Abstract
To investigate the diagnostic value of diagonal earlobe crease (DELC) combined with lipoprotein(a) [Lp(a)] for coronary heart disease (CHD). A total of 862 chest paint patients suspected of CHD were admitted to Chengde Central Hospital between September 2021 and December 2023. According to CAG results, patients were categorized into the experimental group and the control group. Multifactorial logistic analysis was used to analyze association between DELC and Lp(a) levels with the risk of developing CHD. The diagnostic efficacy of DELC, Lp(a) for CHD was evaluated by receiver operating characteristic (ROC) and area under the curve (AUC). The results showed that DELC and Lp(a) were positively correlated with CHD. Age, sex, hypertension, diabetes mellitus, alopecia, DELC, TG and Lp(a) were independent risk factors for CHD. The CHD diagnostic model was constructed based on these risk factors, with the Hosmer-Lemeshow test (P = 0.683) confirming a good fit. The subjects were categorized into group A, B, C, and D, taking group A as the reference group, and the OR values of groups C and D were significantly increased after multi-factor correction. The area under the DELC and Lp(a) curves calculated by ROC curve was 0.729, indicating a strong diagnostic value for CHD. DELC and Lp(a) were independent risk factors for CHD. The combination of DELC and Lp(a) had good application value in the diagnosis of CHD.
Similar content being viewed by others
Introduction
Coronary Heart Disease (CHD) is a kind of heart disease caused by the narrowing or blockage of the lumen due to atherosclerosis of the coronary artery, resulting in myocardial ischemia, hypoxia and even necrosis1. CHD is the most common organ lesion caused by atherosclerosis. In recent years, the incidence trend is younger, and it has become one of the major diseases threatening human health2. It is important to investigate the factors that predict the occurrence of CHD for the diagnosis and treatment of CHD. Some non-invasive examinations, such as electrocardiogram and cardiac ultrasound, have a positive diagnosis accuracy of 41% for CHD3. Invasive examinations like coronary angiography (CAG), which is the “gold standard” for the diagnosis of CHD. However, CAG is expensive, complex, and potentially problematic. Therefore, they are not suitable for use as a screening tool for the diagnosis of CHD. Consequently, there is a need for a non-invasive, simple, and user-friendly technique for diagnosing CHD.
The diagonal earlobe crease (DELC), which is intuitive and simple to recognize in clinical practice, has been frequently confirmed to increase the risk of CHD in recent years. In 1973, Frank reported the phenomenon of the earlobe crease for the first time in the New England Journal of Medicine and named it the DELC. It was also the first time that Frank found a correlation between DELC and CHD4. An autopsy conducted in 2021 on a retrospective study of CHD patients revealed a substantial correlation between coronary atherosclerosis and the existence of an earlobe crease5. Kaukola et al. also found that the positive rate of DELC in the CHD group was 72%, while that in the group without CHD was only 21% (P < 0.001), indicating that DELC was related to CHD, and the positive rate of DELC increased with the increase of age and severity of CHD6.
In addition, Lipoprotein (a) [LP(a)] is an independent lipoprotein that is mainly regulated by inherited genes7,8. recent years, Lp(a) has become a new risk factor in the field of cardiovascular disease. It is crucial to the initiation and progression of atherosclerosis. In a meta-analysis of Mendelian randomization published in 2024, a relationship between Lp(a) levels and CHD was demonstrated9. A meta-analysis conducted in 2008 revealed a correlation between Lp(a) and CHD (OR: 1.60, 95%CI 1.38–1.85) and that the risk of CHD grew progressively as Lp(a) levels rose10. The LPAKIV-2/rs10455872 risk genotype, which corresponds to the Lp(a) level, was found to greatly enhance the prediction risk of CHD in a Mendelian randomization tria11. According to a genome-wide association study, there is a substantial correlation between two LPA variants of Lp (a) and an elevated risk of CHD12. Mendelian randomization, meta-analyses, and genome-wide association studies had demonstrated the link between Lp(a) and cardiovascular disease.
DELC has been identified as a significant contributor to the development of atherosclerosis13. Given the established correlation between atherosclerosis and dyslipidemia, we postulated that DELC might also be associated with dyslipidemia. Although the veracity of this relationship remains to be substantiated, subsequent studies are anticipated to provide further elucidation. Furthermore, DELC has been shown to have two major advantages: first, it is easily identifiable; and second, it is highly stable. When combined with the recently discovered lipid marker Lp(a), it is expected to provide a new perspective and expand the diagnostic tools available for the diagnosis of CHD. The objective of the present study was to determine whether both DELC and Lp(a) are independent risk factors for CHD and whether the diagnostic value of the combination of the two for CHD is superior to the diagnostic value of each factor alone.
Subjects and methods
General information
The present study was a single-center cross-sectional study. A total of 862 chest pain patients suspected of CHD were admitted to Chengde Central Hospital between September 2021 and December 2023. According to the result of coronary angiography (CAG), patients diagnosed with CHD serve as the experimental group (CHD, n = 606), and patients diagnosed with non-CHD were taken as the control group (non-CHD, n = 256). This retrospective study was approved by the Ethics Committee of the Chengde Medical University. The research in Chinese clinical trial registry http://www.chictr.org.cn, registration number: ChiCTR2000041499. All participating subjects were fully aware of the trial and signed informed consent. All methods in this study were performed in accordance with the relevant guidelines and regulations and the Declaration of Helsinki.
Inclusion criteria and exclusion criteria
Inclusion criteria: (1) Individuals over the age of eighteen who reported tightness and had chest pain, suspected of CHD, and agreed to undergo selective CAG were selected. (2) The above patients agreed to participate in the experiment and signed informed consent. (3) The clinical data of the above patients were complete.
Exclusion criteria: (1) Previous history of acute myocardial infarction and CHD was well diagnosed; (2) Prior myocardial reperfusion therapy, such as thrombolytic therapy, percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG); (3) The patient has other heart conditions(such as congenital heart disease, valvular heart disease or great vascular disease); (4) The patient has CAG contraindications (such as severe cardiopulmonary, hepatic and renal insufficiency, iodine contrast agent drug allergy, electrolyte disturbance and severe arrhythmia); (5)The patient has earrings or a pierced ear or ear injury.
Clinical data collection
Baseline information adopted: (1) Demographic characteristics: Age, sex, height, weight, body mass index (BMI) = Weight (kg)/ Height (m2) (kg/m2); (2) Previous history: smoking, drinking, hypertension, diabetes mellitus, cerebral infarction, hypertriglyceridemia, hypercholesterolemia, hyperuricemia, family history of diabetes, family history of CHD; (3) Vital signs: premature gray hair, alopecia, heart rate, systolic blood pressure (SBP), diastolic blood pressure (DBP), diagonal earlobe crease (DELC); (4) First laboratory indicators after admission(All patients fasted for more than 12 h. 5mL blood was drawn from elbow vein the next morning): uric acid (UA), lactate lehydrogenase (LDH), glucose (Glu), triglyceride (TG), total cholesterol (TC), high density lipoprotein (HDL-C), low density lipoprotein (LDL-C), cystatin C, (CysC), lipoprotein (a) [(Lp(a)]; (5) Echocardiography: left ventricular ejection fraction (LVEF), ECG ST-T changes.
CHD diagnosis methods
CHD definition: CAG results show that at least one major coronary artery or its branches have an internal diameter stenosis of ≥ 50%14. CAG is performed by experienced cardiovascular physicians. The CAG results are evaluated by two experienced interventional physicians who are independent and have no conflict of interest in the study, and are decided in consultation with the third physician in dispute.
Definition of indicators
The 2017 guidelines defined hypertension as individuals who have not taken antihypertensive drugs, measured the blood pressure of the brachial artery of the upper arm while sitting at rest, measured the blood pressure of SBP ≥ 140mmHg and (or) DBP ≥ 90mmHg for three times on different days, or have been clearly diagnosed with hypertension and (or) have received antihypertensive treatment15. The classification and diagnosis of diabetes considered that diabetes mellitus are not taken oral glucose-lowering drugs, fasting blood glucose measurement or greater tendency for 7.0 mmol/L, random blood glucose level equal to or exceeding 11.1 mmol/L, oral glucose tolerance test (OGTT) oral glucose tolerance level equal to or exceeding 11.1 mmol / L, or those who have been prescribed and/or been treated with antihypoglycemic drugs16.
DELC and Lp(a)
-
(1)
The DELC is a continuous fold that runs diagonally from the tragus to the back edge of the earlobe at an angle of about 45° and covers more than two-thirds of the total earlobe17. The earlobe fold is observed when the patients are sitting or lying flat under a natural light source. The length > 2/3 of the total earlobe is identified as DELC, otherwise, it is excluded. The positive rate of DELC in two groups is observed. (Fig. 1)
-
(2)
All patients fasted for more than 12 h. 5mL of blood was taken from the elbow vein the next morning. The first post-admission laboratory examination was collected, and Lp(a) levels were recorded in both groups. If there were outliers or extremes in the Lp(a) level, a recheck was performed. Lp(a) level ≥ 30-50 mg/dl was taken as the threshold range for atherosclerotic thrombosis18. The diagnostic efficiency of Lp(a) for CHD was analyzed.
Sample size calculation
The sample size was calculated based on the area under the ROC curve for the model, with all computations performed using R software, version 4.4.1. The risk model demonstrated an AUC of 0.729 for predicting CHD in this study, with a test power (1-β) of 0.9 and a significance level (α) set at 0.05. The ratio of non-CHD to CHD in this study was 1:3. The results indicated that at least 181 patients were needed in the non-CHD group and at least 543 patients in the CHD group. Considering a sample failure rate of 10%, a total of at least 797 cases was necessary for this study.
Statistical analysis
In this study, Statistical analyses in the present study were conducted using SPSS software version 27.0 (IBM Corporation, Armonk, NY, USA), while graphical representations were constructed utilizing R software version 4.4.1 and GraphPad Prism 8.0. The measurement data are tested by Shapiro Wilk for normal distribution. The measurement data conforming to a normal distribution are expressed as mean ± standard deviation (x̄ ± S), and an independent sample t test is used. The non-normal measurement data are expressed as M(Q1, Q2) and the Mann-Whitney U test is adopted. The statistical data are expressed as a rate (%) and a Chi-square (χ2) test is used, with P < 0.05 indicating a statistical difference. The variance inflation factor (VIF) is calculated to test the multicollinearity between the influencing factors. Logistic regression is used to analyze the influencing factors, and the OR and 95% CI are calculated. In univariate logistic regression analysis, P < 0.05 is used as the screening criterion, which is incorporated into the multivariate regression model, and the covariables age, sex, smoking, hypertension, diabetes mellitus, alopecia, TG, and HDL-C are included for correction. Adjusted OR and 95% CI are calculated to analyze the diagnostic effect of the DELC combined Lp(a) level on CHD. The results were visualized through map of forest, which provide an intuitive and user-friendly interface to represent the model’s performance metrics. We conducted a stratified analysis based on DELC = 0 and DELC = 1, using Lp(a) levels [Lp(a) ≤ 20.59 mg/dl = 0, Lp(a) > 20.59 mg/dl = 1] as the dependent variable for logistic regression analysis. The study subjects were categorized into four groups: Group A [DELC = 0, Lp(a) ≤ 20.59 mg/dl], Group B [DELC = 0, Lp(a) > 20.59 mg/dl], Group C [DELC = 1, Lp(a) ≤ 20.59 mg/dl], and Group D [DELC = 1, Lp(a) > 20.59 mg/dl]. Differences between groups were compared. We performed subgroup analyses based on age, sex, hypertension, diabetes mellitus, and smoking status to assess whether these factors influence the relationship between DELC, Lp(a), and CHD. An interaction with a P-value less than 0.05 was deemed statistically significant. The diagnostic efficacy of DELC and Lp(a) for CHD was evaluated by receiver operating characteristic (ROC) and area under the curve (AUC).
Results
Baseline data of patients in the CHD group and non-CHD group
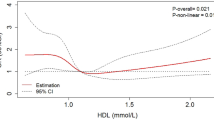
Baseline data of the two groups showed statistically significant differences in age, sex, smoking, premature gray hair, alopecia, hypertension, diabetes mellitus, cerebral infarction, hypercholesterolemia, SBP, Glu, HDL-C, CysC, and ST-T between the CHD group and the non-CHD group (P < 0.05). There were no significant differences in other indexes (P > 0.05). Compared to the non-CHD, which had 128 cases (50.00%), the CHD group had 474 cases (78.20%) with a higher positive rate of DELC [(χ2 = 68.029, P < 0.001)]. The Lp(a) level in CHD patients was significantly higher than that in non-CHD patients, and the difference was statistically significant (P < 0.05). (Table 1; Fig. 2)
Note: BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; DELC, diagonal earlobe crease; UA, uric acid; LDH, lactate lehydrogenase; Glu, glucose; TG, Triglycerides; TC, Total cholesterol; Lp(a), Lipoprotein (a); HDL-C, High density lipoprotein cholesterol; LDL-C, Low density lipoprotein cholesterol; Cys-C, Cystatin C; LVEF, left ventricular ejection fraction.
Baseline data of DELC and non-DELC in CHD group
According to the presence or absence of DELC, the patients with CHD were categorized into the DELC group (n = 474) and the non-DELC group (n = 132). The results showed that patients in the DELC group were older than those without DELC (58.63 ± 8.66 VS. 62.34 ± 8.14, P = 0.000) and more male than those in the non-DELC group (44.70 VS. 60.30, P = 0.001, P = 0.001). Alopecia, Hb, LDH, and CysC were higher than those without DELC, and the differences were statistically significant (P < 0.05). (Table 2)
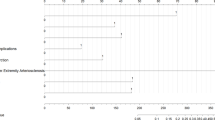
Multivariate logistic regression analysis of the factors affecting the diagnosis of CHD
With the presence of CHD as the dependent variable and age, sex, smoking, hypertension, diabetes mellitus, alopecia, TG, and HDL-C as the independent variables, multivariate logistic regression analysis was performed. The results showed that age, sex, hypertension, diabetes mellitus, alopecia, DELC, and Lp(a) were all independent risk factors for CHD (P < 0.05). (Table 3; Fig. 3).
Forest plots for multivariate regression analysis of CHD.  P < 0.05, the difference was statistically significant;
P < 0.05, the difference was statistically significant;  P > 0.05, the difference was not statistically significant. Lines represent 95% confidence intervals (95%CI) and dots represent odds ratios (OR). DELC, diagonal earlobe crease; TG, Triglycerides; Lp(a), Lipoprotein (a); HDL-C, High density lipoprotein cholesterol.
P > 0.05, the difference was not statistically significant. Lines represent 95% confidence intervals (95%CI) and dots represent odds ratios (OR). DELC, diagonal earlobe crease; TG, Triglycerides; Lp(a), Lipoprotein (a); HDL-C, High density lipoprotein cholesterol.
The influence of DELC combined with Lp(a) on CHD was analyzed by multi-factor logistic regression
With the presence of CHD as the dependent variable, age, sex, smoking, hypertension, diabetes mellitus, alopecia, TG, and HDL-C as the independent variables, multivariate logistic regression analysis was performed. The results showed that DELC combined with Lp(a) was a risk factor for CHD after adjusting for age, sex, smoking, hypertension, diabetes mellitus, alopecia, TG, and HDL-C. Compared with the effect of DELC and Lp(a) on CHD alone, DELC combined with Lp(a) had a greater effect on CHD (P = 0.000). (Table 4)
CHD layered analysis
Stratified analysis was conducted with DELC = 0 and DELC = 1, with CHD status (CHD = 0 as the control group and CHD = 1 as the test group) as the dependent variable. According to the ROC curve, the optimal cut-off value of the Lp(a) level was calculated as 20.59 mg/dl. Lp(a) levels (Lp(a) ≤ 20.59 mg/dl = 0, Lp(a) > 20.59 mg/dl = 1) were utilized as the dependent variable for logistic regression analysis. Results indicated no correlation between Lp(a) level and CHD when DELC = 0 (P > 0.05). However, when DELC = 1, after adjusting for age, sex, smoking, hypertension, diabetes mellitus, alopecia, TG, and HDL-C, the difference was statistically significant (P = 0.000), and Lp(a) was independently correlated with CHD. The subjects were divided into group A [DELC = 0, Lp(a) ≤ 20.59 mg/ml], group B [DELC = 0, Lp(a) > 20.59 mg/ml], group C [DELC = 1, Lp(a) ≤ 20.59 mg/ml], group D [DELC = 1, Lp(a) > 20.59 mg/ml], taking group A as the reference group, whose OR value was 1. After adjusting for age, sex, smoking, hypertension, diabetes mellitus, alopecia, TG, and HDL-C, the OR values of groups C and D were significantly increased (P = 0.000, OR = 2.493, 95%CI 1.593–3.901; P = 0.000, OR = 4.056, 95%CI 2.538–6.482), with a significant statistical difference. (Table 5).
Subgroup analysis
Subgroup analysis was undertaken based on age (< 65 years or ≥ 65 years), sex, hypertension, diabetes mellitus, and smoking, with interaction effects assessed using P-values. The results indicated no significant interaction between the aforementioned variables. This suggests that DELC and Lp(a) are independently associated with the risk of CHD, and this association remains relatively consistent across different subgroups (P for interaction > 0.05). (Fig. 4)
Diagnostic role of DELC and Lp(a) in CHD
CHD is the dependent variable, with DELC and Lp(a) as the independent variables. The area under the curve (AUC) for diagnosing CHD by DELC is 0.641 [(AUC1 = 0.641), (95%CI 1.825–3.620)], and the AUC for diagnosing CHD by Lp(a) is 0.549 [(AUC2 = 0.549), (95%CI 1.145–2.191)]. The AUC of the combined diagnosis of CHD by DELC and Lp(a) is 0.729 [(AUC3 = 0.729), (95%CI 0.692–0.766)]. The VIF of each independent risk factor is less than 10, and there is no multicollinearity. The model Hosmer-Lemeshow test (P = 0.683) suggests that the model fits well. The results indicate that the combined diagnostic value of DELC and Lp(a) is better than that of a single diagnosis. (Fig. 5)
An ROC analysis with respect to the detection of CHD. AUC, Area under the curve; ROC, Receiver operating characteristic. The purple line (AUC2) indicates the area under the curve of DELC; The green line (AUC3) represents the area under the curve of Lp(a). The red line (AUC1) represents the area under the curve for DELC combined with Lp(a).
Discussion
CHD can be classified into chronic coronary diseases and acute coronary syndromes according to its pathogenesis and treatment principles. Chronic coronary diseases include stable angina pectoris, ischemic cardiomyopathy and occult CHD. Acute coronary syndromes include unstable angina pectoris, non-ST elevation myocardial infarction and ST elevation myocardial infarction19. CHD is characterized by a prolonged disease course, sudden onset, urgent change, which seriously threatens human health. Previous studies have identified DELC and Lp(a) as risk factors for CHD12,13, but there is no international study on the diagnosis of CHD in conjunction with DELC and Lp(a). This study aims to investigate the diagnostic effect of DELC and LP(a) on CHD.
DELC is defined as a continuous fold that runs diagonally from the tragus to the back edge of the earlobe at an Angle of about 45°and covers more than 2/3 of the total earlobe length17. The earlobe receives blood supply from both the anterior auricular branch of the superficial temporal artery and the posterior auricular artery. When CHD occurs, the arteries became atheromatous, the lumen became occluded, the blood supply of the earlobe was reduced, the elasticity was reduced, and folds appear. Atherosclerosis can lead to the lack of subdermal matrix, and the earlobe is rich in subdermal matrix. Therefore, when patients with CHD occur, the earlobe is deficient in subdermal matrix, weakened elasticity, and folded18,19. There are also other mechanisms for DELC, such as skin aging, collagen degeneration, or telomere shortening20. Recent pathological studies have shown that myocardial morphological changes are significantly correlated with the existence of earlobe folding, accompanied by changes such as arterial myoelastic fibrosis, Waller-like degeneration of peripheral nerves and fibrosis of the deep tissue at the base of folds21. In a study by Kamal R et al., which selected 200 patients and showed that out of 100 cases, 76 had DELC and 24 did not, whereas out of 100 controls, 36 had DELC and 64 did not (P < 0.001, OR = 5.63, 95% CI 2.91–10.93), and the proportion of DELC in the experimental group was significantly higher than that of the control group, indicating a significant association between DELC and CHD17. Furthermore, Kwae-pingsuenl et al. found that for every 1% increase in the incidence of left-sided DELC, the risk of CHD increased by 1.017 times in a logistic regression model involving 100 subjects22. In this study, multivariate logistic analysis showed that the positive rate of DELC in CHD group was significantly higher than control group, with a 2.57 times higher risk of CHD associated with DELC (OR = 2.570, 95%CI 1.825–3.620, P = 0.000).
Lp(a) is a low-density lipoprotein (LDL)-like particle composed of the large glycoprotein molecules apolipoprotein (a) and apolipoprotein B100 covalently linked by disulfide bonds6. Lp(a) is heterogeneous in size and density. The size of Apo(a) is also heterogeneous. Studies have shown that there is a significant amino acid sequence homology between apolipoprotein (a) and plasminase. Plasminogen enters the fibrinolytic system after being activated by a plasminogen activator, where it may have pre-thrombotic and anti-fibrinolytic effects23. Therefore, Lp(a) also shows homology and may facilitate atherosclerosis and thrombosis24. Lp(a) can impact the function of smooth muscle cells and endothelial cells, thereby influencing vascular homeostasis and promoting atherosclerosis25. Lp(a) contains a variety of unsaturated fatty acids, which is prone to oxidative modification and facilitates the formation of foam cells26,27. It can also accelerate the adhesion and aggregation of inflammatory cells to the blood vessel wall, impede fibrinogen activation, and hinder fibrin formation, thereby increasing local cholesterol accumulation and promoting coronary atherosclerosis18. Lp(a) is an important determinant of cardiovascular risk. For each combination of cardiovascular risk factors, elevated Lp(a) levels further increase the risk of future events28. Individual differences in serum Lp(a) concentrations are significant, and Lp(a) levels in the general population can range from less than 1 mg/dl to more than 1000 mg/dl29. In the 2018 American Heart Association guideline recommendations, the Lp(a) threshold risk value is > 50 mg/dl30, but the risk of CHD increases when it is higher than 30 mg/dl29. In this study of China, Lp(a) levels were significantly higher in patients with CHD compared to those without CHD. For each 1 mg/dl increasing in Lp(a), the risk of CHD increased 1.584 times (OR = 1.584, 95%CI :1.145–2.191, P = 0.005). ROC curve analysis showed that the risk of CHD was increased when Lp(a) > 20.59 mg/dl in populations of China. Therefore, reducing Lp(a) concentration is critical, but studies on statins and Lp(a) are inconclusive. Proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors have been shown to reduce Lp(a) and LDL-C levels. An analysis of ODYSSEY Outcomes trials involving patients with recent acute coronary syndromes showed that PCSK9 inhibitors successfully reduced Lp(a) levels and this reduction was independently associated with a subsequent reduction in major adverse cardiac events (MACE)31. In the future, we can detect serum Lp(a) levels in healthy people, and regular detection can play an important role in early prevention and exclusion of potential cardiovascular diseases.
This study demonstrates that the combination of DELC and Lp(a) holds significant diagnostic value for CHD. Initially, the findings substantiated that both DELC and Lp(a) function as autonomous risk factors for CHD. Secondly, after correcting for potential confounders such as age, sex, hypertension, diabetes, smoking history, hair loss, TG, and HDL-C, both DELC and Lp(a) were found to be significantly and positively associated with the risk of CHD (P < 0.05). A stratified analysis revealed that individuals with both DELC and Lp(a) ≥ 20.59 mg/dl exhibited a 4.056-fold elevated risk of CHD compared to those without DELC (OR = 4.056, 95% CI 2.538–6.482). Subgroup analyses revealed no statistically significant interactions between the distinct clinical subgroups (by age, sex, hypertension, diabetes, smoking status) (P value for interaction > 0.05). Consequently, subject ROC analysis demonstrated that the AUC of DELC in combination with Lp(a) for the diagnosis of CHD reached 0.729, suggesting that DELC possesses satisfactory diagnostic efficacy. Consequently, this study offers substantial evidence supporting the utilization of DELC with Lp(a) in the clinical diagnosis of CHD.
This study has several limitations: (1) Single-center design and sample limitations: This investigation was conducted at a single center, and the sample’s representativeness may be constrained by geographic factors. Future studies should incorporate external datasets to further validate the predictive efficacy of this model. (2) Potential diagnostic bias: The DELC status was determined through manual identification, which may introduce diagnostic bias. (3) This cross-sectional study has controlled for confounders, including age, sex, hypertension, diabetes, and smoking. However, it is possible that other uncontrolled confounders may exist.
Conclusions
Both DELC and Lp(a) are positively correlated with CHD. Furthermore, the combined assessment of DELC and Lp(a) demonstrates substantial diagnostic value for CHD. This finding enhances the ability of primary care physicians to play a more proactive role in clinical practice, enabling early diagnosis and treatment, reducing the risk of missed diagnoses, and ultimately improving the clinical diagnostic rate for CHD patients.
Data availability
The datasets generated during and/or analysed during the current study are not publicly available due to privacy reasons, but are available from the corresponding author on reasonable request.
References
Knuuti, J. et al. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur. Heart J. 41, 407–477 (2020).
GBD 2019 Chronic Respiratory Diseases Collaborators. Global burden of chronic respiratory diseases and risk factors, 1990–2019: An update from the global burden of disease study 2019. EClinicalMedicine 59, 101936 (2023).
Patel, M. R. et al. Low diagnostic yield of elective coronary angiography. N Engl. J. Med. 362, 886–895 (2010).
Frank, S. T. Aural sign of coronary-artery disease. N. Engl. J. Med. 289, 327–328 (1973).
French, C. E. V., Rutherford, J. D., Goossens, L. & Tiemensma, M. The relationship between earlobe creases and the presence, extent, and severity of coronary artery atherosclerosis: A regional Population-Based autopsy study. Am. J. Forensic. Med. Pathol. 42, 155–159 (2021).
Agouridis, A. P., Elisaf, M. S., Nair, D. R. & Mikhailidis, D. P. Ear lobe crease: a marker of coronary artery disease? Archives Med. Science: AMS 11, 1145–1155 (2015).
Bosco, G., Mszar, R., Piro, S., Sabouret, P. & Gallo, A. Cardiovascular risk estimation and stratification among individuals with hypercholesterolemia. Curr. Atheroscler. Rep. 26, 537–548 (2024).
Zhang, J., Jia, L., Yang, Y., Xiao, A. & Lin, X. Lipoprotein (a) and myocardial infarction: Impact on long-term mortality. Lipids Health Dis. 22, 70 (2023).
Yang, R. et al. Causal association between lipoproteins and risk of coronary artery disease-a systematic review and meta-analysis of Mendelian randomization studies. Clin. Res. Cardiology: Official J. German Cardiac Soc. https://doi.org/10.1007/s00392-024-02420-7 (2024).
Bennet, A. et al. Lipoprotein(a) levels and risk of future coronary heart disease: Large-scale prospective data. Arch. Intern. Med. 168, 598–608 (2008).
Kamstrup, P. R., Tybjærg-Hansen, A. & Nordestgaard, B. G. Extreme lipoprotein(a) levels and improved cardiovascular risk prediction. J. Am. Coll. Cardiol. 61, 1146–1156 (2013).
Clarke, R. et al. Genetic variants associated with Lp(a) lipoprotein level and coronary disease. N. Engl. J. Med. 361, 2518–2528 (2009).
Prangenberg, J., Doberentz, E., Johann, L. & Madea, B. The prognostic value of the Frank sign. Forensic Sci. Med. Pathol. 18, 149–155 (2022).
Xu, B. et al. Angiographic quantitative flow ratio-guided coronary intervention (FAVOR III China): A multicentre, randomised, sham-controlled trial. Lancet (London England) 398, 2149–2159 (2021).
Whelton, P. K. et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 71, 1269–1324 (2018).
American Diabetes Association. 2. Classification and diagnosis of diabetes: Standards of medical care in diabetes-2018. Diabetes Care 41, S13–S27 (2018).
Kamal, R. et al. Diagonal earlobe crease as a significant marker for coronary artery disease: A case-control study. Cureus 9, e1013 (2017).
Enas, E. A., Varkey, B., Dharmarajan, T. S., Pare, G. & Bahl, V. K. Lipoprotein(a): An independent, genetic, and causal factor for cardiovascular disease and acute myocardial infarction. Indian Heart J. 71, 99–112 (2019).
Gakovic, B. et al. The relationship of diagonal earlobe crease (Frank’s sign) and obstructive coronary artery disease in patients undergoing coronary angiography. Wien. Klin. Wochenschr. 135, 667–673 (2023).
Stoyanov, G. S., Dzhenkov, D., Petkova, L., Sapundzhiev, N. & Georgiev, S. The histological basis of frank’s sign. Head Neck Pathol. 15, 402–407 (2021).
Bazoukis, G., Papadatos, S. S., Varrias, D. & Tse, G. The importance of inspection in clinical cardiology: Frank’s sign. Clin. Case Rep. 10, e6150 (2022).
Kwai-Ping Suen, L., Lau, Y. K., Ma, H. C., Lai, K. W. & Holroyd, E. Predictive value of auricular diagnosis on coronary heart disease. Evidence-Based Complement. Altern. Med.: eCAM 706249 (2012).
Scanu, A. M. Lipoprotein(a): A genetically determined lipoprotein containing a glycoprotein of the plasminogen family. Semin. Thromb. Hemost. 14, 266–270 (1988).
McLean, J. W. et al. cDNA sequence of human apolipoprotein(a) is homologous to plasminogen. Nature 330, 132–137 (1987).
Orsó, E. & Schmitz, G. Lipoprotein(a) and its role in inflammation, atherosclerosis and malignancies. Clin. Res. Cardiol. Supplements 12, 31–37 (2017).
Seimon, T. A. et al. Atherogenic lipids and lipoproteins trigger CD36-TLR2-dependent apoptosis in macrophages undergoing endoplasmic reticulum stress. Cell Metabol. 12, 467–482 (2010).
Nielsen, L. B., Juul, K. & Nordestgaard, B. G. Increased degradation of lipoprotein(a) in atherosclerotic compared with nonlesioned aortic intima-inner media of rabbits: In vivo evidence that lipoprotein(a) May contribute to foam cell formation. Arterioscler. Thromb. Vasc. Biol. 18, 641–649 (1998).
Sourij, C. et al. Changes in lipoprotein(a) levels in people after ST elevation myocardial infarction-—the STEMI-lipids study. Int. J. Mol. Sci. 24, 15531 (2023).
Vinci, P. et al. Lipoprotein(a) as a risk factor for cardiovascular diseases: Pathophysiology and treatment perspectives. Int. J. Environ. Res. Public Health 20, 6721 (2023).
Grundy, S. M. et al. AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation 139, e1082–e1143 (2019).
Bittner, V. A. et al. Effect of alirocumab on lipoprotein(a) and cardiovascular risk after acute coronary syndrome. J. Am. Coll. Cardiol. 75, 133–144 (2020).
Acknowledgements
The authors extend sincere thanks to the members of the Chengde Central Hospital for their contribution.
Funding
This research was funded by Medical Science Research Project of Hebei Province (No. 20200348), S & T Program of Chengde (No. 202109A019), and Project for Cultivating Innovative Ability of Postgraduates at Chengde Medical University (No. CYCXZZ202508).
Author information
Authors and Affiliations
Contributions
L.D. contributed to the design and conduct of the study, led data validation, project administration, funding acquisition, review and approval of the manuscript, and decision to submit the manuscript for publication. G.R. and Y.H. contributed to the collection, analysis and interpretation of the data, preparation and editing the manuscript. D.J. and G.J. contributed to the collection and management of the data. Z.D. contributed to the design and conduct of the study, review and approval of the manuscript, and decision to submit the manuscript for publication. Y.Y., G.Y., L.L., Y.Y., andG.J. facilitated the planning and carrying out of the study. All authors contributed to the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This retrospective study was approved by the Ethics Committee of the Chengde Medical University. The research in Chinese clinical trial registry http://www.chictr.org.cn, registration number: ChiCTR2000041499. All participating subjects were fully aware of the trial and signed informed consent. All methods in this study were performed in accordance with the relevant guidelines and regulations and the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, R., Yang, H., Dou, J. et al. Diagnostic value of the diagonal earlobe crease in combination with lipoprotein(a) in coronary heart disease. Sci Rep 15, 21047 (2025). https://doi.org/10.1038/s41598-025-06464-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06464-1