Abstract
Cervical cancer remains a major public health concern in Northeast Brazil, ranking as the second most common cancer among women. This study provides the first long-term, population-based estimates of net survival from cervical cancer in Sergipe, a Brazilian state with a medium Human Development Index, using high-quality registry data subjected to rigorous quality control procedures. We analysed data for 3,977 women aged 15–99 years diagnosed with an invasive cervical cancer between 1996 and 2017 and followed up to 2022, after excluding 6,095 in situ neoplasms. Net survival was estimated using the Pohar Perme method, stratified by histological subtype and calendar period, and age-standardised with the International Cancer Survival Standard weights. We observed a substantial decline in survival over time: one-year net survival dropped from 84.6% (1996–1999) to 73.4% (2015–2017), and five-year survival from 60.8 to 49.3%. Squamous cell carcinoma and adenocarcinoma showed similar survival patterns, with five-year survival ranging from 55 to 58%. The persistent decline in net survival may reflect a shift toward more advanced or aggressive invasive cancers, as screening programmes increasingly detect and remove early-stage lesions. Delayed diagnosis and sub-optimal treatment further contribute, underscoring the need to improve screening and timely cancer care access.
Similar content being viewed by others
Introduction
Cervical cancer is the most common gynaecological cancer worldwide1. Despite the availability of preventive measures such as Human Papilloma Virus (HPV) vaccination and regular screening with the Pap smear, limited awareness of the disease and obstacles in access to health services persist, leading to ongoing disparities in the disease burden2.
Squamous cell carcinoma and adenocarcinoma are the most common histological types. Squamous cell carcinoma is characterised by slower growth. Adenocarcinoma arises from glandular cells; it tends to display a more aggressive growth pattern, and is often diagnosed at an advanced stage3,4.
Globally, cervical cancer ranks fourth in both incidence and cancer-related deaths among women, with a significant public health impact in low-income and middle-income countries1. In Brazil, the epidemiological profile of cervical cancer varies between regions. Incidence of invasive cervical cancer is higher in the North and Northeast, where there is a lower socioeconomic profile, more restricted access to health services and lower education levels5,6.
Despite a decline in cervical cancer incidence rates in the state of Sergipe7Northeast Brazil, limited access to health services and socioeconomic disparities remain as persistent barriers to effective disease control. A comprehensive understanding of the impact of this cancer is essential for the strategic planning and implementation of effective interventions.
Population-based survival analyses (net survival) are essential for evaluating the effectiveness of cancer control programmes and for informing evidence-based public health policies8,9. However, such studies are scarce in Brazil, particularly at the state level and with long-term follow-up10,11,12,13. This study addresses these gaps by presenting the first comprehensive population-based analysis of cervical cancer survival by histological subtype in Sergipe, a state in northeastern Brazil, using high-quality cancer registry data on women diagnosed between 1996 and 2017, with follow-up until 2022.
Materials and methods
This study analysed data from Sergipe, a north-eastern Brazilian state encompassing 22,000 km² and comprising 75 municipalities. According to the 2022 Census, Sergipe has a population of approximately 2.2 million. Aracaju, the state capital, and primary regional healthcare centre, has a population of 602,757.
Since 1996, Sergipe has had a Population-Based Cancer Registry in Aracaju. The Aracaju Cancer Registry is well established, with high-quality data, enabling population-based cancer studies.
We examined anonymised individual records from the Aracaju Cancer Registry for adult women (15 to 99 years) who were diagnosed with an invasive primary cervical malignancy in Sergipe State from 1 January 1996 to 31 December 2017, with follow-up for their vital status until 31 December 2022.
Cervical cancer was defined according to the International Classification of Diseases for Oncology, Third Edition (ICD-O-3), covering the endocervix (C53.0), exocervix (C53.1), overlapping lesions of the cervix uteri (C53.8), and tumours of the cervix uteri, not otherwise specified (C53.9)14. We defined histological groups based on the World Health Organization (WHO) Classification of Tumours of Female Reproductive Organs15 and ICD-O-314, as detailed in Supplementary Table 1 (S1).
The study received approval from the Research Ethics Committee of the Federal University of Sergipe (Reference 3.714.982), adhering to relevant guidelines and regulations. Databases were anonymised in accordance with Resolution number 466, 12 December 2012, from the Ministry of Health of Brazil. Due to the retrospective nature of the study, the Research Ethics Committee of the Federal University of Sergipe waived the need of obtaining informed consent.
To conduct survival analysis, passive follow-up was employed to ascertain the vital status and the date of last known vital status of each woman. Verification of the death of registered women, regardless of the cause of death, depended on accessing death records within the Sergipe Mortality Information System, which captures vital statistics at the state level.
Women whose tumour record in the Aracaju Cancer Registry did not match a corresponding death record were considered as alive on the data of study closure, 31 December 2022.
For certain cases with incomplete death information, additional details were sought from the National Registry of Deceased Persons, the Federal Revenue Service, the Brazilian Electoral System, and the National Health Registry. This was to maximise the completeness and accuracy of the data, and to minimise the potential for ‘immortal time bias,’ in which women who had died would be considered as alive if their death record had not been linked to their cancer registration, thus inflating survival estimates.
Control of data quality
The data underwent rigorous data quality control procedures as developed for the VENUSCANCER project, which is embedded in the CONCORD programme and aims to investigate global disparities in patterns of care and short-term survival from breast, cervical and ovarian cancers16.
Supplementary Table 2 (S2) outlines the criteria for the exclusion of records. Out of a total of 10,477 women registered with a cervical tumour, we excluded 255 (2.4%) records with incomplete dates and 6,095 (58.1%) records of an in situ neoplasm. Among 4,127 eligible women, we excluded a further 146 (3.5%) women whose cancer was registered only from a death certificate, and four with invalid dates. Data for the remaining 3,977 women (96.4% of those eligible) were included in survival analysis. Analysis of survival by histological group was restricted to the 3,890 tumours that were microscopically verified and had specific ICD-O-3 morphology codes (97.8% of those eligible).
Statistical analysis
The study monitored women diagnosed over a 22-year period, with annual follow-ups conducted until 31 December 2022.
The cohort approach was employed to estimate survival among women diagnosed during each of five calendar periods (1996–1999, 2000–2004, 2005–2009, 2010–2014 and 2015–2017), since at least five years of potential follow-up were available for all women at the end of 2022 (Supplementary Fig. S3).
Net survival at one and five years after cervical cancer diagnosis was estimated in each of calendar period and by histological group. We used the Pohar Perme estimator, implemented through the stns program in Stata version 1817,18.
Net survival can be interpreted as the probability for cancer patients to survive their cancer after controlling for competing risks of death (background mortality), which are higher in the elderly17. To account for background mortality, complete life tables of all-cause mortality rates by single year of age (0–99 years) among women in Sergipe were constructed for each calendar year 1996–2022, using the numbers of deaths and female population counts by five-year age group (abridged counts) and calendar year. Poisson regression and flexible functions were employed to manage the abridged data, with the age variable centred to enhance estimate stability. Mortality rates were derived using a flexible Poisson model for the years 1997, 2010 and 2018, incorporating data from three adjacent calendar years around each central year to address year-to-year variability. Interpolated data were used to bridge gaps for intermediate years, while data duplication addressed the earliest and latest years19. Mortality rates for 2019, 2020 and 2021 were individually modelled to take into account of the fluctuations arising from the impact of the COVID-19 pandemic on mortality and demographic dynamics.
Survival estimates were produced for five age groups (15–44, 45–54, 55–64, 65–74 and 75–99 years). Age-standardised estimates for all age groups combined were obtained using the International Cancer Survival Standard (ICSS) group 2 weights20appropriate for cancers for which incidence rates do not rise steeply with age.
Where age-specific survival estimates could not be generated or fewer than 10 women were available for analysis in an age group, data for adjacent age groups were merged, and the re-estimated survival was applied to both original age groups. If two or more age-specific estimates could not be produced, or fewer than 10 women were available for analysis in two or more age groups, then only the unstandardised estimate for all ages combined was reported.
Cumulative probabilities of survival were expressed as percentages, truncated within the range 0-100%. Standard errors were calculated using the Greenwood method21with 95% confidence intervals.
Results
The 15–44 age group represented the most common age at diagnosis throughout the entire period, accounting for 34.8% of cases. Of the 3,977 invasive cervical tumours, 85.1% were classified as squamous carcinomas, 10.0% as adenocarcinomas, 2.7% with other specified morphologies, and unspecified (0.9%) or unknown morphologies (1.3%) (Table 1).
The mean age at diagnosis ranged from 50.8 to 59.1 years between morphological groups. The proportion of squamous carcinomas and adenocarcinomas varied slightly with advancing age (Supplementary Tables 4 – S4).
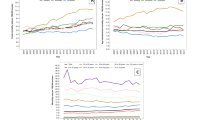
Up to one year after diagnosis, there were no notable differences in survival between age groups, but five-year net survival was higher among women aged 15–44 years (59.4%) than among women aged 75–99 years (50.9%, Table 2). Five-year survival was similar among women aged 45–54 years and 55–64 years (about 53.0%). After one year from diagnosis, survival among women aged 65–74 exceeded that of women aged 45–64 (Fig. 1). Women aged 15–44, 45–54, and 75–99 years with adenocarcinoma had higher one- and five-year survival estimates than women in the same age groups with squamous cell carcinoma (Table 3).
Over the 22-year period 1996–2017, one-year survival declined by about 10%, from 84.6% (95% CI 81.7–87.5%) in 1996–1999 to 73.4% (69.3–77.8%) in 2015–2017, while five-year survival fell from 60.8% (56.6–65.3%) in 1996–1999 to 49.1% (44.1–54.7%) in 2015–2017 (Table 4).
There was a decrease in age-standardised one-year net survival for squamous cell carcinomas, from 85.7% (95% CI 82.8–88.8%) in 1996–1999 to 74.5% (70.0-79.3%) in 2015–2017, with a corresponding decline in five-year survival from 62.5% (58.0-67.3%) to 51.3% (45.7–57.5%) over the same period. Age-standardised net survival for adenocarcinoma could only be estimated for the period 2010–2014, during which both one-year and five-year net survival surpassed those of squamous cell carcinoma. It was not possible to determine trends in age-standardised survival for other specific morphologies, because of small numbers (Fig. 2; Supplementary Tables 6 – S6).
Discussion
This study is the first to examine net survival from cervical cancer for the whole population of the state of Sergipe, Brazil. Our findings revealed a decrease of slightly more than 10% in age-standardised net survival at both one and five years after diagnosis between 1996 and 2017. Squamous cell carcinoma was the most common morphological subtype, representing around 85% of the cases. Age-standardised net survival for squamous carcinoma and adenocarcinoma was similar throughout the 22-year period.
Cervical cancer is recognised as a largely preventable disease, due to the effectiveness of primary and secondary prevention measures. However, despite these advances, disease control remains a challenge, particularly in low-income and middle-income countries, where implementation of these measures is still inequitable. This results in higher incidence and mortality rates1 and lower survival probabilities8 than in more developed nations.
In 2020, WHO launched the Global Strategy to Eliminate Cervical Cancer, establishing ambitious targets and highlighting the significance of population-based studies that focus on incidence, survival and mortality to comprehend the disease burden more fully. These research efforts inform targeted prevention and intervention strategies, with population-based net survival serving as an important metric to assess the effectiveness of healthcare systems in managing cancer22.
Population-based studies have revealed substantial global and regional disparities in cervical cancer survival. The CONCORD programme is the largest international study of cancer survival, covering 15 cancer types in adults in 71 countries and territories8. The third cycle (CONCORD-3) reported five-year net survival ranging from 50 to 70% globally for cervical cancer, with declines observed in Brazil—from 69.3% in 2000–2004 to 60.3% in 2010–2014—and similar patterns in Aracaju, the capital of Sergipe, and in other Latin American countries such as Argentina, Chile and Colombia. In contrast, Cuba experienced an increase, reaching 72.9% in 2010–2014.
The SURVCAN-3 study focused specifically on low- and middle-income countries across Africa, Asia and Latin America between 2008 and 2012, showing survival estimates around 50–60% in countries with national screening programmes (Brazil, Argentina, Chile, Colombia, Ecuador, Peru, Puerto Rico, and Uruguay), and higher estimates, approaching 70%, in Costa Rica and Cuba23.
Our findings revealed a decline in cervical cancer survival in Sergipe over the 22-year period, with five-year survival decreasing from 58.7% in 2000–2004 to 48.5% in 2010–2014. Brazil was one of the pioneering countries in the introduction of the Pap smear in the 1940s. However, coordinated efforts for cervical cancer detection only became more structured in 1995, with the implementation of the ‘Viva Mulher’ Programme. This was followed by the introduction of the Cervical Cancer Information System and the National Cervical Cancer Control Programme. The inclusion of the HPV vaccine in the National Immunisation Programme in 2014 further strengthened preventive measures. Both the HPV vaccine and Pap smears are provided free of charge through the Unified Health System (SUS)24.
Our cohort of 10,477 women with cervical tumours registered between 1996 and 2017 showed a substantial increase in the proportion of in situ tumours, rising from 34.5% in 1996–1999 to 67.8% in 2015–2017. This upward trend reflects progress in screening coverage and its role in detecting early-stage lesions. Despite a decrease in the incidence of invasive cervical cancer in Sergipe over time7we observed a decline in net survival, which may seem paradoxical at first glance.
One possible explanation is a shift in the tumour profile among invasive cancers. As screening preferentially detects and removes more indolent, slower-growing lesions in asymptomatic women, often at the pre-invasive (in situ) stage. The residual group of more biologically aggressive cancers. These may occur among women who are unscreened25, have inadequate follow-up, or develop interval cancers with rapid progression and a shorter sojourn time. This change in case-mix may contribute to the observed decline in survival, because the invasive cancers that are diagnosed clinically, in symptomatic women, tend to progress more rapidly and may have poorer prognosis, even when diagnosed early. In this context, the decline in survival does not necessarily reflect a failure of the screening programme but rather a transformation in the distribution of stage at diagnosis and in the biological aggressiveness of invasive disease within a population where screening is available. Similar patterns have been described in other settings with long-standing screening programmes, where stable or declining survival trends occurred despite reductions in incidence and mortality26,27. However, this interpretation must be considered cautiously.
Cervical cancer screening in Brazil remains largely opportunistic, particularly in less developed regions such as the Northeast24,28. National studies have shown that the majority of Brazilian women, especially in lower Human Development Index (HDI) regions, are still diagnosed at an advanced stage29and the organisation of the screening programme plays a central role in this outcome. In contrast, more structured programmes — such as those incorporating DNA–HPV testing — have demonstrated significantly higher early-stage detection and better age coverage than traditional cytology-based strategies30.
Other contributing factors, such as healthcare inequalities and delays in diagnosis and treatment, probably also play a role. Prolonged waiting times for screening and diagnostic results, coupled with delays in treatment, are significant issues28,31. Additionally, the frequent diagnosis of cervical cancer at a more advanced stage leads to poorer prognosis and lower survival32.
In less developed areas, particularly in the Northeast — the poorest region of Brazil — the lack of access to healthcare facilities, diagnostic resources, and qualified professionals, combined with funding and awareness issues, can lead to delays in diagnosis and treatment33. This adversely affects health outcomes, including survival.
The disparity in HDI across municipalities in Sergipe underscores socioeconomic and healthcare differences, with low to medium HDI levels in most areas, except for the capital, Aracaju, with a high HDI. In regions with lower HDI, inhabitants face substantial hurdles in accessing healthcare services, frequently necessitating travel to urban centres like Aracaju for diagnostic procedures and treatment. This poses a significant barrier for the most vulnerable, who encounter additional difficulties in obtaining early diagnosis and timely treatment. This directly impacts their prognosis.
Our findings align with broader evidence linking cancer survival to socioeconomic factors. A Brazilian study analysing population-based cervical cancer survival in Aracaju, Sergipe’s capital, and Curitiba (South) between 1996 and 2012 found that five-year net survival varied significantly by socioeconomic status, both within and between cities, which may be related to differences in access to screening and follow-up care12. Similarly, the SURVCAN-3 project demonstrated a strong correlation between HDI and net survival across 32 countries, with higher-HDI countries exhibiting better outcomes. Nevertheless, survival disparities persist even among countries with comparable HDI, which may be influenced by differences in healthcare system organization and effectiveness23. For instance, survival estimates vary widely—from 27.9% in Côte d’Ivoire (West Africa) to 80.2% in Mauritius (an island nation in the Indian Ocean)—highlighting how the performance of health systems influences cancer outcomes, beyond economic development alone.
These data underscore the importance of considering socioeconomic context, screening coverage, and healthcare access when interpreting survival estimates. For Sergipe and regions with similar challenges, our results indicate the need for more equitable and effective cancer control strategies, focusing on reducing barriers to early diagnosis and timely treatment to improve survival outcomes.
This study provides important population-based evidence on trends in the probability of survival from cervical cancer by the most common histological sub-types, in a setting that is characterized by health inequalities and limited access to diagnostic resources. Our findings show that age-standardised net survival was similar for squamous cell carcinoma and adenocarcinoma, with estimated survival of approximately 80% at one year and 55–58% at five years post-diagnosis.
Recent advances in cervical cancer classification, particularly regarding adenocarcinomas, emphasize the prognostic relevance of HPV association, as reflected in the updated WHO guidelines and recent literature15,34,35. These developments have refined the understanding of the prognosis of adenocarcinoma, suggesting that HPV-associated adenocarcinomas may have outcomes similar to squamous cell carcinomas.
Nonetheless, our study remains highly relevant as it relies on long-term population-based data from Sergipe, where data on HPV status were not routinely available during the period 1996–2017. Thus, our results reflect survival patterns in a middle-income context with structural inequalities in healthcare access and diagnostic capabilities.
This contrasts with findings from high-income settings such as Sweden, where a nationwide study reported 5-year net survival estimates of at least 80% for early-stage (I–II) squamous cell carcinoma and adenocarcinoma by 2014, while survival for advanced stages (III–IV) improved for squamous cell carcinoma, but remained low for adenocarcinoma36. In our study, five-year net survival for women with squamous cell carcinoma declined over the 22-year period. However, due to limited data availability, we were unable to evaluate whether this decline was associated with changes in stage at diagnosis, further underscoring the need for improved cancer surveillance systems.
Therefore, despite advances in tumour classification and improved survival in high-resource settings, population-based studies in regions facing healthcare disparities remain essential to understand the real-world burden of cervical cancer and to guide context-specific public health strategies aimed at improving early detection, treatment access and thus in patient outcomes.
Conclusions
Our study reveals a decline in one-year and five-year survival among women diagnosed with invasive cervical cancer in Sergipe between 1996 and 2017, reflecting both improvements in early detection through the screening programme and ongoing challenges in managing more aggressive tumours not captured by screening. Notably, squamous cell carcinoma, the most common histological subtype, experienced a marked decrease in survival during this period. Survival probabilities for squamous cell carcinoma and adenocarcinoma were comparable, indicating that difficulties in cervical cancer management affect all histological subtypes alike. These findings underscore the urgent need for comprehensive public health interventions to improve timely diagnosis, access to effective treatment, and overall care for women affected by cervical cancer.
Although age standardisation was not feasible for some analyses, and survival by stage at diagnosis could not be assessed due to limited data availability, this study provides a comprehensive, real-world picture of invasive cervical cancer survival over a 22-year period. The use of high-quality data from the Aracaju Cancer Registry, combined with rigorous quality control and sound methodological approaches, supports the reliability and relevance of our findings. Moreover, these analyses are similar to those in populations with similar HDI levels, thus broadening the understanding of cervical cancer survival in comparable socio-economic settings.
Future research should prioritise enhancing data completeness, particularly regarding stage at diagnosis, and focus on interventions aimed at reducing survival disparities and improving the management of more advanced disease and more aggressive tumour types.
Data availability
The findings of this study are based on data from the Aracaju Cancer Registry, which is part of the Sergipe State Health Department. Access to these data requires authorisation from both the registry coordinator and the Sergipe State Health Department. Researchers interested in accessing the data should contact Dr Carlos Anselmo Lima at regcan.ara@gmail.com. All requests must adhere to established protocols to ensure data security and participant privacy.
References
Ferlay, J. et al. Global Cancer Observatory: Cancer Today 2022. https://gco.iarc.who.int/today (2024).
eClinicalMedicine. Global strategy to eliminate cervical cancer as a public health problem: are we on track? eClinicalMedicine 55. (2023).
Waggoner, S. E. Cervical cancer. Lancet 361, 2217–2225 (2003).
Galic, V. et al. Prognostic significance of adenocarcinoma histology in women with cervical cancer. Gynecol. Oncol. 125, 287–291 (2012).
INCA. Estimativa 2023: Incidência De Câncer No Brasil (Instituto Nacional De Câncer, 2023).
Ministério da Saúde. Vigitel Brasil 2021: Estimativas Sobre Frequência E Distribuição Sociodemográfica De Fatores De Risco E Proteção Para Doenças Crônicas Nas Capitais Dos 26 Estados Brasileiros E No Distrito Federal Em 2021 (Ministério da Saúde, 2022).
da Silva, B. E. B. et al. Gynaecological cancer incidence and mortality trends in a Brazilian state with medium human development index: A 22-year analysis. Cancer Epidemiol. 88, 102493 (2024).
Allemani, C. et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391, 1023–1075 (2018).
Coleman, M. P. Cancer survival: global surveillance will stimulate health policy and improve equity. Lancet 383, 564–573 (2014).
Mafra, A. et al. Cancer survival in the Northwestern of São Paulo state, brazil: A population-based study. Cancer Epidemiol. 83, 102339 (2023).
Renna Junior, N. L., Lima, C. A., Laporte, C. A. & Coleman, M. P. Azevedo e silva, G. Ethnic, Racial and socioeconomic disparities in breast cancer survival in two Brazilian capitals between 1996 and 2012. Cancer Epidemiol. 75, 102048 (2021).
Renna Junior, N. L., Azevedo, E. & de Silva, G. Socioeconomic status and cancer survival in brazil: analysis of population data from the municipalities of Aracaju and curitiba, 1996–2012. Cancer Epidemiol. 85, 102394 (2023).
da Silva, B. E. B. et al. Trends in ovarian cancer net survival in a Northeastern Brazilian state (1996–2017). Cancer Epidemiol. 94, 102720 (2024).
Fritz, A. et al. International classification of diseases for oncology (ICD-O), 3rd ed. https://apps.who.int/iris/handle/10665/42344 (2000).
Höhn, A. K. et al. 2020 WHO classification of female genital tumors. Geburtshilfe Frauenheilkd 81, 1145–1153 (2021).
Allemani, C. Women’s cancers: do variations in patterns of care explain the worldwide inequalities in survival and avoidable premature deaths? The VENUSCANCER project. In: Lodge M, editor. Cancer control: cancer care in emerging health systems 34–39 (Brussels: International Network for Cancer Treatment and Research, 2021).
Perme, M. P., Stare, J. & Estève, J. On Estimation in relative survival. Biometrics 68, 113–120 (2012).
Clerc-Urmès, I., Grzebyk, M. & Hédelin, G. Net survival Estimation with Stns. Stata J. 14, 87–102 (2014).
Spika, D. et al. Life tables for global surveillance of cancer survival (the CONCORD programme): data sources and methods. BMC Cancer. 17, 159 (2017).
Corazziari, I., Quinn, M. & Capocaccia, R. Standard cancer patient population for age standardising survival ratios. Eur. J. Cancer. 40, 2307–2316 (2004).
Greenwood, M. The errors of sampling of the survivorship table. Reports Public Health Med. Subjects 33, (1926).
World Health Organization. Global Strategy To Accelerate the Elimination of Cervical Cancer as a Public Health Problem (World Health Organization, 2020).
Soerjomataram, I. et al. Cancer survival in africa, central and South america, and Asia (SURVCAN-3): a population-based benchmarking study in 32 countries. Lancet Oncol. 24, 22–32 (2023).
Instituto Nacional do Câncer (INCA). Diretrizes Brasileiras Para O Rastreamento Do Câncer Do Colo Do Útero (Ministério da Saúde, 2016).
Leyden, W. A. et al. Cervical cancer in women with comprehensive health care access: attributable factors in the screening process. J. Natl. Cancer Inst. 97, 675–683 (2005).
Bielska-Lasota, M., Inghelmann, R., Van De Poll-Franse, L. & Capocaccia, R. Trends in cervical cancer survival in europe, 1983–1994: A population-based study. Gynecol. Oncol. 105, 609–619 (2007).
Benard, V. B. et al. Cervical cancer survival in the united States by race and stage (2001–2009): findings from the CONCORD-2 study. Cancer 123 (Suppl 24), 5119–5137 (2017).
Instituto Brasileiro de Geografia e Estatística. Pesquisa Nacional de Saúde 2019: Percepção Do Estado de Saúde, Estilos de Vida, Doenças Crônicas e Saúde Bucal: Brasil e Grandes Regiões 113. (2020).
Vale, D. B. et al. Level of human development is associated with cervical cancer stage at diagnosis. J. Obstet. Gynaecol. 39, 86–90 (2019).
Teixeira, J. C. et al. Organization of cervical cancer screening with DNA–HPV testing impact on early–stage cancer detection: a population–based demonstration study in a Brazilian City. Lancet Reg. Health - Americas. 5, 100084 (2022).
Silva, G. A. E. et al. Evaluation of cervical cancer control actions within Brazil and its regions based on data recorded in the Brazilian unified National health system. Cad Saúde Pública. 38, e00041722 (2022).
Rodrigues, A. N. et al. Characteristics of patients diagnosed with cervical cancer in brazil: preliminary results of the prospective cohort EVITA study (EVA001/LACOG 0215). Int. J. Gynecol. Cancer. 32, 141–146 (2022).
Galvão, J. R., Almeida, P. F. D., Santos, A. M. D. & Bousquat, A. Percursos e obstáculos Na Rede de Atenção à Saúde: trajetórias assistenciais de mulheres Em Região de Saúde do Nordeste Brasileiro. Cad Saúde Pública. 35, e00004119 (2019).
Stolnicu, S. et al. Clinical outcomes of HPV-associated and unassociated endocervical adenocarcinomas categorized by the international endocervical adenocarcinoma criteria and classification (IECC). Am. J. Surg. Pathol. 43, 466–474 (2019).
Carvalho, C. F. et al. Prognosis determination of endocervical adenocarcinomas morphologically reclassified as HPV associated or HPV independent. Int. J. Gynaecol. Obstet. 160, 993–1000 (2023).
Sundqvist, A., Moberg, L., Dickman, P. W., Högberg, T. & Borgfeldt, C. Time trends for incidence and net survival of cervical Cancer in Sweden 1960-2014-A nationwide Population-Based study. Cancer Epidemiol. Biomarkers Prev. 31, 1572–1581 (2022).
Acknowledgements
We would like to acknowledge the invaluable support of the professionals at the Aracaju Cancer Registry (José Erinaldo L. de Oliveira, Elma Oliveira, Maria das Graças P. França, Sueli Vieira, Marina Kobilsek, Maria Cristina Santos, Maria das Graças Melo, Josiane Alves, Amanda Gonzaga, Alneide Leite, and Cecília Ferreira) for their significant contributions to the data collection and the preparation of the database for this research.
Funding
This study was partially funded by the Brazilian National Council for Scientific and Technological Development (CNPq), through the Split Fellowship Programme (grant 200465/2022-8). Author B.E.B. da Silva received research support from this programme.
Author information
Authors and Affiliations
Contributions
B.E.B. da Silva: Conceptualisation, Methodology, Data Curation, Validation, Formal Analysis, Visualization, Writing – Original Draft, Writing – Review & Editing. V. Di Carlo: Methodology, Data Curation, Validation, Formal Analysis, Writing – Review & Editing. P. Minicozzi: Methodology, Data Curation, Validation, Formal Analysis, Writing – Review & Editing. N. Ssenyonga: Methodology, Data Curation, Formal Analysis, Writing – Review & Editing. F. Khan Baloch: Methodology, Data Curation, Formal Analysis, Writing – Review & Editing. M. Matz: Methodology, Data Curation, Formal Analysis, Writing – Review & Editing. M. P. Coleman: Conceptualisation, Methodology, Data Curation, Formal Analysis, Supervision, Writing – Review & Editing. C. Allemani: Conceptualisation, Methodology, Data Curation, Formal Analysis, Supervision, Writing – Review & Editing. C.A. Lima: Conceptualization, Methodology, Acquisition of data, Analysis and interpretation, Writing – review & editing, Supervision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the Research Ethics Committee of the Federal University of Sergipe (Reference 3.714.982) and was conducted in compliance with all applicable ethical guidelines and regulations.
Consent to participate
As the data used in this study were anonymised and accessed through secondary sources, informed consent was waived for participants, in accordance with Brazilian Ministry of Health Resolution 466/2012.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
da Silva, B.E.B., Di Carlo, V., Minicozzi, P. et al. Trends in net survival from cervical cancer in a Brazilian state with medium Human Development Index. Sci Rep 15, 25106 (2025). https://doi.org/10.1038/s41598-025-10659-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-10659-x