Abstract
This study explores the experiences and challenges faced by clinical nurses in early identification and intervention of mild cognitive impairment (MCI) risk factors in older adults. This qualitative descriptive study was conducted between September 2020 and January 2021 in three tertiary hospitals in China. Thirteen clinical nurses were recruited through purposive sampling based on their experience with older adults having cognitive concerns. Data were collected via semi-structured interviews, and content analysis was used to identify key categories in the nurses’ experiences. Three main categories emerged: (1) Navigating older adults’ perceptions of aging and self, (2) Challenges in building therapeutic alliances with families, and (3) Facing limitations in translating intentions into practice. Nurses recognized the critical importance of early identification and intervention for MCI but expressed concerns about their limited knowledge and the practical feasibility of implementing interventions. Barriers included patients’ reluctance to acknowledge MCI and their complex perceptions, lack of training and awareness, and insufficient support and resources from families. Findings suggest a need for tailored interventions, targeted education, and enhanced support systems to address these challenges and improve early MCI interventions.
Similar content being viewed by others
Introduction
Mild cognitive impairment (MCI) represents a transitional state of cognitive function between normal aging and dementia, including Alzheimer’s disease1,2. MCI is diagnosed when there is a mild decline in one or more cognitive domains, such as memory, executive functioning, attention, visuospatial skills, or language3,4. Although basic daily living activities are generally preserved5, individuals with MCI may experience difficulties or take longer to complete instrumental activities of daily living, such as driving, daily shopping, managing finances, medication management, and household tasks. The aging population has contributed to an increased prevalence of MCI, with an estimated average prevalence of approximately 16%6,7. Furthermore, individuals with MCI are at a higher risk of progressing to dementia compared to those with normal cognition2,8. While pharmacological interventions for MCI remain limited, non-pharmacological interventions have shown potential in alleviating or stabilizing MCI symptoms, with some individuals even reverting to normal cognition9.
In recent years, early recognition and intervention for MCI have attracted considerable attention in clinical practice. Research has demonstrated that cognitive function and daily living abilities in people with MCI can be improved through non-pharmacological interventions10,11,12. Among these, cognitive training and physical exercise have been particularly effective in improving cognitive function13,14. For example, nurse-led cognitive training programs have demonstrated improvements in certain cognitive abilities in older adults with MCI15. Other interventions, such as lifestyle modifications, psychological support, and dietary interventions, may also improve cognitive function by targeting modifiable risk factors16,17. Integrated interventions led by nurses that target modifiable risk factors have been shown to reduce cognitive decline in older adults with MCI18,19. These findings emphasize the crucial role that nurses play in the early identification and intervention of MCI to help maintain cognitive function.
Despite these advancements, challenges remain. Primary care nurses are well-positioned to support early detection of MCI by providing counseling and guiding patients toward appropriate interventions20. However, the subtle symptoms of MCI can easily be overlooked or misinterpreted, especially in older adults with multiple comorbidities21. In China, the limitations of the primary healthcare system, including a shortage of trained healthcare professionals, insufficient resources for cognitive health screening, and fragmented care pathways, further hinder access to timely medical support for MCI patients22. As a result, many individuals bypass primary care facilities and seek treatment directly at larger hospitals, which often leads to delayed diagnosis and intervention. These systemic challenges contribute to the significant difficulties nurses face in the early recognition and management of MCI23.
Additionally, the lack of awareness and information about MCI among older adults prevents many from seeking early cognitive assessment24,25. Many older adults with MCI, as well as their families, confuse MCI symptoms with normal aging26. Consequently, by the time they recognize cognitive decline, the optimal window for intervention may have passed. Furthermore, the stigma and uncertainty associated with cognitive impairment reduce the likelihood of patients and families seeking appropriate care27. The emotional toll on caregivers also complicates the situation, as they may experience frustration, stress, and health issues such as cognitive fatigue28.
These findings suggest that nurses face significant challenges in the early recognition and intervention of MCI. Thus, this study aims to explore clinical nurses’ experiences and perceived difficulties in identifying and addressing MCI risk factors among older adults.
Methods
Study design
This qualitative descriptive study, guided by the constructivist paradigm, utilized semi-structured individual interviews. A qualitative descriptive design, characterized by minimal theoretical orientation29, was deemed appropriate for this study as it aimed to explore nurses’ experiences and perceived difficulties in identifying and intervening in MCI risk factors among older adults, without adherence to pre-existing theories. This study referred to the Consolidated Criteria for Reporting Qualitative Research (COREQ), a 32-item checklist.
Participants
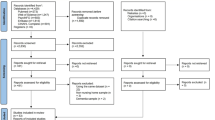
Clinical nurses providing care for older patients with MCI at three tertiary hospitals in Beijing, China, were recruited between September 2020 and January 2021. The inclusion criteria for participants were: (a) registered nurses working full-time, (b) responsible for the care of older patients with MCI, (c) experience in identifying and managing MCI risk factors, and (d) willingness to provide signed informed consent and voluntarily participate in the study. A purposive sampling method was used to ensure diversity in the sample, taking into account factors such as age, education, professional position, title, years of experience in cognitive impairment care and hospitals. One researcher (WHY), who worked at one of the hospitals, was familiar with the nurses and, based on this knowledge, identified potential participants who met the inclusion criteria. Permission for participant recruitment was obtained from the relevant hospital authorities. The sample size was determined when data saturation was reached, meaning no new information or categories emerged from the interviews.
Data collection
Data were collected through individual semi-structured interviews, guided by an interview protocol developed from a literature review and two pilot interviews, which led to minor adjustments. The final interview guide focused on the following topics: perceptions of early identification and intervention for MCI risk factors, experiences in identifying and addressing these factors, and perceived difficulties in implementing these practices in clinical settings. Detailed interview questions are provided in the supplementary materials.
After the two researchers (MJY and WHY) provided a detailed introduction to the study, the participants gave their informed consent and signed the consent form. One author (MJY) contacted participants via WeChat (a widely used social media platform in China) to schedule the interviews. Interviews were conducted in a convenient location chosen by the participants (such as a meeting room or duty room) within their respective hospitals, with an average duration of 42 min (range: 25–59 min). Due to COVID-19 restrictions, two interviews were conducted via secure video call as the participants were in isolation, while the remaining 11 were conducted face-to-face. All interviews were audio-recorded with participants’ consent, and appropriate measures were taken to ensure privacy and confidentiality. Only the researchers had access to the data and recordings. All interviews were audio-recorded with participants’ consent. Participant characteristics, such as age, gender, education level, position, professional title, and years of experience in cognitive impairment care, were collected during the interviews.
Data analysis
Data were analyzed using conventional content analysis as described by Hsieh and Shannon30,31. Audio recordings were transcribed verbatim in Chinese within 24 h of the interview. Transcripts were imported into NVivo 11 for data management and analysis. The two pilot interviews, having provided valuable insights, were included in the final analysis. Initially, transcripts were read multiple times to gain familiarity with the data. Two authors (MJY and WHY) independently conducted inductive coding to ensure a more comprehensive and unbiased analysis, categorizing relevant text into distinct codes. These codes were then organized into potential categories, which were refined and defined to form consistent patterns. The author group discussed the categories until consensus was achieved. The entire analysis process was conducted under the supervision of LZ, an expert in geriatric care and qualitative research. The final results were translated into English by MJY, and checked by ZH, an author fluent in English, to ensure accuracy and consistency.
Ethical considerations
Ethical approval was granted by the Ethical Committee of the School of Nursing, Peking Union Medical College (Ethics Review No. [2020]05). Informed consent was obtained from all participants, who were made aware of their right to withdraw from the study at any time without consequences. To protect confidentiality, all data, including interview transcripts and analysis results, were anonymized, and access was restricted to the research team. All stages of the study were conducted in accordance with the provisions of the Declaration of Helsinki.
Results
A total of 13 eligible nurses from three tertiary hospitals participated in the study, with no withdrawals during the interview process. Table 1 presents the characteristics of the recruited nurses. Eleven subcategories were identified and grouped into three overarching categories, reflecting the perceived sources of difficulties faced by nurses, categorized from the perspectives of patients, family members, and the work environment (Table 2).
Category 1: Navigating older adults’ perceptions of aging and self
This category reflects how older adults perceive their aging process and cognitive changes, often interpreting early signs of MCI through the lens of aging stereotypes, stigma, and concern for their families. These perceptions significantly shape their willingness to acknowledge and respond to cognitive decline. Nurses described that many patients tended to normalize symptoms, view cognitive issues as taboo, or fear becoming a burden. These intertwined beliefs complicate early identification and engagement with MCI care. The following three subcategories highlight the key patterns observed by nurses in patients’ attitudes and behaviors.
Subcategory A. Aging stereotypes
Nurses reported that many older adults often confuse MCI with normal aging when they are unaware of their diagnosis in the early stages of MCI. Even when experiencing cognitive issues such as memory loss or behavioral changes, these individuals view such problems as a natural part of aging, undermining the seriousness of early intervention. Consequently, nurses expressed frustration over their inability to engage patients’ attention despite repeated emphasis on the importance of early recognition and intervention.
“In fact, the patients do not know what the MCI is, even with memory loss, they still think it is a common problem for the elderly, not a big deal.” (N5)
“The patients do not pay attention to the cognitive problems, they think the decline in function in all aspects of their body is normal at this age. They are not willing to accept any intervention.” (N7)
“Both the patients and their families think it is the normal process of aging, so they do not want to receive any treatment or care.” (N13)
Subcategory B. Stigma
Participants noted that a significant number of patients struggle to accept their diagnosis of MCI when informed about their condition and the need for early intervention. Stigma surrounding cognitive impairment often leads patients to deny their condition, resulting in feelings of inferiority and shame. Only a small percentage of patients, typically those with higher education levels, actively seek information about managing their condition.
“Some patients with high self-esteem would deny it, and just tell us not to call them cognitively impaired.” (N6)
“He had something like an inferiority complex in it, feeling that he was useless, and he did not think intervention would help.” (N9)
“First, it is hard for them to accept that they have MCI. Because to them, cognitive impairment or dementia sounds ‘harsh’, they cannot think that they have this disease.” (N13)
Subcategory C. Fear of burdening family
Nurses observed that some older adults hesitate to disclose their cognitive issues to their families when they are diagnosed with MCI, fearing they will become a burden. This reluctance poses significant challenges for early intervention, as patients frequently dismiss their illnesses as unimportant.
“A lot of patients with mild symptoms when they hear that they require treatment would tell us, ‘forget it, I do not want to cause trouble for the kids.’” (N6)
“Given that many old people attach great importance to children, they do not want to be a burden to their children.” (N7)
“Some patients believe that even intervention cannot cure them completely, and they are more worried that their growing cognitive decline will put a greater burden on their families.” (N8)
Category 2: Challenges in building therapeutic alliances with families
This category illustrates the barriers nurses face when trying to collaborate with family members in the care of older adults with MCI. Although family involvement is essential for early detection and intervention, nurses often encounter limited support from patients’ relatives. Some families show insufficient awareness of cognitive symptoms, while others demonstrate low levels of engagement due to time constraints or emotional fatigue. Moreover, the emotional burden of caregiving over time can lead to frustration and disengagement. Together, these factors undermine the establishment of an effective therapeutic alliance and hinder continuity of care. The following subcategories detail these interconnected challenges.
Subcategory A. Insufficient attention
Nurses highlighted difficulties in obtaining information from family members, as MCI symptoms can be subtle. Family members often overlook these symptoms, complicating the nurses’ efforts to communicate intervention options effectively.
“Family members are less likely to pay attention to MCI symptoms, such as memory loss.” (N3)
“Their concerns as children are different from ours. Even in instances where they notice these symptoms, they are likely to ignore or not take them seriously.” (N10)
Subcategory B. Lack of family engagement
Most older patients regard their children as their primary support but find their involvement minimal due to busy schedules. This lack of engagement creates barriers for nurses attempting to encourage family participation in early interventions.
“The patients’ children are so busy that they rarely communicate with us, let alone discuss the treatment options.” (N9, N11)
“The current situation is that everyone works from nine to five, thus, the family members actually do not have enough energy and patience to join in.” (N13)
“Sometimes it is unknown whether the obtained information is true or false because some patients tell contradicting stories.” (N1)
“When asked about the condition of the patients, the family members did not have a consistent story. Some family members may not even know much about the illness.” (N12)
Subcategory C. Emotional exhaustion
Nurses expressed concerns about caregivers experiencing emotional exhaustion due to the sustained nature of cognitive interventions. This fatigue can lead to the development of negative emotions such as frustration, resentment, and helplessness, prompting caregivers to withdraw support for further treatment.
“After spending a long time caring for MCI patients, some family caregivers become more frustrated and resentful. Some even show signs of disengagement towards the patients in front of us, while others may do so when we’re not around.” (N3)
“The cognitive condition of a patient is ever-changing, and thus family members are exhausted at the thought of the series of examinations and treatments needed.” (N13)
Category 3: Facing limitations in translating intentions into practice
This category highlights the gap between nurses’ intentions to support MCI care and the practical barriers they face in implementing interventions. Despite recognizing the importance of early identification and management of MCI, nurses encountered significant limitations in communication, unclear professional roles, and lack of training and resources. Additionally, the clinical feasibility of interventions was often challenged by patients’ comorbidities, resistance to non-pharmacological options, and nurses’ limited time due to workload pressures. The following five subcategories outline the multi-layered challenges that impede the translation of knowledge and intention into routine practice.
Subcategory A. Communication deficit
Nurses encountered challenges when discussing MCI interventions with patients. Many patients were unaware of their diagnosis, complicating the communication process. Furthermore, discrepancies in information from family members added to the difficulty of accurately assessing patient conditions.
“Many patients were ‘tricked’ to go to hospital by their families in the name of medical examination. In such instances, we cannot tell the patient directly about the condition as usual because it might irritate them, which hinders the communication.” (N3)
“For example, in the process of assessing, the older patients with hearing impairments respond slowly to questions and sometimes even make mistakes. At this point, it is hard to tell if they do not understand or they cannot hear clearly.” (N7)
Subcategory B. Unclear role and responsibilities in MCI identification and intervention
While most nurses recognized the importance of early intervention for MCI, many felt unclear about how to identify risk factors and implement interventions. They often relied on existing clinical experience rather than formal training. Some nurses believed that the assessment and treatment of risk factors for MCI were still mainly done by doctors, and it was not clear what they could do in this regard.
“In terms of intervention, we are still doing simple things such as teaching patients to exercise. We do not know what else we can do.” (N5)
“I really do not know enough about the risk factors of MCI. Thus, it is difficult for us to identify these risk factors, and frankly we do not know how to intervene.” (N7, N11)
“Doctors may be more responsible for the identification and treatment of MCI. What we can do is very little and mainly lies in education.” (N1, N2)
Subcategory C. Implementability concerns
Nurses voiced concerns about the feasibility of early interventions, particularly given the prevalence of comorbid conditions among older patients with MCI. Many patients preferred medication over non-pharmacological interventions.
“I think it is difficult to implement MCI intervention because not all older MCI patients can accept the disease, let alone get them to accept the intervention.” (N3, N9)
“Many older patients are dependent on drugs, so they preferred medication to some non-pharmacological intervention.” (N12)
“The biggest problem is that most of the older MCI patients still have more serious diseases, thus, they already have a lot of other interventions that may not cooperate with MCI intervention.” (N5)
Subcategory D. Resource constraints
Although nurses acknowledged the importance of early MCI interventions, they reported limited access to specialized training, standardized protocols, and educational resources. This lack of professional support led to uncertainty about identifying risk factors and implementing appropriate care. As a result, they often turned to informal sources such as peer experience or online videos.
“There is no specific training or materials on the identification and intervention of risk factors for MCI, we actually do not know exactly what to do.” (N7)
“I can only learn some finger exercises from related videos and the experiences of other nurses to help patients improve their cognitive function.” (N13)
Subcategory E. Time and workload restrictions
Nurses frequently cited time constraints and heavy workloads as major barriers to delivering cognitive care. Clinical duties often took precedence over MCI-related interventions, which were viewed as secondary to routine treatment and care. In addition, responsibilities in research and teaching further limited their available time and energy.
“In fact, we have a large amount of daily treatments and workload. Although cognitive care is very important, we do not have time to do it because we have to ensure that we complete the main and most basic treatment and care. That is to say, we must have time first.” (N11)
“Besides clinical work, we still have research and teaching tasks. There is a lot of pressure on us.” (N9)
Discussion
This study explored the experiences of clinical nurses in identifying and intervening in risk factors for MCI in older patients, revealing significant challenges faced by nurses in the Chinese context. Three interconnected categories were identified: navigating older adults’ perceptions of aging and self, challenges in building therapeutic alliances with families, and facing limitations in translating intentions into practice. Concurrently, eleven subcategories were described from three perspectives that further specified the difficulties perceived by nurses under each category.
A prominent issue highlighted by nurses was the lack of sufficient attention paid to cognitive impairment by patients and their families. This aligns with existing literature that underscores the critical role of early detection and intervention in preventing or delaying cognitive decline in individuals with MCI32. Research has shown that nurses are pivotal in understanding the challenges faced by older adults with MCI, assisting patients and their caregivers in recognizing the causes and risk factors of cognitive impairment, and facilitating discussions with healthcare providers regarding early intervention strategies33,34. The findings from our interviews indicate that complex emotional responses from older adults with MCI and their caregivers, as well as the clinical work environment, significantly influence nurses’ efforts to address risk factors for MCI.
Consistent with prior studies, older adults with MCI and their caregivers often normalize forgetfulness as a natural part of aging35,36. This misconception can hinder timely intervention, as patients frequently interpret their cognitive decline as an expected aging process rather than a sign of MCI26. Additionally, ageism, or age-related stereotypes, may contribute to the reluctance of both patients and healthcare providers to acknowledge and address cognitive decline as a serious medical issue. Ageist attitudes can lead to the dismissal of cognitive symptoms as just part of aging, which further delays appropriate intervention27,37. The interviews suggest that enhancing community awareness and education about MCI and its differentiating factors from normal aging is essential. Current national policies addressing aging issues are progressing, but the implementation of primary healthcare services related to MCI remains sluggish.
Moreover, perceived stigma and feelings of being a burden were found to deter older adults with MCI from confronting their condition38. The societal view of dementia as a devastating illness exacerbates fears of social stigma, leading many patients to avoid discussing their cognitive issues26,39. The emotional toll from a diagnosis of MCI often manifests as feelings of fear, hopelessness, and reluctance to seek support, which complicates the nurses’ role in providing information and support40,41. This suggests that effective nursing care for MCI patients involves not only enhancing cognitive function but also sensitively communicating the realities of cognitive impairment, coping with stigma, and providing strategies for adaptation to cognitive changes.
Social support from caregivers and community involvement is vital in mitigating the negative psychological effects associated with MCI and promoting cognitive health42,43. However, our findings reveal a gap in family support for older patients with MCI, largely due to the increased demands placed on adult children in modern society. The demographic pressures stemming from China’s family planning policies have led to a scenario where adult children are tasked with caring for multiple aging relatives while managing their own families44. Consequently, the time and attention they can devote to their elderly parents diminish, leading to insufficient support for patients45,46. Additionally, family caregivers often experience emotional exhaustion, negatively impacting their capacity to provide necessary support to patients46,47. This emphasizes the need for targeted interventions not only for MCI patients but also for their caregivers, who are often overlooked.
In terms of work-related challenges, nurses identified several work-related challenges in MCI care, including limited knowledge of actionable interventions, insufficient training resources, and overwhelming workloads. Despite the existence of international guidelines for MCI diagnosis, care, and management, which outline the role of healthcare providers like nurses, our findings reveal a significant gap in their practical implementation3,9,33. Consistent with a Canadian research on dementia care professionals, our study found that nurses often face role ambiguity, which limits their ability to provide comprehensive support48. Similarly, a study conducted in Germany show that general practitioners struggle to recognize MCI without formal assessments21, mirroring our findings that nurses frequently rely on clinical intuition rather than standardized protocols. This reliance is compounded by the lack of structured training and systematic tools, further hindering early intervention. Additionally, nurses face difficulties in communicating with older adults—such as explaining MCI, gathering patient histories, and discussing treatment plans—highlighting systemic issues that impede effective care48,49. The increasing prevalence of multimorbidity also complicates nursing care, requiring a delicate balance between managing multiple health conditions and addressing cognitive decline. As nurses juggle numerous responsibilities, the pressure to provide comprehensive care can detract from their focus on cognitive health needs50.
In conclusion, addressing these multifaceted challenges requires a concerted effort to enhance awareness and education regarding MCI, improve support systems for families, and provide nurses with the resources and training necessary to effectively manage cognitive health in older patients. The insights gained from this study highlight the critical need for integrated approaches that prioritize both patient care and the well-being of their caregivers.
Limitations
The participants in this study were all female nurses, which may limit the generalizability of the findings and overlook potential gender-related influences on the survey results. Moreover, most participants were young nurses, with only two individuals over the age of 40, which may have influenced the perspectives captured. Older, more experienced nurses may offer different insights, and future research should include a more age-diverse sample. Additionally, although we took steps to ensure accurate translation, including review by bilingual experts, some nuanced meanings may have been lost in the process. Furthermore, the research was conducted in only three tertiary hospitals in Beijing, indicating that future studies should encompass a broader range of hospitals across different regions and levels, particularly community health service centers. Additionally, this study focused solely on the barriers to early recognition and intervention of MCI from the perspective of nurses; hence, future research should include other healthcare professionals involved in the treatment or care of MCI patients, such as geriatricians, neurologists, and staff from community and nursing homes. The perceived difficulties reported by nurses may also be influenced by the small sample size and limited coping resources. Future studies could explore alternative perspectives, including positive experiences, suggestions, and coping strategies. Employing an intersectionality framework, alongside methods such as observations, focus group discussions, and longitudinal approaches, could enhance the robustness of subsequent research.
Conclusion
This study provides valuable insights into the challenges faced by nurses in the early identification and intervention of MCI among older patients. Nurses play critical roles in facilitating early recognition, delivering interventions, and ensuring effective communication with MCI patients, their families, and other medical professionals. However, the findings reveal that nurses encounter significant obstacles, including managing patients’ complex perceptions of MCI, insufficient family involvement, overwhelming workloads, and uncertainty regarding effective coping strategies and resources for addressing cognitive decline. These findings underscore the urgent need for interventions aimed at supporting nurses in their care for patients with MCI. Enhancing nurses’ understanding of how to navigate patients’ emotional responses, fostering family engagement, and providing targeted interventions are essential. Healthcare authorities should carefully assess the work needs and appropriate workload for nurses caring for MCI patients, offering effective support through professional skills training, financial resources, and relevant materials. Additionally, policies should be formulated to enhance the availability of primary care services for patients with MCI.
Statement
The study was carried out in accordance with the Consolidated Criteria for Reporting Qualitative Research (COREQ).
Data availability
All data generated or analysed during this study are included in this article.
References
Petersen, R. C. et al. Mild cognitive impairment: clinical characterization and outcome. Arch. Neurol. 56(3), 303–308. https://doi.org/10.1001/archneur.56.3.303 (1999).
Langa, K. M. & Levine, D. A. The diagnosis and management of mild cognitive impairment: a clinical review. JAMA 312(23), 2551–2561. https://doi.org/10.1001/jama.2014.13806 (2014).
Albert, M. S. et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 7(3), 270–279. https://doi.org/10.1016/j.jalz.2011.03.008 (2011).
Gauthier, S. et al. Mild cognitive impairment. Lancet 367(9518), 1262–1270. https://doi.org/10.1016/S0140-6736(06)68542-5 (2006).
Petersen, R. C. et al. Mild cognitive impairment: a concept in evolution. J. Intern. Med. 275(3), 214–228. https://doi.org/10.1111/joim.12190 (2014).
Ismail, Z. et al. Prevalence of Depression in Patients With Mild Cognitive Impairment: A Systematic Review and Meta-analysis. Jama Psychiat. 74(1), 58–67. https://doi.org/10.1001/jamapsychiatry.2016.3162 (2017).
Eshkoor, S. A., Hamid, T. A., Mun, C. Y. & Ng, C. K. Mild cognitive impairment and its management in older people. Clin. Interv. Aging 10, 687–693. https://doi.org/10.2147/CIA.S73922 (2015).
Roberts, R. & Knopman, D. S. Classification and epidemiology of MCI. Clin. Geriatr. Med. 29(4), 753–772. https://doi.org/10.1016/j.cger.2013.07.003 (2013).
Kasper, S. et al. Management of mild cognitive impairment (MCI): The need for national and international guidelines. World J. Biol. Psychiatry 21(8), 579–594. https://doi.org/10.1080/15622975.2019.1696473 (2020).
Rodakowski, J., Saghafi, E., Butters, M. A. & Skidmore, E. R. Non-pharmacological interventions for adults with mild cognitive impairment and early stage dementia: An updated scoping review. Mol. Aspects Med. 43–44, 38–53. https://doi.org/10.1016/j.mam.2015.06.003 (2015).
Wang, C. et al. Non-pharmacological interventions for patients with mild cognitive impairment: a meta-analysis of randomized controlled trials of cognition-based and exercise interventions. J. Alzheimers Dis. 42(2), 663–678. https://doi.org/10.3233/JAD-140660 (2014).
Teixeira, C. V. et al. Non-pharmacological interventions on cognitive functions in older people with mild cognitive impairment (MCI). Arch. Gerontol. Geriatr. 54(1), 175–180. https://doi.org/10.1016/j.archger.2011.02.014 (2012).
Gavelin, H. M. et al. Combined physical and cognitive training for older adults with and without cognitive impairment: A systematic review and network meta-analysis of randomized controlled trials. Ageing Res. Rev. 66, 101232. https://doi.org/10.1016/j.arr.2020.101232 (2021).
Hong, Y. J., Jang, E. H., Hwang, J., Roh, J. H. & Lee, J. H. The Efficacy of Cognitive Intervention Programs for Mild Cognitive Impairment: A Systematic Review. Curr. Alzheimer Res. 12(6), 527–542. https://doi.org/10.2174/1567205012666150530201636 (2015).
Oh, M. W. et al. Nurse-Led Computerized Cognitive Training for Mild Cognitive Impairment: A Preliminary Study. Rehabil. Nurs. https://doi.org/10.1097/RNJ.0000000000000264 (2020).
McGrattan, A. M., McEvoy, C. T., McGuinness, B., McKinley, M. C. & Woodside, J. V. Effect of dietary interventions in mild cognitive impairment: a systematic review. Br. J. Nutr. 120(12), 1388–1405. https://doi.org/10.1017/S0007114518002945 (2018).
Whitty, E. et al. Efficacy of lifestyle and psychosocial interventions in reducing cognitive decline in older people: Systematic review. Ageing Res. Rev. 62, 101113. https://doi.org/10.1016/j.arr.2020.101113 (2020).
Etgen, T., Sander, D., Bickel, H. & Forstl, H. Mild cognitive impairment and dementia: the importance of modifiable risk factors. Dtsch. Arztebl Int. 108(44), 743–750. https://doi.org/10.3238/arztebl.2011.0743 (2011).
Xu, Z. et al. A pilot feasibility randomized controlled trial on combining mind-body physical exercise, cognitive training, and nurse-led risk factor modification to reduce cognitive decline among older adults with mild cognitive impairment in primary care. PeerJ 8, e9845. https://doi.org/10.7717/peerj.9845 (2020).
Olazaran, J. et al. Mild cognitive impairment and dementia in primary care: the value of medical history. Fam. Pract. 28(4), 385–392. https://doi.org/10.1093/fampra/cmr005 (2011).
Kaduszkiewicz, H. et al. Do general practitioners recognize mild cognitive impairment in their patients?. J. Nutr. Health Aging 14(8), 697–702. https://doi.org/10.1007/s12603-010-0038-5 (2010).
Xiao, N., Long, Q., Tang, X. & Tang, S. A community-based approach to non-communicable chronic disease management within a context of advancing universal health coverage in China: progress and challenges. BMC Public Health 14(Suppl 2), S2. https://doi.org/10.1186/1471-2458-14-S2-S2 (2014).
Wu, Q., Zhao, L. & Ye, X. C. Shortage of healthcare professionals in China. BMJ 354, i4860. https://doi.org/10.1136/bmj.i4860 (2016).
Lin, F. et al. Awareness of memory abilities in community-dwelling older adults with suspected dementia and mild cognitive impairment. Dement. Geriatr. Cogn. Disord. 30(1), 83–92. https://doi.org/10.1159/000318752 (2010).
Werner, P., Heinik, J., Giveon, S., Segel-Karpas, D. & Kitai, E. Help-seeking preferences in the area of mild cognitive impairment: comparing family physicians and the lay public. Clin. Interv. Aging 9, 613–619. https://doi.org/10.2147/CIA.S60248 (2014).
Scodellaro, C. & Pin, S. The ambiguous relationships between aging and Alzheimer’s disease: a critical literature review. Dementia (London). 12(1), 137–151. https://doi.org/10.2147/CIA.S60248 (2013).
Morris, J. L. et al. Patients’ and Family Members’ Subjective Experiences of a Diagnostic Evaluation of Mild Cognitive Impairment. J. Patient Exp. 7(1), 124–131. https://doi.org/10.1177/2374373518818204 (2020).
Carlozzi, N. E. et al. Caring for an individual with mild cognitive impairment: a qualitative perspective of health-related quality of life from caregivers. Aging Ment. Health. 22(9), 1190–1198. https://doi.org/10.1080/13607863.2017.1341468 (2018).
Kim, H., Sefcik, J. S. & Bradway, C. Characteristics of Qualitative Descriptive Studies: A Systematic Review. Res. Nurs. Health 40(1), 23–42. https://doi.org/10.1002/nur.21768 (2017).
Hsieh, H. F. & Shannon, S. E. Three approaches to qualitative content analysis. Qual. Health Res. 15(9), 1277–1288. https://doi.org/10.1177/1049732305276687 (2005).
Erlingsson, C. & Brysiewicz, P. A hands-on guide to doing content analysis. Afr. J. Emerg. Med. 7(3), 93–99. https://doi.org/10.1016/j.afjem.2017.08.001 (2017).
Petersen, R. C. Clinical practice. Mild cognitive impairment. N. Engl. J. Med. 364(23), 2227–2234. https://doi.org/10.1177/1533317518791401 (2011).
Lin, F., Vance, D. E., Gleason, C. E. & Heidrich, S. M. Caring for older adults with mild cognitive impairment: an update for nurses. J. Gerontol. Nurs. 38(12), 22–35. https://doi.org/10.3928/00989134-20121106-03 (2012).
Petersen, R. C. et al. Practice guideline update summary: Mild cognitive impairment: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology 90(3), 126–135. https://doi.org/10.1212/WNL.0000000000004826 (2018).
Gomersall, T., Smith, S. K., Blewett, C. & Astell, A. ‘It’s definitely not Alzheimer’s’: Perceived benefits and drawbacks of a mild cognitive impairment diagnosis. Br. J. Health Psychol. 22(4), 786–804. https://doi.org/10.1111/bjhp.12255 (2017).
Nogueras, D. J., Postma, J. & Van Son, C. Why didn’t I know? Perspectives from adult children of elderly parents with dementia. J. Am. Assoc. Nurse Pract. 28(12), 668–674. https://doi.org/10.1002/2327-6924.12382 (2016).
Hinton, W. L. & Levkoff, S. Constructing Alzheimer’s: narratives of lost identities, confusion and loneliness in old age. Cult. Med. Psychiatry 23(4), 453–475. https://doi.org/10.1023/a:1005516002792 (1999).
Lion, K. M. et al. Do people with dementia and mild cognitive impairments experience stigma? A cross-cultural investigation between Italy, Poland and the UK. Aging Ment. Health 24(6), 947–955. https://doi.org/10.1080/13607863.2019.1577799 (2020).
Beard, R. L. & Neary, T. M. Making sense of nonsense: experiences of mild cognitive impairment. Sociol. Health Illn. 35(1), 130–146. https://doi.org/10.1111/j.1467-9566.2012.01481.x (2013).
Werner, P. & Heinik, J. Stigma by association and Alzheimer’s disease. Aging Ment. Health 12(1), 92–99. https://doi.org/10.1080/13607860701616325 (2008).
Jolley, D. J. & Benbow, S. M. Stigma and Alzheimer’s disease: causes, consequences and a constructive approach. Int. J. Clin. Pract. 54(2), 117–119 (2000).
Bartfay, E. & Bartfay, W. J. Quality-of-life outcomes among Alzheimer’s disease family caregivers following community-based intervention. West J. Nurs. Res. 35(1), 98–116. https://doi.org/10.1177/0193945911400763 (2013).
Leung, P., Orrell, M. & Orgeta, V. Social support group interventions in people with dementia and mild cognitive impairment: a systematic review of the literature. Int. J. Geriatr. Psychiatry 30(1), 1–9. https://doi.org/10.1002/gps.4166 (2015).
Hesketh, T., Zhou, X. & Wang, Y. The End of the One-Child Policy: Lasting Implications for China. JAMA 314(24), 2619–2620. https://doi.org/10.1001/jama.2015.16279 (2015).
Yikilkan, H., Aypak, C. & Gorpelioglu, S. Depression, anxiety and quality of life in caregivers of long-term home care patients. Arch. Psychiatr. Nurs. 28(3), 193–196. https://doi.org/10.1016/j.apnu.2014.01.001 (2014).
D’Onofrio, G. et al. Caregiver burden characterization in patients with Alzheimer’s disease or vascular dementia. Int. J. Geriatr. Psychiatry 30(9), 891–899. https://doi.org/10.1002/gps.4232 (2015).
Cheng, S. T., Mak, E. P., Lau, R. W., Ng, N. S. & Lam, L. C. Voices of Alzheimer Caregivers on Positive Aspects of Caregiving. Gerontologist 56(3), 451–460. https://doi.org/10.1093/geront/gnu118 (2016).
De Witt, L. & Ploeg, J. Caring for older people living alone with dementia: Healthcare professionals’ experiences. Dementia (London) 15(2), 221–238. https://doi.org/10.1177/1471301214523280 (2016).
Gronning, H. et al. Caregiver burden and psychosocial services in patients with early and late onset Alzheimer’s disease. Dan. Med. J. 60(7), A4649 (2013).
Salisbury, C. et al. Management of multimorbidity using a patient-centred care model: a pragmatic cluster-randomised trial of the 3D approach. Lancet 392(10141), 41–50. https://doi.org/10.1016/S0140-6736(18)31308-4 (2018).
Acknowledgements
The authors are grateful to the nurses who shared their experiences, and sincerely thank the nursing administrators of the three hospitals for their support in selecting participants and data collection.
Funding
This study was supported by grants from the National Natural Science Foundation of China (72404282).
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript, approved the final version, and were accountable for all aspects of the work. Jingya Ma: conceptualization, methodology, data collection, data analysis, writing—original draft, writing—editing. Haiyan Wang: data collection, data analysis. Huan Zhang: data analysis, writing—review. Zheng Li: conceptualization, methodology, writing—review and editing, supervision, project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
Ethical approval was granted by the Ethical Committee of the School of Nursing, Peking Union Medical College (Ethics Review No. [2020]05). Informed consent was obtained from all participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, J., Wang, H., Zhang, H. et al. Nurses’ perspectives on barriers to managing risk factors for mild cognitive impairment in older adults using a qualitative descriptive approach. Sci Rep 15, 26523 (2025). https://doi.org/10.1038/s41598-025-08126-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-08126-8