Abstract
Although the immunohistochemical expression of the transmembrane sialoglycoprotein podoplanin (D2-40) has been repeatedly reported as a factor of prognosis in various tumor entities—its potential prognostic relevance in squamous cell carcinomas of the vulva remains to be evaluated. In the present study, we evaluated 68 patients with primary vulvar carcinomas (VC) and analyzed the cytoplasmic/membranous immunohistochemical expression of podoplanin in viable tumor cells and cancer-associated fibroblasts (CAFs) within the adjacent peritumoral stroma. To determine potential associations between podoplanin expression and traditional clinicopathological parameters (e.g., tumor stage, infiltration depth, groin lymph node metastasis), as well as with local recurrences, metastases, and patient’s overall survival, subsequent data analysis was conducted using Spearman correlation analysis, Fisher’s exact test and the log-rank test (Mantel-Cox). Although our results did not substantiate a positive correlation of podoplanin expression in tumor cells or CAFs with traditional histomorphological parameters, we propose a prognostic potential of podoplanin as a tissue-based biomarker in HPV-associated VC. In our exploratory pilot study, we observed a significantly improved overall survival in this distinct subgroup (Log-rank (Mantel-Cox) test; p = 0.0399). The results of our retrospective study may support the expectations that podoplanin, a common and widely available antibody, could be used as a tool for prognostic purposes in the future. Further research and validation are necessary before these markers can be implemented in clinical practice.
Similar content being viewed by others
Introduction
The academic-driven establishment of commonly available and easily applicable diagnostic and prognostic markers remains key in “orphan diseases” such as vulvar cancer (VC), where a variety of factors for instance the absence of particular screening programs as well as the challenge of enrolling a sufficient number of patients within clinical trials—just to name a few—have so far hindered effective improvements in terms of long-term survival1. Up to now, several approaches aimed to assess histomorphological aspects of the neoplasm, its (micro-)environment, or the interaction of them both in order to stratify the individual underlying biological tumor behavior. The prognostic relevance of the overall pattern of tumor infiltration, the morphological aspect of infiltrating nuclei, as well as distinct immunohistochemical aspects of an epithelial-to-mesenchymal transition (EMT) at the front of invasion were tested with partially promising results2,3,4,5.
Due to its common use as a diagnostic marker in routine surgical pathology for detection of lymphovascular space infiltration also in VC patients, the mucin-type sialoglycoprotein podoplanin (D2-40), is broadly available in almost all pathological laboratories and most research labs. Despite the specific labeling of the lymphatic endothelium, cancer cells as well as dendritic cells and especially cancer-associated fibroblasts (CAFs) express podoplanin to varying degrees—with poor clinical prognosis in case of high-rates CAFs within pulmonary adenocarcinoma as well as invasive breast cancers and a distinct relation with patient clinical outcome in case of tumoral D2-40 expression on cancer cells6,7,8,9,10,11. Despite the employment of the D2-40 antibody for the detection of intratumoral lymphatic vessel density in VC by Goes et al., a distinct evaluation of podoplanin expression in VC cells and corresponding CAFs has—to our knowledge—not yet been established12. In the present study, we systematically examined the clinical relevance and the prognostic role of both podoplanin-expressing tumor cells as well as podoplanin expressing CAFs in HPV-associated and HPV-independent squamous cell carcinomas of the vulva.
Material and methods
Study cohort
In this study, 68 patients who underwent vulvectomy for squamous cell carcinoma of the vulva were included. Each patient subsequently received a detailed diagnostic pathological evaluation of the surgical specimen at the University Hospital of Saarland in Homburg, Germany. Patients were identified in cooperation with the Saarland University Medical Center for Tumor Diseases (UTS) registry by searching the hospital’s internal databases using the ICD-O codes 8085/3, 8086/3, and 8070/3. As a priori defined, we excluded patients with solely high-grade squamous cell intraepithelial neoplasias (HSIL) and neoplasms of the vulva other than squamous cell carcinomas (e.g., adenocarcinomas, melanomas). Additionally, recurrent cancerous affections as well as patients who underwent only palliative surgery were excluded. Available data on survival, occurring local recurrences, and metastases were retrieved by the statewide-operating cancer registry ‘Saarland Cancer Registry’. The study was approved by the Ethics Committee of Saarland (study identification number 249/23, approved on 07. March 2024) and was performed according to the Declaration of Helsinki13.
Immunohistochemical stainings and interpretation
Immunohistochemical analysis was employed to assess the expression patterns of podoplanin in epithelial neoplastic cells and cancer-associated fibroblasts (CAFs). Therefore, the surgical specimens were formalin fixed, paraffin embedded and cut into three 4 µm thin cuts (Leica RM 2235 rotation microtome, Leica Microsystems, Wetzlar, Germany), which were mounted on slides (Matsunami TOMO) using a water bath (46 °C), and consecutively stored at 37 °C. Subsequent H&E staining was performed and served as a morphological control. For the immunohistochemical analysis, a primary antibody specific for podoplanin (mouse monoclonal antibody, Dako/Agilent, Santa Clara, CA, USA; clone D2-40) was applied for 32 min at 37 °C using the Benchmark Ultra (Ventana Medical Systems). Antibody binding was detected employing the ultraView Universal Alkaline Phosphatase Red Detection (Roche, Basel, Switzerland) in alignment with the manufacturer’s instructions and antigen retrieval at 97 °C (heat-induced) was performed using CC1 buffer (Ventana) for 64 min. Every staining series incorporated negative controls by waiving the primary antibody; lymphatic endothelium served as the internal on-slide positive control.
Furthermore, available p16 stainings of the associated diagnostic cases were re-evaluated as part of the study (n = 60); as defined by the ‘WHO Classification of Female Genital Tumors’, it hereby served as a surrogate marker for HPV association14, and a ‘block type’ p16 expression of at least 20 neighboring p16-expressing tumor cells was considered as HPV positive (HPV-associated VC). Tumors with a ‘patchy’ (irregular, nuclear and cytoplasmatic stainings distributed in a heterologous manner) p16 expression or the absence of its immunohistochemical expression were considered as HPV-independent.
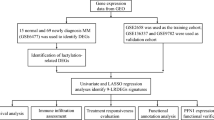
As a first step in the analysis, the overall percentage of cytoplasmatically/membranously podoplanin stained tumor cells was determined; to further evaluate a potential prognostic impact of podoplanin, a ‘podoplanin positive’ cohort with > 2% protein expression and ‘podoplanin negative’ cohort with ≤ 2% protein expression in viable tumor cells were defined. According to the analysis of CAFs by the team of Schoppmann et al., the CAFs at the invasive tumor front were rated as either ‘CAFs podoplanin positive’ in case > 10% of the fibromatous component of the peritumoral stroma expressed podoplanin or ‘CAFs podoplanin negative’ in case the podoplanin expression of the fibromatous component of the peritumoral stroma was less than 10%. Figure 1 outlines concrete examples of our defined cohorts. In order to reduce inter-observer variability, histomorphological analyses were performed collaboratively using a multi-head light microscope (GGK, AB, MP, MN), and upcoming discrepancies were addressed through consensus-based discussions (MW).
Display of immunohistochemical podoplanin expression types. (A) ‘Podoplanin positive’ expression type with > 2% viable tumor cells showing a cytoplasmatic staining pattern. (B) ‘Podoplanin negative’ expression type with ≤ 2% viable tumor cells showing cytoplasmatic staining pattern. (C) Within the peritumoral stroma > 10% of the fibromatous component showed podoplanin-expression (‘CAFs podoplanin positive’). As a regular on-slide positive control, podoplanin positive lymphatic endothelium can be seen in the right half of the image.
Statistical analysis
All data were stored in an Excel file and imported into GraphPad (Boston, MA 02110, US) for calculations. Spearman correlation analysis was used to assess the statistical relationships between percentage of podoplanin expression and clinicopathological variables. Positive correlations were tested against the null hypothesis of being due to random sampling. In a next step Fisher’s exact test was employed to test for differences in recurrence and metastasis between our priori defined groups and consecutively Log-rank (Mantel-Cox) test was used to test for the prognostic impact of podoplanin expression in CAFs and tumor cells on overall survival. Solely results with α < 0.05 were considered as statistically significant.
Results
Patient data
Our cohort comprises a total of 68 patients with primary surgically treated VC (median age 65.5 years [52–78.5 years, 25%-75% Percentile]). Among these, 11 patients presented with tumor stage T1a, 44 with T1b, 12 with T2, and 1 with T3. Overall, 16 patients showed involvement of the inguinal lymph nodes (videlicet at least N1 according to the actual TNM guidelines, 8th edition 2018), while 52 patients had no affection of the groin lymph nodes. During an average follow-up period of 60.1 months, 14 patients developed a locoregional recurrence, 6 patients experienced distant metastasis, and 22 patients died. Refer to Table 1 for a summary of the clinical information of our study cohort.
Correlation analysis of D2-40 expression with classic pathomorphological parameters
Our preliminary correlation analysis did not identify any significant correlations of the amount of D2-40 expression/CAFs and considered clinicopathological parameters; hereby, they were neither associated with tumor stage, infiltration depth, amount of groin lymph node affection, nor histological tumor grade, see Tables 2 and 3 for Spearman r and two-tailed p-values of each individual analysis. Additionally, the amount of podoplanin-expressing tumor cells was not associated with D2-40 positive CAFs (r = 0.1635 [CI: − 0.08511 to 0.3929]; p = 0.1828).
Impact of D2-40 expression on recurrence, metastasis, and survival
Within our cohort, neither recurrence risk nor the development of metastasis differed significantly with regard to podoplanin expression (Fisher’s exact test; p = ≥ 0.9999) or amount of podoplanin positive CAFs (Fisher’s exact test; p = 0.2909 and p = 0.6201 respectively). Furthermore, overall survival was not distinctively impaired in relation to the immunohistochemical expression of podoplanin within neoplastic cells (Log-rank (Mantel-Cox) test; p = 0.0523, x2 = 3.767) or podoplanin-positive CAFs (Log-rank (Mantel-Cox) test; p = 0.5091, x2 = 0.4359); see Fig. 2A, B. Nevertheless, consecutive further subgroup analyses—achieved by splitting the study cohort with regard to inguinal nodal involvement (N0 vs. N-positive), tumor stage (locally confined tumors defined as T1a and T1b vs. local anatomical structures infiltrating tumors defined as T2 and T3), and HPV status (positive vs. negative)—suggested a significant impact on survival in the cohort of HPV-associated VC. Here, patients with an expression of podoplanin in viable tumor cells (‘podoplanin positive’) showed a significantly better prognosis (Log-rank (Mantel-Cox) test; p = 0.0399, x2 = 4.223); the analysis of CAFs did not play a prognostic role in any of the subgroups put to test. Table 4 and Fig. 2C, D visualize the association of podoplanin expression with regard to selected (sub-)groups.
Survival of VC patients stratified by podoplanin-expression in cancer cells and CAFs. Although within our study cohort overall survival was initially neither related to podoplanin (podoplanin positive vs. podoplanin negative tumors) expression (A) nor the amount of podoplanin positive CAFs (B), a subsequent subgroup analysis determined the prognostic potential of podoplanin positive HPV-associated tumors (Log-rank (Mantel-Cox) test; p = 0.0399, x2 = 4.223; (C). Interestingly, such an effect could not be observed in patients with HPV-independent tumorigenesis (D).
Discussion
In the present study, we systematically examined the immunohistochemical expression of podoplanin as an easily applicable and broadly available biomarker in not only viable vulvar carcinoma cells but also peritumoral fibroblasts. Hereby, we did not only consider biologically and histologically established risk factors such as the presence of inguinal lymph node metastases or the depth of infiltration but also we evaluated the prognostic relevance of D2-40 expression with regard to the underlying tumor entity and its respective (viral) tumorigenesis, namely in HPV-associated VC and HPV-independent VC.
Comparable approaches in diverging tumor entities have already been described in the literature—albeit with so far inconclusive evidence9,15,16,17,18,19. With respect to squamous cell carcinomas of the oral cavity a recent review by Mello et al. identified 22 cohort and seven cross-sectional studies that analyzed the prognostic impact of D2-40 expression within tumor cells on patient`s survival and/or clinicopathological variables15. Four out of twelve studies determined a general negative association between podoplanin expression and overall survival9,16,17,20. Hu et al. systematically reviewed the prognostic value of D2-40 within lung squamous cell cancer and included 8 studies in a comprehensive metanalysis. Although they determined a high correlation of its immunohistochemical expression with tumor differentiation, they did not identify any correlation with lymphatic and vascular invasion or metastasis; interestingly, they postulate a positive (better) association between podoplanin expression and survival21. Within squamous cell carcinoma of the skin podoplanin expression was reported to be associated with higher risk of lymph node metastasis and lymphovascular invasion22 and shorter survival18,23. Interestingly, Neinaa et al. showed a varying D2-40 expression depending on the underlying tumor entity (basal cell carcinoma, squamous cell carcinoma, basosquamous carcinoma); nevertheless, all examined tumor types differed in their higher podoplanin expression in contrast to physiological control epidermis. From a pathophysiological point of view, podoplanin as a transmembrane glycoprotein may be linked in particular to processes of EMT, cell migration, and platelet aggregation via interactions with the cell–cell adhesion protein E-cadherin and the C-type lectin-like receptor 224,25,26,27.
In our study, we neither detected any impact of podoplanin expression on classical prognostic parameters such as infiltration depth, nor did we find a clear association with the risk of local recurrence or metastasis in VC. Furthermore, we did not find a relevant use case for podoplanin staining of CAFs in VC—in contrast to preliminary findings, for example in breast cancer8. Even though the expression of D2-40 was not related to overall survival in the initial log-rank analysis within our cohort, a consecutive subgroup analysis proposed a significant prognostic potential within HPV-associated tumors, where patients with ‘podoplanin positive’ tumors had a favorable prognosis in comparison to ‘podoplanin negative’ tumors. In terms of their clinical utility, the results facilitate the identification of a subgroup with arguably good prognosis, which could be quickly and routinely inferred from a block-type p16 positivity (HPV association) and existing podoplanin expression.
Since there is great disagreement in the existing literature regarding the optimal cut-off of a defined podoplanin expression, we decided against an arbitrary value, which would divide interpretations/quantifications of the stainings into different groups of podoplanin expression (high/medium/low). In comparison, we opted for a cut-off that follows the all-or-nothing principle (either negative or positive). We attached particular importance to not directly define the value ‘0%’ as a negative cut-off since our selected cut-off of ≤ 2% as ‘negative’ allowed not only further reduction of potentially occurring interobserver variabilities but also avoids confusion with regular staining artifacts. In our opinion, alternative binary cut-off values, of for example, 5%, 10%, 20%, and 50%, do not sufficiently reflect this consideration and were therefore not adopted for our analysis16,17,28,29. Nevertheless, it is important to note that conflicting results of the prognostic ability of podoplanin expression were repeatedly reported15,21 and it remains to be resolved if differing results and conclusions arise from either laboratory, diagnostic or biological variations in the different studies. When interpreting our results, several potential limitations must be considered, including the sample size, the retrospective study design, and the exploratory nature of the study. Further external validation is required before these findings can be translated into clinical practice. Furthermore, future studies could explore the relationship between distinct patterns of tumor infiltration (e.g., pushing vs. spray-like invasion) and podoplanin expression. Looking ahead, only a uniformity of the methodology and the creation of an experimental-methodological consensus regarding e.g., specific antibodies and interpretations of the expression analysis would allow for inter-institutional comparability and subsequently can guarantee a higher level of evidence in a next step.
In conclusion, our pilot study suggests the prognostic value of the widely available immunohistochemical marker podoplanin for assessing the prognosis of HPV-associated vulvar epithelial neoplasia. However, further studies are needed to validate the results and further compare the expression of podoplanin in VC also with additional clinicopathological parameters such as PD-L1 expression or genomic alterations. Nevertheless, the search for new potential tissue-based biomarkers and individualized treatment approach in HPV-associated VC is particularly reasonable for younger patients, who are often affected by a virus-dependent pathogenesis.
Data availability
Interested parties are warmly invited to contact the corresponding author for individual options.
References
Bucchi, L., Pizzato, M., Rosso, S. & Ferretti, S. New insights into the epidemiology of vulvar cancer: Systematic literature review for an update of incidence and risk factors. Cancers 14, 389 (2022).
Rodrigues, I. S. et al. Epithelial-mesenchymal transition-like events in vulvar cancer and its relation with HPV. Br. J. Cancer 109, 184–194 (2013).
Brambs, C. E. et al. Epithelial-mesenchymal transition (EMT) in vulvar cancer with and without inguinal lymph node involvement. J. Cancer Res. Clin. Oncol. 148, 1183–1193 (2022).
Zare, S. Y., Ciscato, A. & Fadare, O. Tumor budding activity is an independent prognostic factor in squamous cell carcinoma of the vulva. Hum. Pathol. 126, 77–86 (2022).
Trietsch, M. D. et al. Spindle cell morphology is related to poor prognosis in vulvar squamous cell carcinoma. Br. J. Cancer 109, 2259–2265 (2013).
Kawase, A. et al. Podoplanin expression by cancer associated fibroblasts predicts poor prognosis of lung adenocarcinoma. Int. J. Cancer 123, 1053–1059 (2008).
Hoshino, A. et al. Podoplanin-positive fibroblasts enhance lung adenocarcinoma tumor formation: Podoplanin in fibroblast functions for tumor progression. Cancer Res. 71, 4769–4779 (2011).
Schoppmann, S. F. et al. Podoplanin-expressing cancer-associated fibroblasts are associated with poor prognosis in invasive breast cancer. Breast Cancer Res. Treat. 134, 237–244 (2012).
Kreppel, M., Scheer, M., Drebber, U., Ritter, L. & Zöller, J. E. Impact of podoplanin expression in oral squamous cell carcinoma: Clinical and histopathologic correlations. Virchows Arch. 456, 473–482 (2010).
Shibahara, J., Kashima, T., Kikuchi, Y., Kunita, A. & Fukayama, M. Podoplanin is expressed in subsets of tumors of the central nervous system. Virchows Arch. 448, 493–499 (2006).
Krishnan, H. et al. Podoplanin: An emerging cancer biomarker and therapeutic target. Cancer Sci 109, 1292–1299 (2018).
Goes, R. S. et al. Intratumoral lymphatic vessel density in vulvar squamous cell carcinomas. Int. J. Gynecol. Pathol. 31, 8–14 (2012).
World Medical Association Declaration of Helsinki. JAMA 310, 2191 (2013).
Lokuhetty D, et al. Female Genital Tumours. WHO Classification of Tumours. (Internal Agency for Research on Cancer (IARC), 2020).
Mello, F. W. et al. Prognostic and clinicopathological significance of podoplanin immunoexpression in oral and oropharyngeal squamous cell carcinoma: A systematic review. J. Oral Pathol. Med. 50, 1–9 (2021).
Seki, S. et al. Prognostic value of podoplanin expression in oral squamous cell carcinoma-a regression model auxiliary to UICC classification. Pathol. Oncol. Res. 20, 521–528 (2014).
Hwang, Y. S. et al. Insulin-like growth factor-II mRNA binding protein-3 and podoplanin expression are associated with bone invasion and prognosis in oral squamous cell carcinoma. Arch. Oral Biol. 69, 25–32 (2016).
Kreppel, M. et al. Podoplanin expression in cutaneous head and neck squamous cell carcinoma—Prognostic value and clinicopathologic implications. J. Surg. Oncol. 107, 376–383 (2013).
Kühn, J. P. et al. Podoplanin expression in lymph node metastases of head and neck cancer and cancer of unknown primary patients. Int. J. Biol. Mark. 37, 280–288 (2022).
Kreppel, M. et al. Podoplanin expression predicts prognosis in patients with oral squamous cell carcinoma treated with neoadjuvant radiochemotherapy. Oral Oncol. 47, 873–878 (2011).
Hu, L. et al. Podoplanin is a useful prognostic marker and indicates better differentiation in lung squamous cell cancer patients? A systematic review and meta-analysis. BMC Cancer 20, 424 (2020).
Gülseren, D., Gököz, Ö., Karahan, S. & Karaduman, A. Podoplanin expression in cutaneous squamous cell carcinomas and its relationship to histopathological prognostic factors. J. Histotechnol. 43, 147–152 (2020).
Cañueto, J. et al. The expression of podoplanin is associated with poor outcome in cutaneous squamous cell carcinoma. J. Cutan. Pathol. 44, 144–151 (2017).
Krishnan, H. et al. Podoplanin: An emerging cancer biomarker and therapeutic target. Cancer Sci. 109, 1292–1299 (2018).
Swain, N., Kumar, S. V., Routray, S., Pathak, J. & Patel, S. Podoplanin—a novel marker in oral carcinogenesis. Tumor Biol. 35, 8407–8413 (2014).
Lowe, K. L., Navarro-Nunez, L. & Watson, S. P. Platelet CLEC-2 and podoplanin in cancer metastasis. Thromb. Res. 129, S30–S37 (2012).
Martín-Villar, E. et al. Podoplanin binds ERM proteins to activate RhoA and promote epithelial-mesenchymal transition. J. Cell. Sci. 119, 4541–4553 (2006).
Foschini, M. P. et al. Podoplanin and E-cadherin expression in preoperative incisional biopsies of oral squamous cell carcinoma is related to lymph node metastases. Int. J. Surg. Pathol. 21, 133–141 (2013).
Wakisaka, N. et al. Induction of epithelial–mesenchymal transition and loss of podoplanin expression are associated with progression of lymph node metastases in human papillomavirus-related oropharyngeal carcinoma. Histopathology 66, 771–780 (2015).
Acknowledgements
Figure 1 was created with Biorender.com. This manuscript was submitted as an abstract to the ESGO 2025 Congress. All data was handled in alignment with the Ethics Committee of Saarland, this study (study identification number 249/23) was approved on 07. March 2024 and was further conducted in alignment with national law. Due to the retrospective nature of the study, the Ethics Committee of Saarland waived the need of obtaining informed consent. Neither personal data nor images that allow identification of the patients are presented. During the revision of this work the authors used ChatGPT 4 (OpenAI; USA) in order to increase readability of certain phrasings and wordings. After using this tool/service, the authors reviewed and edited the content as needed and take full responsibility for the content of the publication.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research received no external funding.
Author information
Authors and Affiliations
Contributions
Study design: GGK, AB, MPN Acquisition of samples and data: BHH, EFS, AB, MP, LS, BH, Statistical analysis: GGK, MPN Data analyzation/interpretation: GGK, MPN, AH, RS Histological tissue processing/Pathological diagnostics/interpretation: ME, GGK, MPN, MW Coordination and supervision: MW, AH, RS GGK wrote the first draft. All authors contributed to the final draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests pertaining to this study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Klamminger, G.G., Nigdelis, M.P., Bitterlich, A. et al. Evaluation of podoplanin expression in vulvar squamous cell carcinoma and stromal fibroblasts and its prognostic implications. Sci Rep 15, 20224 (2025). https://doi.org/10.1038/s41598-025-06908-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-06908-8