Abstract
This study investigated the application effect of lean management in the treatment of acute stroke in medical laboratories and evaluated the impact on laboratory turnaround time (TAT) and operator satisfaction. In this study, 287 patients with acute stroke were selected from the Second People’s Hospital of Hunan Province and divided into a control group (129 cases, before lean management) and an experimental group (158 cases, after lean management). Lean management measures included establishing fast transfer channels, information management, optimisation of the centrifuge configuration, priority management, personnel training, use of the 6 S method, and visual management to optimise the process. The effects of lean management were evaluated by comparing the TAT of key inspection items using an operator satisfaction questionnaire. Lean management shortened the TAT for coagulation (21–18 min) and biochemical (33–29 min) tests (P = 0.000). Laboratory operators reported that lean management positively affects the overall performance of the laboratory. The application of lean management in medical laboratories can effectively improve the treatment efficiency of patients with acute stroke, shorten the TAT of key detection items, and provide high satisfaction among laboratory personnel.
Similar content being viewed by others
Introduction
Cerebrovascular accident, commonly known as stroke, is a leading cause of permanent disability worldwide, learning to a substantial socioeconomic burden and consumption of medical resources. From a pathophysiological perspective, stroke mainly involves ischaemic and haemorrhagic factors, of which ischaemic stroke is the most common. Treatment strategies for stroke remain limited and focus on acute interventions1. Timing is critical in managing acute stroke, and prompt treatment can restore perfusion in the penumbra region, thereby minimising neurological impairment. Neuropathological studies have confirmed that up to 1.9 million neurons are destroyed per minute in patients with untreated ischaemic stroke2highlighting the importance of early diagnosis and timely intervention. According to current clinical guidelines, intravenous thrombolytic therapy with recombinant tissue plasminogen activator (alteplase) may be considered for patients with acute ischaemic stroke diagnosed within 4.5 h of symptom onset. This regimen significantly reduces long-term disability significantly3. The HERMES meta-analysis has demonstrated that endovascular therapy within 6 h of acute ischaemic stroke onset significantly improves reperfusion rates and clinical prognosis in patients with large vessel occlusion and is particularly safe and effective in patients with low ASPECTS scores4. However, the prognosis for some patients remains poor, even with endovascular therapy, the efficacy and safety of requires further study in patients with low ASPECTS scores more than 6 h after stroke onset5. Recently, Tenecteplase, also known as TNK, a genetically modified plasminogen activator of Atilase, has gradually become a potential alternative for thrombolytic therapy in acute ischaemic stroke because of its longer half-life, higher fibrin specificity, and convenient administration through a single intravenous injection6.
However, intravenous thrombolytic therapy carries the potential risk of intracranial haemorrhage, which is particularly prominent in specific patient populations, including those who are receiving anticoagulation with warfarin, are on antiplatelet agents, or have thrombocytopenia7. According to the guidelines for the early management of acute ischaemic stroke, intravenous thrombolytic therapy should not be delayed by waiting for laboratory test results unless the patient has a clear risk of bleeding (e.g. thrombocytopenia, coagulation dysfunction, or anticoagulant use). Computed Tomography Angiography can be performed directly without waiting for creatinine results for patients who meet the indications for mechanical embolectomy if they have no history of renal function damage8. In actual medical treatment, the situation is often complex and variable, especially when an accurate medication history (e.g. anticoagulant use) cannot be obtained quickly because the patient has impaired consciousness or is unaccompanied and clinicians must rely on laboratory tests, such as coagulation function (International Normalized Ratio/Activated Partial Thromboplastin Time), to rule out contraindications to thrombolysis. However, hospitals must often wait for these critical laboratory results before safely initiating intravenous thrombolytic therapy for medical quality control and to avoid the risk of medical disputes. Therefore, rapid and accurate laboratory test results are of great clinical importance for optimising treatment decisions and improving prognosis when treating patients with acute ischaemic stroke.
In patients with acute stroke, the timeliness and quality of laboratory test results are at the heart of the medical process, from diagnosis and intervention to treatment and rehabilitation. This link has significant time-sensitive characteristics, its quality is directly related to the scientific validity and effectiveness of medical decision-making, and it plays an irreplaceable role in clinical practice9. Medical laboratory turnaround time (TAT), defined as ‘the period from sample collection to laboratory report to clinician’10has been introduced to clinical practice as a key quality indicator to objectively evaluate the service effectiveness of laboratories. This study introduced an innovative lean management model to comprehensively improve the quality of laboratory management. Lean management originated in the manufacturing industry, and its core concept is improving operational efficiency by systematically identifying and eliminating waste in processes, particularly through the application of Toyota’s production system. With its successful utilisation in the medical field, various organisations have adopted this management concept, including hospitals. Studies have shown that by implementing lean management principles, medical institutions can significantly optimise workflow stability and reliability, improve operational efficiency, reduce healthcare costs, improve patient satisfaction, and enhance management efficiency11.
Several international empirical studies have verified its significance in healthcare management. In Poland, a study on the economic benefits of factors influencing the prolongation of hospitalisation in the neurology department of a hospital showed that by applying lean management tools to identify key influencing factors and implementing targeted interventions, patients’ hospitalisation cycle can be effectively shortened and significant economic benefits can be generated12. The empirical application of lean management in the sleep department of a public hospital in Spain verified the clinical utility of implementing lean management to integrate personnel training and engagement, process waste identification and optimisation, and performance monitoring and improvement. The systematic implementation of lean management practices and tools across the entire service value chain was found to significantly improve the efficiency of patient process management (i.e. effectiveness, quality, and efficiency indicators) while simultaneously promoting the organisational transformation of healthcare institutions to a lean culture13. The importance of value stream mapping as a foundational tool for lean healthcare at the implementation level has been widely recognised. A 2015–2019 scoping review revealed that the adoption of value stream matching is concentrated in tertiary care settings and the United States is leading the way in this practice area14. Lean management implementation follows a standardised five-step cyclical process that is cross-situationally universal: (1) accurately define value connotations based on patient needs, (2) identify process bottlenecks and system constraints through value stream mapping, (3) systematically eliminate non-value-added activities to optimise the value flow, (4) land improvement programs and validating patient access, and (5) establish continuous improvement mechanisms to achieve service perfection enhancement15. This standardised framework provides a clear path for implementing lean management in healthcare organisations.
This study focused on the optimisation of the laboratory processing process of emergency stroke samples and adopts a systematic research approach. First, rapid transport channel stream mapping was established and optimised to accurately identify key bottlenecks affecting efficiency. Then, based on lean management principles, targeted process optimization strategies were designed and a standardized workflow system was built. By comparing and analysing TAT data before and after implementing lean management, the processing efficiency and quality improvement effect of acute stroke green channel samples were systematically evaluated. Finally, laboratory staff members’ understanding of lean management, mastery of the lean concept, acceptance of process improvement, and perceived implementation barriers were systematically evaluated using a questionnaire survey, which provided an important reference for the effective implementation of lean improvement actions.
Methods
General participant Information
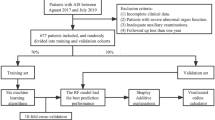
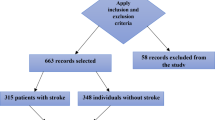
In this study, based on the laboratory information management system (LIMS) and electronic medical records of the Second People’s Hospital of Hunan Province (Hunan Provincial Brain Hospital), we rigorously screened and included a total of 287 specimens. The control group comprised 129 specimens collected between 1 January and 30 June 2023, which were handled using the routine testing process before the improvement of lean management. The experimental group included 158 specimens collected between 1 October 2023 and 31 March 2024 which were analysed by applying the stroke specimen testing process optimised using lean management. The inclusion criteria were patients 40–85 years of age with clinically confirmed acute ischaemic stroke (meeting the criteria of the Chinese Guidelines for the Diagnosis and Treatment of Acute Ischaemic Stroke 2023, confirmed by CT/MRI), with onset-to-submission time ≤ 4.5 h. Those with comorbid malignant tumours, coagulation disorders, or ineligible specimens were excluded. This study used a before-and-after design. Regarding the potential limitations of the control group, we effectively controlled for seasonal fluctuations in the incidence of acute stroke (e.g. higher incidence in winter) by rigorously matching the historical control and intervention groups based on age, sex, and onset time (including seasonal distribution). During the study period, the turnover rate of key laboratory personnel remained below 5% (with laboratory technicians having an average tenure of 4.2 ± 1.1 years), and the core operational team maintained a high level of stability, thereby minimising the interference of human factors on the measurement of laboratory TAT.
Laboratory examination
Complete blood count (CBC) tests were performed using a haematology analyser (Mindray BC7500). Coagulation tests were performed using a HeatMecan coagulation instrument (Coapresta3000). Biochemical parameters were analysed using biochemical and immune pipeline analysers (Mindray SAL6000, SAL9000).
This study was approved by the Ethics Committee of the Second People’s Hospital of Hunan Province (Brain Hospital of Hunan Province). All experiments were performed according to the relevant guidelines and regulations.
Specific implementation methods
This study used a controlled design to systematically compare the traditional testing process with an optimised lean management testing process. The aim was to comprehensively evaluate the impact of lean management on laboratory work efficiency and testing quality. The control group utilised the conventional testing process before the implementation of lean management, which was characterized by the following features: (1) sample processing primarily depended on manual operations, including manual sample classification and information verification; (2) traditional testing equipment was used, resulting in low automation; and (3) process standardisation was inadequate, as evidenced by the need to manually enter samples into the LIMS individually, a lack of testing sequence optimisation, conventional reporting of test results, and significant efficiency bottlenecks throughout the process.
The experimental group implemented lean management and optimised the testing process, strictly adhering to the principles of systematic improvement. The optimisation process followed two steps. First, the Delphi method was used to collect feedback from laboratory operators, and two rounds of expert consultations were conducted to identify key issues in the routine process, thereby gaining an in-depth understanding of the challenges and pain points in actual operations. Second, the time and motion study method was used to systematically analyse various aspects of the testing process. This method can capture precise time node data by quantitatively recording the time spent and operational actions involved at critical stages, such as sample processing, testing operations, and result review. A detailed analysis of the time node data was performed for each step of the process. Additionally, failure mode and effect analysis was used to systematically evaluate the severity, frequency, and detectability of potential failures within the process. For example, this analysis helped reduce the risk of laboratory contamination and identify key potential risk points. Through this comprehensive analysis, we identified three key bottlenecks in the process: (1) sample transport time, (2) prolonged waiting time for centrifugation, and (3) extended waiting time for boarding.
Based on the analysis results, we utilized a value stream mapping tool to systematically evaluate the laboratory testing process. This method identifies non-value-added elements of the process (e.g. sample transport waiting time) by visualising the dynamic mapping of the sample, information, and resource flows. We also conducted a systematic time-data analysis of the entire process from clinical ordering to result review. Establishing a real-time monitoring system allowed us to accurately track the time spent on each step, pinpoint efficiency bottlenecks, and develop targeted process optimisation plans. The specific optimisation measures included the following: (1) introducing an automated sample processing system, (2) optimising the sample transport path, (3) implementing a batch centrifugation strategy, (4) establishing a priority detection mechanism, and (5) enhancing the functionality of the LIMS. All optimisation measures were implemented following a feasibility assessment and pre-experimental verification (Fig. 1).
Strategies to improve delays in transport, centrifugation, and on-machine detection
During the processing of stroke samples in the laboratory, the maximum delay time for nursing staff to transport these samples to the testing department was 8 min. The longest delay for sample centrifugation was 15 min, and the maximum delay time for machine testing was 10 min. These delays resulted in three critical sample transport times, extended waiting times for sample centrifugation, and excessive waiting times for machine testing. Thus, several lean management improvement measures were implemented, as described below.
Fast transit channel establishment and optimisation
A standardised emergency specimen transport system was established, incorporating a rapid ‘collection-to-testing’ response mechanism. To ensure efficiency, a dedicated stroke sample transport channel was implemented utilising multilayer labelled transfer boxes (44 × 26.1 × 24.5 cm) and an intelligent dispatch system to guarantee real-time courier response. A priority transport network for patients with stroke should be implemented in the hospital, utilising specialised identification and rapid transport tools to maximise the safety and timeliness of the transport process.
Information management system construction
In this study, RFID and QR code technology were used to construct an LIMS. RFID technology realises the automatic identification of reagent consumables and monitoring of the storage environment, and the QR code system tracks the entire sample testing process. Through an intelligent early warning mechanism, this system realises the visual monitoring of material management and sample flow, thereby significantly improving the efficiency of laboratory management and quality control. The logic of RFID technology is presented in Supplementary Annex 1.
Intelligent upgrade of the centrifuge configuration
This system integrates remote control, real-time monitoring, and data analysis functions to improve operational safety and provide reliable data support for quality control and scientific research.
Establishing a specimen priority management system
Evidence-based medicine was developed based on the classification criteria for patients with stroke, time window of onset, National Institutes of Health Stroke Scale (NIHSS) scores, and other clinical indicators that can be comprehensively evaluated. A multidimensional priority evaluation system was established to facilitate this process. The information system enabled the automatic grading and prioritisation of samples, thereby ensuring that samples from critically ill patients were identified promptly.
Optimising experimental human resource allocation
Post- and regional-responsibility systems should be implemented, along with the establishment of a standardised operational process training system. Regular professional skill training and competency assessments can enhance inspectors’ operational proficiency and accuracy. By analysing historical data and utilising predictive models, the personnel scheduling system can be optimised to ensure the effective allocation of human resources during peak testing periods, thereby minimising delays in detection caused by human factors.
Addressing circulation issues and enhancing efficiency
Based on the urgent need for rapid detection of acute stroke samples, this study identified several key efficiency bottlenecks in the laboratory workflow through systematic onsite observations, time-action research, and quantitative data analysis. the first, the inefficient design of personnel movement resulted in a high frequency of path crossings (52%). Second, job responsibilities were poorly defined, leading to overlapping functions. Third, human resources were unevenly distributed, with the workload index for some positions being significantly higher (30%). (Fourth, equipment utilisation showed notable disparities, with the utilisation rate reaching 85% during peak hours (8:00–10:00), dropping to 50–60% during lunchtime (12:00–14:00), and remaining low at 35–45% during nighttime hours (22:00–6:00), while key equipment utilisation rates fluctuated between 35% and 85%. These issues not only diminished detection efficiency but also increased biosafety risks in the laboratory, as evidenced by a biosafety risk assessment score of 77 points for Level 2 laboratories. These challenges were addressed in this study using standardised improvement tools from the lean management system utilised in hospitals, as follows: (1) the 6 S management method (sorting, setting in order, shining, standardising, sustaining, and safety); (2) a visual management system that conveys system status through colour coding, electronic signboards, and other intuitive displays; (3) Poka-Yoke technology, which prevents errors through physical constraints or programmatic enforcement, thereby eliminating human error; and (4) the A3 problem-solving method, which is a systematic approach that presents the background of the problem, root cause analysis, improvement measures, and validation results in a structured one-page report. This approach, combined with the principles of Business Process Reengineering, allowed us to fundamentally redesign the emergency testing process. By eliminating non-value-added steps, optimising resource allocation, and restructuring workflows, we established a new model of ‘sample-on-arrival-on-examination’ for emergency testing. The implemented targeted improvement measures are detailed below (Fig. 2).
On-site management and quantitative analysis
This study used a blended research method to systematically analyse laboratory workflows through a combination of direct observation and semi-structured in-depth interviews. A high-precision time-and-motion study design was used to quantitatively assess the laboratory workflow. By meticulously recording the operational steps of personnel, equipment usage efficiency, and time consumption patterns, this method emphasises micro-motion analysis and time allocation assessment for key steps, including sample reception, preprocessing, testing, and result review. This study established a comprehensive database of time nodes throughout the process, providing precise data support for subsequent process optimisation. This study introduced the 6 S management method (i.e. Sorting, Set in order, Shine, Standardise, Sustain, and Safety) to enhance the laboratory working environment and implemented three key improvement measures. First, a standardised item classification system was established along with a visual identification management system. Second, the storage layout of items was optimised and minimum and maximum inventory standards were formulated. Third, a systematic regular cleaning and maintenance program was established, including a preventive maintenance schedule for instruments and equipment, according to a predetermined maintenance cycle, to ensure stable equipment performance. Simultaneously, the Responsibility Assignment Matrix was utilised to clarify the specific responsibilities associated with each position in the cleaning work. The division of labour was presented in a tabular format to eliminate any ambiguity regarding responsibilities. Furthermore, a tiered training system was employed to systematically enhance the 6 S management capabilities of the medical staff.
To foster continuous improvement, the laboratory established an employee participation mechanism including: (1) a 6 S improvement suggestion box, (2) regular quality improvement meetings, and (3) an evaluation and reward system for improvement suggestions. Each professional group developed a tailored process optimisation plan based on the ‘PDCA’ (Plan-Do-Check-Act) cycle and achieved continuous improvement through closed-loop management in the planning, implementation, checking, and processing phases. Key performance indicators were established to quantitatively assess the laboratory’s operational efficiency, testing quality, and service level. Additionally, a regular inspection and feedback mechanism was instituted to ensure that the improvement measures were implemented effectively. The laboratory standardised work area management, significantly reduced sample TAT, and optimised process connectivity using a multidimensional analysis framework encompassing space utilisation, time efficiency, image management, and economic benefits. The A3 problem-solving method was used to establish a rapid response mechanism for laboratory quality. Key elements, such as problem description, root cause analysis, countermeasure formulation, and effect verification, were integrated using a structured one-page reporting system to facilitate comprehensive management from problem identification to measure implementation. This approach aimed to create a virtuous cycle encompassing problem analysis, countermeasure implementation, and effect-tracking. Regular management reviews and internal audits were conducted. Management reviews, led by laboratory management, focus on assessing the strategic compliance and operational effectiveness of the quality management system, whereas internal audits identify potential risks and implements preventive measures through systematic compliance checks. These two mechanisms work in tandem to ensure that continuous improvement initiatives align with the actual needs of the laboratory.
Lab layout optimisation
In this study, computer-aided design and digital twin technology were used to systematically optimise the laboratory’s spatial layout. A digital model of the laboratory was constructed using 3D laser scanning, and the functional area was scientifically planned based on a path optimisation algorithm. The main optimisation measures included placing the sample receiving area adjacent to the pretreatment area to shorten the sample transmission distance by 54%, repositioning equipment according to frequency of use to reduce the average distance that operators travelled by 3.2 m (95%CI: 2.8–3.6 m), and introducing an intelligent error-proofing system to reduce the error rate by 45%. Through digital modelling and intelligent optimisation, these solutions significantly improved space utilisation, work efficiency, and operational safety. The technical logic of the computer-aided design is shown in Supplementary Annex 1.
Restructuring process and parallel processing
Systematic process reconstruction was used to significantly improve the operational efficiency and quality control level of the laboratory. Process mining technology was used to analyse the log data of the laboratory information system, and six non-value-added steps were successfully identified and eliminated. Furthermore, the traditional serial processing mode was transformed into a hybrid mode combining parallel processing and pipeline operation, thereby increasing detection efficiency by 45% (95%CI: 42–48%). Implementing preventive maintenance programs, automatic calibration systems, and error-proofing technology enabled an operating error rate below 3% to be maintained. Applying the critical path method reduced the average wait time by 7 min, and full laboratory automation automated 80% of the testing steps. A vision management system was used to reduce exception response times by 30% through standardised and electronic signage. These comprehensive measures not only optimised the work process but also established an efficient and accurate modern laboratory operation system.
Efficient sample processing and intelligent monitoring systems
This study significantly enhanced the accuracy and reliability of detection results by establishing an intelligent sample quality monitoring system. Machine vision technology was used to automatically identify test tube types (98% accuracy) and make high-precision volume measurements (error ± 0.3µL), combined with an intelligent centrifuge monitoring system ensuring standardised sample processing by real-time monitoring of rotational speeds of 3000–3500 rpm and a temperature of 25 °C. A serum quality assessment system based on multispectral imaging was implemented to quantify degrees of haemolysis, lipemia, and jaundice, with all testing data being fully traceable through a high-resolution imaging system. Furthermore, an Internet of Things monitoring platform reduced reagent waste by 20% (95%CI: 18–22%) through real-time monitoring of reagent consumption rates, remaining test counts, and expiration alerts aided by an intelligent allocation algorithm. Simultaneously, as lifecycle monitoring system for analytical instruments was implemented to collect data in real-time from three dimensions: calibration status, quality control indicators, and abnormal alerts. This system utilised machine learning algorithms to achieve a 94% accuracy rate in fault warnings and integrate advanced features, such as critical value alerts, intelligent matching of patient information, and dynamic visualisation of samples, thereby comprehensively improving laboratory management efficiency and testing quality.
Evaluating the effectiveness of lean management implementation
The time from the execution of the doctor’s orders to the receipt of the sample, as well as the TAT for the whole blood cell, coagulation, and biochemical tests were compared before and after lean management implementation.
Laboratory operator satisfaction survey
We used convenience sampling to select 39 staff members from a medical laboratory to complete a self-administered questionnaire to analyse the application of lean management in the laboratory and its impact on stroke treatment efficiency. The questionnaire included eight core indicators: staff awareness of lean management concepts, training effectiveness, practical application, work efficiency, work atmosphere, resource allocation, workflow optimisation, and overall performance impact. It comprised questions with ‘yes/no’ options, and data were collected electronically via QR codes. The results were analysed using statistical methods, and the evaluation of each indicator was visualised as percentages to assess the potential contribution of lean management to improving the efficiency of stroke detection, such as by reducing TAT.
Statistical methods
SPSS 25.0 (IBM Corp., Armonk, NY, USA) was used for data analysis. The normality of the data was assessed using the Kolmogorov–Smirnov test (large sample, n = 254) for all continuous variables, and the level was set to α = 0.05 (two-sided). The Shapiro–Wilk test was performed as a sensitivity analysis for some key variables to enhance the robustness of the test. The results of both tests showed that the study data did not conform to a normal distribution (P < 0.05). Based on the non-normally distributed characteristics, the Mann–Whitney U test was used to compare the experimental and control groups. Data were described as medians (M) and interquartile ranges (IQR), specifically M (P25, P75). The threshold for statistical significance was set at P < 0.05 (bilateral).
Results
Lean management process efficiency in the laboratory
The laboratory systematically optimised its core processes using lean management tools, which significantly enhanced detection efficiency and quality. In response to key bottlenecks, such as sample transport, centrifugation wait times, and detection delays, an intelligent transport system and standardised emergency sample handling procedures were introduced, reducing transfer times by over 50%. Furthermore, optimising the laboratory layout and minimising operational pathways improved workflow efficiency, and dynamic human resource scheduling was implemented to stabilise detection capacity. Regarding quality control, the laboratory deployed an intelligent monitoring system to achieve full-process sample tracking. Automated detection equipment and priority management mechanisms were applied to further reduce manual intervention and enhance detection stability. Preventive maintenance strategies and 6 S on-site management were used to significantly optimise the reliability of the laboratory environment and equipment, thereby reducing operational error rates.
Emergency stroke specimen turnaround time
The lean management method was employed to systematically optimise the entire stroke specimen detection process, enhance detection efficiency, and ensure the quality of the results. Regarding process optimisation, the sample pretreatment stage streamlined the workflow to reduce the time required for registration and centrifugal preparation. Improved equipment scheduling and batch processing during the detection and analysis stages effectively shortened wait times for onboard detection and increased processing capacity. Simultaneously, quality management was strengthened, leading to improved accuracy in specimen identification, expedited re-examination of abnormal results, and a 100% timely reporting rate for critical values. Specific data indicated that the TAT for blood coagulation tests decreased significantly from 21 min (IQR 19–27; 95%CI [18, 23]) to 18 min (IQR 15–24; 95%CI [16, 20]). The TAT for biochemical tests decreased from 33 min (IQR 30–36; 95%CI [30.9, 35.1]) to 29 min (IQR 27–30; 95%CI [28.0, 30.0]), whereas the TAT for whole blood cell counts remained at 4 min, and the time from the execution of medical advice to receipt of samples was 11 min. These results demonstrate that lean management can significantly enhances the overall efficiency and stability of stroke specimen detection, particularly in coagulation and biochemical testing (Table 1).
Lean management satisfaction questionnaire
This study systematically assessed the significant role of lean management in enhancing service quality, optimising costs, and improving time management in medical laboratories. A sample of 39 laboratory staff members was used to examined the impact of lean management on stroke care efficiency by collecting data through a self-administered questionnaire including eight core indicators. To ensure the scientific validity of the satisfaction questionnaire, two hospital management experts and two laboratory directors were invited to evaluate its content validity and ensure that the items were professional and representative. Subsequently, a pre-test was conducted among 10 target employees, and the data analysis showed that the questionnaire had good internal consistency. In terms of concept mastery, 90% of the respondents demonstrated a strong understanding of the core principles of lean management, whereas the remaining 10% remained in the learning phase. Regarding training satisfaction, 95% of the respondents expressed satisfaction with the content, format, and effectiveness of the training, with only 5% providing suggestions for improvement. Concerning the application of concepts, 70% of the respondents reported that they could effectively apply lean management principles to their daily work, whereas 30% indicated that they required additional practical guidance. With respect to work efficiency, 90% of the respondents believed that lean management significantly enhanced laboratory efficiency. Furthermore, all the respondents (100%) agreed that lean management positively affected the work atmosphere in the laboratory. Regarding resource utilisation, 80% of the respondents believed that lean management optimises resource allocation, whereas the remaining 20% still saw room for improvement. The impact of process optimisation was also widely acknowledged, with 95% of the respondents affirming the positive effects of lean management on work processes. Furthermore, all the respondents (100%) agreed that lean management positively influenced the overall performance of the laboratory. In summary, lean management achieved significant results in enhancing laboratory work efficiency, optimising resource allocation, improving the work environment, and promoting process optimisation. However, some opportunities for improvement remain in terms of conceptual depth and practical guidance (Table 2).
Discussion
Time is of the essence in the treatment of patients with acute stroke. The complexity and urgency of the medical environment make the application of the lean management theory particularly crucial. Studies have shown that 86% of healthcare institutions have widely adopted lean management concepts16reflecting their significant advantages in improving healthcare efficiency and core value as a patient-centred management philosophy. Lean management is dedicated to creating optimal medical value for patients by maximising the use of available resources and human skills. Some studies have optimised the stroke treatment process by applying value stream analysis in lean management and standardising the stroke centre process. This has involved adjusting the thrombolysis site and establishing a lean stroke management team, which has been shown to significantly reduce the costs associated with treating cerebral infarction17.
This study innovatively applied lean management concepts to significantly optimise the medical laboratory process and provide valuable time to treat patients with acute stroke. To improve the timeliness of stroke treatment, we systematically identified and eliminated waste in the testing process, thereby achieving more efficient testing services with less resource consumption. This methods applied in this study comprehensively improved inspection efficiency through the synergy of five core strategies: establishment of a rapid transport channel for stroke specimens, construction of a whole-process information management system, implementation of intelligent centrifuge upgrades, establishment of a specimen priority management system based on clinical critical values, and optimisation of experimental human resource allocation. Specifically, increasing the transport system speed decreased the time needed for specimen detection in patients with stroke, information management realised real-time tracking of specimen status, intelligent equipment ensured test quality, and optimisation of human resources facilitated the execution of key links. In a quality improvement practice of a urine analysis laboratory, through systematically implementing lean management measures for five months, including comprehensively applying tools such as Gemba Walk, Takt Time, cycle time optimisation, value stream mapping, the TAT of routine urine testing items was significantly improved18.
In this study, the sample TAT was significantly shortened by comprehensively optimising the testing process of stroke samples, thereby improving the efficiency and quality of laboratory treatments for patients with stroke. Through a systematic evaluation of the processing of fast-track samples for acute stroke, we compared TAT data before and after lean management implementation and proposed targeted optimisation strategies. Specifically, TAT for the coagulation and biochemical tests decreased from 21 to 18 min and 33 to 29 min, respectively, and the difference was statistically significant (P = 0.000). These improvements are mainly attributed to several measures. First, sample centrifuge wait times can be significantly reduced by optimising centrifuge configuration and introducing remote monitoring technology. Second, priority management strategies can be implemented to ensure that high-priority samples are prioritised. Third, the standardised operation training of laboratory personnel can be strengthened, the operation proficiency and accuracy of testing personnel can be improved, and human error can be reduced. In addition, optimising the laboratory layout and improving the flow line design, especially by reducing path crossings and shortening sample transport distance, can further improve detection efficiency. However, despite significant results of lean management in coagulation and biochemical testing, no significant improvement was observed in CBC detection. This may be related to the effectiveness of the CBC test itself. As a routine testing item, the operation process of CBC testing is relatively simple and highly standardised, and a short TAT can be maintained even without implementing lean management. However, this does not imply that lean management does not play a role in CBC testing. Lean management can still help maintain the efficiency and accuracy of CBC testing by optimising the overall laboratory environment and improving the skill levels of the testing personnel.
In this study, laboratory operations were optimised from different dimensions through four efficiency schemes: on-site management improvement and quantitative analysis, laboratory layout optimisation, process reorganisation and parallel processing, efficient sample processing, and intelligent monitoring systems. These improvements enhanced the quality of the laboratory and testing systems that respond quickly to the needs of emergency stroke care. The results show that the lean management method has important application value in clinical laboratory process optimisation, as it can significantly improve the timeliness of routine tests without affecting quality. A previous study that focused on the mechanisms by which lean and Six Sigma methodologies influence clinical laboratory service quality and operational effectiveness by describing a management framework for continuous quality and process improvement in healthcare organisations showed that laboratory service delivery systems can be comprehensively upgraded by eliminating non-value-added activities, reducing process variability, and optimising resource allocation15. Kanamori et al.19. implemented a one-year lean program at the Swedish Health Center, focusing on the application of 6 S management (sorting, rectification, sweeping, cleaning, literacy, safety), which effectively improved the working environment by reducing redundant items, improving order, optimising signage, and improving service quality. However, successful implementation in healthcare must draw on the experience of the manufacturing industry, with due consideration of the unique nature of the services provided by healthcare organisations. Successful implementation depends not only on an in-depth understanding of the internal environment but also on selecting appropriate improvement methods and ensuring the long-term effectiveness of improvement measures through continuous follow-up20.
Furthermore, a satisfaction survey in this study showed that the laboratory staff was highly accepting of lean management implementation. A virtuous cycle of ‘process optimisation-treatment acceleration-personnel empowerment’ confirms the dual value of lean management in improving the quality of stroke treatment and laboratory operation efficiency. The survey results show that 90% of the respondents reported having mastered the concept of lean management, indicating its wide dissemination and recognition among laboratory employees. The staff’s mastery of the concept is the basis for implementing lean management and a key factor for the smooth implementation of subsequent improvement measures21. This high proportion of concept mastery has laid a solid cognitive foundation for continuous improvements in the laboratory. Moreover, 70% of the respondents applied the lean management concept to their daily work, reflecting its effective implementation in the stroke testing process. Furthermore, 95% of the respondents were satisfied with the lean management training, indicating its effectiveness and relevance. Through systematic training, employees not only understand the core principles and methodologies of lean management but also master specific operational skills and application tools. Moreover, training increases employees’ self-confidence and sense of belonging, further improving their job satisfaction.
Regarding the implementation effect, 90% of the respondents believed that lean management improved laboratory work efficiency and 80% believed that resource utilisation was more effective. These improvements are mainly attributed to the following aspects: (1) optimisation of the laboratory layout, which reduces the sample transport distance through spatial reorganisation; (2) reconstruction of the detection process, which uses parallel processing and an assembly line operation mode, significantly shortening sample processing time; (3) introduction of automation equipment, which reduces human operation errors and improves detection consistency; and (4) implementation of priority management strategies, which ensures that high-priority samples are processed on time and meet the timeliness requirements of stroke treatment. All respondents agreed that lean management significantly improved the working atmosphere in the laboratory, a finding that highlights the combined effect of improving employee satisfaction and team cohesion. By optimising the laboratory environment, strengthening teamwork and communication, and establishing incentive mechanisms, lean management created a positive, harmonious working atmosphere. This atmosphere not only stimulates the enthusiasm and creativity of employees but also enhances the cohesion and centripetal force of the team. Notably, 95% of the employees rated workflow optimisation positively. Lean management systematically optimises work processes by eliminating non-value-added steps, simplifying workflows, and improving employee work efficiency. Furthermore, all respondents perceived lean management has having a positive effect on the overall performance of the laboratory, which was reflected in shorter laboratory testing cycles, improved work efficiency, optimised resource utilisation, and increased employee satisfaction.
However, some employees had differing opinions regarding the effectiveness of lean management. First, 10% faced difficulties in actively learning and mastering the lean management concept, which may be related to individual cognitive differences and learning abilities. In the future, employees should strengthen their understanding and ability to apply the core concept of lean management through hierarchical classification training and personalised guidance. Second, the poor effectiveness of training (5%) may be related to the training content’s lack of practical relevance. The adoption of diverse training methods such as case teaching and scenario simulation is recommended to enhance practicality and participation in training. Furthermore, 30% of employees did not apply lean management concepts in their daily work, which may be related to practical barriers. The in-depth integration of concepts and practices should be promoted by establishing a mentorship system and practice-sharing platform. The view that the improvement in work efficiency was insignificant (10%) may be related to the adaptation period and intensity in the early stages of implementation. Regarding resource utilisation, 20% of the respondents believed that the improvement was limited, which may be related to the allocation and management mechanism of hardware resources. Further improving the efficiency of resource utilisation by introducing an intelligent resource management system and optimising the consumable supply chain is recommended. Finally, regarding the sustainability of workplace climate improvement, establishing sound communication, feedback mechanisms, and employee care plans to maintain a positive organisational atmosphere is recommended. Notably, a case study at the Jordan Cancer Center revealed that lean management implementation significantly improved employee relationships and motivation22. This finding corroborates the results of this study, highlighting the universal value of lean management in improving organisational effectiveness.
Through the comprehensive staff questionnaire survey, we gained an in-depth understanding of the staff’s level of awareness of lean concepts, training systems, and patient-centred service awareness, which provided key data support for subsequent lean healthcare reform. The results of the survey showed that the staff’s mastery of the lean concept and the efficiency of cross-departmental collaboration substantially improved compared to the pre-lean improvement period. These findings verified the scientific validity of the implementation framework constructed based on the questionnaire survey. As a systematic management strategy, lean management implementation has long-term characteristics and complexity. As experts in the hospital management field stated, ‘Lean theory is very simple, but the practical application is very complete’23. Through empirical evidence, this study found that although lean management in the laboratory has achieved remarkable results, room for improvement remains in optimising the medical process of stroke treatment, such as errors in doctor’s order transmission, standardisation of nurses’ operations, and preservation, transport, and handover of specimens. The results show that the key to reducing delays for in-hospital diagnosis and treatment comprises optimising the patient diagnosis and treatment process, reconstructing the specimen handover mechanism between the clinical and laboratory departments, and ensuring the accurate transmission of test information and timely specimen processing24. This process requires both technological upgrades and efficient collaboration among multidisciplinary teams25.
Extending the concept of lean management from the laboratory department to the entire hospital and building a quality management system covering the full diagnosis and treatment process can systematically improve the quality and safety of medical care. This is in line with the characteristics of this study as a hospital-wide QI initiative. First, from a policy background perspective, the project was not only a strategic quality improvement plan deployed by hospitals through a resolution of the 2022 hospital council but also a necessary measure to meet the certification requirements of the ‘National Health Commission’s Guidelines for the Construction of Hospital Stroke Centers (2024 Edition)’. Second, from a system implementation perspective, because it involves upgrading the information system of the entire hospital and the unified deployment of equipment, realising a differentiated operation of grouping is technically difficult. Implementing this type of whole-hospital intervention for medical quality improvement has objective limitations, which explains the need to promote the construction and implementation of lean management systems on a broader level.
The historical control design adopted in this study has several limitations. First, the data of the control group and the experimental group were from different time periods, which may be affected by environmental factors (e.g. seasonal differences in stroke onset, changes in the experience of medical staff), fluctuations in demographic characteristics (e.g. differences in health consciousness and economic level), and testing standards. Second, the superposition effects of other quality improvement measures implemented during the same period as the system-level intervention are difficult to isolate completely. Third, although this study reduced bias through strict inclusion criteria and time matching, the controlled design may still be affected by unknown confounding factors. Future research should validate the universality of lean management through randomised controlled trials, particularly regarding its application across medical centres. These limitations suggest that the conclusions of this study must be validated in a wider population and healthcare setting to better control for confounding factors and improve the level of evidence. International practice has shown that the King Hussein Cancer Center significantly improved key performance indicators, such as medical quality, operational efficiency, and patient satisfaction, by implementing lean management26. This successful case indicates that the lean transformation of medical institutions must be based on the support and resources of the administrative department, systematic training and employment development plans, and continuous cultural cultivation and concept dissemination mechanisms to jointly build a cultural atmosphere that encourages lean thinking. In the future, the research team will continue to improve follow-up work and explore the in-depth integration of lean management concepts into routine testing projects. An artificial intelligence-assisted diagnostic system and big data analysis technology are planned to increase the accuracy and timeliness of test results. Cross-departmental collaboration can eliminate barriers between departments and establish a patient-centred, integrated stroke emergency service system. This approach will provide innovative solutions to enhance the treatment success rate and quality of care for patients with acute stroke.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author upon reasonable request.
References
Monivas Gallego, E. & Zurita Castillo, M. Mesenchymal stem cell therapy in ischemic stroke trials. A systematic review. Regen Ther. 27, 301–306. https://doi.org/10.1016/j.reth.2024.03.007 (2024).
Saver, J. L. Time is brain—quantified. Stroke 37, 263–266. https://doi.org/10.1161/01.STR.0000196957.55928.ab (2006).
Walter, K. What is acute ischemic stroke. JAMA 327, 885. https://doi.org/10.1001/jama.2022.1420 (2022).
Legere, B. et al. Success with incrementally faster times to endovascular therapy (SWIFT-EVT): a systematic review and meta-analysis. J. Stroke Cerebrovasc. Dis. 33, 107964. https://doi.org/10.1016/j.jstrokecerebrovasdis.2024.107964 (2024).
Chen, H. et al. Endovascular stroke thrombectomy for patients with large ischemic core: a review. JAMA Neurol. 81, 1085–1093. https://doi.org/10.1001/jamaneurol.2024.1513 (2024).
Wang, Y. et al. Efficacy and safety outcomes of tenecteplase versus Alteplase for thrombolysis of acute ischemic stroke: a meta-analysis of 9 randomized controlled trials. J. Neurol. Sci. 458, 122912. https://doi.org/10.1016/j.jns.2024.122912 (2024).
Cucchiara, B. et al. A risk score to predict intracranial hemorrhage after Recombinant tissue plasminogen activator for acute ischemic stroke. J. Stroke Cerebrovasc. Dis. 17, 331–333. https://doi.org/10.1016/j.jstrokecerebrovasdis.2008.04.007 (2008).
Powers, W. J. et al. Guidelines for the Early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50, e344–e418. https://doi.org/10.1161/STR.0000000000000211 (2019).
Emmanuel, I. et al. Laboratory turnaround time of surgical biopsies at a histopathology service in Nigeria. Niger Med. J. 61, 180–183. https://doi.org/10.4103/nmj.NMJ_23_20 (2020).
Rudat, K. S., Henry, J. & Mosley, J. Improving laboratory results turnaround time. Best Pract. Benchmarking Healthc. 1, 301–306 (1996).
Huhs, E., Gliebe, W. & Sendlhofer, G. Qualitative analysis of lean management in healthcare: perspectives of Austrian and Swiss experts. Z. Evid. Fortbild. Qual. Gesundhwes. 143, 8–14. https://doi.org/10.1016/j.zefq.2019.03.003 (2019).
Zdęba-Mozoła, A. et al. Implementation of lean management tools using an example of analysis of prolonged stays of patients in a multi-specialist hospital in Poland. Int. J. Environ. Res. Public. Health. 20, 27256. https://doi.org/10.3390/ijerph20027256 (2023).
Prado-Prado, J. C. et al. Increasing competitiveness through the implementation of lean management in healthcare. Int. J. Environ. Res. Public. Health. 17, 4981. https://doi.org/10.3390/ijerph17144981 (2020).
Marin-Garcia, J. A. et al. The role of value stream mapping in healthcare services: a scoping review. Int. J. Environ. Res. Public. Health. 18, 199. https://doi.org/10.3390/ijerph18010199 (2021).
Improta, G., Borrelli, A. & Triassi, M. Machine learning and lean six Sigma to assess how COVID-19 has changed the patient management of the complex operative unit of neurology and stroke unit: a single center study. Int. J. Environ. Res. Public. Health. 19, 5215. https://doi.org/10.3390/ijerph19095215 (2022).
Tiso, A., Crema, M. & Verbano, C. A framework to guide the implementation of lean management in emergency department. J. Health Organ. Manag. 35, 315–337. https://doi.org/10.1108/JHOM-05-2020-0183 (2021).
Qin, C. et al. Application of lean management in cost control of cerebral infarction single disease in stroke center. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. 31, 637–640. https://doi.org/10.3760/cma.j.issn.2095-4352.2019.05.018 (2019).
Kontautas, E. et al. Lean methodology in health care practice: an example of application for clinical laboratory Urinalysis processing. Lab. Med. 56, 199–211. https://doi.org/10.1093/labmed/lmad123 (2025).
Kanamori, S. et al. Implementation of 5S management method for lean healthcare at a health center in senegal: a qualitative study of staff perception. Glob Health Action. 8, 27256. https://doi.org/10.3402/gha.v8.27256 (2015).
Abdallah, A. A. Healthcare engineering: a lean management approach. J. Healthc. Eng. 2020, 8875902. https://doi.org/10.1155/2020/8875902 (2020).
Bektas, G. & Kiper, F. Applications of lean in human resources management in healthcare. J. Pak Med. Assoc. 72, 532–536. https://doi.org/10.47391/JPMA.22-42 (2022).
Hammoudeh, S. et al. The impact of lean management implementation on waiting time and satisfaction of patients and staff at an outpatient pharmacy of a comprehensive cancer center in Jordan. Hosp. Pharm. 56, 737–744. https://doi.org/10.1177/0018578720931759 (2021).
Froman, M. N. et al. Applying lean principles to create a high throughput mass COVID-19 vaccination site. BMJ Open. Qual. 11, e001617. https://doi.org/10.1136/bmjoq-2021-001617 (2022).
White, B. A. et al. Applying lean methodologies reduces ED laboratory turnaround times. Am. J. Emerg. Med. 33, 1572–1576. https://doi.org/10.1016/j.ajem.2015.07.040 (2015).
Cegłowska, U. et al. Using a lean management approach in acute ischemic stroke management: a systematic review. Postep Psychiatr Neurol. 33, 67–79. https://doi.org/10.5114/ppn.2024.136234 (2024).
Al-Hyari, K. et al. The impact of lean bundles on hospital performance: does size matter. Int. J. Health Care Qual. Assur. 29, 877–894. https://doi.org/10.1108/IJHCQA-11-2015-0134 (2016).
Funding
This work was supported by the National Key Clinical Specialty Scientific Research Project (Z2023044).
Author information
Authors and Affiliations
Contributions
N. M: Conceptualization, Data curation, Investigation, Methodology, Writing – original draft, Writing – review & editing. X.D: Conceptualization, Data curation, Investigation, Writing – original draft. X.T: Data curation, Methodology, Writing – original draft. Z. X: Data curation, methodology, writing – original draft. Q. G: Investigation, Software, Writing – original draft. Y. Y: Data curation, supervision, writing – original draft. K.Y: Supervision, Visualization, Writing – original draft, Writing – review & editing. G. Z: Conceptualization, funding acquisition, supervision, writing – original draft, writing – review & editing.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study strictly followed the ethical guidelines of the World Medical Association Declaration of Helsinki. The study protocol has been approved by the ethics committee of the Second People’s Hospital of Hunan Province (Hunan Provincial Brain Hospital), and all experiments were conducted according to relevant guidelines and regulations.
Informed consent
Due to the retrospective nature of the study, the Ethics Committee of the Second People’s Hospital of Hunan Province (Brain Hospital of Hunan Province) waived the need to obtain informed consent.
Equipment and settings
The figures in this article were drawn using Microsoft Visio Professional Edition 2019. URL: https://visio.iruanhui.com/.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, N., Ding, X., Tang, X. et al. Application of lean management in medical laboratories to help treat patients with acute stroke. Sci Rep 15, 27485 (2025). https://doi.org/10.1038/s41598-025-12955-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-12955-y