT-IR
The potential interactions between the components of the CEP–β-CD inclusion complex and the characteristic absorption peaks of each substance were analyzed using FT-IR (FT-IR-1500, Zhongshiwoke Technology Development Co., Ltd.). The samples were uniformly mixed with KBr particles, ground into fine powder, and compressed into thin wafers. The infrared spectra of the samples were collected within the wavelength range of 500–4000 cm−1.
DSC
The CEP-β-CD inclusion complex melting point changes were measured with a simultaneous thermal analyzer (NETZSCH STA 449F3, Germany). The samples were heated at 10 °C/min within a temperature range of 30–500 °C. The weight of each sample was approximately 10 mg.
Determination of encapsulation efficiency
Approximately 20 mg CEP–β-CD inclusion complex was weighed and dissolved in 10 mL absolute ethanol. The solution was diluted 40 times and filtered through a 0.22-µm filter membrane, and the free CEP content in the solution was measured using a UV–Vis spectrophotometer (UV-2600, Shimadzu, Japan). The encapsulation efficiency was calculated using the formula:
Particle size
The particle size analysis of CEP–β-CD inclusion complex was performed with Dry Laser Particle Size Analyzer (BT-2001, Dandong Bate Instrument Co., Ltd.)
Preparation and characterization of CEP–β-CD inclusion complex oral tablets
Oral tablets were prepared using the powder direct pressing method as follows: 1.2 g of CEP–β-CD inclusion complex, 50 mg of aspartame as a sweetener, 200 mg of dextrin as a filler and binder, 20 mg of CMS-Na (sodium carboxymethyl starch) as a disintegrant, and 30 mg of talc as a glidant and lubricant were mixed in equal amounts and pressed into tablets with a rotary tablet press (ZP-15, Shanghai Tianfeng Pharmaceutical Equipment Co., Ltd.). Each tablet weighed 150 mg.
Tablet weight variation
Twenty randomly selected CEP–β-CD inclusion complex oral tablets were precisely weighed using an electronic analytical balance (BS110S, Beijing Sartorius Balance Co., Ltd.). The total weight was divided by 20 to calculate the average weight per tablet. Subsequently, the weights of the 20 oral tablets were sequentially measured and recorded.
Friability
Twenty CEP–β-CD inclusion complex oral tablets were placed into the two cylinders of a friability tester (CS-A, Tianjin Pharmacopoeia Standard Instrument Factory). The tablets were rotated 100 times. After removal, detached powder was blown away with an air blower, and the tablets were precisely weighed. The weight change of each buccal tablet was recorded23.
Hardness
Five randomly selected CEP–β-CD inclusion complex oral tablets were subjected to hardness testing using a Tablet Hardness Tester (YPD-300D, Shanghai Huanghai Pharmaceutical Testing Instrument Co., Ltd.), and the results were recorded23.
Time limit for disintegration
A disintegration basket (LB-2B, Shanghai Huanghai Pharmaceutical Testing Instrument Co., Ltd.) was immersed into a 1000-mL beaker, and the position of the basket was adjusted so that when it descended, the screen was 25 mm above the bottom of the beaker. The beaker was filled with water at 37℃ ± 1℃, and the water level was adjusted such that when the basket ascended, the screen was 15 mm below the water surface. Six randomly selected CEP–β-CD inclusion complex oral tablets were placed inside the glass tube of the basket. The disintegration apparatus was activated, and the complete disintegration time for each buccal tablet was recorded23.
In vitro drug release
A PBS solution of pH 6.8 was prepared by mixing 250 mL of 0.2 mol/L potassium dihydrogen phosphate solution with 118 mL of 0.2 mol/L sodium hydroxide solution. Then, the mixture was diluted with deionized water to 1000 mL23.
Simulated artificial saliva of pH 6.824 was prepared by weighing 2.38 g of disodium hydrogen phosphate, 0.19 g of potassium dihydrogen phosphate, and 8 g of sodium chloride and dissolving them in 1000 mL deionized water. Subsequently, the pH was adjusted to 6.8 using phosphoric acid.
Then, 900 mL of pH 6.8 PBS and 900 mL of pH 6.8 simulated artificial saliva were injected into the drug dissolution tester measuring cups (ZRS-8G, Tianjin University Wireless Factory). The temperature was raised to maintain a liquid temperature of 37 °C ± 0.5℃. Three randomly selected CEP–β-CD inclusion complex oral tablets were individually placed into three measuring cups, and the rotating device was activated with the timer started. At 5 min, 10 min, 15 min, 20 min, 30 min, 45 min, 1 h, and 1.5 h, an appropriate amount of the solution was withdrawn from each measuring cup and filtered through a 0.45-µm microporous membrane. The CEP content in the solution at each time point was measured using a UV–Vis spectrophotometer.
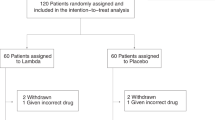
Pharmacokinetic studies in Beagles
Before administering the CEP–β-CD inclusion complex oral tablets, the experimental dogs were fasted for one day but allowed free access to water. A double-dose, double-period, and double-sequence crossover design was adopted for drug administration. During the first period, the dogs in group A were given one CEP–β-CD inclusion complex oral tablet, whereas the dogs in group B received an intravenous injection of 2 mL CEP solution. In the second period, the dogs in group A received an intravenous injection of 2 mL of CEP solution, and the dogs in group B were given one CEP–β-CD inclusion complex oral tablet. (Oral tablets administration: Place the tablets under the beagle’s tongue and immobilize its mouth to prevent it from swallowing the tablets by mistake until they are completely contained.) Following administration, 1 mL blood was collected from the cephalic vein of each dog at 1 min, 5 min, 15 min, 0.5 h, 1 h, 1.5 h, 2 h, 4 h, 6 h, 8 h, 12 h, 24 h, 32 h, and 48 h post-dosing into anticoagulant tubes. The blood samples were centrifuged at 8000 r/min for 10 min to collect the plasma. To each plasma sample, 300 µL of methanol and an internal standard (chidamide at a concentration of 100 ng/mL) were added. The samples were vortexed for 1 min and then centrifuged at 8000 r/min for 10 min. Finally, 200 µL of the supernatant was taken for detection.
The SCIEX Triple Quad 6500 (SCIEX, USA) was used to measure the CEP content in the centrifuged plasma samples, adopting the previously reported in vivo bioanalytical method25. The pharmacokinetic parameters of each beagle were analyzed and calculated using Phoenix 64 (8.2.0.4383) WinNonlin.
Cell viability assay to determine the anti-inflammatory activity of CEP–β-CD inclusion complex oral tablets in vitro
MH-S macrophages were seeded into 96-well plates at a density of 3000 cells per well and incubated for 24 h in a 37 °C, 5% CO2 incubator. The cells were pretreated with varying concentrations of the CEP-β-CD inclusion complex (0.25, 0.5, 2.5, 5, 25, and 50 µg/mL) for 24 h. After incubation, the media in each well was aspirated, and CCK8 solution (MA0218-Jun-15 L, Meilun Biotech, Dalian, China) was added at a volume of 10 µL per well. The plates were allowed to react for 3 h. Subsequently, the absorbance was measured using a microplate reader at 450 nm.
For ELISA, MH-S macrophages were seeded into 96-well plates at a density of 3000 cells per well and incubated for 24 h in a 37 °C incubator with 5% CO2. The cells were pretreated with varying concentrations of the CEP-β-CD inclusion complexes (0.25, 0.5, 1, and 2.5 µg/mL) for 1 h. Subsequently, the cells were either left untreated or stimulated with 100 ng/mL LPS for an additional 24 h. The concentrations of the cytokines TNF-α, IL-6, and IL-1β in the supernatants were determined using a mouse-specific ELISA kit (Biolegend, San Diego, CA, USA) according to the manufacturer’s instructions.
Anti-inflammatory effects of CEP–β-CD inclusion complex oral tablets in mice
Animal experiments
After 3 days of adaptive feeding, the mice were randomly divided into four groups: (1) control group, which received normal feeding with sterile water from days 1 to 3; (2) model group, which received normal feeding with sterile water from days 1 to 3 and was administered with LPS solution (2.5 mg/mL) via intratracheal instillation on day 3 to induce acute pneumonia; (3) gavage group, which received 0.2 mL of CEP-CMC-Na suspension from days 1 to 3, and LPS solution (2.5 mg/mL) was administered via intratracheal instillation to induce acute pneumonia 1.5 h after the last administration on day 3; and (4) oral tablet group, which received 0.5 mg of oral tablet powder from days 1 to 3, followed by two drops of saline solution, and LPS solution (2.5 mg/mL) was administered via intratracheal instillation to induce acute pneumonia1.5 h after the last administration on day 3. Six hours later, mice from each group were euthanized via enucleation, blood was collected in anticoagulant tubes, and lung tissues were dissected for subsequent analysis.
Lung appearance
The collected lung tissues were rinsed thoroughly with saline, dried to remove surface moisture, and then photographed for record.
Histopathologic analysis
The collected lung tissues were fixed in 4% paraformaldehyde for 24 h for histopathological analysis. After dehydration with an alcohol gradient, the lung tissue samples were embedded in paraffin. Tissue sections were stained with hematoxylin and eosin (H&E).
Immunohistochemical staining
Mouse lung tissue sections were dewaxed in xylene for 30 min, followed by dewaxing in 100%, 95%, 80%, and 70% ethanol and ddH2O for 5 min each. Antigen retrieval was performed by immersing the sections in EDTA antigen retrieval buffer (pH 9.0) and incubating in a 3% H2O2 aqueous solution. The retrieved sections were blocked with 3% BSA for 30 min. The primary antibodies, CD45 (diluted 1:4000, Abcam, Cambridge, MA, USA), CD68 (diluted 1:200, Abcam), and Ly6g (diluted 1:1000, Service bio Technology, Wuhan, China), were incubated with the sections overnight at 4 °C. After rinsing with PBS three times, the sections were incubated with the appropriate secondary antibodies. DAB was used as the chromogen, and counterstaining was performed with hematoxylin. Finally, the sections were mounted with neutral resin and observed with an optical microscope.
Inflammatory cytokine detection
The TNF-α, IL-1β, and IL-6 levels in mouse plasma were measured using a mouse-specific ELISA kit (Biolegend) according to the manufacturer’s instructions.
Statistical analysis
GraphPad Prism 8.3.0 software was used for statistical data analysis (one-way ANOVA), and the experimental data are expressed as mean ± SD. A p value of < 0.01 was considered statistically significant.
Results and discussion
Phase solubility diagram
Figure 1 shows the phase solubility diagram of CEP with β-CD. It was observed that β-CD had a good solubilizing effect on CEP, and the CEP concentration in water increased with the concentration of β-CD. This suggests that β-CD forms a soluble inclusion complex with CEP. The calculated stability constant was 909M − 1.
Characteristics of the CEP–β-CD inclusion complex
Surface morphology
SEM is used to determine the surface morphology of substances post interaction, offering an auxiliary method for monitoring the formation of inclusion complexes26. As illustrated in Fig. 2, CEP had a smooth, compact, block-like structure (Fig. 2A). However, β-CD had a rough, loose cavity structure (Fig. 2B). The physical mixture of CEP and β-CD revealed a combination of these forms, characterized by the smooth irregular blocks of CEP and the rough block-like structures of β-CD (Fig. 2C). Notably, the inclusion complex shape was distinct from that of the physical mixture, as the CEP–β-CD inclusion complex presented a novel spherical structure. Thus, the CEP–β-CD inclusion complex was successfully formed27. However, the 2:1 mass ratio group exhibited large blocky materials, and the number of spherical structures was fewer than that of the group with a mass ratio of 1:1. Consequently, a mass ratio of 1:1 for CEP and β-CD was selected for subsequent experiments.
XRD
The formation of solid dispersions as well as any changes in drug crystallinity can be detected by XRD analysis. The crystalline properties of guest molecules change with inclusion complex formation with β-CD28,29. As shown in Fig. 2, due to its crystalline nature, β-CD exhibited a sharp crystalline peak at 12.62° (Fig. 3C), whereas CEP displayed sharp peaks at 11.38°, 15.37°, and 19.08° (Fig. 3D). In the physical mixture of CEP and β-CD, characteristic peaks of both CEP and β-CD were observed (Fig. 3B). In the diffraction pattern of the CEP–β-CD inclusion complex (Fig. 3A), the diffraction peak intensities of CEP and β-CD were significantly reduced, and the overall peak pattern became flatter, indicating an amorphous structure, thereby confirming the inclusion complex formation.
FT-IR
FT-IR analysis, a method for identifying inclusion complex formation, can determine the functional groups present in complexes by identifying the vibrational modes of molecular bonds30. As shown in Fig. 4C, CEP exhibited characteristic absorption peaks at 1370 cm−1, 1360 cm−1, 1222 cm−1, and 1150 cm−1, corresponding to -CH3 bending, C-N stretching vibration, aromatic in-plane deformation, and C-O-C stretching, respectively. The β-CD spectrum displayed a characteristic -OH peak at 3345 cm−1, with C-H stretching vibrations of the cyclic structure observed at 2950 cm−1, and a characteristic C-O-C stretching absorption peak at 1150 cm−1 (Fig. 4D). The physical mixture spectrum of β-CD and CEP revealed a simple superposition of the absorption peaks of CEP and β-CD (Fig. 4A). Notably, absorption peak intensity changes were discernible in the spectrum of the CEP–β-CD inclusion complex. Such spectral alterations are common in CD inclusion complexes and are typically induced by weak intermolecular forces, including ionic bonding, van der Waals forces, electrostatic interactions, and hydrogen bonding31. For example, the intensity of the -OH characteristic peak of β-CD at 3345 cm−1 decreased, and the peak shape broadened (Fig. 4B), which is caused by the participation of -OH in the formation of hydrogen bonds. Meanwhile, the characteristic absorption peaks of CEP at 1370 cm−1, 1360 cm−1, 1222 cm−1 and 1150 cm−1 in Fig. 4B are reduced in intensity, shifted or even disappeared, which may be caused by van der Waals forces and other non-bonding interactions. These results collectively suggest the successful formation of the inclusion complex.
DSC
Thermal analysis is a vital tool to indicate inclusion complex formation32. DSC and thermogravimetry/derivative thermogravimetry (TG/DTG) were used to investigate changes in the physical properties of inclusion complexes with temperature and time. The DSC-TG/DTG results for each sample are depicted in Fig. 5. The TG curve (green) displays thermal degradation profiles, with CEP exhibiting a degradation temperature range of 330–400 °C (Fig. 5A). The TG plot of β-CD revealed two weight loss events: the first at 100 °C, attributed to the evaporation of moisture in the sample, which is favorable for inclusion complex formation, and the second occurring around 300 °C, which corresponded to the primary degradation of β-CD (Fig. 5B); these findings were consistent with those of previous studies33,34. The CEP–β-CD inclusion complex exhibited a degradation temperature range of 290–400 °C (Fig. 5D). As evident from the DTG traces (red), CEP, β-CD, and the CEP–β-CD inclusion complex underwent mass losses at 340 °C, 321 °C, and 338 °C, respectively. Notably, inclusion complex formation resulted in slower CEP degradation, indicating enhanced thermal stability upon encapsulation within β-CD. From the DSC thermal profile (blue), it can be seen that CEP showed a sharp change in the two endothermic peaks at 305 °C and 320 °C; β-CD showed three endothermic peaks changes at 300 °C, 305 °C, and 400 °C, with the latter two changes not being very noticeable; while the CEP–β-CD inclusion complex showed two relatively gradual endothermic peak changes at 308 °C and 318 °C, with the endothermic peak of CEP shifting and becoming less pronounced, and the endothermic peak of β-CD changing, indicating that CEP and β-CD have established some interactions.
Encapsulation rate
In this study, CEP was encapsulated within β-CD, necessitating an encapsulation efficiency assessment to quantify the CEP amount encapsulated in the inclusion complex. The encapsulation efficiency of the CEP–β-CD inclusion complex in this study was 81.45% ± 2.10%, indicating a high encapsulation rate.
Particle size
Table 1 shows the particle sizes of β-CD, CEP, a physical mixture of CEP and β-CD, and the CEP-β-CD inclusion complex. The particle size of the CEP-β-CD inclusion complex is 51.31 ± 0.14 μm, which is smaller than that of the physical mixture of CEP and β-CD, which is also evidence of the successful preparation of the inclusion complex.
Characteristics of CEP–β-CD inclusion complex oral tablets
Tablet weight variation
Twenty randomly selected CEP oral tablets had a total weight of 2.963 g. The average tablet weight was 148.1 mg, whereas the labeled weight per tablet was 150 mg. And the diameter was 7 mm, the thickness was 3.5 mm. These findings comply with the weight variation requirements for tablets specified in the 2020 edition of the Chinese Pharmacopoeia: for tablets with an average or labeled weight < 0.30 g, the weight variation must be within ± 7.5%, translating to an acceptable range of 138.75–161.25 mg for the oral tablets (Fig. 6A).
Friability
For the randomly selected oral tablets, the weight variation of each tablet before and after the friability test was < 1%, meeting the friability requirements for tablets specified in the 2020 edition of the Chinese Pharmacopoeia (Fig. 6B).
Hardness
Five randomly selected CEP oral tablets were individually tested for hardness. All samples met the hardness requirements for tablets outlined in the 2020 edition of the Chinese Pharmacopoeia, with the minimum range typically between 4.5 and 5.5 kg and the maximum range between 9.5 and 10.5 kg (Fig. 6C).
Time limit for disintegration
The disintegration time of six randomly selected CEP oral tablets was tested using a disintegration tester. The disintegration time for all six tablets fell within 10–30 min, complying with the 2020 edition of the Chinese Pharmacopoeia requirements, which specifies that oral tablets should not completely disintegrate or dissolve within 10 min (Fig. 6D).
In vitro drug release
A drug dissolution tester was used to evaluate the drug release profile of the CEP oral tablets in PBS at pH 6.8 and simulated artificial saliva at pH 6.8, and an in vitro drug release curve was plotted (Fig. 7A). As depicted in Fig. 7A, the CEP oral tablets achieved a dissolution rate of > 80% within 30 min, followed by a stable release profile.
Elevated bioavailability in Beagles
A pharmacokinetic study conducted in beagle dogs following intravenous (2 mg/kg) and oral (6 mg/kg) administration of CEP demonstrated that the oral tablets formed with β-CD enhanced the CEP-related pharmacokinetic parameters (Fig. 7B). Based on the intravenous injection parameters, the absolute bioavailability of oral administration was 27.6% (Fig. 7C). Compared with existing research, which has reported an oral bioavailability of 13.15% for CEP in rats25, the bioavailability of the oral tablets was more than doubled.
Due to its poor water solubility and low bioavailability, CEP’s druggability is limited. By forming an inclusion complex with β-CD, its water solubility can be enhanced35, and its inherent bitter taste can be masked36,37. When formulated as an oral tablet, the drug is absorbed through the buccal and sublingual mucosa, avoiding the first-pass effect and thereby improving the bioavailability of CEP.
Safety evaluation by cell viability assay
The EC50 value of the CEP–β-CD inclusion complex, formed after CEP encapsulation with β-CD, was 3.89 ± 0.15 µg/mL. As the concentration increased, the CEP–β-CD inclusion complex significantly inhibited MH-S macrophage growth and proliferation (Fig. 8A). Based on the cell viability assay for the CEP–β-CD inclusion complex, the maximum drug concentration used in subsequent cellular experiments was set to no more than 2.5 µg/mL.
In vitro anti-inflammatory assay of CEP–β-CD inclusion complex
MH-S macrophages were used to evaluate the in vitro anti-inflammatory effects of the CEP–β-CD inclusion complex. Using ELISA, we measured inflammatory cytokine levels in MH-S macrophages exposed to various concentrations of the CEP–β-CD inclusion complex in the presence of LPS. Compared with the LPS-stimulated group, exposure to different concentrations of the CEP–β-CD inclusion complex significantly reduced IL-6, TNF-α, and IL-1β levels (Fig. 8B) in the cell supernatants. The reduction effect gradually increased as the concentration increased, and the most pronounced effect was observed at 2.5 µg/mL. These findings suggest that the CEP–β-CD inclusion complex exerts anti-inflammatory effects by inhibiting proinflammatory factor release from macrophages.
Mechanistic evaluation in cells. (A) Cytotoxicity assessment and cell viability of MH-S cells treated with the CEP–β-CD inclusion complex. (B) CEP–-β-CD inclusion complex inhibits the LPS-induced secretion of inflammatory cytokines. n = 5, \(\bar{\text{x}}+\text{s}\), **** P < 0.0001, *** P < 0.001 vs. the model group.
Anti-inflammatory effect of the CEP–β-CD inclusion complex oral tablets in mice
Lung appearance and histopathologic analysis
The appearance of lung tissue directly reflects the degree of lung damage in mice (Fig. 9A). The lung tissue in the control group exhibited a pink color, smooth surface, soft texture, and no congestion. In contrast, the lungs of mice in the model group appeared dark red with patchy hemorrhagic areas on the surface, indicating successful model establishment. Compared to the model group, both the CEP oral tablet group and the CEP gavage group showed alleviation of lung damage.
HE staining was performed on lung tissue sections from each group to further confirm the ameliorative effects of CEP–β-CD inclusion complex oral tablets on lung inflammation (Fig. 9A). The results revealed that the alveolar structures in the control group were clear and intact, with no apparent abnormal changes. In contrast, the model group exhibited alveolar wall collapse, irregular alveolar dilation, and substantial inflammatory cell infiltration. Compared to the model group, both drug-treated groups showed reduced infiltration of inflammatory cells.
Immunohistochemical analysis
Inflammatory cells, such as neutrophils and macrophages, are crucial for regulating various diseases, including acute and chronic inflammatory conditions38. Immunohistochemical analysis was conducted on inflammatory cell markers in the mouse lungs, including CD45 (a hematopoietic cell marker), CD68 (a macrophage marker), and Ly6G (a neutrophil marker). As shown in Fig. 10A, the model group exhibited increased CD45+, CD68+, and Ly6G + cells in lung tissue, indicating inflammatory cell infiltration and activation. This suggests lung inflammation development following LPS stimulation in mice. In contrast, treatment with CEP oral tablets and CEP by gavage resulted in the alleviation of lung inflammation, with a significant reduction in the number of CD45+, CD68+, and Ly6G + cells compared with that in the model group. In addition, we used Image J software to quantitatively analyze the average optical density of these three positive cell types (Fig. 10B).
Expression of lung inflammatory cell markers. (A) Immunohistochemical staining (20×) of the lung hematopoietic cell marker CD45, the macrophage marker CD68, and the neutrophil marker Ly6G. (B) Average optical density of CD45+, CD68+, and Ly6G + cells in the lungs. n = 5, \(\bar{\text{x}}+\text{s}\); * P < 0.05 vs. the model group.
CEP–β-CD inclusion complex oral tablets exhibit an anti-inflammatory effect
The inflammatory cytokine levels in mouse plasma were monitored using ELISA. As shown in Fig. 9B, the inflammatory cytokine levels in the model group were significantly higher than those in the control group. However, after drug administration, inflammatory factor levels decreased, with the effect of the CEP oral tablets group being slightly superior to that of the intragastric administration group. These results indicate that the CEP–β-CD inclusion complex oral tablets alleviate lung inflammation in mice by inhibiting the proinflammatory factors IL-6, TNF-α, and IL-1β.
Conclusions
CEP has garnered significant attention due to its excellent safety profile and unique pharmacological properties, including anti-inflammatory, antioxidant, immunomodulatory, and antiviral effects. However, the hydrophobic nature of CEP hinders its oral absorption and results in poor bioavailability, thereby limiting its clinical application. In this study, we developed a CEP–β-CD oral tablet using inclusion complex technology to encapsulate CEP with β-CD, followed by the addition of various excipients. This approach not only masks the unpleasant taste of CEP but also enhances its bioavailability. The pharmacokinetic results revealed that the absolute bioavailability of CEP via oral administration reached 27.6%, more than double that of conventional oral administration. Both in vitro and in vivo pharmacodynamic studies demonstrated the robust anti-inflammatory effects of CEP–β-CD oral tablets. These findings suggest that CEP–β-CD oral tablets represent a convenient dosage form with significant scientific implications for preventing and treating lung injuries caused by Long COVID.
Data availability
The data supporting this work are accessible upon reasonable request from the corresponding author.
References
Kiba, Y., Tanikawa, T. & Kitamura, M. Ciclesonide inhibits SARS-CoV-2 Papain-Like protease in vitro. Biol. Pharm. Bull. 47, 965–966 (2024).
Dl, G. How to understand the overlap of long COVID, chronic fatigue syndrome/myalgic encephalomyelitis, fibromyalgia and irritable bowel syndromes. Semin. Arthritis Rheum. 67 (2024).
Montani, D. et al. Post-acute COVID-19 syndrome. Eur. Respiratory Rev. 31, 210185 (2022).
Adjaye-Gbewonyo, D., Vahratian, A., Perrine, C. G. & Bertolli, J. Long COVID in adults: united States, 2022. NCHS Data Brief 1–8 (2023).
Nevalainen, O. P. O. et al. Effect of Remdesivir post hospitalization for COVID-19 infection from the randomized SOLIDARITY Finland trial. Nat. Commun. 13, 6152 (2022).
Ms, D. et al. Association of nirmatrelvir for acute SARS-CoV-2 infection with subsequent long COVID symptoms in an observational cohort study. J. Med. Virol. 96 (2024).
Xie, Y., Choi, T. & Al-Aly, Z. Molnupiravir and risk of post-acute sequelae of covid-19: cohort study. BMJ 381, e074572 (2023).
Xu, W. et al. Cepharanthine synergistically promotes Methylprednisolone pharmacodynamics against human peripheral blood mononuclear cells possibly via regulation of P-glycoprotein/glucocorticoid receptor translocation. BMC Complement. Med. Ther. 24, 186 (2024).
S, K. et al. [Clinical efficacy of Cepharanthin(R)for Radiotherapy-Induced Leukopenia - A nationwide, multicenter, and observational study]. Gan Kagaku Ryoho Cancer Chemother. 43 (2016).
Liu, Z. et al. The genome of Stephania Japonica provides insights into the biosynthesis of cepharanthine. Cell. Rep. 43, 113832 (2024).
J, Z. et al. Cepharanthine attenuates cerebral ischemia/reperfusion injury by reducing NLRP3 inflammasome-induced inflammation and oxidative stress via inhibiting 12/15-LOX signaling. Biomed. Pharmacother. Biomed. Pharmacother. 127 (2020).
Huang, H. et al. Cepharanthine, an alkaloid from Stephania cepharantha Hayata, inhibits the inflammatory response in the RAW264.7 cell and mouse models. Inflammation 37, 235–246 (2014).
Paudel, K. R., Karki, R. & Kim, D. W. Cepharanthine inhibits in vitro VSMC proliferation and migration and vascular inflammatory responses mediated by RAW264.7. Toxicol. Vitro. 34, 16–25 (2016).
Uto, T., Nishi, Y., Toyama, M., Yoshinaga, K. & Baba, M. Inhibitory effect of cepharanthine on dendritic cell activation and function. Int. Immunopharmacol. 11, 1932–1938 (2011).
Deng, Y., Wu, W., Ye, S., Wang, W. & Wang, Z. Determination of cepharanthine in rat plasma by LC-MS/MS and its application to a Pharmacokinetic study. Pharm. Biol. 55, 1775–1779 (2017).
Gao, P. et al. Correction to: Preparation and evaluation of Self-emulsifying drug delivery system (SEDDS) of cepharanthine. AAPS PharmSciTech. 22, 255 (2021).
Feng, W. et al. Direct electrospinning for producing multiple activity nanofibers consisting of aggregated luteolin/hydroxypropyl-gamma-cyclodextrin inclusion complex. Int. J. Biol. Macromol. 270, 132344 (2024).
Carneiro, S. B. et al. Cyclodextrin–Drug inclusion complexes: in vivo and in vitro approaches. Int. J. Mol. Sci. 20, 642 (2019).
Salústio, P. J. et al. Advanced technologies for oral controlled release: cyclodextrins for oral controlled release. AAPS PharmSciTech. 12, 1276 (2011).
Conceicao, J., Adeoye, O., Cabral-Marques, H. M. & Lobo, J. M. S. Cyclodextrins as drug carriers in pharmaceutical technology: the state of the Art. Current Pharm. Design 24, 1405–1433 .
Conceição, J., Adeoye, O., Cabral-Marques, H. M., & Lobo, J. M. S. Cyclodextrins as excipients in tablet formulations. Drug Discov. Today 23 (2018).
Darekar, T. et al. Characterization and in vivo evaluation of lacidipine inclusion complexes with β-cyclodextrin and its derivatives. J. Incl. Phenom. Macrocycl. Chem. 84, 225–235 (2016).
Singh, S. Y., Salwa, Shirodkar, R. K., Verma, R. & Kumar, L. Enhancement in dissolution rate of Atorvastatin trihydrate calcium by formulating its porous tablet using sublimation technique. J. Pharm. Innov. 15, 498–520 (2020).
Topuz, F., Kilic, M. E., Durgun, E. & Szekely, G. Fast-dissolving antibacterial nanofibers of cyclodextrin/antibiotic inclusion complexes for oral drug delivery. J. Colloid Interface Sci. 585, 184–194 (2021).
Li, J. et al. Bioavailability enhancement of cepharanthine via pulmonary administration in rats and its therapeutic potential for pulmonary fibrosis associated with COVID-19 infection. Molecules 27, 2745 (2022).
Ho, S., Thoo, Y. Y., Young, D. J. & Siow, L. F. Inclusion complexation of Catechin by β-cyclodextrins: characterization and storage stability. LWT 86, 555–565 (2017).
Upadhyay, S. K. & Ali, S. M. Molecular recognition of Flunarizine dihydrochloride and β-cyclodextrin inclusion complex by NMR and computational approaches. Chem. Cent. J. 12, 33 (2018).
Suvarna, V., Thorat, S., Nayak, U., Sherje, A. & Murahari, M. Host-guest interaction study of Efavirenz with hydroxypropyl–β–cyclodextrin and l–arginine by computational simulation studies: Preparation and characterization of supramolecular complexes. J. Mol. Liq. 259, 55–64 (2018).
Amiri, S. & Nalbandi, B. Improve solubility and bioavailability of silver sulfadiazine via formation of inclusion complex by cyclodextrin. J. Inorg. Organomet. Polym. 28, 1764–1774 (2018).
Sancho, M. I., Andujar, S., Porasso, R. D. & Enriz, R. D. Theoretical and experimental study of inclusion complexes of β-Cyclodextrins with chalcone and 2’,4’-Dihydroxychalcone. J. Phys. Chem. B 120, 3000–3011 (2016).
Quilaqueo, M. et al. Inclusion of Piperine in β-cyclodextrin complexes improves their bioaccessibility and in vitro antioxidant capacity. Food Hydrocoll. 91, 143–152 (2019).
Galvão, J. G. et al. Lippia gracilis essential oil in β-cyclodextrin inclusion complexes: an environmentally safe formulation to control Aedes aegypti larvae. Pest Manag. Sci. 75, 452–459 (2019).
Cui, H., Zhang, C., Li, C. & Lin, L. Preparation and antibacterial activity of Litsea cubeba essential oil/dandelion polysaccharide nanofiber. Ind. Crops Prod. 140, 111739 (2019).
Wang, Y. et al. β-Cyclodextrin inclusion complex containing Litsea cubeba essential oil: preparation, optimization, physicochemical, and antifungal characterization. Coatings 10, 850 (2020).
Brewster, M. E. & Loftsson, T. Cyclodextrins as pharmaceutical solubilizers. Adv. Drug Deliv Rev. 59, 645–666 (2007).
Lee, C. W. et al. Preparation of bitter taste masked Cetirizine dihydrochloride/β-cyclodextrin inclusion complex by supercritical antisolvent (SAS) process. J. Supercrit. Fluids. 55, 348–357 (2010).
Stojanov, M., Wimmer, R. & Larsen, K. L. Study of the inclusion complexes formed between Cetirizine and α-, β-, and γ-cyclodextrin and evaluation on their taste-masking properties. J. Pharm. Sci. 100, 3177–3185 (2011).
Navegantes, K. C. et al. Immune modulation of some autoimmune diseases: the critical role of macrophages and neutrophils in the innate and adaptive immunity. J. Transl Med. 15, 1–21 (2017).
Acknowledgements
Research in this publication was supported by the Beijing Municipal Natural Science Foundation (No. 20SWAQK22).
Author information
Authors and Affiliations
Contributions
D.L proposed the research concept and design, conducted Data analysis and wrote the preliminary draft; ZH.L was responsible for Data Curation and Investigation; P.H and H.G was responsible for Methodology and the use of software; ZY.M and SC.L supervised the research process and guided the other authors; ZN.W were responsible for the Project Administration; LN.D and GF.D reviewed and edited the manuscript, while RL.G and GF.D acquired the funding. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The animal study protocol was approved by the Institution of Animal Care and Use Committee, Academy of Military Medical Science (IACUC-DWZX-2024-P626, Beijing, China). All animal experiments were complied with the ARRIVE guidelines, and were carried out in accordance with the U.S. Public Health Service Policy on Humane Care and Use of Laboratory Animals.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liang, D., Lv, Z., Meng, Z. et al. Development and evaluation of cepharanthine-β-cyclodextrin inclusion complex oral tablets for prevention and treatment of COVID-19 lung injury. Sci Rep 15, 20989 (2025). https://doi.org/10.1038/s41598-025-04167-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04167-1