Abstract
To develop a predictive model based on the perioperative plasma concentration of amino-terminal pro-brain natriuretic peptide (NT-pro BNP) in elderly patients to assess the risk of severe postoperative complications. Elderly patients (age ≥ 65 years) enrolled in this prospective observational study underwent general surgery. Plasma NT-Pro BNP concentration was measured before surgery and 2 h after surgery. Univariate and multivariate logistic regression analyses were used to identify the significant predictors. To evaluate the model performance, we applied the receiver operating characteristic (ROC) curve, Hosmer–Lemeshow test, and decision curve analysis (DCA) to evaluate the net clinical benefit. Prediction model was visualised by drawing nomogram and establishing web calculator. A total of 174 elderly patients were enrolled; 15 patients (8.6%) developed severe complications. The area under the ROC curve, sensitivity, and specificity of the two prediction models were 0.899 (95% CI 0.845–0.940), 86.67%, 91.82%, 0.956 (95% CI 0.902–0.985), 100%, and 81.42%, respectively. The net benefit of the post-model was higher than pre-model. We established two postoperative severe complication assessment models based on perioperative NT-Pro BNP levels for elderly patients with reliable accuracy. The nomogram and web calculator will be easy to use by clinicians and other researchers.
Clinical significance: The biomarker, NT-pro BNP seem to correlate with some postoperative complications, however no studies have evaluated its relationship with severe postoperative complications in elderly patients. In this study, we evaluated the relationship between NT-pro BNP and severe postoperative complications in elderly patients, and established a prediction model and a web calculator based on the prediction model. Clinicians can easily use this prediction model to identify high-risk patients at an early stage.
Similar content being viewed by others
Introduction
According to the survey results of the Chinese Ministry of Health, the elderly population aged 65 years and above accounted for 12.6% of the total population in 2019, and the proportion of the elderly population continues to rise compared with 20181,2. Some studies have predicted that the elderly population in China will exceed 25.8% by 20503,4. With the ageing population, many elderly patients are undergoing surgery and anaesthesia. The increased risk of postoperative pulmonary complications, major cardiovascular adverse events, and death in elderly patients is 3.9 times, 5.5 times, and 9 times compared to that in patients under 50 years of age2.
Elderly patients are usually complicated with heart, brain, and other systemic diseases, and the risk of postoperative complications is much higher than that in adult patients of other ages. In particular, serious postoperative complications increase mortality, length of stay, hospitalisation costs, and reduce quality of life. Existing risk stratification tools for postoperative adverse events mainly rely on doctors’ skills, experience, and subjective judgment. Therefore, there is an urgent need for an early, rapid, and objective postoperative complication risk assessment tool that reflects the effects of surgery and anaesthesia.
Brain natriuretic peptide (BNP) and amino-terminal pro-brain natriuretic peptide (NT-Pro BNP) are members of the natriuretic peptide family. They are synthesised and released by cardiac myocytes in response to various stimuli, including myocardial extension, ischaemia, and fibrosis, and inflammation caused by volume expansion and pressure overload5,6. In recent years, BNP/NT-Pro BNP target-guided therapy and its predictive value have attracted considerable attention7,8,9,10.
Perioperative monitoring of plasma BNP/NT-Pro BNP concentration can assess the patients’ preoperative circulation and cardiac function status7 and predict the occurrence of postoperative cardiopulmonary complications. Hara et al.11 showed that a high preoperative NT-Pro BNP level is a risk factor for postoperative complications in thoracic surgery. In addition, if the NT-Pro BNP level continues to rise within five days after surgery, the risk of early postoperative complications and long-term complications is significantly increased. Brandstrup et al.12 found that in colorectal resection patients, the serum NT-pro BNP level was correlated with the amount of fluid treatment, and the increase in fluid amount led to an increase in NT-pro BNP concentration. Therefore, NT-pro BNP may be a potentially effective biomarker for predicting severe postoperative complications, especially in elderly patients, and is expected to provide a new prediction tool for severe postoperative complications.
Method
Study design and approval
The ethics committee of West China Hospital of Sichuan University (No. 2020(155)) approved this single-centre, prospective observational study, and it was registered on chictr.org.cn (ChiCTR1900026223) before starting this trial. This prospective study recruited all elderly patients who planned to undergo general surgery (level 4) from June 2020 to October 2020 at the West China Hospital of Sichuan University. All methods were performed in accordance with the relevant guidelines and regulations, including the Declaration of Helsinki and institutional ethical requirements.
The eligibility criteria were as follows: (1) age ≥ 65 years; (2) ASA classification of I–III; (3) general surgery was planned; (4) general anaesthesia was intended; and (5) the level of surgery was four. The exclusion criteria were: (1) Patients with mental illness, hearing impairment, and language impairment; (2) age ≤ 65 years; (3) scheduled cardiac surgery; (4) organ transplant surgery; and (5) surgery lasting less than 2 h.
Measurement of NT-pro BNP
For 2 h before surgery, the investigator evaluated the patients in the anaesthesia preparation room according to the admission criteria. If the patients met the inclusion criteria, they were fully informed of the clinical trial process and related risks. After obtaining informed consent from the patient, informed consent was obtained from the clinical trial. A trained nurse collected two millilitres of venous blood from the peripheral veins. Blood samples were analysed using NT-Pro BNP real-time detection equipment (FS-205 dry fluorescence immunoassay analyser, Guangzhou Wanfu Biotechnology CO., LTD., Guangzhou, China).
The end of the surgical skin suture was defined as the end of the surgery. For 2 h after surgery, 2 ml of peripheral venous blood was collected by a trained nurse. Real-time detection equipment was used to detect and record the concentration of NT-Pro BNP in the sample.
All participants received the same surgical technique and anaesthesia management protocols that our hospital previously developed. No additional intervention was performed.
Outcomes and data collection
The outcome was severe postoperative complications, defined as Clavien-Dindo Classification (CDC) ≥ Grade III. All postoperative complications were graded according to the CDC system13. Grade I: Any deviation from the normal postoperative course without the need for pharmacological treatment or surgical, endoscopic, or radiological intervention. Allowed therapeutic regimens include antiemetics, antipyretics, analgesics, diuretic electrolytes, and physiotherapy. This grade also included wound infections that occurred at the bedside. Grade II: Requires pharmacological treatment with drugs other than those allowed for grade I complications. Blood transfusions and total parenteral nutrition were also administered. Grade III: Requires surgical, endoscopic, or radiological intervention. Grade IIIa: Intervention not under general anaesthesia. Grade IIIb: Intervention under general anaesthesia. Grade IV: Life-threatening complications (including central nervous system complications) require intermediate or intensive care unit management. Grade IVa: single-organ dysfunction (including dialysis). Grade IVb: Multi-organ dysfunction. Grade V: Death of a patient.
After patients were enrolled, we collected their demographic information, preoperative vital signs and comorbidities, American Society of Anaesthesiologists (ASA) classification, operation type and time, anaesthesia time, intraoperative fluid infusion type, and volume. Details of the variables included in this study are listed in Supplementary Table S1. All patients were followed-up for 30 days after surgery. Postoperative complications such as cardiovascular events, postoperative cognitive impairment, acute kidney injury, pulmonary complications, anaemia, and death were recorded (Supplementary Table S2).
Statistical analysis
The Kolmogorov–Smirnov test evaluated whether the data followed a normal distribution. For normal data, a t-test was used to determine differences; non-normal data were analysed using the Mann–Whitney U test. The Pearson test was performed to calculate the correlation for normal data, whereas the Spearman test was performed for non-normal data.
Univariate logistic regression was used to screen potential variables with a P value ≤ 0.1. Variables with a P value < 0.05 and clinically significant variables without statistical significance were included in the multivariate logistic regression model, which was used to develop the prediction model. The variance inflation factor (VIF) was calculated to identify multicollinearity. Strongly correlated variables were excluded based on the correlation coefficient between different variables, VIF values, and specialised knowledge. The receiver operating characteristic (ROC) curves and the area under the curve (AUC) of the ROC values were used to evaluate the discriminative ability of the model. The Hosmer–Lemeshow test was used to evaluate the calibration degree of the model. Decision curve analysis (DCA) evaluated the clinical net benefit obtained using the predictive model14,15. A nomogram was drawn, and a web calculator was established to visualise the predictive model16.
Statistical analysis was performed using R software (version 4.0.5), IBM SPSS statistics (version 24.0), and MedCalc Statistical Software Version 19.0.7 (MedCalc Software BVBA, Ostend, Belgium).
Sample size
In this study, MedCalc was used to estimate the sample size, and the AUC was assumed to be 0.7 with α and power (1 − β) equal to 0.05 and 0.9, respectively. The incidence of serious complications was hypothesised to be 9%. The final sample size required 182 cases, with an expected loss rate of 10%.
Results
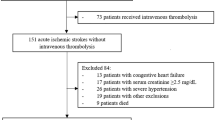
A total of 256 patients were recruited, of which 59 did not meet the inclusion criteria, 14 were excluded, and nine dropped out (five cases with an operation duration of less than 2 h, two cases lost to follow-up, and two cases dropped out halfway). In total, 174 patients were included in the final analysis (Fig. 1). Demographic information and preoperative comorbidities are shown in Table 1; 56 (32.2%) women and 118 (67.8%) men were included, and the median age of the patients was 70 (range 67–75). A total of fifteen patients (8.6%) had postoperative complications of CDC grade ≥ 3, three patients (1.7%) died, eight patients (4.6%) developed acute kidney injury (AKI), and 22 patients (12.6%) developed pulmonary complications. The median of NT-Pro BNP was 198.8 pg/ml before surgery, and the median of NT-Pro BNP was 187.45 pg/ml at 2 h after surgery (Supplementary Table S1).
Correlation analysis
The Spearman correlation test was used to calculate NT-Pro BNP levels before surgery and NT-Pro BNP levels 2 h after surgery with preoperative, intraoperative, and postoperative variables. Preoperative NT-Pro BNP level and age (r = 0.24, P = 0.001), preoperative coronary heart disease (r = 0.15, P = 0.047), intraoperative blood transfusion (r = 0.32, P < 0.001), serious postoperative complications (r = 0.38, P < 0.001), postoperative hospital stay (r = 0.17, P = 0.025), ICU stay (r = 0.32, P < 0.001), postoperative pulmonary complications (r = 0.27, P < 0.001), and postoperative major cardiovascular events (r = 0.27, P = 0.034) were significantly correlated. NT-Pro BNP levels at 2 h after surgery were significantly correlated with age (r = 0.22, P = 0.015), sex (r = − 0.20, P = 0.032), preoperative coronary heart disease (r = 0.24, P = 0.009), intraoperative blood transfusion (r = 0.29, P = 0.001), serious postoperative complications (r = 0.31, P < 0.001), ICU stay (r = 0.25, P = 0.006), and postoperative pulmonary complications (r = 0.27, P = 0.003) (Supplementary Table S2). There was no significant correlation between NT-Pro BNP level before surgery or 2 h after surgery and height, weight, ASA grade, anaesthesia time, operation time, and intraoperative fluid volume.
Difference analysis
Mann–Whitney U test showed that the preoperative median NT-Pro BNP level was 500.6 pg/ml in the severe complications group and 186.5 pg/ml in the non-occurrence group, U = 257.0, P < 0.001. The median NT-Pro BNP level at 2 h after surgery was 429.3 pg/ml in the group with serious complications and 182.8 pg/ml in the group without serious complications, U = 90.0, P = 0.001. The preoperative and postoperative NT-Pro BNP levels in the group with serious complications were significantly higher than those in the group without serious complications.
Development of predictive model
Univariate logistic regression analysis was used to screen variables, and variables with P ≤ 0.1, considered potential predictors, were incorporated into multivariate logistic regression. The backward step method was used in the multivariate logistic regression, and variables with P value < 0.05 were regarded as statistically significant. Variables with no statistical significance but significant clinical significance were also included in the final prediction model.
Univariate logistic regression (Table 2) showed variables with P ≤ 0.1 including preoperative NT-Pro BNP, postoperative NT-Pro BNP, age, ASA classification, body weight, anaesthesia time, operation time, intraoperative fluid volume, intraoperative blood transfusion volume, and intraoperative crystal volume. Using multivariate logistic regression (Table 2), we developed two predictive models based on preoperative and postoperative NT-Pro BNP levels. Variables in the model based on preoperative NT-Pro BNP levels (pre-model) included age, weight, anaesthesia time, and preoperative NT-Pro BNP concentration. ASA classification was considered a variable with no statistical significance but clinical significance and was incorporated into the pre-model. Variables in the model based on postoperative NT-Pro BNP levels (post-model) included weight and postoperative NT-Pro BNP concentration. The ASA classification was also considered a clinically significant variable and was incorporated into the post-model.
The ROC curve of the pre-model identified an AUC of 0.899, Yoden index of 0.78, sensitivity of 0.87, and a specificity of 0.92. The Hosmer–Lemeshow test showed that the chi-square value was 8.3, P = 0.403, demonstrating that the prediction model had a good calibration degree. The negative and positive predictions accuracies were 0.98 and 0.33, and the overall accuracy was 0.93 (Table 3). The VIF of all variables included in the pre-model was less than 5, indicating that the variables were independent of each other and had no collinearity. For the post-model, the AUC was 0.956, and the Yoden index was 0.814. The sensitivity and specificity were 1 and 0.81, respectively. The Hosmer–Lemeshow test showed that the Chi-square value was 8 (P = 0.996), demonstrating that the prediction model had a good calibration degree. The accuracy of negative and positive predictions were 0.99 and 0.57, and the overall accuracy was 0.97 (Table 3). The VIF showed that the variables were independent of each other and had no collinearity. DCA demonstrated that the pre-model achieved a higher clinical net benefit under a decision threshold probability lower than 0.3 compared to the post-model. In contrast, the post-model had a higher clinical net benefit when the decision threshold probability was greater than 0.3 (Fig. 2).
The result of DCA between Pre-model and Post-model. The sloping thin grey line is the net benefit of treating all men whether or not undergoing postoperative severe complication; the green line is the net benefit of treating men on the predicting of the Pre-model; the red line is the net benefit of treating men on the predicting of Post-model; the horizontal thick black line is the net benefit of treating no man. The DCA demonstrated that the Pre-model achieved higher clinical net benefit under the decision threshold probability lower than 0.3 compared to Post-model. In contrast, Post-model had a higher clinical net benefit when the decision threshold probability was greater than 0.3. DCA: decision curve analysis; NT-Pro BNP: N-terminal pro-B-type natriuretic peptide; Pre-model: the model based on preoperative NT-Pro BNP; Post-model: the model based on postoperative NT-Pro BNP.
Finally, we visualised the two predictive models by drawing nomograms and establishing a web calculator (pre-model: https://zhuyihao.shinyapps.io/DynNomappPRE/; post-model: https://zhuyihao.shinyapps.io/dynnomapp/), to estimate individual probabilities of severe postoperative complications during hospitalisation for older patients undergoing general surgery (pre-model: Fig. 3; post-model: Fig. 4).
Nomogram (A) and ROC (B) of Pre-model and the web calculator (C). A: Through drawing a vertical line from corresponding variable to the top line (Points), the score of every variable and total score can be got. The predicted probability can be obtain by drawing a vertical line form the total points line to the bottom risk line. C In the web calculator developed by us, directly input the value of the corresponding variable on the left side, the result of prediction probability and 95% confidence interval will be output on the right side. ROC: receiver operating characteristic curve; ASA-PS: American Society of Anesthesiologists Physical Status; NT-Pro BNP: N-terminal pro-B-type natriuretic peptide; Pre-model: the model based on preoperative NT-Pro BNP.
Nomogram (A) and ROC (B) of Pre-model and the web calculator (C). A: Through drawing a vertical line from corresponding variable to the top line (Points line), the score of every variable and total score can be got. The predicted probability can be obtain by drawing a vertical line form the total points line to the bottom risk line. C: In the web calculator developed by us, directly input the value of the corresponding variable on the left side, the result of prediction probability and 95% confidence interval will be output on the right side. ROC: receiver operating characteristic curve; ASA-PS: American Society of Anesthesiologists Physical Status; NT-Pro BNP: N-terminal pro-B-type natriuretic peptide; Post-model: the model based on postoperative NT-Pro BNP.
Discussion
We developed two prediction models based on perioperative NT-Pro BNP levels. We found that ASA classification, age, weight, and anaesthesia time were significant predictors of severe postoperative complications in elderly patients. The AUC value showed a good discriminative ability of the two models, and the post-model was better than the pre-model. DCA identified that the post-model had more net benefits compared to the pre-model. All results revealed that perioperative NT-Pro BNP concentration is an important biomarker for predicting serious postoperative complications.
The present study showed that the cut-off values of preoperative NT-Pro BNP and postoperative NT-Pro BNP were 348.3 pg/ml and 339.5 pg/ml, respectively. Feringa and colleagues17 suggested that preoperative NT-Pro BNP level was an important predictor of mortality 6 months after non-cardiac aortic surgery. Its cut-off value was 319 pg/ml, which is consistent with our study. The AUC of the pre-model was 0.892 in our study, while the AUC in the study by Feringa and colleagues17 was 0.73, which may be due to serious complications being a composite outcome, and the participants in the present study were all elderly. The addition of other predictors incorporated into our models, such as age and ASA classification, may increase the predictive ability of our model. Wijeysundera et al.18 stratified the risk of postoperative prognosis by preoperative NT-Pro BNP levels. The results showed that the predictive value of preoperative NT-Pro BNP was the same as the value of activity tolerance. In the present study, the predictive ability of preoperative NT-Pro BNP level was consistent with the results of Wijeysundera et al.18. In addition, our research revealed that the predictive ability of postoperative NT-Pro BNP levels was higher than that of preoperative NT-Pro BNP levels.
In this study, the perioperative NT-Pro BNP level in the group with serious complications was considerably higher than that without serious complications. Eggers et al.19 proved by continuous measurement of NT-Pro BNP levels that the elderly with increased NT-Pro BNP levels have a higher risk of all-cause mortality, and high NT-Pro BNP levels may dynamically reflect risk. Our research also proved that the post-model (based on postoperative NT-Pro BNP) had better predictive ability than the pre-model (based on preoperative NT-Pro BNP). Thus, the continuous monitoring of NT-Pro BNP levels may be of great significance. For patients with high preoperative risk who cannot postpone surgery, the measurement of postoperative NT-Pro BNP may be helpful to achieve accurate early warning and guide clinical decisions.
In univariate logistic regression, the amount of fluid infusion, blood transfusion, anaesthesia time, and operation time were risk factors for postoperative complications, and anaesthesia time was an independent risk factor for postoperative complications. However, in the post-model, these were no independent risk factors. Brandstrup et al.12 proposed that NT-Pro BNP levels were positively correlated with intraoperative fluid volume, and intraoperative infusion volume was related to postoperative cardiopulmonary complications. Therefore, postoperative NT-Pro BNP concentration may respond to risks such as surgery, anaesthesia, and infusion volume. It can more accurately reflect the risk of postoperative complications.
Nomograms and web calculators are popular methods for visualising predictive models. They are simple and easy to apply in practice. The score of every variable was obtained by drawing a vertical line from the corresponding variable to the top line. The total score is the sum of the scores for each variable. We can then obtain the predicted probability by drawing a vertical line from the total score to the bottom risk line. For a web calculator, the user only needs to enter the value of the corresponding variable, and the predicted probability and risk are directly calculated and displayed. In addition, this study was the first to evaluate the ability of perioperative NT-Pro BNP to predict severe postoperative complications in elderly patients, and the results indicated that it might be a great biomarker of potential value.
This study has some limitations. First, the sample size included in this study was only 174, and external data was not used for external validation; therefore, the internal accuracy of the model may be high, while the external authenticity may be reduced. Second, we only used univariate logistic regression to screen variables. Sensitivity analysis was not conducted in this study; therefore, the results may not be sufficiently robust. A sensitivity analysis will be included in subsequent studies. Thirdly, only one biomarker, NT-Pro BNP, was investigated in this study, and other related serum markers, such as C-reactive protein, troponin T and myohaemoglobin, were not analysed. Troponin T is also a well-established indicator of myocardial injury and has demonstrated significant prognostic value in perioperative settings20. Its inclusion might have provided additional insight into the cardiovascular risk of surgical patients. Future studies incorporating both NT-Pro BNP and Troponin T may offer a more comprehensive evaluation of cardiac risk and improve the predictive accuracy of postoperative complications. Another limitation of this study is the fixed timing of blood sampling. While the 2-h preoperative sampling reflects a practical and clinically stable period, earlier sampling points, such as 12 or 24 h prior to surgery, may provide a purer baseline, unaffected by fasting, premedication, or procedural stress. Future studies could explore more flexible or earlier sampling strategies, which may benefit to potentially improving the predictive accuracy of NT-Pro BNP.
Conclusions
Two postoperative severe complication assessment models based on perioperative NT-Pro BNP for elderly patients with reliable accuracy were established to achieve preoperative risk stratification and timely warning, provide guidance for early postoperative intervention to reduce the incidence of severe postoperative complications, and improve perioperative medical quality. The nomogram and web calculator based on the model developed by us are easy to use by clinicians and other researchers.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Shi, X. M. Research progress in geriatric epidemiology in China. Zhonghua Liu Xing Bing Xue Za Zhi 42(10), 1713–1721 (2021).
Shi, X. M. Key public health challenges of the Chinese elderly in a new situation. Zhonghua Yi Xue Za Zhi 101(44), 3613–3619 (2021).
Deng, Y. et al. The prevalence of mild cognitive impairment among Chinese people: A meta-analysis. Neuroepidemiology 55(2), 79–91 (2021).
Ma, L., Chhetri, J. K. & Chan, P. Frailty in China: From research to practice. J. Nutr. Health Aging 25(4), 479–483 (2021).
Sabatine, M. S. et al. Acute changes in circulating natriuretic peptide levels in relation to myocardial ischemia. J. Am. Coll. Cardiol. 44(10), 1988–1995 (2004).
Phelan, D. et al. Modest elevation in BNP in asymptomatic hypertensive patients reflects sub-clinical cardiac remodeling, inflammation and extracellular matrix changes. PLoS ONE 7(11), e49259 (2012).
De Vecchis, R., Esposito, C. & Cantatrione, S. Natriuretic peptide-guided therapy. Herz 38(6), 618–628 (2013).
McLellan, J. et al. Natriuretic peptide-guided treatment for heart failure: A systematic review and meta-analysis. BMJ Evid. Based Med. 25(1), 33–37 (2020).
Rezapour, A., Palmer, A. J., Alipour, V., Hajahmadi, M. & Jafari, A. The cost-effectiveness of B-type natriuretic peptide-guided care in compared to standard clinical assessment in outpatients with heart failure in Tehran Iran. Cost Eff. Resour. Alloc. 19(1), 1–6 (2021).
Zusli, S. et al. Point of care with serial NT-proBNP measurement in patients with acute decompensated heart failure as a therapy-monitoring during hospitalization (POC-HF): Study protocol of a prospective, unblinded, randomized, controlled pilot trial. Contemp. CLIN. Trials Commun. 23(1), 23–29 (2021).
Hara, K. et al. Relationship between perioperative N-terminal pro-brain natriuretic peptide (NT-proBNP) and complications in thoracic surgery. Open J. Thorac. Surg. 8(2), 29–36 (2018).
Brandstrup, B. et al. The influence of perioperative fluid therapy on N-terminal-pro-brain natriuretic peptide and the association with heart and lung complications in patients undergoing colorectal surgery: Secondary results of a clinical randomized assessor-blinded multicenter trial. Ann. Surg. 272(6), 941–949 (2019).
Dindo, D., Demartines, N. & Clavien, P.-A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240(2), 205–213 (2004).
Vickers, A. J. & Elkin, E. B. Decision curve analysis: A novel method for evaluating prediction models. Med. Decis. Mak. 26(6), 565–574 (2006).
Vickers, A. J., Cronin, A. M., Elkin, E. B. & Gonen, M. Extensions to decision curve analysis, a novel method for evaluating diagnostic tests, prediction models and molecular markers. BMC Med. Inform. Decis. Mak. 8(1), 26–35 (2008).
Jalali, A. et al. Visualising Statistical Models using Dynamic Nomograms. R package version 5.0 (2019).
Feringa, H. H. H. et al. Plasma N-terminal pro-B-type natriuretic peptide as long-term prognostic marker after major vascular surgery. Heart 93(2), 226 (2007).
Wijeysundera, D. N., Pearse, R. M., Shulman, M. A., Abbott, T. E. F. & Wijeysundera, H. C. Assessment of functional capacity before major non-cardiac surgery: An international, prospective cohort study. Lancet 391(10140), 2631–2640 (2018).
Eggers, K. M., Venge, P. & Lind, L. Prognostic usefulness of the change in N-terminal pro B-type natriuretic peptide levels to predict mortality in a single community cohort aged ≥70 years. Am. J. Cardiol. 111(1), 131–136 (2013).
Duchnowski, P., Śmigielski, W. & Kołsut, P. Usefulness of myocardial injury parameters in predicting prolonged postoperative use of inotropes drugs in patients undergoing heart valve surgery. J. Clin. Med. 14(8), 2719 (2025).
Funding
This study was supported by Key R&D Project of Science and Technology Department of Sichuan Province (2019YFG0491) and “The 13th Five-Year Plan” National Key Research and Development Program (2018YFC2001800).
Author information
Authors and Affiliations
Contributions
YHZ and FW have contributed equally to this article. TZ supported the funding. Yi Zhao detected the plasma concentration of NT-Pro BNP. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The protocol of this study was approved by the ethics committee of West China Hospital of Sichuan University (No. 2020(155)) with waiver of informed consent and was registered in chictr.org.cn (ChiCTR1900026223) before started this trial.
Consent for publication
All authors read and approved the final manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, Y., Zhao, Y., Zhu, T. et al. Perioperative NT pro BNP can predict severe postoperative complications in elderly patients undergoing noncardiac surgery. Sci Rep 15, 26184 (2025). https://doi.org/10.1038/s41598-025-11760-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-11760-x