Abstract
Erector spinae plane block (ESPB) improves recovery and reduces opioid use, while intraoperative blood pressure variability (IBPV) negatively impacts postoperative outcomes. This study evaluates ESPB’s efficacy in reducing IBPV and improving perioperative outcomes in transforaminal lumbar interbody fusion (TLIF). We retrospectively analyzed TLIF patients with and without ESPB from January 2021 to June 2023. ESPB was performed under ultrasonography guidance by anesthesiologists or operators. Intraoperative arterial blood pressure was assessed. Coefficient of variation (CV) and mean arterial pressure difference (MAPD) were calculated as IBPV metrics. Secondary outcomes included blood loss, operation time, postoperative pain, morphine consumption, time to line removal, and discharge. Sixty patients (30 ESPB, 30 non-ESPB) were included, with median ages of 61.3 and 69.5 years, respectively. The ESPB cohort showed significantly lower MAPD (42.0 mmHg vs. 47.1 mmHg, p = 0.02), CV (13.0% vs. 14.7%, p = 0.01), blood loss (268.3 mL vs. 426.7 mL, p < 0.01), and blood loss per level (105.1 mL vs. 157.6 mL, p = 0.02). ESPB also reduced pain in the recovery room (4.7 vs. 6.7, p < 0.01) and on postoperative day 1 (2.3 vs. 2.8, p < 0.01) and accelerated nutritional recovery (1.7 days vs. 3.0 days, p < 0.01). The only complication was observed in the non-ESPB group. ESPB significantly reduced IBPV, blood loss, and postoperative pain in TLIF. It also resulted in lower morphine consumption and earlier mobilization, though these differences did not reach statistical significance. No ESPB-related complications were observed, supporting its safety and its role as an effective component of perioperative management in spine surgery.
Similar content being viewed by others
Introduction
Spinal fusion surgery is recognized as one of the most painful surgical interventions, ranking second and third among 179 surveyed procedures depending on surgical vertebral levels. The median pain intensity, as measured on the numerical rating scale, hovers around 7>1. This surgery is frequently associated with substantial perioperative pain, which can pose challenges to postoperative rehabilitation and impede the recovery process2.
Erector spinae plane block (ESPB) has gained increasing utilization since 2017, attributed to its efficacy in providing postoperative pain relief, contributing to improved quality of recovery, and enhancing overall patient satisfaction3. Reducing morphine consumption mitigates side effects like nausea and vomiting and facilitates early postoperative mobility. This early ambulation is crucial for minimizing perioperative complications and reducing hospital stay lengths, ultimately fostering improved functional independence upon discharge2.
We observed a noticeable difference in intraoperative blood pressure fluctuations between patients with and without ESPB (Fig. 1). Increased variability in intraoperative blood pressure can lead to fluctuations that threaten end organ perfusion, resulting in potential complications such as endothelial dysfunction, vascular and cardiac hypertrophy, kidney disease, and cerebrovascular dysfunction. Our study aims to explore the effects of combining general anesthesia with ESPB on Intraoperative blood pressure variability (IBPV). In addition, we collect comprehensive data on intraoperative blood loss, operation time, perioperative pain scores, equivalents of morphine consumption, durations of catheter and intravenous (IV) line usage, lengths of hospital stay, and any arising complications. Li et al. highlighted ESPB’s benefits in improving hemodynamic stability, reducing opioid use, and enhancing recovery in elderly hip arthroplasty patients4. However, its impact on intraoperative blood pressure liability in spinal fusion surgery remains underexplored. This study evaluates ESPB’s efficacy in enhancing patient safety and postoperative pain management in spinal fusion.
Methods
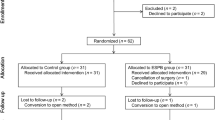
Study design and participants
This retrospective cohort study evaluated the efficacy of ESPB in transforaminal lumbar interbody fusion (TLIF) from January 2021 to June 2023. ESPB was performed using ultrasonography guidance by trained anesthesiologists or operators. Patients with tumors or infections were excluded to focus on ESPB’s effects in primary spinal fusion. Patient demographic and clinical characteristics were recorded, including history of hypertension, arrhythmia, myocardial infarction, congestive heart failure, and cerebrovascular events. In addition, the Charlson Comorbidity Index and ASA physical status classification were documented to assess overall health status and baseline surgical risk. To account for baseline differences between groups, sensitivity analysis was performed in the comparison of key perioperative outcomes. The hypothesis tested whether ESPB fails to reduce IBPV, blood loss, or improve postoperative pain compared to conventional anesthesia.
Study parameters
We analyzed intraoperative arterial blood pressure using Digitizelt software (Digitizelt; Braunschweig, Germany), measuring mean arterial pressure (MAP) at 5-minute intervals. IBPV was assessed via the coefficient of variation (CV) and MAP difference (MAPD), with higher values indicating greater variability. Secondary outcomes included intraoperative blood loss, operation time, postoperative pain scores, morphine use, and recovery milestones such as time to line removal and discharge. Pain scores were recorded in the recovery room, on postoperative day one, and at discharge, while morphine dosage was documented in both the recovery room and ward. Recovery indicators included foley catheter removal upon independent ambulation and IV line discontinuation upon adequate oral intake. Complications were tracked to evaluate safety.
Techniques for ultrasound-guided ESPB block
The patients were placed prone, and landmarks from C7 to L2 were identified for precise needle placement. A sterile, high-frequency ultrasound probe was positioned 3 cm lateral to the L1 spinous process, clearly visualizing the trapezius and erector spinae muscles (Fig. 2). After disinfecting the skin, a local anesthetic was administered to enhance patient comfort.
An 18-G Tuohy needle was inserted in-plane toward the anterior fascial plane of the erector spinae muscle. Placement was confirmed by observing fluid spread beneath the muscle, away from the transverse process. For the ESPB procedure, a total volume of 21 mL was administered per side, consisting of 10 mL of 1% ropivacaine, 1 mL of dexamethasone (5 mg/mL), and 10 mL of normal saline. The procedure was repeated bilaterally for complete analgesic coverage. Additionally, all anesthetic protocols were standardized according to institutional guidelines to minimize variability. These measures were implemented to reduce the influence of potential confounders on our assessment of intraoperative and postoperative outcomes. Vital parameters, including ECG, oxygen saturation, heart rate, and blood pressure, were monitored throughout, with recordings taken at baseline, post-block, and every five minutes for 30 min. Complications, such as hypotension or vascular puncture, were documented to ensure safety and refine procedural techniques.
Perioperative multimodal pain management in both groups
Both ESPB and non-ESPB cohorts employed a preemptive analgesia approach, injecting 20 mL of 1% xylocaine mixed with 10 mL normal saline locally before the skin incision to reduce initial surgical pain. Before wound closure, 2 vials of levobupivacaine were administered subcutaneously to prolong postoperative analgesia.
Postoperative pain management included oral acetaminophen, NSAIDs, and, when appropriate, IV parecoxib and dexamethasone to control pain and inflammation. This multimodal strategy aimed to optimize pain relief, reduce opioid use, and support faster recovery.
Subgroup analysis based on single and multiple level fusion
Subgroup analysis was performed comparing outcomes for single-level (two vertebral bodies) and multiple-level (three or more vertebral bodies) spinal fusions between the ESPB and non-ESPB cohorts, focusing on blood loss, operative time, MAPD, and CV. Given the limited sample size, a post hoc power analysis was performed to assess the statistical strength of the observed effects within each subgroup.
Statistical analysis
Data normality was assessed using the Shapiro-Wilk test and Q-Q plots. Continuous variables were reported as mean (standard deviation, SD) or median (interquartile range, IQR) and analyzed with Student’s t-test or the Mann-Whitney U test, based on distribution. Categorical variables were expressed as numbers (percentages) and compared using chi-squared or Fisher exact tests. Statistical analyses were conducted with SPSS version 29.0.1.0 (IBM Corp., Armonk, N.Y., USA), and a two-sided p-value < 0.05 was considered significant.
Results
In our study, sixty patients were evenly divided into two cohorts of thirty each. The baseline characteristics, including age, sex, operative vertebral levels, and underlying comorbidities, were comparable across both groups. Specifically, the incidences of hypertension, arrhythmia, myocardial infarction, congestive heart failure, and cerebrovascular events were similar. However, the American Society of Anesthesiologists (ASA) physical status classification differed significantly between groups, with a higher proportion of class III patients observed in the non-ESPB cohort. Although the differences did not reach statistical significance, the ESPB group had a younger mean age, a higher proportion of single-level fusions (defined as two operated vertebrae), and a greater prevalence of hypertension. (Table 1).
A significant reduction in IBPV was observed in the ESPB cohort, demonstrated by the MAPD of 42.0 mmHg (IQR = 24.2) compared to 47.1 mmHg (IQR = 13.1) in the control group (p = 0.02), and a CV of 13.0% (IQR = 5.1) versus 14.7% (IQR = 4.2) (p = 0.01).
In the ESPB group, both total intraoperative blood loss and intraoperative blood loss per level were significantly reduced, with mean values of 268.3 ± 174.9 mL compared to 426.7 ± 256.2 mL in the control group (p < 0.01), and 105.1 ± 63.0 mL per level versus 157.6 ± 101.3 mL per level (p = 0.02), respectively. The total operative time and the operative time per level did not differ significantly between the groups, with median durations of 164.5 (IQR = 54.0) minutes versus 178.0 (IQR = 39.8) minutes (p = 0.10), and 66.8 (IQR = 21.3) minutes per level compared to 68.3 (IQR = 20.7) minutes per level (p = 0.82), respectively.
Pain scores in the ESPB group were notably lower immediately after surgery (4.7 ± 2.7 vs. 6.7 ± 1.9, p < 0.01) and on the first postoperative day (2.3 ± 0.6 vs. 2.8 ± 0.8, p < 0.01) compared to the control group. Additionally, patients in the ESPB cohort achieved faster recovery to adequate nutrition, with a significant difference observed (1.7 vs. 3.0 days, p < 0.01) (Table 2).
Although the cumulative morphine requirement in the recovery room and ward was lower in the ESPB group, these differences did not reach statistical significance (p = 0.16 and p = 0.13, respectively). Pain scores at discharge and the duration of Foley catheterization did not differ significantly between the groups.
Within the sensitivity analysis adjusting for ASA physical status classification, statistically significant differences between the ESPB and non-ESPB groups persisted across multiple outcomes. These included MAPD, CV, postoperative pain scores in the recovery room and on postoperative day one, intravenous fluid supplementation, intraoperative blood loss, and blood loss per level (all p < 0.05). Surprisingly, the duration of Foley catheter usage was significantly shorter in the ESPB group compared to the non-ESPB group (1.8 vs. 2.2 days; p = 0.04), suggesting faster recovery to mobility.
Importantly, there were no instances of block failure or block-related complications reported. No complications were observed in the ESPB cohort. In contrast, one non-ESPB patient developed left ankle dorsiflexion weakness caused by hematoma-induced neural compression. This condition necessitated surgical evacuation, and full recovery was achieved by the six-month follow-up period. Furthermore, no patients in the ESPB group experienced nausea and vomiting requiring medication, highlighting the potential benefits of ESPB in enhancing postoperative recovery and reducing the incidence of complications.
In the single-level fusion subgroup, ESPB significantly reduced operative time per level by 14.7 min (68.8 min vs. 83.5 min, p < 0.01), with an effect size of 1.06 and estimated power of 68%, indicating a moderately strong association. Reductions in blood loss (75 mL) and blood loss per level also showed moderate power of approximately 66%, though not statistically significant. In contrast, MAPD and CV showed minimal differences with low effect sizes (0.15) and power (< 6%), indicating negligible impact. In the multiple-level fusion subgroup, ESPB was associated with significantly lower MAPD (36.5 vs. 47.1 mmHg, p < 0.01) and CV (11.7% vs. 14.7%, p < 0.01), with high statistical power (97.4% and 95%, respectively), supporting a robust effect on hemodynamic control. Although blood loss was lower in the ESPB group (275 vs. 400 mL, p = 0.06), the associated power was low (22–25%). Differences in operative time and operative time per level were not significant and underpowered (≤ 16%). These findings suggest that ESPB may meaningfully enhance intraoperative hemodynamic stability in multi-level fusion, while its impact on other outcomes requires further investigation (Table 3).
Discussion
In our study, most patients were 65 years old. ESPB was associated with a significant reduction in IBPV and intraoperative blood loss without extending surgical time. Additionally, ESPB significantly decreased postoperative pain, particularly immediately after surgery and on the first postoperative day, while also reducing the need for nutritional supplementation. However, pain scores at discharge were similar between groups. Although morphine consumption in the recovery room and ward was not significantly reduced, ESPB was associated with earlier removal of the Foley catheter after adjustment for ASA physical status classification, suggesting a faster recovery of functional mobility. Notably, no adverse events occurred in the ESPB group. In contrast, one patient in the non-ESPB group experienced dorsiflexion weakness due to hematoma-induced nerve compression, which required surgical evacuation and improved during follow-up. These findings underscore the potential of ESPB as an effective add-on strategy for perioperative pain management, hemodynamic, and recovery enhancement, without introducing additional complications.
Although intraoperative blood pressure can fluctuate on a second-to-second basis, especially during spinal procedures like TLIF, the use of 5-minute interval monitoring remains a validated and clinically meaningful approach for assessing blood pressure variability. Prior studies have demonstrated that variability measured over 5-minute intervals is significantly associated with outcomes such as postoperative mortality and acute kidney injury5,6. This interval allows for the detection of sustained hemodynamic trends while minimizing the influence of transient artifacts. While high-frequency or continuous monitoring may offer additional granularity, the 5-minute resolution used in this study aligns with standard anesthetic recordkeeping and supports the practical and reproducible assessment of ESPB’s effect on intraoperative hemodynamic stability.
Various definitions of IBPV in the literature6,7,8,9 complicate cross-study comparisons. SD is commonly used as it reflects data dispersion from the mean and offers a straightforward measure of variability. However, the CV, which normalizes SD to the mean, has gained traction for its ability to facilitate comparisons across studies with diverse scales and units10. This normalization facilitates more meaningful comparisons, making the CV a particularly useful tool for synthesizing and interpreting IBPV data from different research endeavors.
First described in 2016 by Forero et al., ESPB has proven effective in managing rib neuropathic pain11. The ESPB regimen varies among operators. Ropivacaine was selected for its favorable pharmacologic profile, offering effective sensory blockade with minimal motor impairment and a lower risk of cardiotoxicity compared to bupivacaine. The addition of dexamethasone was intended to prolong the duration of analgesia, based on its established efficacy as an adjuvant in regional anesthesia12. In our study, ESPB significantly reduced pain scores immediately post-operation (4.7 vs. 6.7) and on postoperative day one (2.3 vs. 2.8), aligning with prior studies showing reduced pain and morphine use within the first 12 hours13,14. Comparable pain scores were noted at discharge. Though not statistically significant, the ESPB group features lower rescue opioid use in the recovery room (3.5 mg vs. 4.8 mg, p = 0.11) and required no ward-administered morphine, unlike the control group (1.2 mg). Beyond its analgesic effects, ESPB may offer important intraoperative hemodynamic benefits. Anatomical and cadaveric studies have demonstrated that local anesthetic administered via ESPB can spread to the paravertebral and epidural spaces, affecting the dorsal and ventral rami as well as the sympathetic chain15,16. This broad neural blockade is thought to modulate sympathetic tone and blunt the physiological stress response to noxious surgical stimuli. In our study, this was reflected in significantly lower MAPD and CV in the ESPB group, particularly in multi-level fusion cases where autonomic load is greater. These findings suggest that ESPB may contribute to improved intraoperative stability, potentially reducing the risk of end-organ hypoperfusion, excessive blood loss, and complications related to hemodynamic fluctuations.
In our study, ESPB was associated with reduced MAPD (42.0 mmHg vs. 47.1 mmHg) and lower CV (13.0% vs. 14.7%), indicating diminished intraoperative blood pressure fluctuation. Elevated IBPV, regardless of the presence of hypotension, has the potential to induce perfusion disturbances. Alterations in blood pressure may surpass the adaptive capacity, leading to insufficient simultaneous neurohormonal and vascular responses10. IBPV has been identified as a negative prognostic factor in numerous studies. For instance, Bencivenga et al. linked increased blood pressure variability to cardiovascular events, stroke, cognitive impairment, and other adverse outcomes17. Wiórek et al. demonstrated that a CV exceeding 13.6% increased the risk of postoperative mobility issues by 3.5 times in noncardiac surgery18while Park et al. associated higher CV with postoperative acute kidney injury6. Similarly, IBPV correlated with an increased risk of postoperative delirium in patients undergoing hip fracture fixation9. In our study, total blood loss and blood loss per vertebra were significantly lower in the ESPB group. Additionally, the only complication—muscle weakness secondary to nerve compression—occurred in the non-ESPB group, though improved after hematoma evacuation.
Subgroup analysis further highlighted ESPB’s benefits in both single-level and multiple-level spinal fusions. For single-level fusions, ESPB was associated with reduced operative time per vertebra (68.8 min vs. 83.5 min, p < 0.01). While a 14.7 min reduction in operative time per level is statistically significant, its clinical relevance may vary depending on surgical context, particularly in high-volume or resource-limited settings where even modest efficiency gains can translate to reduced anesthesia exposure. In multiple-level fusions, ESPB significantly improved hemodynamic stability, evidenced by lower MAPD (36.5 mmHg vs. 47.1 mmHg, p < 0.01) and CV (11.7% vs. 14.7%, p < 0.01). These findings suggest ESPB’s advantages in maintaining hemodynamic control, particularly in extensive procedures.
Importantly, our study mainly focused on intraoperative hemodynamic stability—an area less explored in ESPB research. Unlike prior ESPB studies centered on hip arthroplasty or decompression surgeries, our data suggest that ESPB may help mitigate hemodynamic fluctuations during prone-positioned, longer-duration TLIF surgeries, where autonomic stress is prominent. This distinguishes our findings and highlights a potentially underrecognized benefit of ESPB in major spine surgery.
Recent comparative studies have explored how ESPB performs relative to other regional anesthesia techniques in spine surgery. Compared with the thoracolumbar interfascial plane (TLIP) block, ESPB has been shown in several randomized trials to provide similar or even superior postoperative analgesia. Dilsiz et al. found that ESPB led to significantly lower opioid consumption and pain scores at 24 h compared to TLIP in lumbar discectomy patients, along with earlier mobilization19. However, a recent meta-analysis involving five randomized controlled trials concluded that ESPB and TLIP provided comparable efficacy in terms of postoperative pain scores and 24-hour morphine consumption, with no statistically significant differences between them20. Additionally, when compared to caudal epidural block (CEB), ESPB appears to offer longer-lasting postoperative pain control and was associated with reduced intraoperative blood loss and surgical duration in lumbar fusion cases21. While each technique has unique anatomical targets and practical considerations, the current evidence suggests that ESPB is a versatile and effective option. While ESPB was not directly compared to other regional techniques in this study, it offers practical advantages including ease of administration, lower procedural risk, and effective multi-dermatomal coverage. Future head-to-head comparisons are warranted to determine whether ESPB offers superior clinical benefit or is simply more feasible.
Pain management is essential in spine surgery. Bae et al. identified triple-drug therapy—paracetamol, NSAID, and an adjunct like gabapentinoids—as the most effective intervention22. The rise of regional blocks has enabled advancements like “awake spinal fusion” and “enhanced recovery after surgery” (ERAS)23. Dietz et al. found ERAS reduces complications, readmissions, hospital stay, and opioid use while improving functional recovery24. The ERAS® Society highlighted ESPB’s role in reducing morphine-related nausea, supporting early nutrition, and promoting mobilization25. In our study, ESPB provided immediate pain relief, reduced IV line use, and enabled earlier dietary intake. Though not statistically significant, it also revealed lower morphine use and shorter foley catheter duration, indicating faster recovery.
Taken together, our findings suggest that ESPB may contribute meaningfully to both intraoperative physiologic stability and postoperative recovery in TLIF surgery, though further large-scale studies are needed to confirm these benefits and compare ESPB to alternative block techniques.
Limitations
This study is the first to examine ESPB’s effects on IBPV in spinal fusion, but several limitations must be noted. First, intraoperative blood pressure was recorded at five-minute intervals, which, while adequate for an overview, lacked the precision of more frequent measurements. Second, while ESPB reduced blood pressure variability, blood loss, pain scores, and recovery times, a direct causal relationship could not be established, warranting further investigation. Third, the small subgroup sample sizes limited the statistical power of findings on hemodynamic stability in multiple-level fusions. Fourth, two patients in the non-ESPB cohort were excluded from the Foley catheter usage comparison: one due to difficult catheter insertion requiring cystofix placement, and the other due to end-stage renal disease on hemodialysis with anuria. Another limitation of this study is the lack of long-term follow-up data. Our analysis focused on the immediate postoperative period, from postoperative day one through discharge, without evaluating outcomes beyond hospitalization. As a result, we were unable to assess the sustained effects of ESPB on chronic pain, long-term opioid use, functional recovery, or quality of life. Future prospective studies with extended follow-up—such as at one month and three months postoperatively—are warranted to better understand the durability of ESPB’s analgesic benefits and its potential role in enhancing long-term recovery after spinal fusion surgery. Lastly, the retrospective design restricts the ability to draw causal conclusions. We acknowledge that conducting a RCT is both well-founded and essential. This retrospective study serves as a pivotal foundation for the design of our upcoming RCT. The clinical evidence generated provides critical support for IRB approval and informs the methodological planning of the prospective trial. These preliminary findings enhance our ability to justify and refine the design of a rigorous, high-quality RCT aimed at further evaluating the efficacy of ESPB in spinal fusion surgery.
Conclusions
ESPB improves perioperative management in spinal fusion surgery by reducing intraoperative blood pressure variability, minimizing blood loss, and alleviating postoperative pain, all without increasing complication rates. Subgroup analyses revealed procedure-specific advantages: ESPB shortened operative time in single-level fusions and provided superior hemodynamic control and reduced blood loss in multiple-level fusions. Although differences in morphine consumption and time to mobilization did not reach statistical significance, observed reductions support the potential role of ESPB in enhanced recovery protocols. These findings underscore ESPB as a promising adjunct in spinal fusion surgery, meriting further prospective, randomized studies to validate its clinical benefits and inform optimal implementation.
Data availability
The dataset generated and analyzed during the current study is available; it is added to the submission of this manuscript as a separate file.
Abbreviations
- CV:
-
Coefficient of variation
- ESPB:
-
Erector spinae plane block
- IBPV:
-
Intraoperative blood pressure variability
- IQR:
-
Interquartile range
- IV:
-
Intravenous
- MAPD:
-
Mean arterial pressure difference
- SD:
-
standard deviation
- TLIF:
-
Transforaminal lumbar interbody fusion
- ASA:
-
American Society of Anesthesiologists
References
Gerbershagen, H. J. et al. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology 118, 934–944 (2013).
Adogwa, O. et al. Early ambulation decreases length of hospital stay, perioperative complications and improves functional outcomes in elderly patients undergoing surgery for correction of adult degenerative scoliosis. Spine (Phila. Pa.) 42, 1420–1425 (2017).) 42, 1420–1425 (2017). (1976).
Ní Eochagáin, A., Singleton, B. N., Moorthy, A. & Buggy, D. J. Regional and neuraxial anaesthesia techniques for spinal surgery: a scoping review. Br. J. Anaesth. 129, 598–611 (2022).
Li, Q., Zhang, L., Zhou, H. M. & Wu, X. W. Ultrasound-guided erector spinae plane block in elderly patients undergoing total hip arthroplasty: A triple-blind, randomized controlled trial. J. Arthroplasty. https://doi.org/10.1016/j.arth.2024.10.052 (2024).
James, L. A., Levin, M. A., Lin, H. M. & Deiner, S. G. Association of preoperative frailty with intraoperative hemodynamic instability and postoperative mortality. Anesth. Analg. 128, 1279–1285 (2019).
Park, S. et al. Intraoperative arterial pressure variability and postoperative acute kidney injury. Clin. J. Am. Soc. Nephrol. 15, 35–46 (2020).
Hirsch, J., DePalma, G., Tsai, T. T., Sands, L. P. & Leung, J. M. Impact of intraoperative hypotension and blood pressure fluctuations on early postoperative delirium after non-cardiac surgery. Br. J. Anaesth. 115, 418–426 (2015).
Benolken, M. M., Meduna, A. E., Klug, M. G. & Basson, M. D. Preoperative and intraoperative blood pressure variability independently correlate with outcomes. J. Surg. Res. 266, 387–397 (2021).
Zhang, C. et al. Association between intraoperative mean arterial pressure variability and postoperative delirium after hip fracture surgery: a retrospective cohort study. BMC Geriatr. 23, 735 (2023).
Putowski, Z., Czok, M. & Krzych, Ł. J. The impact of intraoperative blood pressure variability on the risk of postoperative adverse outcomes in non-cardiac surgery: a systematic review. J. Anesth. 36, 316–322 (2022).
Forero, M., Adhikary, S. D., Lopez, H., Tsui, C. & Chin, K. J. The erector spinae plane block: A novel analgesic technique in thoracic neuropathic pain. Reg. Anesth. Pain Med. 41, 621–627 (2016).
An, K., Elkassabany, N. M. & Liu, J. Dexamethasone as adjuvant to bupivacaine prolongs the duration of thermal antinociception and prevents bupivacaine-induced rebound hyperalgesia via regional mechanism in a mouse sciatic nerve block model. PLoS One. 10, e0123459 (2015).
Zhang, Q., Wu, Y., Ren, F., Zhang, X. & Feng, Y. Bilateral ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal fusion: A randomized controlled trial. J. Clin. Anesth. 68, 110090 (2021).
Singh, S., Choudhary, N. K., Lalin, D. & Verma, V. K. Bilateral ultrasound-guided erector spinae plane block for postoperative analgesia in lumbar spine surgery: A randomized control trial: A randomized control trial. J. Neurosurg. Anesthesiol. 32, 330–334 (2020).
Ma, J. et al. Erector spinae plane block for postoperative analgesia in spine surgery: a systematic review and meta-analysis. Eur. Spine J. 30, 3137–3149 (2021).
Pawa, A., King, C., Thang, C. & White, L. Erector spinae plane block: the ultimate ‘plan A’ block? Br. J. Anaesth. 130, 497–502 (2023).
Bencivenga, L. et al. Blood pressure variability: A potential marker of aging. Ageing Res. Rev. 80, 101677 (2022).
Wiórek, A. & Krzych, Ł. J. Intraoperative blood pressure variability predicts postoperative mortality in non-cardiac surgery-A prospective observational cohort study. Int. J. Environ. Res. Public. Health. 16, 4380 (2019).
Dilsiz, P. et al. A comparison of the effects of thoracolumbar interfascial plane (TLIP) block and erector spinae plane (ESP) block in postoperative acute pain in spinal surgery. Eur. Spine J. 33, 1129–1136 (2024).
Khor, W. T. et al. Erector spinae plane block versus thoracolumbar interfascial plane block in lumbar spine surgery: A meta-analysis of randomized controlled trials. Global Spine J. 15, 1367–1374 (2025).
Patel, Y. et al. Comparison between relative efficacy of erector spinae plane block and caudal epidural block for postoperative analgesia in lumbar fusion surgery- A prospective randomized controlled study. Global Spine J 21925682231203653 (2023).
Bae, S. et al. Efficacy of perioperative Pharmacological and regional pain interventions in adult spine surgery: a network meta-analysis and systematic review of randomised controlled trials. Br. J. Anaesth. 128, 98–117 (2022).
Garg, B., Ahuja, K. & Sharan, A. D. Regional anesthesia for spine surgery. J. Am. Acad. Orthop. Surg. 30, 809–819 (2022).
Dietz, N. et al. Enhanced recovery after surgery (ERAS) for spine surgery: A systematic review. World Neurosurg. 130, 415–426 (2019).
Debono, B. et al. Consensus statement for perioperative care in lumbar spinal fusion: enhanced recovery after surgery (ERAS®) society recommendations. Spine J. 21, 729–752 (2021).
Acknowledgements
We extend our heartfelt gratitude to the Anesthesiology Department for their invaluable support in the design of our study. Their expertise in the ESPB technique and their commitment to ensuring intraoperative safety were instrumental in the success of our research.
Author information
Authors and Affiliations
Contributions
Wei-Cheng Chen participated in conceptualization, data curation, formal analysis, methodology, software, and writing original and revision draft. Ping-Yeh Chiu participated in conceptualization, methodology, project administration, resources, supervision, validation, and review and editing. Fu-Cheng Kao, Tsung-Ting Tsai, Chi-Chien Niu, Lih-Huei Chen, and Po-Liang Lai are all contributed to supervision, validation and review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Ethical approval was not required for this study as determined by the local Ethics Committee of Chang Gung Memorial Hospital, given its retrospective design and the fact that all procedures were conducted as part of standard clinical practice.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, WC., Tsai, HI., Kao, FC. et al. Effects of erector spinae plane block on intraoperative blood pressure variability, blood loss, and postoperative pain in transforaminal lumbar interbody fusion. Sci Rep 15, 27721 (2025). https://doi.org/10.1038/s41598-025-13518-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-13518-x