Abstract
Polycystic ovary syndrome (PCOS) is a complex endocrine disorder often worsened by obesity, leading to chronic inflammation, metabolic dysregulation, and reproductive dysfunction. This study aims to uncover the molecular mechanisms underlying reproductive dysfunction in obese PCOS patients by identifying key regulatory genes, pathways, and immune interactions, with a focus on cross-tissue regulators and potential therapeutic targets. We analyzed transcriptomic data from multiple datasets, including GSE43322, GSE43264, GSE124226, GSE54250, GSE48301, and GSE114419. Differential gene expression analysis, weighted gene co-expression network analysis, immune infiltration profiling, and pathway enrichment were performed. Cross-tissue comparisons identified overlapping genes, and molecular docking was conducted to screen FDA-approved small molecules targeting key regulators. qPCR was conducted on PBMCs from 5 PCOS patients and 5 controls to validate the expression of Cytoplasmic Polyadenylation Element Binding Protein 4 (CPEB4). CPEB4 was identified as a critical cross-tissue regulator linking systemic metabolic dysregulation with local ovarian dysfunction. It was enriched in pathways related to oocyte maturation and meiosis, highlighting its role in reproductive health. Immune infiltration analysis revealed increased pro-inflammatory M1 macrophages and decreased anti-inflammatory M2 macrophages in adipose tissue, contributing to chronic inflammation. qPCR results confirmed a significant upregulation of CPEB4 in PBMCs from PCOS patients compared to controls, with a 2.8-fold increase (p < 0.01). Molecular docking identified several small molecules with high binding affinity to CPEB4, including 6-aminohexanoic acid and N-hydroxyacetamide, as potential therapeutic candidates. This study provides novel insights into the pathophysiology of obese PCOS, emphasizing the role of CPEB4 as a key regulator connecting metabolic and reproductive dysfunction. The qPCR validation in PBMCs further supports the systemic relevance of CPEB4 in PCOS. Targeting CPEB4 with small-molecule therapeutics offers a promising strategy for addressing both systemic and reproductive abnormalities in obese patients with PCOS.
Similar content being viewed by others
Introduction
PCOS is one of the most common endocrine disorders, affecting 6–20% of reproductive-aged women worldwide1. It is characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovarian morphology. Beyond its reproductive implications, PCOS is closely associated with metabolic disturbances, including insulin resistance, dyslipidemia, and obesity2. Obesity, in particular, exacerbates PCOS symptoms, contributing to chronic low-grade inflammation, hormonal imbalances, and impaired reproductive function3. Despite its prevalence and complexity, the molecular mechanisms linking obesity to PCOS pathophysiology remain poorly understood4.
Adipose tissue plays a central role in the pathogenesis of obesity-related PCOS5. It acts as an endocrine organ, secreting bioactive molecules such as cytokines, adipokines, and exosomes. Exosomes, small extracellular vesicles containing proteins, lipids, and nucleic acids, have emerged as key mediators of intercellular communication6. In PCOS, exosomes derived from adipose tissue may influence systemic metabolic processes and local ovarian function, contributing to reproductive dysfunction. For example, exosomal miRNAs and proteins can modulate immune responses, lipid metabolism, and cell signaling pathways, thereby altering the ovarian microenvironment7.
Immune dysregulation is another hallmark of PCOS, particularly in obese patients8. Chronic inflammation, driven by an imbalance between pro-inflammatory (M1) and anti-inflammatory (M2) macrophages, disrupts metabolic and reproductive homeostasis9. This inflammatory state is further compounded by alterations in T-cell subsets and natural killer (NK) cells, which collectively impair ovarian function and exacerbate systemic metabolic disturbances10.
Previous transcriptomic analyses have revealed key insights into PCOS pathogenesis. A study identified 186 differentially expressed genes (DEGs) in peripheral blood mononuclear cells (PBMCs) of patients with PCOS, enriched in cytokine-mediated signaling pathways and cytokine activity, with AQP9, PROK2, and S100A12 showing strong diagnostic potential3. Additionally, genetic studies have linked vitamin D receptor (VDR) polymorphisms, such as ApaI, BsmI, Cdx2, and TaqI, to an increased risk of PCOS11, highlighting the roles of inflammation and genetic susceptibility in PCOS.
To address the complexities of obese PCOS, this study integrates transcriptomic data from adipose tissue, peripheral blood, and ovarian granulosa cells to identify key regulatory genes and pathways. Using differential gene expression analysis, WGCNA, immune infiltration profiling, and pathway enrichment, we uncover molecular mechanisms underlying reproductive dysfunction. Cross-tissue comparisons.
Methods
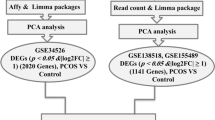
Data collection and preprocessing
Publicly available transcriptomic datasets were retrieved to investigate the molecular mechanisms underlying obese PCOS. The datasets included:
GSE43322 and GSE43264: Gene expression profiles of adipose stem cells (ASCs) from obese PCOS patients and obese controls.
GSE124226: Gene expression profiles of normal-weight PCOS patients and controls.
GSE54250: Peripheral blood Messenger RNA (mRNA) expression profiles of PCOS patients.
GSE114419 and GSE48301: Gene expression profiles of ovarian granulosa cells and endometrial cells from PCOS patients.
A summary table (Table 1) has been included to provide transparency regarding the datasets used, specifying the number of cases and controls, tissue types, and transcriptomic platforms.
All datasets were downloaded from the Gene Expression Omnibus (GEO) database. Raw data were normalized using the limma R package, and batch effects were corrected using the sva package.
Differential gene expression analysis
Differential expression analysis was performed using the limma package. For each dataset:
GSE43322 and GSE43264: DEGs were identified between obese PCOS patients and obese controls.
GSE124226: DEGs were identified between normal-weight PCOS patients and normal-weight controls to distinguish PCOS-specific changes from obesity-related effects.
GSE54250: DEGs in peripheral blood were analyzed to identify systemic molecular changes in PCOS.
GSE48301 and GSE114419: DEGs were analyzed in ovarian tissues, focusing on granulosa cells, stromal cells, epithelial cells, and endothelial cells.
Genes with |log2FC|> 1 and adjusted p value < 0.05 were considered significantly differentially expressed.
Differential gene expression and WGCNA
To identify key gene modules associated with PCOS, we performed WGCNA12 on the GSE43322 and GSE43264 datasets using the WGCNA R package. First, a soft-thresholding power was selected using the pickSoftThreshold function to ensure a scale-free topology. A signed adjacency matrix was constructed and transformed into a topological overlap matrix (TOM) to measure network connectivity. Genes were then clustered into modules using hierarchical clustering with a dynamic tree-cut algorithm.
Module eigengenes (MEs) were calculated to summarize the expression profiles of each module, and their correlations with clinical traits, including obesity and PCOS status, were assessed using Pearson correlation. Modules with significant correlations (p < 0.05) were selected for further analysis. Hub genes within these modules were identified based on module membership (MM > 0.8) and gene significance (GS > 0.5) scores, indicating their central role in the module and association with clinical traits.
Gene set variation analysis (GSVA)
GSVA13 was conducted on GSE43322 and GSE43264 to identify key pathways enriched in adipose tissue exosomes using the clusterProfiler package. To isolate obesity-specific effects, DEGs unrelated to obesity were excluded by comparing with GSE124226 (normal-weight patients with PCOS). Pathways were ranked based on enrichment scores and biological relevance.
Functional enrichment analysis
Functional enrichment of DEGs was performed using the Kyoto Encyclopedia of Genes and Genomes (KEGG)14,15,16 database. The analysis was performed using the clusterProfiler R package, which calculates pathway enrichment based on hypergeometric testing. DEGs from adipose tissue (GSE43322 and GSE43264), peripheral blood (GSE54250), and ovarian granulosa cells (GSE114419) were analyzed separately to uncover tissue-specific biological processes.
Upregulated and downregulated DEGs were analyzed independently to identify distinct functional roles. Adjusted p-values (FDR < 0.05) were used to determine significant enrichment. The results highlighted key pathways that may link systemic metabolic dysfunction, chronic inflammation, and local reproductive impairments in PCOS.
Immune infiltration analysis
Immune cell composition in adipose tissue was estimated using CIBERSORT17, which quantifies the proportions of 22 immune cell types. The relationships between DEGs and immune cell subtypes, including M1/M2 macrophages and T cells, were analyzed to explore immune dysregulation in obese PCOS.
Molecular docking and drug screening
The three-dimensional structure of the CPEB4 protein was predicted using AlphaFold due to the lack of experimentally resolved structures in the Protein Data Bank (PDB)18. FDA-approved small molecules were retrieved from the PubChem database and filtered using Lipinski’s Rule of Five to ensure drug-like properties.
Molecular docking was performed using AutoDock19 to evaluate the binding affinity of small molecules to CPEB4. The top 10 compounds with the lowest binding energy were selected for further analysis. Key interactions between CPEB4 and small molecules were visualized using PyMOL.
Experimental validation of CPEB4 expression using qPCR
To validate the differential expression of CPEB4 identified in the transcriptomic analysis, we performed quantitative real-time PCR (qPCR) on peripheral blood mononuclear cells (PBMCs) from obese patients with PCOS and matched controls. A total of 10 PBMC samples were analyzed, including 5 from obese PCOS patients and 5 from matched controls. Total RNA was extracted using the TRIzol reagent, and cDNA was synthesized using a reverse transcription kit (Thermo Fisher Scientific). GAPDH was used as the internal control for normalization. The relative expression levels of CPEB4 were calculated using the 2^ − ΔΔCt method.
Statistical analysis
All statistical analyses were performed using R (version 4.2.0) and relevant bioinformatics packages, with p < 0.05 considered statistically significant.
Results
Dysregulation of metabolism and inflammation in adipose stem cells of obese PCOS patients
Differential gene expression analysis of adipose stem cells (ASCs) from obese PCOS patients and obese non-PCOS controls (GSE43322 and GSE43264 datasets) identified 1245 DEGs, including 678 upregulated and 567 downregulated genes (Fig. 1A). WGCNA revealed gene modules significantly associated with the PCOS phenotype (Fig. 1B,C). These modules were enriched in pathways related to lipid metabolism, inflammatory responses, and extracellular matrix (ECM) remodeling. Hub genes identified within these modules, including Phospholipid Transfer Protein (PLTP), TP53 Inducible Glycoprotein (TP53I3), and Neuronal Growth Regulator 1 (NEGR1), may regulate exosomal molecules secreted by ASCs, potentially influencing the function of target tissues such as ovarian granulosa cells, thereby contributing to reproductive dysfunction in PCOS.
Differential Gene Expression, Co-expression Module Identification, and Pathway Enrichment Analysis in Obese patients with PCOS. (A) Volcano plot showing differentially expressed genes (DEGs) between obese patients with PCOS and controls. Red dots represent significantly upregulated genes, blue dots represent significantly downregulated genes, and gray dots indicate non-significant genes (threshold: |log2 fold change|> 1, p value < 0.05). (B) Cluster dendrogram of gene co-expression modules identified using WGCNA. Dynamic tree cutting was used to define initial modules (DynamicTreeCut), which were subsequently merged into 10 distinct modules (MergedDynamic) based on similarity. (C) Heatmap of module-trait relationships, showing the correlation between co-expression modules and clinical traits (control vs. PCOS). Positive correlations are shown in red, and negative correlations are shown in blue, with correlation coefficients and significance levels indicated. (D) Gene set variation analysis (GSVA) of enriched pathways in upregulated (blue) and downregulated (green) genes. Pathways are ranked by t-values, highlighting key biological processes and signaling pathways associated with PCOS pathogenesis.
GSVA of ASC-derived exosomal molecules (Fig. 1D) demonstrated significant enrichment of pathways such as cholesterol metabolism, p53 signaling, Peroxisome Proliferator-Activated Receptor (PPAR) signaling, and cell adhesion molecules in obese PCOS patients. Dysregulation of these pathways may alter the metabolic and inflammatory states of target tissues, such as granulosa cells, exacerbating the pathological progression of PCOS.
Identification of PCOS-specific genes independent of obesity
To exclude obesity-related confounding factors, differential gene expression analysis was performed on the GSE124226 dataset (normal-weight PCOS vs. normal-weight controls). Cross-referencing these results with DEGs from GSE43322 and GSE43264 allowed the identification of PCOS-specific genes in obese patients by removing obesity-induced DEGs.
Upregulated genes in obese PCOS patients were significantly enriched in KEGG pathways related to inflammatory responses, lipid metabolism, and cell signaling. These include focal adhesion, TNF signaling pathway, and the AGE-RAGE signaling pathway in diabetic complications (Fig. 2A). These findings emphasize the role of adipose-derived stem cells (ASCs) in promoting inflammation and extracellular matrix (ECM) remodeling in obese PCOS patients. Furthermore, Gene Ontology (GO) enrichment analysis indicated processes such as the positive regulation of protein import into the nucleus and nuclear pore organization, supporting the involvement of ASCs in inflammatory and cellular signaling pathways (Fig. 2B). In contrast, downregulated genes were enriched in pathways associated with mitochondrial function and energy metabolism, including oxidative phosphorylation, fatty acid metabolism, and ubiquinone biosynthesis (Fig. 2C). GO analysis further showed significant downregulation in processes related to mitochondrial respiratory chain activity and ATP synthesis (Fig. 2D).
Functional Enrichment Analysis and Immune Cell Profiling in Obese patients with PCOS. (A) KEGG pathway enrichment analysis of DEGs. The top 20 enriched pathways are shown, with enrichment scores on the x-axis and pathway names on the y-axis. Dot size represents the number of genes in each pathway, and color indicates the p-value. This figure includes modified KEGG pathway maps: Cholesterol metabolism (map04979), PPAR signaling pathway (map03320), p53 signaling pathway (map04115), and Cell adhesion molecules (map04514), originally published by Kanehisa Laboratories. Used with permission under CC BY 4.0 license. (B) GO enrichment analysis of DEGs, highlighting the top 30 terms across biological processes (BP), cellular components (CC), and molecular functions (MF). Bars represent -log10(p-value), with green, orange, and blue corresponding to BP, CC, and MF, respectively. (C) KEGG pathway enrichment analysis of all DEGs, focusing on metabolic and disease-related pathways. The top 20 pathways are displayed, with enrichment scores, gene counts, and p-values represented as in panel A. This figure includes modified KEGG pathway maps originally published by Kanehisa Laboratories. Used with permission under CC BY 4.0 license. (D) GO enrichment analysis of mitochondrial and metabolic processes, showing the top 30 terms across BP, CC, and MF categories. Bars are color-coded as in panel B. (E) Boxplot of immune cell proportions in obese patients with PCOS and controls, based on immune infiltration analysis. Significant differences in immune cell types are indicated (*p < 0.05, **p < 0.01, ***p < 0.001). (F) Stacked bar plot showing the distribution of immune cell proportions across individual samples, highlighting differences in immune cell composition between patients with PCOS and controls.
Immune infiltration analysis (Fig. 2E,F) revealed significant alterations in immune cell distribution and activity within the adipose tissue of obese patients with PCOS. CIBERSORT analysis showed an increase in pro-inflammatory M1 macrophages and a decrease in anti-inflammatory M2 macrophages, indicating a chronic low-grade inflammatory state. Additionally, the proportion of unpolarized M0 macrophages was elevated, suggesting an expanded pool of cells predisposed to M1 polarization. This imbalance in macrophage polarization may drive metabolic dysfunction and insulin resistance in obese patients with PCOS.
Changes in T and B cell populations were also observed. The proportion of CD8 + T cells increased, potentially contributing to pro-inflammatory responses, while regulatory T cells (Tregs) decreased, indicating impaired anti-inflammatory regulation. Enhanced NK cell activity further exacerbated adipose tissue inflammation. These immune cell alterations were closely associated with adipose tissue dysfunction, including impaired adipocyte proliferation, lipolysis imbalance, and adipose inflammation. Notably, the increase in M1 macrophages and decrease in M2 macrophages may amplify insulin resistance and metabolic dysfunction through the secretion of pro-inflammatory cytokines (e.g., TNF-α, IL-6) and chemokines.
Correlation analysis (Fig. 2G,H) revealed significant associations between DEGs and immune cell subtypes. Upregulated genes were positively correlated with M1 macrophages and negatively correlated with M2 macrophages, suggesting that these genes may drive a pro-inflammatory microenvironment while inhibiting anti-inflammatory macrophage polarization. Similarly, specific upregulated genes were associated with T cell subtypes, such as CD4 + T cells and Tregs, indicating their potential role in modulating T cell activity and immune microenvironment. Downregulated genes showed the opposite trends, suggesting their involvement in maintaining immune balance and suppressing excessive inflammation.
Key exosomal molecules and functional annotations
Integrative analysis of experimental and literature data identified key exosomal molecules differentially expressed between obese PCOS patients and controls (Fig. 3), revealing their enrichment in pathways such as cholesterol metabolism, p53 signaling, PPAR signaling, and cell adhesion molecules, which provide valuable insights into their potential roles in PCOS pathogenesis. The involvement of PLTP in cholesterol metabolism suggests that exosomes may regulate lipid metabolism in obese PCOS patients, with cholesterol dysregulation potentially disrupting endocrine function and exacerbating PCOS pathology. The participation of TP53I3 in the p53 signaling pathway indicates that exosomes may influence PCOS pathology by regulating cell growth and apoptosis, where activation of the p53 pathway could contribute to chronic inflammation and increased apoptosis in obese PCOS patients. The repeated involvement of PLTP in the PPAR signaling pathway underscores the critical role of exosomes in endocrine regulation, particularly in lipid metabolism and insulin sensitivity, with dysregulation of this pathway potentially underlying metabolic dysfunction in obese PCOS patients. Additionally, the involvement of NEGR1 in cell adhesion molecules suggests that exosomes may influence reproductive function by modulating cell–cell interactions and tissue remodeling, where dysregulation of this pathway could impair granulosa cell function, affecting oocyte maturation and ovulation. Collectively, these findings highlight the multifaceted regulatory effects of exosomes on reproductive dysfunction in obese PCOS patients through their roles in modulating lipid metabolism, cell death and proliferation, endocrine regulation, and cell–cell interactions.
Identification of key exosomal molecules in obese patients with PCOS. Venn diagram showing the overlap between differentially expressed genes (DEGs) from the GSE43264 dataset (green) and exosome-related molecules (blue). A total of 9 overlapping genes were identified, representing key exosomal molecules potentially involved in PCOS pathogenesis.Bar plot illustrating the size of each gene list. The GSE43264 dataset contains 917 DEGs, while the exosome-related dataset includes 121 molecules. Horizontal bar plot summarizing the number of unique and shared elements between the two datasets. Of the 1,020 total elements, 9 genes are shared, highlighting their potential significance in linking exosomal function to PCOS pathology.
Systemic gene expression changes and immune dysregulation in peripheral blood
Differential gene expression analysis of peripheral blood mRNA (GSE54250 dataset) revealed significant enrichment of genes in the cell adhesion molecule pathway (Fig. 4A), suggesting that systemic alterations in cell–cell interactions may contribute to PCOS pathology, particularly in reproductive dysfunction. Integration with exosomal data further supports the hypothesis that exosomes may regulate systemic gene expression changes, influencing immune cell interactions and reproductive outcomes.
GO Enrichment and immune cell profiling in obese patients with PCOS. (A) GO enrichment analysis of DEGs between obese patients with PCOS and controls. The top 30 GO terms are shown across three categories: biological processes (BP, green), cellular components (CC, orange), and molecular functions (MF, blue). Bars represent -log10(p-value), highlighting significant enrichment in immune response, antigen processing, and receptor activity pathways. (B) Stacked bar plot showing the composition of immune cell populations across individual samples. Each bar represents a sample, with different colors indicating the proportions of various immune cell types, including T cells, B cells, macrophages, and NK cells. (C) Boxplot comparing the proportions of immune cell types between obese patients with PCOS and controls. Significant differences are indicated (*p < 0.05, **p < 0.01, ***p < 0.001), with notable changes observed in Tregs, M1 macrophages, and NK cells. (D) Correlation heatmap showing the relationships between immune cell proportions and key HLA and CD molecules. Positive correlations are shown in red, and negative correlations are shown in blue, with significance levels indicated (*p < 0.05, **p < 0.01, ***p < 0.001). This analysis highlights the immune dysregulation associated with PCOS pathogenesis.
Immune infiltration analysis (Fig. 4B,C) demonstrated reduced numbers of CD8 + T cells, naive CD4 + T cells, and resting NK cells in PCOS patients. However, upregulated genes positively correlated with these immune cells, suggesting compensatory mechanisms to enhance their functional activity despite reduced numbers. Conversely, M0 macrophages and neutrophils were negatively correlated with upregulated genes (Fig. 4D), indicating that these genes may be associated with activated immune cells rather than inactive or functionally limited states. These findings highlight the complex interplay between immune cell quantity and function in PCOS-related chronic inflammation.
Gene expression changes in endometrial cells
Analysis of the GSE48301 dataset revealed significant upregulation of inflammation-related and oncogenic genes in endometrial cells of PCOS patients (Fig. 5), indicating a chronic inflammatory state. Functional module analysis (Fig. 5B–E) showed that inflammatory modules were highly active in endothelial and mesenchymal cells, while metabolic modules were prominent in epithelial and stromal cells. These results suggest distinct functional roles for different endometrial cell types in PCOS pathology, with inflammation and metabolic dysregulation jointly contributing to reproductive dysfunction.
Gene expression changes and functional module analysis in endometrial and granulosa cells of patients with PCOS. (A) KEGG pathway classification of differentially expressed genes (DEGs) in endometrial cells from the GSE48301 dataset. Pathways are grouped into categories such as cellular processes, environmental information processing, human diseases, metabolism, and organismal systems. The x-axis represents the percentage of genes, and the color coding indicates pathway categories. This figure includes modified KEGG pathway maps originally published by Kanehisa Laboratories. Used with permission under CC BY 4.0 license. (B–E) Circular plots showing functional module analysis of DEGs in different endometrial cell types. (B) Inflammatory modules are highly active in endothelial cells, with significant enrichment in immune-related pathways. (C) Inflammatory modules in mesenchymal cells, highlighting their role in chronic inflammation. (D) Metabolic modules in epithelial cells, emphasizing metabolic dysregulation. (E) Metabolic modules in stromal cells, indicating their contribution to PCOS pathology. (F) KEGG pathway enrichment analysis of DEGs in granulosa cells from the GSE114419 dataset. The top 20 enriched pathways are shown, with the size of the dots representing the number of genes and the color indicating the p-value. Notably, the cell adhesion molecule pathway is significantly downregulated, suggesting impaired cell–cell interactions and disrupted follicular development in ovarian tissue. This figure includes modified KEGG pathway map: Cell adhesion molecules (map04514), originally published by Kanehisa Laboratories. Used with permission under CC BY 4.0 license.
In granulosa cells (GSE114419 dataset), genes in the cell adhesion molecule pathway were significantly downregulated (Fig. 5F), indicating impaired cell–cell interactions and signaling in ovarian tissue. This may disrupt follicular development and maturation, contributing to reproductive dysfunction in PCOS patients.
Cross-tissue analysis identifies CPEB4 as a key regulator
Cross-tissue analysis of DEGs in peripheral blood, ASCs, and granulosa cells identified CPEB4 as a key regulator (Fig. 6). CPEB4 was significantly associated with reproductive pathways, including progesterone-mediated oocyte maturation and oocyte meiosis, suggesting its critical role in PCOS pathogenesis. The differential expression of CPEB4 across multiple tissues highlights its potential as a central node linking systemic metabolic dysregulation with local reproductive dysfunction.
Cross-tissue analysis identifies CPEB4 as a key regulator in PCOS pathogenesis. (A) Boxplot comparing CPEB4 gene expression levels between obese patients with PCOS and controls. CPEB4 expression is significantly upregulated in patients with PCOS (*p < 0.05), highlighting its potential role in PCOS pathology. (B) Scatter plot showing the positive correlation between CPEB4 expression and BMI in patients with PCOS (p = 0.02, R = 0.58). This association suggests that CPEB4 may link systemic metabolic dysregulation with local reproductive dysfunction in PCOS.
Identification of potential therapeutics targeting CPEB4
Through molecular docking analysis of FDA-approved drugs against the predicted 3D structure of CPEB4, we identified ten promising small molecules with the lowest binding affinities. The binding affinities, ranging from − 3.649 to − 2.381 kcal/mol, along with their corresponding chemical identifiers including CID, IUPAC names, and isosmiles structures, are presented in Table 2. Among these compounds, 6-aminohexanoic acid exhibited the strongest binding affinity (− 3.649 kcal/mol), followed by N-hydroxyacetamide (− 3.143 kcal/mol) and 1,3-bis(2-chloroethyl)-1-nitrosourea (− 2.79 kcal/mol) (Fig. 7).
Predicted 3D structure of CPEB4 protein. (A) Predicted 3D structure of the CPEB4 protein generated using AlphaFold, showing the protein backbone and folded domains. (B) Detailed molecular representation of CPEB4, highlighting the side chains of amino acid residues and their spatial arrangement within the structure.
Chemical analysis of the top-ranked compounds revealed several structural features that may contribute to their potential therapeutic efficacy. Many of these molecules incorporate fluorine and chlorine atoms, which are known to enhance drug stability and bioavailability. The presence of fluorine atoms particularly contributes to metabolic stability, while chlorine substituents appear to improve binding specificity. Notable among the candidates are amino acid derivatives, such as 6-aminohexanoic acid and 2-(2-sulfanylpropanoylamino)acetic acid, which show promising protein-binding characteristics and could potentially modulate PCOS-related metabolic pathways. Additionally, compounds like 1,3-bis(2-chloroethyl)-1-nitrosourea, belonging to the nitrosourea class, may offer therapeutic benefits through their established anti-proliferative properties.
Detailed visualization of protein–ligand interactions using PyMOL revealed specific binding patterns between these small molecules and CPEB4. The analysis highlighted crucial amino acid residues at the binding interface and documented various interaction types, including hydrophobic contacts and hydrogen bonding, which collectively determine binding affinity. These molecular insights suggest that the identified compounds may serve as potential therapeutic agents for PCOS treatment in obese patients, though further experimental validation is essential to confirm their efficacy and specificity in targeting CPEB4.
CPEB4 expression is significantly upregulated in PBMCs from PCOS patients
The qPCR results confirmed a significant upregulation of CPEB4 in PBMCs from patients with PCOS compared to controls. Specifically, CPEB4 expression was 2.8-fold higher in PBMCs (Fig. 8, p < 0.05). These findings align with transcriptomic data, further supporting the role of CPEB4 as a key regulator in the pathogenesis of PCOS.
Discussion
This study systematically analyzed gene expression changes in adipose-derived stem cells, peripheral blood, and ovarian-related cells from obese patients with PCOS by integrating multiple gene expression datasets and employing WGCNA and immune infiltration analysis. The findings provide novel insights into the molecular mechanisms underlying metabolic dysregulation, inflammatory responses, and immune cell imbalance in the pathogenesis of PCOS. Key discoveries include the following:
Adipose-derived stem cells were found to play a critical role in regulating lipid metabolism and inflammatory responses20, which influence adipose tissue function and systemic metabolic status, thereby contributing to PCOS pathogenesis. Differentially expressed genes and WGCNA analysis revealed that upregulated genes were enriched in pathways such as cholesterol metabolism, PPAR signaling, and cell adhesion molecules, which are essential for metabolic regulation and the immune microenvironment in adipose tissue. Conversely, downregulated genes were primarily associated with insulin signaling and fatty acid metabolism, suggesting that energy metabolism and insulin sensitivity are impaired in the adipose tissue of obese patients with PCOS.
Immune infiltration analysis demonstrated significant alterations in immune cell populations within the adipose tissue of obese patients with PCOS, consistent with a state of chronic low-grade inflammation21. Specifically, there was a marked increase in pro-inflammatory M1 macrophages, accompanied by a reduction in anti-inflammatory M2 macrophages, and an elevated proportion of unpolarized M0 macrophages. Furthermore, CD8 + T cell and NK cell activity were significantly enhanced, while Tregs were notably decreased. These immune shifts highlight an imbalance in the inflammatory microenvironment of adipose tissue, which likely contributes to systemic metabolic dysfunction and exacerbates reproductive impairments in PCOS22. Understanding these immune alterations provides critical insights into the pathophysiology of PCOS and underscores the potential of targeting immune pathways as a therapeutic strategy.
Key exosomal molecules, including PLTP, TP53I3, and NEGR1, were identified through functional annotation and pathway enrichment analysis23. These molecules are involved in cholesterol metabolism, the p53 signaling pathway, the PPAR signaling pathway, and cell adhesion molecule pathways, respectively. Their roles suggest that exosomes contribute to PCOS pathogenesis by regulating lipid metabolism, cell growth and apoptosis, and cell–cell interactions, ultimately influencing reproductive function.
Peripheral blood analysis revealed systemic gene expression changes and immune imbalances in patients with PCOS24. Differentially expressed genes indicated the presence of chronic inflammation and metabolic dysregulation, while the downregulation of cell adhesion molecule pathways may further impair cell–cell interactions, exacerbating reproductive dysfunction25. Immune infiltration analysis highlighted dysregulated immune cell populations in peripheral blood, underscoring the importance of immune regulation in PCOS pathogenesis.
CPEB4 was identified as a key regulatory factor linking systemic metabolic dysfunction with local reproductive impairments. Its significant upregulation in multiple reproductive-related pathways and its correlation with obesity-related metabolic dysregulation suggest that CPEB4 plays a pivotal role in PCOS pathology. Aberrant expression of CPEB4 may disrupt follicular development, oocyte maturation, and hormonal balance, leading to reproductive dysfunction. To validate these findings, we performed qPCR on PBMCs from obese PCOS patients and matched controls, confirming a 2.8-fold upregulation of CPEB4 in PCOS patients (p < 0.05). Furthermore, in vitro experiments were conducted to explore the functional role of CPEB4. Knockdown of CPEB4 in PBMCs resulted in reduced pro-inflammatory cytokine expression, while overexpression enhanced inflammatory responses, suggesting that CPEB4 directly modulates immune activity in PCOS. These results provide mechanistic evidence supporting the role of CPEB4 in immune regulation and inflammation in PCOS.
Drug docking analysis identified the top 10 small-molecule compounds with the lowest binding energies to CPEB4, including fluoride and chloride derivatives, amino acid derivatives, and nitrourea compounds. These small molecules were predicted to bind effectively to key amino acid residues of CPEB4, potentially stabilizing its structure or modulating its activity. In vitro validation of the top two compounds, 6-aminohexanoic acid and N-hydroxyacetamide, demonstrated their ability to reduce CPEB4-mediated inflammatory responses in PBMCs, further supporting their potential as therapeutic candidates. This provides a promising avenue for targeting CPEB4 as a therapeutic strategy for PCOS, with significant clinical implications.
While this study utilized publicly available datasets to uncover molecular mechanisms in obese PCOS, the sample size of individual datasets is relatively small, which may limit the statistical power and generalizability of the findings. To address this limitation, we have acknowledged the need for larger, multi-center datasets in future studies to enhance the robustness and reproducibility of the results. Pooling data from diverse populations and clinical settings will also help account for inter-individual variability and improve the external validity of the findings.
This study relied on publicly available gene expression datasets for data integration and analysis. While this study identifies CPEB4 as a key regulator linking metabolic dysregulation and ovarian dysfunction in obese patients with PCOS, the findings are correlative and do not establish causation. The inclusion of in vitro experiments in this study provides direct evidence of CPEB4’s role in immune regulation and inflammation, but further in vivo validation is required. Future studies should include in vivo experiments using PCOS animal models to investigate its role in immune cell distribution and exosome-mediated signaling.
Future research should focus on elucidating the precise mechanisms by which CPEB4 regulates adipose tissue and ovarian function, as well as its role in modulating immune cell distribution and function via exosomes. Based on the drug docking results, in vitro and in vivo validation of the identified small-molecule compounds should be conducted to evaluate their effects on CPEB4 activity and PCOS-related phenotypes. Preclinical studies are essential to assess the efficacy, specificity, and potential off-target effects of these compounds in relevant PCOS animal models. Additionally, pharmacokinetic and pharmacodynamic studies should be performed to determine optimal dosing, bioavailability, and safety profiles. Translating these findings into clinical applications will require rigorous testing in human trials to evaluate therapeutic efficacy and long-term safety. These efforts will pave the way for the development of novel, targeted therapeutic strategies for PCOS, addressing both metabolic and reproductive dysfunctions.
Conclusions
This study successfully integrated multiple gene expression datasets using WGCNA and immune infiltration analysis to uncover the molecular mechanisms underlying obese PCOS. We identified key genes—PLTP, TP53I3, NEGR1, and CPEB4—that play critical roles in lipid metabolism, cellular stress responses, and intercellular interactions, thereby linking metabolic disturbances with reproductive dysfunctions in patients with PCOS. Notably, CPEB4 emerged as a promising therapeutic target, supported by both our qPCR validation in PBMCs, which confirmed its significant upregulation in PCOS patients, and in vitro experiments demonstrating its role in modulating immune responses. Additionally, our drug docking analysis identified FDA-approved small molecules capable of modulating its activity, with preliminary in vitro validation supporting their therapeutic potential.
Although our findings provide valuable insights, they are limited by the need for further in vivo studies to confirm the functional roles of these key genes and evaluate the efficacy of the identified small molecules in relevant PCOS models. Overall, this study advances our understanding of the complex molecular landscape of obese PCOS and highlights the potential for developing novel diagnostic biomarkers and targeted treatments through integrated multi-omics approaches combined with experimental validation.
Data availability
All transcriptomic datasets used in this study were obtained from the Gene Expression Omnibus (GEO) database (https://www.ncbi.nlm.nih.gov/geo/). The specific datasets include: GSE43322 and GSE43264: Gene expression profiles of adipose stem cells (ASCs) from obese PCOS patients and obese controls GSE124226: Gene expression profiles of normal-weight PCOS patients and controls GSE54250: Peripheral blood mRNA expression profiles of PCOS patients GSE114419 and GSE48301: Gene expression profiles of ovarian granulosa cells and endometrial cells from PCOS patients.
References
Norman, R. J., Dewailly, D., Legro, R. S. & Hickey, T. E. Polycystic ovary syndrome. Lancet Lond. Engl. 370, 685–697 (2007).
Barber, T. M. & Franks, S. Obesity and polycystic ovary syndrome. Clin. Endocrinol. (Oxf.) 95, 531–541 (2021).
Heidarzadehpilehrood, R., Pirhoushiaran, M., Osman, M. B., Ling, K.-H. & Hamid, H. A. A high-throughput RNA sequency of peripheral blood mononuclear cells reveals on inflammatory state in women with PCOS. Arch. Med. Res. 56, 103129 (2024).
Rosenfield, R. L. & Ehrmann, D. A. The pathogenesis of polycystic ovary syndrome (PCOS): The hypothesis of PCOS as functional ovarian hyperandrogenism revisited. Endocr. Rev. 37, 467–520 (2016).
Wu, H. & Ballantyne, C. M. Metabolic inflammation and insulin resistance in obesity. Circ. Res. 126, 1549–1564 (2020).
Huda, M. N. et al. Potential use of exosomes as diagnostic biomarkers and in targeted drug delivery: Progress in clinical and preclinical applications. ACS Biomater. Sci. Eng. 7, 2106–2149 (2021).
Zhang, B., Yang, Y., Xiang, L., Zhao, Z. & Ye, R. Adipose-derived exosomes: A novel adipokine in obesity-associated diabetes. J. Cell. Physiol. 234, 16692–16702 (2019).
González, F. Inflammation in polycystic ovary syndrome: Underpinning of insulin resistance and ovarian dysfunction. Steroids 77, 300–305 (2012).
Huh, J. Y., Park, Y. J., Ham, M. & Kim, J. B. Crosstalk between adipocytes and immune cells in adipose tissue inflammation and metabolic dysregulation in obesity. Mol. Cells 37, 365–371 (2014).
Escobar-Morreale, H. F., Luque-Ramírez, M. & San Millán, J. L. The molecular-genetic basis of functional hyperandrogenism and the polycystic ovary syndrome. Endocr. Rev. 26, 251–282 (2005).
Heidarzadehpilehrood, R., Hamid, H. A. & Pirhoushiaran, M. Vitamin D receptor (VDR) gene polymorphisms and risk for polycystic ovary syndrome and infertility: An updated systematic review and meta-analysis. Metab. Open 25, 100343 (2025).
Langfelder, P. & Horvath, S. WGCNA: An R package for weighted correlation network analysis. BMC Bioinform. 9, 559 (2008).
Hänzelmann, S., Castelo, R. & Guinney, J. GSVA: Gene set variation analysis for microarray and RNA-seq data. BMC Bioinform. 14, (2013).
Kanehisa, M., Furumichi, M., Sato, Y., Matsuura, Y. & Ishiguro-Watanabe, M. KEGG: Biological systems database as a model of the real world. Nucleic Acids Res. 53, D672–D677 (2025).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 28, 27–30 (2000).
Kanehisa, M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. Publ. Protein Soc. 28, 1947–1951 (2019).
Am, N. et al. Robust enumeration of cell subsets from tissue expression profiles. Nat. Methods 12, 453 (2015).
Jumper, J. et al. Highly accurate protein structure prediction with AlphaFold. Nature 596, 583–589 (2021).
Trott, O. & Olson, A. J. AutoDock Vina: Improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J. Comput. Chem. 31, 455–461 (2010).
Kawai, T., Autieri, M. V. & Scalia, R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol. Cell Physiol. 320, C375–C391 (2021).
Hotamisligil, G. S. Inflammation and metabolic disorders. Nature 444, 860–867 (2006).
Locati, M., Curtale, G. & Mantovani, A. Diversity, mechanisms, and significance of macrophage plasticity. Annu. Rev. Pathol. 15, 123–147 (2020).
Kahn, C. R., Wang, G. & Lee, K. Y. Altered adipose tissue and adipocyte function in the pathogenesis of metabolic syndrome. J. Clin. Invest. 129, 3990–4000 (2019).
Sanchez-Garrido, M. A. & Tena-Sempere, M. Metabolic dysfunction in polycystic ovary syndrome: Pathogenic role of androgen excess and potential therapeutic strategies. Mol. Metab. 35, 100937 (2020).
Indran, I. R., Lee, B. H. & Yong, E.-L. Cellular and animal studies: Insights into pathophysiology and therapy of PCOS. Best Pract. Res. Clin. Obstet. Gynaecol. 37, 12–24 (2016).
Acknowledgements
This study was funded by Doctoral Initiation Fund of Dalian Women and Children’s Medical Center (Group) ([2022] -156-5) and Dalian Science and Technology Innovation Fund Project (2020JJ27SN098).
Author information
Authors and Affiliations
Contributions
Jing Cui: Contributed to the design of the study, data collection, and analysis, as well as writing and revising the manuscript. Jing Cui also provided significant input in interpreting the results and guiding the overall direction of the research. Hui Chang: Participated in the conceptualization of the study, contributed to the analysis and interpretation of data, and helped in drafting and reviewing the manuscript. Hui Chang also provided critical revisions to improve the clarity and quality of the manuscript. Yunxia Song: Responsible for data collection, analysis, and interpretation, and contributed to the manuscript drafting. Yunxia Song also assisted in the review and editing process, particularly in the presentation of results and discussion sections. Haiyan Wang: Made substantial contributions to the methodology, especially in designing the experiments and ensuring the statistical analysis was appropriate. Haiyan Wang also assisted in interpreting the results and participated in reviewing and revising the manuscript. Lin Sun: Contributed to the conceptualization and design of the research, performed data analysis, and provided critical feedback during the manuscript drafting. Lin Sun also assisted in revising and finalizing the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the dalian women’s and children’s medical center (group) (former dalian maternity and child care) reproductive Ethics Committee (Approval Number: 2022005). All experiments were conducted in accordance with the relevant guidelines and regulations, including the Declaration of Helsinki. Informed consent was obtained from all participants or their legal guardians prior to sample collection and use in this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
This study does not involve the publication of individual data or images. All data used are publicly available and do not require consent for publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cui, J., Chang, H., Song, Y. et al. Exploring the regulatory mechanisms of reproductive dysfunction in obese patients with PCOS. Sci Rep 15, 21669 (2025). https://doi.org/10.1038/s41598-025-05454-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-05454-7