Abstract
This study analyzed the prevalence of metabolic syndrome (MetS) among Korean adults aged 19 and older over the past 15 years. A cross-sectional study of data from the Korea National Health and Nutrition Examination Survey (KNHANES) from 2007 to 2022 was conducted. The study included 87,397 subjects. MetS was defined according to the National Cholesterol Education Program-Third Adult Treatment Panel (NCEP-ATP) III and the Korean Society for the Study of Obesity (KOSSO) criteria. MetS prevalence increased from 22.8% in 2007 to 28.6% in 2022 but showed sex differences, with males increasing (24.5% to 36.8%) and females decreasing (20.6% to 19.5%). Among the components of MetS, hyperglycemia and abdominal obesity showed the most significant increases (1.51-fold and 1.29-fold, respectively). While hyperglycemia increased across all age groups in both sexes, abdominal obesity increased most in males aged 30–39 (1.98-fold) and 19–29 (1.81-fold). Low high-density lipoprotein cholesterol (HDL-C) was the only component that decreased (0.62-fold) and was more prevalent among females. In the sub-analysis of those aged 65 and older, MetS increased in both males and females but was more prevalent in females. Individuals with MetS had higher rates of current smoking, heavy drinking, physical inactivity, and carbohydrate consumption. The prevalence of MetS is gradually increasing in Korea, and hyperglycemia and abdominal obesity are rapidly increasing, especially in younger males. Although the prevalence of MetS in females is decreasing due to changes in the social environment, continuous efforts are needed for postmenopausal females. Targeted health policies and interventions should be established.
Similar content being viewed by others
Introduction
Metabolic syndrome (MetS) is a cluster of conditions, including obesity, hypertension, insulin resistance, and dyslipidemia, which significantly increase the risk of chronic diseases such as cardiovascular disease and type 2 diabetes mellitus1. A prospective cohort study involving 11,512 participants found that MetS increased all-cause mortality by 1.4 times in both men and women and increased cardiovascular disease mortality by 2.3 times in men and 2.8 times in women2.
With the spread of the Western lifestyle, MetS has become a global epidemic. Modern sedentary lifestyles, physical inactivity, and high-calorie-low fiber fast food consumption are major factors to MetS3. In the United States, the prevalence of MetS reached 36.9% from 2015 to 2016, increasing with age4. Given the rapidly aging population in South Korea5, intensified efforts to manage MetS are necessary. Effective intervention requires understanding MetS characteristics across different age and sex groups.
Based on the Korea National Health and Nutrition Examination Survey (KNHANES), the prevalence of MetS in South Korea has increased from 24.9% in 1998 to 31.3% in 20076. By 2020, it reached 33.2%, indicating that approximately one in three individuals had MetS7. However, recent studies in Korea lack detailed stratification by sex, age, and behavioral habits and need to be updated. Therefore, in-depth analyses are necessary to understand the effects of societal changes, dietary shifts, and other overlooked factors.
Accordingly, this study not only presents evidence on the recent trend in MetS based on the data from KNHANES from 2007 to 2022 but also provides evidence for sex, age, habits such as smoking, drinking, and physical activity, energy intake, and carbohydrate, protein, and fat intake. The focus was on nutritional factors such as protein and fat intake according to well-defined health behavior definitions8. Therefore, we aimed to provide valuable insights to support the formulation of Korea’s healthcare strategy.
Results
Prevalence of metabolic syndrome from 2007 to 2022
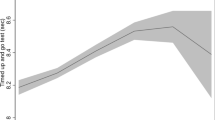
Figure 1 shows the secular trends of MetS and its components from 2007 to 2022. The age-standardized prevalence of MetS in the population increased from 22.8% in 2007 to 28.6% in 2022. Regarding sex-specific changes, the prevalence of MetS in males increased from 24.5% to 36.8%, while in females, it decreased from 20.6% to 19.5%, highlighting a sex disparity.
Secular trends of metabolic syndrome (A) and its components; high waist circumference (B), high blood pressure (C), high glucose (D), high triglyceride (E), and low HDL(high-density lipoprotein) cholesterol (F), between 2007 and 2022. The grey, blue, and orange lines represent the prevalence of total population, male, and female, respectively. Direct standardization was performed based on the 2005 projected population.
Among the components of MetS, high WC and high glucose levels consistently increased. High WC rose from 26.0% in 2007 to 33.6% in 2022, and high glucose from 21.1% to 31.9%. In males, high WC increased from 25.7% to 42.9%, and high glucose from 25.7% to 39.8%. However, in females, high WC fluctuated but recently decreased from 25.9% in 2020 to 23.2% in 2022, while high glucose increased from 16.5% to 23.6% over the study period, indicating sex-specific differences. After decreasing between 2009 and 2014, the prevalence of high BP remained stable, ranging from 29.4% to 33.7%. High TG showed an upward trend, from 30.6% to 34.6%. Although sex disparities existed in high BP and high TG, these differences were less significant compared to other components of MetS. Low HDL-C consistently decreased from 43.4% to 27.2% and was more prevalent among females. The decline was more significant in females, reducing sex disparity, with males showing a higher prevalence by 2022.
Trends in the mean values of each component are shown in Supplementary Table 1. HDL-C levels showed the largest increase over the study period, with a 19.7% rise in the total population (rising 13.4% in males and 25.7% in females).
Prevalence of metabolic syndrome by age and sex
Figure 2 summarizes the prevalence ratios of MetS and its components between 2007 and 2022 by age and sex groups. The prevalence of MetS increased across all age groups, especially in those aged 30–39, followed by the over 70 group (1.36-fold and 1.26-fold, respectively). For females, the prevalence of MetS increased only in those aged 70 and older (1.20-fold), while it decreased in all other age groups.
Prevalence ratios of metabolic syndrome and its components between 2022 and 2007. Each cell represents the prevalence ratio of metabolic syndrome and respective components; high waist circumference, high blood pressure, high glucose, high triglyceride, and low HDL(high-density lipoprotein), for a specific age group and sex in 2022 compared to 2007. The color scale indicates the relative increase (red) or decrease (blue) in prevalence. Maximum prevalence ratio, ratio of 1.00 and minimum prevalence ratio was depicted as red, white and blue, respectively. HDL, high-density lipoprotein.
High WC increased the most in males aged 30–39, with a 1.98-fold increase, followed by males aged 19–29, with a 1.81-fold increase. In the total population, the prevalence of high BP increased only in the over-70 group (1.06-fold). While this increase of hypertension in older adults was observed in both sexes, the age-specific patterns differed slightly. In males, high BP prevalence increased in both the 60–69 (1.02-fold) and ≥ 70 (1.09-fold) age groups, whereas it decreased in all younger age groups. In females, the increase was observed only in the ≥ 70 age group (1.05-fold). High glucose increased in all groups, with the most changes in those aged 19–29 and 30–39 (1.60-fold and 1.55-fold, respectively) in the total population. This pronounced increase in hyperglycemia among younger age groups was observed in both sexes. The prevalence of high TG remained relatively stable in younger adults while increasing 1.48-fold in those aged 70 and older. Low HDL-C levels decreased across all groups except for males aged 70 and older, with the most change observed in younger females.
Figure 3 presents the age-specific prevalence of MetS and its components in 2022. In the total population (Fig. 3-A), among younger adults (aged 19–49), the prevalence of MetS components was highest for high WC, followed by high TG. For those aged over 60, high BP and high glucose had the highest prevalence rates, while high WC was the least prevalent. When analyzed by sex (Fig. 3-B, 3-C), low HDL-C was one of the most prevalent components among females across all age groups. While Fig. 2 illustrates changes between 2007 and 2022, and Fig. 3 focuses on the latest data (2022), Supplementary Table 2 provides specific yearly prevalence rates by sex and age group.
Age-specific prevalence of metabolic syndrome and its components by sex in 2022. Grey lines represent the overall prevalence trend of metabolic syndrome in 2022 across age groups. Components of metabolic syndrome are represented as grouped bar charts for each age group. WC = waist circumference, BP = blood pressure, TG = triglyceride, HDL-C = high-density lipoprotein cholesterol, MetS = metabolic syndrome.
Subgroup analysis of the prevalence of metabolic syndrome in older adults
In the sub-analysis results of those aged 65 and older, the prevalence of MetS increased from 50.2% in 2007 to 62.0% in 2022. It increased from 37.8% to 55.3% in males and 59.2% to 67.4% in females, narrowing the sex disparity from 21.4% to 12.1% in 2007 to 2022, respectively.
High WC decreased from 43.8% in 2007 to 34.7% in 2014 but increased to 48.5% in 2022 while recently reducing since 2022. High BP prevalence increased from 66.5% to 73.1%, with a narrowed sex disparity by 2022. High glucose and high TG steadily increased, from 41.6% in 2007 to 59.9% in 2022 and 40.4% in 2007 to 55.6% in 2022, respectively. High glucose was the only component that was more prevalent in males. Low HDL-C in females decreased over the study period, while that of males increased. (Table 1).
Prevalence of metabolic syndrome according to lifestyle variables
The energy intake percentage from carbohydrates was higher in people with MetS. Total energy intake showed no statistically significant difference between people with and without MetS in the total population. The prevalence of current smoking was higher in the MetS group compared to the non-MetS group (21.0% vs 17.4%, respectively, p < 0.0001). Similarly, heavy drinking was more prevalent in the MetS group (15.8% vs 11.2%, respectively, p < 0.0001). Physical activity was lower in the MetS group compared to the non-MetS group (39.3% vs 50.0%, respectively, p < 0.0001). These trends were more pronounced in males. (Table 2). In the additional analysis by SES, a higher prevalence of MetS in females was observed only among those with elementary education or less and those in the low household income group (Supplementary Table 3).
Discussion
MetS has steadily increased over the past 15 years, especially in males. A notable sex difference in trends was observed in females under 70, which showed a decreasing trend. The increase in MetS was primarily driven by increases in hyperglycemia and abdominal obesity, particularly among younger males. Among the components of MetS, only low HDL-C decreased significantly in younger females. Conversely, MetS were more prevalent in older adults than females, narrowing the sex difference.
The prevalence of MetS increased with age in both males and females. Among individuals aged 70 and older, the prevalence of MetS increased by 13.1% over the study period, resulting in approximately 6.4 out of 10 individuals having MetS in 2022 (Supplementary Table 2). There was a sharp rise in the prevalence among males between the age group 19–29 and 30–39 and among females between the age group 40–49 and 50–59. The difference between sexes implies that social, environmental, and lifestyle changes due to involvement in social activities and marriage are major factors influencing MetS in males, while hormonal changes due to menopause are significant in females9,10.
Contrary to our findings, the analysis of MetS prevalence in the United States from 2011 to 2016 didn’t exhibit a disparity between sex (35.1% for men and 34.3% for women, p = 0.47)4. In China, MetS was much more prevalent in women, likely due to higher rates of abdominal obesity and low HDL-C compared to men11. A study analyzing trends in the prevalence of MetS components in the U.S. from 2007 to 2014 revealed that high WC among women was more prevalent than in men (p < 0.05) and showed a sharp increasing trend (p-trend = 0.009)12. Moreover, in most countries, obesity prevalence and average BMI tend to be higher in males than in females of all ages13. This is believed to stem from the biological differences in female’s fat storage capacity as an adaptation for childbearing10. Therefore, the relatively low abdominal obesity among Korean females is likely to be influenced more by sociocultural factors than biological reasons. (Fig. 1) These factors may include increased female participation in social activities, a higher average age of marriage, lower birth rates, and a social preference for slim females. Furthermore, in South Korea, young women not only possess a heightened awareness of health maintenance but also tend to overestimate their body size, which may be influenced by the prevailing sociocultural preference for a slender physique14.
For older females, factors such as decreased social activities due to changes in employment status and reduced social pressure to maintain a slender physique, in addition to hormonal changes due to menopause, may have played a role, resulting in a distinct pattern among older adults15. These results indicate that while the prevalence of MetS is gradually decreasing in females, there is a critical need for ongoing health management efforts, particularly for postmenopausal females.
Meanwhile, our study’s unique pattern of high WC prevalence highlights the necessity of managing abdominal obesity, particularly in younger males9. Abdominal obesity in young adulthood can contribute to metabolic burden, potentially increasing susceptibility to obesity-related metabolic diseases such as coronary heart disease and diabetes as these individuals age16. Additionally, together with obesity, prediabetes is a key mechanism leading to MetS1. In 2020, the prevalence of prediabetes among Korean adults reached 39.3%, with diabetes mellitus increasing in young adults. However, diabetes management outcomes remained inadequate17. Similar to abdominal obesity, earlier onset of diabetes results in adverse long-term consequences, including complications and quality of life18. Therefore, comprehensive measures targeting weight reduction blood glucose management in young adults should be made to reduce future health burdens at both individual and national levels.
Smoking, heavy alcohol consumption, physical inactivity, and poor dietary choices are well-known unhealthy lifestyle factors. As these are modifiable factors that can reduce the risk of chronic diseases, understanding their epidemics is essential for effective public health management19. The relationship between these unhealthy lifestyle factors and the presence of MetS was more pronounced in males in our study.
This phenomenon could be attributed to two factors. First, females generally have lower smoking rates20 and monthly binge drinking rates21 compared to males, so the impact of these behaviors on MetS may be relatively less significant. Second, females with MetS may have become more health-conscious and adopted healthier lifestyles after diagnosis. It can be inferred that increasing physical activity and addressing smoking and drinking, particularly in males, are important areas of focus. However, the results should be interpreted with caution due to the cross-sectional nature of our study and the lack of quantitative stratification for each behavior. Additionally, the health behavior variables were self-reported, thus being subjective to recall bias and social desirability bias.
Previous studies have shown mixed results regarding sex-specific behavioral effects on MetS. An analysis of Korean adults aged over 20 from 2015 to 2016 found that heavy drinkers (≥ 28.1 g/day) had higher risk of MetS in males, with a 42% increase compared to 18% increase in females. A similar pattern was observed among moderate drinkers (14.1–28.0 g/day), with increasing 25% in males and 7% in females22. In contrast, a study based on 1998 KNHANES found no statistically significant association between alcohol consumption and MetS in either sex. Meanwhile, current smoking was more strongly associated with MetS in females (OR = 1.6) than in males (OR = 1.4)23.
Carbohydrates directly and indirectly influence our metabolic state, affecting conditions such as dyslipidemia and MetS24. According to a study based on the 2008–2011 KNHANES, a high carbohydrate intake was associated with a higher prevalence of MetS in males. In females, a high carbohydrate and low-fat intake was related to a higher prevalence of MetS25. Although carbohydrate consumption decreased by 6.8% between 2001 and 20207, our analysis demonstrated that carbohydrate consumption is still significantly associated with the presence of MetS. This may suggest that diet composition, particularly the proportion of carbohydrates, is more critical than total energy intake.
Our findings regarding SES and MetS in each sex aligns with previous study reporting pronounced association between low SES and MetS among females than in males. Several explanations have been proposed for this sex-specific vulnerability, including promoting differing health behaviors (e.g., smoking, alcohol consumption, physical exercise and dietary pattern) and inequitable social and economic conditions for females26,27. These results may suggest that cultural and structural characteristics of the society should also be taken into consideration when establishing health policy.
According to recent research, MetS can influence neurological complications and disease pathologies not only through behavioral habits but also via alterations in tissue mechanical homeostasis and metabolic pathways28. Therefore, it becomes crucial for future studies to explore the correlation between mechanical signals and metabolic dysfunctions through cellular environment and metabolic regulation.
Given the high internet usage rates among younger populations, digital health interventions based on information and communication technology (ICT) can be efficient health management tools29. Since no single medication for treating MetS exists, lifestyle modifications such as healthy eating habits and weight reduction are crucial therapeutic strategies3. ICT interventions hold strong potential for supporting these lifestyle changes30,31.
Considering prominent increase in hyperglycemia and abdominal obesity among younger males, who tend to have high digital accessibility and engagement, wearable devices linked to smartphones could be used to monitor real-time health indicators (e.g., blood glucose levels, body weight changes, heart rate and step count) and provide personalized exercise plans based on an individual’s activity and metabolic trends. In females, the prevalence of MetS showed a declining trend across all age groups except those aged ≥ 70 years. For younger and middle-aged females, digital health–based self-monitoring tools may be useful in encouraging continuous health management and promoting preventive behaviors. Among older females, such technologies may also serve an educational role of providing information and guidance on managing physiological changes associated with menopause and strategies for healthy aging.
There are some limitations to this study. First, as this is a cross-sectional study, it is difficult to determine whether behavior changes led to a higher prevalence of the condition or if the higher prevalence led individuals to adopt certain habits. Future longitudinal or prospective cohort-based studies may further elaborate the association identified in this study toward a causal interpretation. Second, health behavior data were self-reported, resulting in memory decay bias and recall bias. Moreover, 24-h recall method used to collect dietary data may be influenced by day-to-day variability compared to the Food Frequency Questionnaire (FFQ) method. To mitigate these biases, KNHANES utilizes standardized, structured questionnaires administered by well-trained personnel using face-to-face interviews32. Furthermore, efforts to expand the database, for instance, by linking with the national health insurance data, have been made33. Third, other unmeasured confounders influencing MetS prevalence (e.g., menopausal status, healthcare assessment, social support) may exist, which may be considered in future studies for better understanding of multifactorial nature of MetS. Fourth, only the presence or absence of behavioral habits was reflected; therefore, the effect of degree may not be considered. Similarly, the comparison only involved the average energy intake percentage from each macronutrient between those with and without MetS. The proportion of individuals exceeding the recommended intake was not considered, nor was there a comparative analysis of the nutrient quality or sources34.
Despite these limitations, this study remains significant as it conducted research analyzing nationally representative data, carrying out statistical analyses based on detailed age and sex stratification.
In conclusion, the prevalence of MetS in South Korea has steadily increased over the past 15 years. Fasting hyperglycemia and abdominal obesity have risen rapidly, and health disparity between sexes has been exacerbated. It is crucial to implement lifestyle modifications, including balanced eating habits. This study provides a better understanding of MetS trends. It offers valuable insights for formulating health policies and management strategies for the Korean population and other populations with similar socioeconomic status. Specifically, targeted solutions regarding the characteristics according to age and sex should be established.
Methods
The data analyzed in this study were obtained from the Korea National Health and Nutrition Examination Survey (KNHANES) from 2007 to 2022. The KNHANES is a nationally representative survey provided by the Korea Centers for Disease Control and Prevention (KCDC) for national health promotion, disease prevention, and comparative health data analysis32. The data is publicly accessible from the KCDC website (https://knhanes.kdca.go.kr/). We merged datasets from the years 2007 to 2022, covering the period after KNHANES transitioned to a continuous annual survey. The merging process was conducted using unique participant identifiers and consistent variable definitions provided in the official documentation to ensure standardization across survey years.
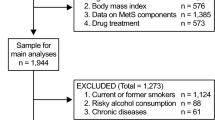
Out of 126,446 subjects from KNHANES (2007–2022), 27,005 individuals under 19 were excluded. Among the remaining 99,441 subjects, 12,044 individuals were excluded due to missing data for defining MetS. Thus, the final study population consisted of 87,397 subjects. Participants missing data on waist circumference, systolic blood pressure (BP), diastolic BP, fasting plasma glucose, triglyceride, or high-density lipoprotein cholesterol (HDL-C) were considered to lack a complete definition of MetS. Complete case analysis was conducted by excluding participants with missing data.
The research protocol was approved by the Institutional Review Boards of the KDCA (2007-02 CON-04-P, 2008-04EXP-01-C, 2009-01 CON-03–2 C, 2010-02 CON-21-C, 2011-02 CON-06-C, 2012-01EXP-01–2 C, 2013-07 CON-03–4 C, 2013-12EXP-035 C, 2018–01–03-P-A, 2018–01–03-C-A, 2018–01–03–2 C-A, 2018–01–03–5 C-A, 2018–01–03–4 C-A). All participants provided written informed consent before participation. Additionally, KNHANES data are publicly accessible and serve as a valuable resource for various epidemiological studies. The principles of the Declaration of Helsinki conducted this study. The study was approved by the Institutional Review Board of the Kyunghee University Hospital (No. 2024–07–021). Informed consent was waived.
This study used the definition provided by the National Cholesterol Education Program-Third Adult Treatment Panel (NCEP-ATP) III, with waist circumference criteria modified according to the cutoffs established by the Korean Society for the Study of Obesity (KOSSO)35,36. Subjects were defined as MetS if they met three or more of the following criteria:
-
1.
Waist circumference (WC) ≥ 90 cm in males or ≥ 85 cm in females
-
2.
BP ≥ 130/85 mmHg or taking antihypertensive drugs
-
3.
Fasting plasma glucose ≥ 100 mg/dL or taking diabetes mellitus drugs
-
4.
Serum Triglyceride (TG) ≥ 150 mg/dL or taking dyslipidemia drugs
-
5.
Serum HDL-C < 40 mg/dL in males, < 50 mg/dL in females, or taking dyslipidemia drugs
Individuals self-reported health behaviors such as smoking, drinking, and physical activity. Each definition is followed by.
Current smoking was defined as those currently smoking and having smoked more than 5 packs (100 cigarettes) throughout their lifetime. Heavy drinking was defined as those who drank more than twice per week and consumed more than 7 glasses of alcohol per occasion for males and 5 glasses for females within the past year. The physical activity group was defined as those who spent more than 150 min on moderate physical activity, 75 min on vigorous physical activity, or an equivalent combination. (vigorous physical activity 1 min = moderate physical activity 2 min)37 Nutritional data was collected using a 24-h dietary recall method. Total energy intake was calculated as the sum of calories consumed daily. The energy intake percentage from each macronutrient was calculated using the following formulas8;
Socioeconomic status (SES) was compared according to self-reported data of educational attainment, household income and region. Educational attainment was stratified to elementary school or less, middle school graduate, high school graduate and college graduate or higher. Household income was assessed through self-reported health surveys. Stratification was based on the variables provided by the KCDC, which categorizes individuals into sex- and age-specific quartiles based on monthly equivalized household income. The equivalized income was calculated as the monthly household income divided by the square root of the household size. Region was classified as urban for administrative areas designated as dong, and rural for areas designated as eup or myeon.
Changes in the age-standardized prevalence of MetS were calculated using direct standardization method based on the 2005 projected population data from the Korean Statistical Information Service (KOSIS) with age groups categorized as 19–29, 30–39, 40–49, 50–59, 60–69, and ≥ 70 years. To assess the potential influence of age and sex on the transition of MetS prevalence, age and sex stratified analysis was performed. Considering the high prevalence of MetS in the elderly, subgroup analysis was additionally conducted for individuals aged 65 and older. Health behavior status, energy intake and SES of each sex were compared according to the presence of MetS.
The primary objective of this study was to examine trends across survey years 2007 to 2011. All analyses incorporated sampling weights, stratification, and clustering to account for the complex survey design, using SAS survey procedures (PROC SURVEYMEANS, PROC SURVEYFREQ, and PROC SURVEYREG) in SAS version 9.4 (SAS Institute Inc., Cary, NC, USA). Categorical variables were presented as percentages with 95% confidence intervals and analyzed using the Rao-Scott chi-square test. Continuous variables were presented as means with 95% confidence intervals and analyzed using the t-test. Statistical significance was defined as p < 0.05.
Data availability
The data are available upon request. The study protocol and statistical code are available from KDH (hkd917@naver.com). The dataset, available from the Korea National Health and Nutrition Examination Survey by the Korea Disease Control and Prevention Agency, can be accessed via the following link (https://knhanes.kdca.go.kr/knhanes/main.do).
References
Grundy, S. M. Pre-diabetes, metabolic syndrome, and cardiovascular risk. J. Am. Coll. Cardiol. 59, 635–643. https://doi.org/10.1016/j.jacc.2011.08.080 (2012).
Hu, G. et al. Prevalence of the metabolic syndrome and its relation to all-cause and cardiovascular mortality in nondiabetic european men and women. Arch. Intern. Med. 164, 1066–1076. https://doi.org/10.1001/archinte.164.10.1066 (2004).
Saklayen, M. G. The global epidemic of the metabolic syndrome. Curr. Hyperten. Rep. 20, 12. https://doi.org/10.1007/s11906-018-0812-z (2018).
Hirode, G. & Wong, R. J. Trends in the prevalence of metabolic syndrome in the United States, 2011–2016. JAMA 323, 2526–2528. https://doi.org/10.1001/jama.2020.4501 (2020).
Statistics Korea. 2023 Statistics on the Aged. 2023. https://kostat.go.kr/board.es?mid=a20101000000&bid=11759&act=view&list_no=427605&tag=&nPage=13&ref_bid=11707,11708,11709,11711,11712,11713,11715,11716,11717,11718,11719,11721,11722,11723,11724,11725,11726,12071,11727,11728,11729,11730,11731,11732,11733,11734,11735,12051,11786,11736,11737,11738,11739,11740,11741,11742,11743,11744,11745,11746,11747,11748,11749,11773,11774,11750,11751,11752,11754,11755,11756,11757,11758,11759,11760,11761,11762,12050,11763,11764,11765,11766,11767,11768,11769,11770,11771,11772&keyField=&keyWord= (2023).
Lim, S. et al. Increasing prevalence of metabolic syndrome in Korea: The Korean national health and nutrition examination survey for 1998–2007. Diabet. Care 34, 1323–1328. https://doi.org/10.2337/dc10-2109 (2011).
Park, D. et al. 20-Year trends in metabolic syndrome among Korean adults from 2001 to 2020. Asia 3(491), 502. https://doi.org/10.1016/j.jacasi.2023.02.007 (2023).
Jung, C. H. et al. Diabetes fact sheets in Korea, 2020: An appraisal of current status. Diabet. Metab. J. 45, 1–10. https://doi.org/10.4093/dmj.2020.0254 (2021).
Jeong, S.-M. et al. 2023 obesity fact sheet: prevalence of obesity and abdominal obesity in adults, adolescents, and children in Korea from 2012 to 2021. JOMES 33, 27–35. https://doi.org/10.7570/jomes24012 (2024).
Mauvais-Jarvis, F. Sex differences in metabolic homeostasis, diabetes, and obesity. Biol. Sex Differ. 6, 14. https://doi.org/10.1186/s13293-015-0033-y (2015).
Gu, D. et al. Prevalence of the metabolic syndrome and overweight among adults in China. Lancet 365, 1398–1405. https://doi.org/10.1016/s0140-6736(05)66375-1 (2005).
Shin, D., Kongpakpaisarn, K. & Bohra, C. Trends in the prevalence of metabolic syndrome and its components in the United States 2007–2014. Int. J. Cardiol. 259, 216–219. https://doi.org/10.1016/j.ijcard.2018.01.139 (2018).
Jaacks, L. M. et al. The obesity transition: Stages of the global epidemic. Lancet Diabet. Endocrinol. 7, 231–240. https://doi.org/10.1016/s2213-8587(19)30026-9 (2019).
Doyeon Kim, Y. K., Hyejin Kim, & Kyungwon, Oh. Attempts to lose weight and related factors according to body mass index among adults in the Republic of Korea, 2013–2021. Pub. Health Wkl. Rep. 17, 1–16. https://doi.org/10.56786/PHWR.2024.17.1.1 (2024).
Rhee, S. Y., Park, S. W., Kim, D. J. & Woo, J. Gender disparity in the secular trends for obesity prevalence in Korea: Analyses based on the KNHANES 1998–2009. Korean J. Intern. Med. 28, 29–34. https://doi.org/10.3904/kjim.2013.28.1.29 (2013).
Reis, J. P. et al. Association between duration of overall and abdominal obesity beginning in young adulthood and coronary artery calcification in middle age. JAMA 310, 280–288. https://doi.org/10.1001/jama.2013.7833 (2013).
Bae, J. H. et al. Diabetes fact sheet in Korea 2021. Diabet. Metab. J. 46, 417–426. https://doi.org/10.4093/dmj.2022.0106 (2022).
Lascar, N. et al. Type 2 diabetes in adolescents and young adults. Lancet Diabet. Endocrinol. 6, 69–80. https://doi.org/10.1016/s2213-8587(17)30186-9 (2018).
Nyberg, S. T. et al. Association of healthy lifestyle with years lived without major chronic diseases. JAMA Intern. Med. 180, 760–768. https://doi.org/10.1001/jamainternmed.2020.0618 (2020).
Korea Disease Control and Prevention Agency. national health and nutrition examination survey, trends in average daily smoking amount of current smokers. https://kosis.kr/statHtml/statHtml.do?orgId=177&tblId=DT_11702_N003&conn_path=I2
Korea Disease Control and Prevention Agency. national health and nutrition examination survey, trends in monthly binge drinking rate. https://kosis.kr/statHtml/statHtml.do?orgId=177&tblId=DT_11702_N234&conn_path=I2
Park, E. J. et al. The effect of alcohol drinking on metabolic syndrome and obesity in Koreans: Big data analysis. Int. J. Environ. Res. Pub. Health https://doi.org/10.3390/ijerph19094949 (2022).
Park, H. S., Oh, S. W., Cho, S. I., Choi, W. H. & Kim, Y. S. The metabolic syndrome and associated lifestyle factors among South Korean adults. Int. J. Epidemiol. 33, 328–336. https://doi.org/10.1093/ije/dyh032 (2004).
Volek, J. S., Fernandez, M. L., Feinman, R. D. & Phinney, S. D. Dietary carbohydrate restriction induces a unique metabolic state positively affecting atherogenic dyslipidemia, fatty acid partitioning, and metabolic syndrome. Prog. Lipid. Res. 47, 307–318. https://doi.org/10.1016/j.plipres.2008.02.003 (2008).
Kwon, Y. J., Lee, H. S. & Lee, J. W. Association of carbohydrate and fat intake with metabolic syndrome. Clin. Nutr. 37, 746–751. https://doi.org/10.1016/j.clnu.2017.06.022 (2018).
Park, S. J. et al. Sex differences in the relationship between socioeconomic status and metabolic syndrome: The Korean national health and nutrition examination survey. Diabet. Res. Clin. Pract. 96, 400–406. https://doi.org/10.1016/j.diabres.2011.12.025 (2012).
Santos, A. C., Ebrahim, S. & Barros, H. Gender, socio-economic status and metabolic syndrome in middle-aged and old adults. BMC Pub. Health 8, 62. https://doi.org/10.1186/1471-2458-8-62 (2008).
Gerardo, H., Oliveira, P. J., Cavadas, C., Grãos, M. & Teixeira, J. The (un)known crosstalk between metabolism and mechanotransduction: Implications for metabolic syndrome (MetS)-associated neurological complications. Biochim. et Biophys. Acta (BBA) – Mol. Basis Dis. 1871, 167678. https://doi.org/10.1016/j.bbadis.2025.167678 (2025).
Rhee, S. Y., Kim, C., Shin, D. W. & Steinhubl, S. R. Present and future of digital health in diabetes and metabolic disease. Diabet. Metab. J. 44, 819–827. https://doi.org/10.4093/dmj.2020.0088 (2020).
Chatterjee, A., Prinz, A., Gerdes, M. & Martinez, S. Digital interventions on healthy lifestyle management: Systematic review. J. Med. Internet. Res. 23, e26931. https://doi.org/10.2196/26931 (2021).
Kim, S., Rhee, S. Y., Lee, S., Obesity, C. o. I. c. T. o. M. S. t. K. S. f. t. S. o. Effectiveness of information and communications technology-based interventions for obesity and metabolic syndrome. JOMES 31, 201–207. https://doi.org/10.7570/jomes22027 (2022).
Kweon, S. et al. Data resource profile: The Korea national health and nutrition examination survey (KNHANES). Int. J. Epidemiol. 43, 69–77. https://doi.org/10.1093/ije/dyt228 (2014).
Oh, K. et al. Korea national health and nutrition examination survey, 20th anniversary: Accomplishments and future directions. Epidemiol. Health 43, e2021025. https://doi.org/10.4178/epih.e2021025 (2021).
Kweon, S. et al. Trends in food and nutrient intake over 20 years: findings from the 1998–2018 Korea national health and nutrition examination survey. Epidemiol. Health 43, e2021027. https://doi.org/10.4178/epih.e2021027 (2021).
Huang, P. L. A comprehensive definition for metabolic syndrome. Dis. Model Mech. 2, 231–237. https://doi.org/10.1242/dmm.001180 (2009).
Lee, S. Y. et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabet. Res. Clin. Pract. 75, 72–80. https://doi.org/10.1016/j.diabres.2006.04.013 (2007).
Bull, F. C. et al. World health organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sport. Med. 54, 1451–1462. https://doi.org/10.1136/bjsports-2020-102955 (2020).
Acknowledgements
This research was supported by the Bio and Medical Technology Development Program of the National Research Foundation (NRF), funded by of Korean government (MIST) (No. RS-2023-00262002). We thank the Korean Society for the Study of Obesity and the Korea Centers for Disease Control and Prevention for their support.
Author information
Authors and Affiliations
Contributions
Study concept and design: SH, RSY, HK, KS; acquisition of data: all authors; analysis and interpretation of data: all authors; drafting of the manuscript: KY, CY and LK-N; critical revision of the manuscript: all authors; statistical analysis: LK-N and HK; and study supervision: SYR and KS.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, Y., Choi, Y., Lee, KN. et al. Disparities in trends of metabolic syndrome in Korea from 2007 to 2022 by age, sex, and lifestyle factors. Sci Rep 15, 21185 (2025). https://doi.org/10.1038/s41598-025-04193-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-04193-z
Keywords
This article is cited by
-
Unveiling sex-specific cardiometabolic and adiposity risk profiles for precision prevention
European Journal of Medical Research (2026)