Abstract
Bilateral stroke is an important risk factor for long-term prognosis of post-stroke dysphagia (PSD). To investigate neuroanatomical characteristics of bilateral hemispheric lesions associated with 6-month swallowing outcomes in PSD, 134 acute ischemic stroke patients referred for videofluoroscopic swallowing study were included. The chronicity, location, volume of brain lesions, and swallowing function were quantitatively analyzed, with 6-month swallowing outcomes dichotomized into good and poor recovery based on the need for tube feeding or diet modification. Permutation testing revealed significantly higher rates of acute and chronic lesions in the globus pallidus, putamen, and internal capsule (GP/PUT/IC) in patients with poor recovery (n = 16) than in those with good recovery (n = 118). Bilateral chronic lesions in the GP/PUT/IC were significantly associated with 6-month swallowing outcomes in the univariate (odds ratio [OR], 19.44; P < 0.001) and multivariable (OR, 13.79; P = 0.001) analyses. The volume of chronic lesions in the GP/PUT/IC was significantly larger in patients with poor swallowing recovery than in those with good recovery (P = 0.001). Bilateral chronic lesions in the GP/PUT/IC were also significantly associated with the pharyngeal phase score of the videofluoroscopic dysphagia scale (P = 0.009). This study highlights the prognostic value of chronic bilateral brain lesions involving GP/PUT/IC in patients with PSD.
Similar content being viewed by others
Introduction
Post-stroke dysphagia (PSD) is a common and serious complication. It can persist in 13–18% of patients for up to 6 months after stroke1,2. PSD can compromise nutritional intake and increase the risk of aspiration pneumonia, resulting in functional decline, extended hospital stays, and increased mortality in stroke survivors3. Despite the high prevalence and subsequent severe consequences of PSD, the neuroanatomical characteristics of brain lesions associated with long-term swallowing prognosis remain not fully elucidated. The identification of patients at high risk for PSD based on the neuroanatomical characteristics of brain lesions is important in preventing adverse outcomes and establishing timely and tailored treatment strategies.
Bilateral stroke is an important risk factor associated with long-term prognosis of PSD4,5. This is supported by the physiological underpinnings of swallowing, which is regulated by the bilateral hemispheres of the brain in an asymmetrical manner, involving sensory and motor cortical areas that interact through ascending and descending white matter pathways with diverse subcortical and brainstem regions6. During the recovery process of PSD, it is hypothesized that bilateral representations of the swallowing network and alternative pathways of innervations contribute to facilitating swallowing recovery, including cortical reorganization in the unaffected hemisphere7,8. Notably, quantitative analyses on the detailed neuroanatomical characteristics of the bilateral hemispheric lesions related to long-term prognosis of PSD are lacking, particularly regarding the chronicity, location, and volume of the brain lesions. Given that both acute and chronic lesions in the bilateral hemispheres can affect the functional outcomes of PSD, the individual premorbid status of swallowing-related brain topography prior to acute stroke should be included in quantitative analyses9.
This study aimed to investigate the neuroanatomical characteristics of bilateral hemispheric lesions associated with 6-month swallowing outcomes in patients with PSD. First, permutation testing was used to explore lesion locations associated with poor swallowing recovery in patients with PSD. Second, the risks of poor swallowing recovery in PSD patients with bilateral lesions at the identified locations were compared with those in patients with unilateral lesions.
Methods
Study population
All consecutive patients admitted to a single tertiary hospital between January 1, 2014, to July 31, 2022 were considered for inclusion if they met the following criteria: (1) diagnosis of acute ischemic stroke confirmed by magnetic resonance imaging (MRI), and (2) referral for videofluoroscopic swallowing study (VFSS) due to clinically suspected swallowing difficulty. The patients with any of the following conditions were excluded: (1) age < 19 years, (2) presence of neurological disorders that can affect swallowing function (e.g., Parkinsonism, amyotrophic lateral sclerosis), (3) presence of tracheostomy, (4) severe impairment of consciousness, or (5) low quality, incomplete coverage, or absence of brain MRI images. In the dysphagia management process, referral for VFSS in patients with stroke was based on clinical symptoms or signs suggestive of PSD, following routine standardized screening tests or clinical examination performed by physicians, and swallowing therapy was subsequently initiated according to the VFSS findings and the corresponding clinical recommendations. This study was approved by the Institutional Review Board of Seoul National University Hospital (No. 2211-105-1380), and the requirement for informed consent was waived for this retrospective review. This study was performed in accordance with all relevant guidelines and regulations.
Patient characteristics
Demographic, clinical, and neuroanatomical characteristics were obtained, including age, sex, National Institutes of Health Stroke Scale (NIHSS) at admission, laterality of acute lesions, laterality of chronic lesions, lesion location, duration from stroke onset to brain MRI, duration from stroke onset to initial VFSS, clinical dysphagia scale10 at initial VFSS, videofluoroscopic dysphagia scale (VDS)11,12 at initial VFSS, recommended diet at initial VFSS, and swallowing therapy. Swallowing outcomes at 6 months after stroke onset were dichotomized into good and poor swallowing recovery. If the patient did not require tube feeding or diet modification, the swallowing outcome was considered good; otherwise, it was considered poor.
Image acquisition and lesion analysis
MRI images were obtained in all patients according to a standardized protocol, including T1-weighted, T2-weighted fluid-attenuated inversion recovery (FLAIR), and diffusion-weighted imaging (DWI) sequences on the following MRI scanner systems: GE Signa HDxt 1.5 T, GE Signa EXCITE 1.5 T, GE Discovery MR750W 3 T (GE Healthcare, Chicago. IL, USA), Philips Ingenia 1.5 T, Philips Ingenia Cx 3 T, Achieva 3 T (Philips, Amsterdam, The Netherlands), Siemens Avanto 1.5 T, Siemens Espree 1.5 T, Siemens Sonata 1.5 T, Siemens Magnetom Essenza 1.5 T, Siemens Skyra 3 T, Siemens Skyra fit 3 T, Siemens TrioTim 3 T, and Siemens Verio 3 T (Siemens, Munich, Germany). Details of brain MRI sequences are heterogeneous among patients because of the retrospective nature of this study over 8 years (2014–2022), different MRI scanners, and technological updates in MRI sequences. T1-weighted images were acquired with slice thickness/gap of 1–5/1–7 mm, repetition time of 8–2,822 ms, and echo time of 3–26 ms. T2-weighted FLAIR images were acquired with slice thickness/gap of 4–5/4.8–7 mm, repetition time of 7,000–11,002 ms, and echo time of 87–129 ms. DWI images were acquired at b values of 0 s/mm2 and 1000 s/mm2, slice thickness/gap of 3–5/3–7 mm, repetition time of 2791–13,254 ms, and echo time of 54–182 ms. Although brain imaging was typically performed promptly after stroke onset for the diagnosis of acute ischemic stroke, if initial brain MRI images were of suboptimal quality or if the lesion was more clearly delineated on the follow-up scan, follow-up brain MRI images were used for the lesion analysis in this study.
The acute and chronic lesions in all patients with stroke were independently reviewed and manually outlined on DWI images at a b value of 1000 s/mm2 and FLAIR images, respectively, using MRIcron13 and ITK-SNAP14 by two clinicians blinded to the clinical information. A consensus was reached after discussion in cases of disagreement. Acute lesions were defined as areas of high signal intensity on DWI images, and chronic lesions were defined as areas of low signal intensity on FLAIR images. To distinguish chronic lesions from acute or subacute changes, only areas showing low signal intensity similar to that of cerebrospinal fluid on FLAIR images were considered chronic, and therefore, white matter hyperintensities in the periventricular areas were not included in the analysis. The lesion maps were smoothed using a 3-mm full-width half-maximum Gaussian kernel to remove uneven edges15. T1-weighted images were skull-stripped and manually edited using FreeView, a visualization tool implemented in the FreeSurfer software (https://surfer.nmr.mgh.harvard.edu/fswiki). The DWI and FLAIR images of each patient were skull-stripped and linearly registered to the corresponding T1-weighted images using Advanced Normalization Tools (ANTs)16 utilizing an inversion map of lesions as a mask image. The skull-stripped T1-weighted images were normalized to the Montreal Neurological Institute (MNI) template using ANTs with rigid, affine, and deformable SyN registration stages. When lesions were visually inspected on T1-weighted images, an inversion map of the lesions was used as a mask image during normalization. Transformation maps generated during the registration and normalization processes were used to normalize the lesion maps in the DWI and FLAIR images to the MNI template with nearest-neighbor interpolation. The lesion volumes of the normalized lesion maps in the DWI and FLAIR images were quantified using the FMRIB software library (https://fsl.fmrib.ox.ac.uk).
Quantitative analysis for swallowing function
To examine the association between lesion laterality at the acute or chronic stage and PSD, swallowing function at the initial VFSS was quantitatively assessed using the VDS. It is a validated tool that quantifies dysphagia severity based on VFSS findings in both the oral and pharyngeal phases, and has been validated in patients with various etiologies, including stroke11,12. Previous studies have reported significant associations between VDS scores and stroke-related lesion characteristics17,18. In the present study, VDS was evaluated by a physiatrist with six years of VFSS interpretation experience who was blinded to lesion location.
Statistical analysis
Demographic, clinical, and neuroanatomical characteristics were compared between patients with good and poor swallowing recovery using the independent-samples t-test or Mann–Whitney U-test and the chi-squared test or Fisher’s exact test. Permutation testing was employed to identify lesion locations with significant differences in 115 regions of interest from the Harvard Oxford Cortical and Subcortical atlases and the JHU ICBM-DTI-81 White-Matter Labels atlas between stroke patients with good and poor swallowing recovery19. In the permutation testing, a region of interest was regarded as a lesion location if it encompassed at least one voxel affected by the lesion. Statistical significance was tested using randomly assigned dichotomized datasets for good and poor swallowing recovery through 5000 permutations, generating a null distribution to compare with the actual difference. Univariate logistic regression analyses were conducted to evaluate associations of lesion laterality in the bilateral hemispheres and that in the globus pallidus, putamen, and/or internal capsule (GP/PUT/IC) with 6-month swallowing outcomes. Multivariable logistic regression analyses were performed to adjust for potential confounding effects of age and sex. One-way analysis of variance or the Kruskal–Wallis test was conducted to compare VDS scores according to the laterality of acute, chronic, and all lesions in the bilateral hemispheres and the GB/PUT/IC. Post-hoc analyses were performed using the Tukey test or the Mann–Whitney U-test, with the Bonferroni correction applied to adjust for multiple comparisons. Chi-squared test or Fisher’s exact test was conducted to evaluate the associations between individual VDS parameters in the oral and pharyngeal phases and the laterality of acute, chronic, and all lesions in the bilateral hemispheres and GB/PUT/IC. The overall and post-hoc significance level were set at P < 0.05 and P < 0.017, respectively. Statistical analyses were conducted using SPSS software (version 25; IBM Corp., Armonk, NY, USA) and MATLAB 2023a (MathWorks Inc., Natick, MA, USA).
Results
Clinical characteristics
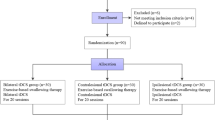
In this study, a total of 3,968 patients were newly diagnosed with acute ischemic stroke from January 1, 2014, to July 31, 2022 at a single tertiary hospital. Of the 292 patients referred for VFSS due to suspected dysphagia, 134 were included in the final analysis after applying both inclusion and exclusion criteria. Sixteen (11.9%) patients showed poor swallowing recovery. Among the 134 patients included in the analysis, 61 of the 128 patients with good swallowing recovery and 12 of the 16 patients with poor swallowing recovery had chronic lesions. Table 1 shows clinical characteristics showing significant differences between the patients with good and poor swallowing recovery, including sex (good, 58 [49.2%] vs. poor, 14 [87.5%], P = 0.006), clinical dysphagia scale at initial VFSS (good, 15.7 ± 13.5 vs. poor, 27.3 ± 18.6, P = 0.008), recommended diet at initial VFSS (P < 0.001), stroke lesions in the GP (good, 44 [37.3%] vs. poor, 11 [68.8%]; P = 0.02) and IC (good, 74 [62.7%] vs. poor, 14 [87.5%]; P = 0.05), the total (good, 29.9 ± 17.2 vs. poor, 57.8 ± 13.1, P < 0.001), oral phase (good, 8.0 ± 7.2 vs. poor, 14.1 ± 7.5, P = 0.005), and pharyngeal phase (good, 21.9 ± 13.7 vs. poor, 43.8 ± 12.2, P < 0.001) scores of the VDS. There were no other clinical characteristics showing significant differences between the two groups.
Lesion location associated with poor swallowing recovery
Significantly higher rates of acute and chronic lesions in the left GP, the left IC, and the right PUT were observed in the patients with poor swallowing recovery than those with good swallowing recovery (Supplemental Figure S1). The lesion probability maps also showed that acute and chronic lesions with high frequency were located at the GP, PUT, and IC in the patients with poor swallowing recovery compared to those with good swallowing recovery (Fig. 1).
Lesion laterality associated with poor swallowing recovery
In Table 2, only bilateral chronic lesions were associated with increased risk of poor swallowing recovery compared to no chronic lesion in the univariate logistic regression analysis (odds ratio [OR], 3.84; 95% confidence interval [CI], 1.03–14.26; P = 0.045), but not in the multivariable logistic regression analysis.
In Table 3, bilateral chronic lesions in the GP/PUT/IC were significantly associated with increased risk of poor swallowing recovery compared to no chronic lesion in the GP/PUT/IC in the univariate (OR, 19.44; 95% CI, 4.38–86.38; P < 0.001) and multivariable (OR, 13.79; 95% CI, 2.84–67.06; P = 0.001) analyses. Additionally, bilateral all lesions in the GP/PUT/IC were significantly associated with increased risk of poor swallowing recovery compared to no lesion in the GP/PUT/IC in the univariate (OR, 13.08; 95% CI, 2.52–67.90; P = 0.002) and multivariable (OR, 10.41; 95% CI, 1.80–60.16; P = 0.009) analyses.
Lesion volume associated with poor swallowing recovery
In Table 4, the volume of chronic lesions in the bilateral hemispheres significantly differed between the patients with good and poor swallowing recovery (good, 1.54 ± 6.10 cm3; poor, 2.93 ± 5.62 cm3; P = 0.014), whereas those of acute and all lesions showed no significant difference. The volume of chronic lesions in the GP/PUT/IC was significantly larger in the patients with poor swallowing recovery (good, 0.10 ± 0.26 cm3; poor, 0.43 ± 0.55 cm3; P = 0.001), whereas acute and all lesion volumes did not differ significantly between the groups.
Quantitative analysis for swallowing function
Among a total of 134 patients, one patient with good swallowing recovery was not included in the quantitative analysis for swallowing function due to poor VFSS video quality. In Supplemental Table 1, the total, oral phase, and pharyngeal phase scores of the VDS did not significantly differ according to the laterality of acute and chronic lesions in the bilateral hemispheres. In Table 5, the total and pharyngeal phase scores of the VDS differed significantly according to the laterality of chronic lesions in the GP/PUT/IC (total score, P = 0.011, post-hoc P = 0.008 for no lesion vs. bilateral lesions; pharyngeal score, P = 0.009, post-hoc P = 0.006 for no lesion vs. bilateral lesions). The total and pharyngeal phase scores of the VDS also differed significantly according to the laterality of all lesions in the GP/PUT/IC (total score, P = 0.009, post-hoc P = 0.016 for no lesion vs. bilateral lesions, post-hoc P = 0.011 for unilateral lesions vs. bilateral lesions; pharyngeal score, P = 0.008, post-hoc P = 0.006 for unilateral lesions vs. bilateral lesions). There were no other findings showing significant differences.
Table 6 indicates the associations between VDS parameters and the laterality of acute, chronic, and all brain lesions. Pyriform sinus residue was the only parameter to be significantly associated with the laterality of chronic lesions in the bilateral hemispheres (P = 0.030). For brain lesions in the GP/PUT/IC, lip closure and triggering of pharyngeal swallow was associated significantly with the laterality of acute lesions (P = 0.007, P = 0.030), and lip closure, vallecular residue, pyriform sinus residue, and aspiration were associated significantly with the laterality of chronic and all lesions (chronic, P = 0.035, P = 0.036, P < 0.001, P = 0.015; all, P < 0.001, P = 0.022, P < 0.001, P = 0.018). Apraxia was also significantly associated with the laterality of all lesions in the GP/PUT/IC (P = 0.005).
Discussion
This study aimed to demonstrate the neuroanatomical characteristics of bilateral hemispheric lesions associated with 6-month swallowing outcomes in PSD patients after acute ischemic stroke. Patients were divided into good and poor swallowing recovery groups based on the need for tube feeding or diet modification. Permutation testing revealed that the GP/PUT/IC exhibited significantly higher rates of acute and chronic lesions in patients with poor swallowing recovery than in those with good recovery. Based on the results, the GP/PUT/IC were adopted as lesion locations for analyzing the associations between bilateral hemispheric lesions and 6-month swallowing outcomes. Chronic lesions in the bilateral hemispheres showed a significant association with poor swallowing recovery in the univariate analysis only and indicated significantly increased lesion volume in patients with poor swallowing recovery compared to those with good recovery. Specifically, chronic lesions in the bilateral GP/PUT/IC showed a significant association with poor swallowing recovery in both univariate and multivariable analyses and indicated significantly increased lesion volume in patients with poor swallowing recovery compared to those with good recovery. Additionally, all lesions in the bilateral GP/PUT/IC showed a significant association with poor swallowing recovery in both univariate and multivariable analyses.
Previous neurophysiological and functional imaging studies on animal and human cerebral cortices have established that the neural representation of swallowing in the brain is bilateral, although possible equi-hemispheric contribution to cortical swallowing control is suggested in animal species, whereas bilateral hemispheric representation with an asymmetric dominance is identified in the human cortex20. Previous clinical studies have also demonstrated an increased risk of PSD necessitating the use of feeding tubes in cases of bilateral stroke21,22. Particularly when the dominant hemisphere for swallowing control is affected, the long-term prognosis of PSD may be worse in patients with bilateral stroke23. Considering the swallowing regulatory mechanism, bilateral hemispheric lesions after stroke have been considered to result in the severe deterioration of swallowing function by interfering with compensatory reorganization on the undamaged side7,24. Our results are partially consistent with those in the previous literature in that the risk of poor swallowing recovery was substantially high in PSD patients with bilateral lesions of GP/PUT/IC, rather than bilateral lesions encompassing the entire hemispheres or unilateral lesions within GP/PUT/IC.
This study indicated that long-term swallowing prognosis was associated with subcortical lesions in the GP/PUT/IC, rather than lesions in cortical regions, including the primary motor and somatosensory cortices, inferior frontal gyrus, anterior cingulate cortex, orbitofrontal cortex, and supramarginal gyrus, which reported to be associated with PSD15,25,26. Indeed, subcortical lesions have shown relatively strong associations with PSD compared to cortical lesions23. Lesions of subcortical areas such as GP, PUT, and corona radiata are associated with pharyngeal swallowing or aspiration in PSD27. Injuries of the GP, PUT, and associated white matter tracts, which are part of a neural circuit of voluntary swallowing, may lead to dysfunction of the corticomedullary tract, cortico–neostriatum–thalamocortical and neostriatum–substantia nigral loops, resulting in impaired inhibition of the medulla oblongata28,29. Lesions at the GP and PUT can deteriorate the maintenance of normal tone of the pharyngeal and laryngeal muscles and induce hyper-reflexive contraction of the cricopharyngeal muscles30,31 which is consistent with the findings of current study in that swallowing function in the pharyngeal phase was more impaired in patients with bilateral chronic lesions in the GP/PUT/IC. Additionally, the severity and location of white matter lesions have been considered important factors influencing the outcomes of PSD26,32. Particularly, damage to the corticobulbar tract, which is located at the posterior limb of the IC, can lead to the disconnection between the brain cortex and the swallowing center of the brainstem, consequently leading to compromised swallowing function33. The impairment of the bilateral corticobulbar tracts is associated with both short-34,35 and long-term5,36 swallowing recovery in patients with PSD. Future studies are needed to examine deteriorative and compensatory mechanisms underlying the disruption of swallowing-related neural circuits involving the GP, PUT, or IC, which may facilitate the development of alternative therapeutic strategies for patients with PSD.
Interestingly, acute lesions in the bilateral hemispheres or the bilateral GP/PUT/IC were not associated with long-term swallowing prognosis. As shown in Tables 2 and 3, acute lesions in the bilateral hemispheres were found in 37 out of 134 patients (27.6%), whereas only 2 patients (1.5%) had acute lesions in the GP/PUT/IC, which imply that most bilateral acute lesions likely occurred in regions other than these specific subcortical structures. Given the small number of patients with acute lesions in the GP/PUT/IC, this finding should be interpreted with caution. In contrast, both chronic lesions and all lesions in the GP/PUT/IC were significantly associated with long-term swallowing prognosis in this study. Similarly, the volume of chronic lesions in the bilateral GP/PUT/IC was greater in patients with poor swallowing recovery than in those with good recovery. The volume difference was not observed in patients with acute lesions or all lesions in those regions. It is considered less likely that a single, acute stroke would involve bilateral lesions in the GP/PUT/IC, although chronic stroke may have a relatively higher likelihood of involving these regions bilaterally. Additionally, in previous case studies, chronic lesions combined with acute lesions in the operculum or subcortical regions of the bilateral hemispheres can result in severe PSD, which was reported as bilateral opercular syndrome or Foix–Chavany–Marie syndrome37,38,39. Moreover, bilateral chronic lesions, such as small lacunar infarcts or white matter hyperintensities in the subcortical areas, typically assessed by the Fazekas scale40 are associated with the occurrence and severity of PSD and may cause high susceptibility to corticobulbar tract dysfunction, thereby interfering with neural control of swallowing5,34,41. These findings may indicate that chronic lesions could reflect accumulated structural damages in subcortical pathways, potentially a more enduring impact on swallowing functions than acute lesions alone. The present study highlights that chronic bilateral brain lesions involving GP/PUT/IC are significantly associated with long-term swallowing outcomes in patients with acute ischemic stroke, underscoring their prognostic value in clinical assessments. Even if most small lacunar infarcts or white matter injuries have been regarded as asymptomatic or associated with gradual cognitive decline rather than severe neurologic deterioration, pre-existing chronic lesions should be considered an essential cause of the severe swallowing impairment that persists up to 6 months after stroke.
This study had several limitations. First, the sample size was small, especially for the patients with poor swallowing recovery. Permutation testing was used as a non-parametric method to compare the frequency of lesion locations between the patients with good and poor swallowing recovery via 5000 permutations. This contributed to the identification of the GP, PUT, and IC with significantly higher rates of acute and chronic lesions in the brain in the patients with poor swallowing recovery. Second, this study was conducted on retrospective cohorts. Swallowing function in all patients with PSD was evaluated using VFSS, a standardized, instrumental swallowing assessment with high sensitivity and specificity for detecting swallowing impairment in patients with stroke, although the information regarding follow-up VFSS was not included in the analysis. Previous history of dysphagia or stroke was not available in the clinical records because of retrospective nature of this study, which could have affected the swallowing outcomes and interpretations of the results. Acute stroke in all patients was also confirmed using brain MRI; however, the details of the MRI sequences and MRI scanners varied across the patients. Further prospective studies are warranted to investigate the neuroanatomical characteristics based on a homogenous, standardized protocol for acquiring brain MRI images, thereby ensuring the development of long-term outcome prediction models with high accuracy and robustness based on stroke lesions.
In conclusion, this study highlights the prognostic value of chronic bilateral brain lesions involving GP/PUT/IC as a crucial neuroanatomical characteristic in patients with PSD. In particular, bilateral chronic subcortical lesions, including the GP, PUT, and IC, are associated with poor swallowing recovery and show increased lesion volume in patients with poor swallowing recovery compared to those with good swallowing recovery. This study suggests that clinicians should consider the impact of pre-existing chronic brain lesions on the long-term swallowing prognosis in patients with PSD following acute ischemic stroke. Future studies are needed to examine the deteriorative and compensatory mechanisms underlying the disruption of swallowing-related neural circuits involving the GP, PUT, and IC, which may facilitate the development of alternative therapeutic strategies for patients with PSD.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Smithard, D. G. et al. The natural history of dysphagia following a stroke. Dysphagia 12, 188–193. https://doi.org/10.1007/PL00009535 (1997).
Mann, G., Hankey, G. J. & Cameron, D. Swallowing function after stroke: prognosis and prognostic factors at 6 months. Stroke 30, 744–748. https://doi.org/10.1161/01.str.30.4.744 (1999).
Cohen, D. L. et al. Post-stroke dysphagia: A review and design considerations for future trials. Int. J. Stroke. 11, 399–411. https://doi.org/10.1177/1747493016639057 (2016).
Broadley, S. et al. Predictors of prolonged dysphagia following acute stroke. J. Clin. Neurosci. 10, 300–305. https://doi.org/10.1016/s0967-5868(03)00022-5 (2003).
Lee, W. H. et al. Development of a novel prognostic model to predict 6-Month swallowing recovery after ischemic stroke. Stroke 51, 440–448. https://doi.org/10.1161/STROKEAHA.119.027439 (2020).
Hamdy, S. et al. The cortical topography of human swallowing musculature in health and disease. Nat. Med. 2, 1217–1224. https://doi.org/10.1038/nm1196-1217 (1996).
Hamdy, S. et al. Recovery of swallowing after dysphagic stroke relates to functional reorganization in the intact motor cortex. Gastroenterology 115, 1104–1112. https://doi.org/10.1016/s0016-5085(98)70081-2 (1998).
Li, S. et al. Functional magnetic resonance imaging study on dysphagia after unilateral hemispheric stroke: a preliminary study. J. Neurol. Neurosurg. Psychiatry. 80, 1320–1329. https://doi.org/10.1136/jnnp.2009.176214 (2009).
Wilmskoetter, J., Daniels, S. K. & Miller, A. J. Cortical and subcortical control of Swallowing-Can we use information from lesion locations to improve diagnosis and treatment for patients with stroke?? Am. J. Speech Lang. Pathol. 29, 1030–1043. https://doi.org/10.1044/2019_AJSLP-19-00068 (2020).
Chun, S. W. et al. Inter-rater agreement for the clinical dysphagia scale. Ann. Rehabil Med. 35, 470–476. https://doi.org/10.5535/arm.2011.35.4.470 (2011).
Han, T. R., Paik, N. J. & Park, J. W. The functional dysphagia scale using videofluoroscopic swallowing study in stroke patients. J. Korean Acad. Rehabil Med. 23, 1118–1126 (1999).
Kim, J. et al. Validation of the videofluoroscopic dysphagia scale in various etiologies. Dysphagia 29, 438–443 (2014).
Yushkevich, P. A. et al. User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31, 1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015 (2006).
Rorden, C., Karnath, H. O. & Bonilha, L. Improving lesion-symptom mapping. J. Cogn. Neurosci. 19, 1081–1088. https://doi.org/10.1162/jocn.2007.19.7.1081 (2007).
Wilmskoetter, J. et al. Mapping acute lesion locations to physiological swallow impairments after stroke. NeuroImage Clin. 22, 101685. https://doi.org/10.1016/j.nicl.2019.101685 (2019).
Avants, B. B. et al. A reproducible evaluation of ants similarity metric performance in brain image registration. Neuroimage 54, 2033–2044 (2011).
Mo, S. J., Jeong, H. J., Han, Y. H., Hwang, K. & Choi, J. K. Association of brain lesions and videofluoroscopic dysphagia scale parameters on patients with acute cerebral infarctions. Annals Rehabilitation Med. 42, 560–568 (2018).
Moon, H. I., Jeong, Y. J. & Suh, J. H. Voxel-based lesion symptom mapping analysis for dysphagia in stroke patients with isolated cerebellar lesions. J. Neural Transm. 129, 65–74 (2022).
Mori, S. et al. Stereotaxic white matter atlas based on diffusion tensor imaging in an ICBM template. Neuroimage 40, 570–582 (2008).
Hamdy, S. Role of cerebral cortex in the control of swallowing. GI Motil. Online (2006).
Ickenstein, G. W. et al. Predictors of feeding gastrostomy tube removal in stroke patients with dysphagia. J. Stroke Cerebrovasc. Dis. 12, 169–174. https://doi.org/10.1016/S1052-3057(03)00077-6 (2003).
Kumar, S. et al. Predictors of percutaneous endoscopic gastrostomy tube placement in patients with severe dysphagia from an acute-subacute hemispheric infarction. J. Stroke Cerebrovasc. Dis. 21, 114–120. https://doi.org/10.1016/j.jstrokecerebrovasdis.2010.05.010 (2012).
Cheng, I., Takahashi, K., Miller, A. & Hamdy, S. Cerebral control of swallowing: an update on neurobehavioral evidence. J. Neurol. Sci. 442, 120434. https://doi.org/10.1016/j.jns.2022.120434 (2022).
Teismann, I. K. et al. Cortical swallowing processing in early subacute stroke. BMC Neurol. 11, 34. https://doi.org/10.1186/1471-2377-11-34 (2011).
Suntrup-Krueger, S. et al. The impact of lesion location on dysphagia incidence, pattern and complications in acute stroke. Part 2: oropharyngeal residue, swallow and cough response, and pneumonia. Eur. J. Neurol. 24, 867–874. https://doi.org/10.1111/ene.13307 (2017).
Hess, F., Foerch, C., Keil, F., Seiler, A. & Lapa, S. Association of lesion pattern and dysphagia in acute intracerebral hemorrhage. Stroke 52, 2921–2929. https://doi.org/10.1161/STROKEAHA.120.032615 (2021).
Jang, S., Yang, H. E., Yang, H. S. & Kim, D. H. Lesion characteristics of chronic dysphagia in patients with supratentorial stroke. Ann. Rehabil Med. 41, 225–230. https://doi.org/10.5535/arm.2017.41.2.225 (2017).
Mosier, K. & Bereznaya, I. Parallel cortical networks for volitional control of swallowing in humans. Exp. Brain Res. 140, 280–289. https://doi.org/10.1007/s002210100813 (2001).
Qin, Y., Tang, Y., Liu, X. & Qiu, S. Neural basis of dysphagia in stroke: A systematic review and meta-analysis. Front. Hum. Neurosci. 17, 1077234. https://doi.org/10.3389/fnhum.2023.1077234 (2023).
Wan, P. et al. Dysphagia post subcortical and supratentorial stroke. J. Stroke Cerebrovasc. Dis. 25, 74–82. https://doi.org/10.1016/j.jstrokecerebrovasdis.2015.08.037 (2016).
Kim, J. Y., Yoon, S. Y., Kim, J. & Wook Kim, Y. Neural correlates of cricopharyngeal dysfunction after supratentorial stroke: A voxel-based lesion-symptom mapping with propensity score matched case-control. Int. J. Stroke. 17, 207–217. https://doi.org/10.1177/17474930211006300 (2022).
Moon, H. I., Kim, G. S. & Lee, E. Is the location of white matter lesions important in the swallowing function of older patients with mild stroke? Dysphagia 34, 407–414 (2019).
Yim, S. H. et al. Distribution of the corticobulbar tract in the internal capsule. J. Neurol. Sci. 334, 63–68. https://doi.org/10.1016/j.jns.2013.07.015 (2013).
Fandler, S. et al. Dysphagia in supratentorial recent small subcortical infarcts results from bilateral pyramidal tract damage. Int. J. Stroke. 13, 815–819. https://doi.org/10.1177/1747493018778141 (2018).
Im, S. et al. Role of bilateral corticobulbar tracts in dysphagia after middle cerebral artery stroke. Eur. J. Neurol. 27, 2158–2167. https://doi.org/10.1111/ene.14387 (2020).
Jang, S. H. et al. Prognostic prediction of dysphagia by analyzing the corticobulbar tract in the early stage of intracerebral hemorrhage. Dysphagia 35, 985–992. https://doi.org/10.1007/s00455-020-10093-3 (2020).
Theys, T. et al. Neural correlates of recovery from Foix-Chavany-Marie syndrome. J. Neurol. 260, 415–420. https://doi.org/10.1007/s00415-012-6641-0 (2013).
Bradley, N., Hannon, N., Lebus, C., O’Brien, E. & Khadjooi, K. Bilateral Corona radiata infarcts: a new topographic location of Foix-Chavany-Marie syndrome. Int. J. Stroke. 9, E39. https://doi.org/10.1111/ijs.12387 (2014).
Rivas, K., Pan, J., Chen, A., Gutiérrez, B. & Julayanont, P. in Baylor University Medical Center Proceedings. 389–390 (Taylor & Francis).
Fazekas, F., Chawluk, J. B., Alavi, A., Hurtig, H. I. & Zimmerman, R. A. MR signal abnormalities at 1.5 T in alzheimer’s dementia and normal aging. Am. J. Roentgenol. 149, 351–356 (1987).
Wei, K. C., Wang, T. G. & Hsiao, M. Y. The cortical and subcortical neural control of swallowing: a narrative review. Dysphagia 39, 177–197 (2024).
Funding
This study was supported by Grant No. 0420170660 from the Seoul National University Hospital Research Fund. This research was also supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number : RS-2023-00264326).
Author information
Authors and Affiliations
Contributions
EK: formal analysis, investigation, methodology, writing-original draft, writing - review and editing, visualization. M-Y L: data curation, formal analysis, investigation, methodology, writing-original draft. HG S and B-M O: conceptualization, data curation. YL L: formal analysis, investigation, writing-original draft, writing - review and editing. WH L: conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, supervision, writing-original draft, writing - review and editing. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, E., Lee, MY., Seo, H.G. et al. Impact of bilateral and unilateral cerebral lesions on swallowing recovery at 6 months in poststroke dysphagia. Sci Rep 15, 26825 (2025). https://doi.org/10.1038/s41598-025-12688-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-12688-y