Abstract
Background
Rear-foot eversion increases the patellofemoral joint stress through the mechanism of lower extremity coupling. Therefore, the present clinical trial aimed to evaluate the effects of altering walking foot strike pattern in combination with lower extremity strengthening on lower limb alignment in females with patellofemoral pain (PFP).
Methods
Forty women with PFP were randomly assigned to experimental (n = 20) and control groups (n = 20). For 8 weeks, the experimental group received the forefoot strike pattern combined with foot-knee strengthening exercises. Versus, the control group during 8 weeks did not receive any intervention aimed at treating PFP. The primary outcome was self-reported pain. The secondary outcome was rear-foot eversion, dynamic knee valgus (DKV), pelvic drop, hip extensor, hip abductor, and knee extensor muscle strength, which were measured before and after 8 weeks. Covariance analysis was used to compare the results between the two groups.
Results
A significant difference was observed in reduced pain (P < 0.001, η2 = 0.884), rear-foot eversion (P < 0.001, η2 = 0.880), DKV (P < 0.001, η2 = 0.740), and pelvic drop (P < 0.001, η2 = 0.540). In addition, a significant difference was observed in the increase in the muscle strength of the hip extensor (P < 0.001, η2 = 0.743), hip abductor (P < 0.001, η2 = 0.770), and knee extensor (P < 0.001, η2 = 0.811).
Conclusion
Eight weeks the lower limb strengthening and changes in foot strike during walking can have clinical importance in reducing self-reported pain, rear-foot eversion, DKV, and pelvic drop during a single leg squat.
Similar content being viewed by others
Introduction
Patellofemoral pain (PFP) is defined as pain around or behind the patella that is exacerbation during patellofemoral joint loading tasks such as stair climbing, squatting, and running 1,2. The prevalence of PFP in the general population has been reported as 22.7% and women experience PFP 2.23 times more than men 3. The exact etiology of PFP remains unclear. However, patellofemoral joint stress is a common hypothesis in the pathophysiology of PFP that is influenced of distal (foot) and proximal (hip) mechanics 4,5,6.
A systematic review and meta-analysis showed that foot pronation is a risk factor for PFP 7. Foot pronation leads to internal rotation of the tibia that could induce a compensatory medial rotation of the femur to maintain the relative lateral rotation of the tibia plateau about the femoral condyles associated with knee extension 8. As a result, the dynamic knee valgus (DKV) increases and subsequently diminishes the activation of some stabilizing muscle activity such as the gluteus maximus (GMAX), gluteus medius (GMED), and vastus medialis Oblique (VMO) 3. Theoretically, DKV is a faulty movement pattern that increases patellofemoral joint stress by reduced patellofemoral joint contact area 9. Therefore, by understanding the role of the foot in great patellofemoral joint stress, foot interventions may correct knee faulty movement and ultimately reducing the patellofemoral joint stress.
Interventions to control foot pronation in patients with PFP are focused on active strengthening exercises and foot orthoses 10. However, interventions that reduce pronation, such as orthoses, do not reduce patellofemoral joint stress 11. Often, active exercises that are used to strengthen the intrinsic foot muscles and reduce foot pronation include picking up objects, towel toe curls, and short foot exercises 10. The previous studies showed that adding foot exercises to knee exercises is more effective in improving clinical outcomes than knee exercises alone in patients with PFP 2,12. In this line, Kısacık et al. (2021) reported that adding short-foot exercise to knee and hip exercises had positive effects on rear-foot posture, and knee pain in patients with PFP 12. However, the traditional interventions may not improve the movement impairment 13. Movement impairment is proposed to result from the repetitive use of alignments and movements abnormal that over time are proposed to become impaired and eventually induce patho-anatomical changes in tissues and joint structures that finally develop injury and pain 14. For example, DKV is a movement impairment pattern that contributes to the etiology or exacerbation of PFP 15. This issue highlights the necessity of gait retraining applications to improve the faulty movement pattern in patients with PFP.
A systematic review reported that gait retraining should be part of the rehabilitation programs of patients with PFP when a faulty movement pattern is observed 16. Clinical trials have shown that the forefoot strike pattern can reduce patellofemoral joint stress and may be beneficial for the rehabilitation of PFP 17,18. For example, Roper et al. (2016) reported that the forefoot strike pattern reduced knee pain and can be considered as a strategy for PFP management 17. Overall, there is still no strong evidence to confirm whether gait retraining can promote the effect of exercise therapy on the rehabilitation outcomes of PFP patients 13. To our knowledge, no randomized controlled trial has yet trialed the effect of a forefoot strike pattern combined with foot-knee strengthening exercises on the lower limb alignment in patients with PFP. Therefore, the present clinical trial aimed to evaluate the effects of altering walking foot strike pattern in combination with lower extremity strengthening on lower limb alignment in females with PFP. We hypothesized that after 8 weeks of a rehabilitation program, self-reported pain, rear-foot eversion, DKV, and pelvic drop would decrease and muscle strength of hip extensor, hip abductor, and knee extensor would increase.
Methods
Study design
This study was a double-blind randomized controlled trial (patients/ assessors) that lasted from April to July 2023. Forty women with PFP were randomly assigned to the experimental and control groups. The experimental group received the rehabilitation protocol (forefoot strike pattern with foot-knee exercises) for 8 weeks, while the control group did not receive any intervention. Outcome measures were self-reported pain as the primary outcome and secondary outcomes were rear-foot eversion, DKV, pelvic drop, muscle strength of hip extensor, hip abductor, and knee extensor that were evaluated before and after 8 weeks.
Trial registered
The present clinical trial was approved by the ethics committee of Bu-Ali Sina University (R.BASU.REC.1402.012). The trial was registered in the Clinical Trials Registry Iran (IRCT20230425057991N1) on 08/06/2023. All methods were performed according to the relevant guidelines and regulations. Also, this study adhered to the ethical principles of the 2013 Declaration of Helsinki.
Participants
The statistical population of this clinical trial was women with PFP who were recruited from orthopedic and physiotherapy clinics in Hamedan province. First, an orthopedic clinician (≥ 15 years of experience) screened the patients with Clark’s and step-down tests, and then a physiotherapist examined the eligibility criteria. Inclusion criteria included insidious onset of PFP, self-reported pain of 3 out of 10 visual analog scale (VAS) during daily activities, pain exacerbation during weight-bearing activities, ordinary active people, normal static alignment of upper and lower limbs, the age range of 18 to 45, right foot dominant (determined by a kicking ball test), PFP in the right knee, suffering from PFP for more than 6 weeks, and rear-foot eversion ≥ 5 degrees during single-leg squat. More specifically, we used calipers and goniometers to assess static posture of the foot (flat feet, pes cavus, hallux valgus), the knee (genu varus, genu valgus, genu rectum), as well as flexible rulers and a scoliometer were used to assess spinal posture (kyphosis, lordosis, scoliosis). In assessing the foot alignment, a navicular drop of more than 10 mm is considered as flat feet, and less than 4 mm is known as pes cavus 19. Moreover, hallux valgus was diagnosed if the lateral deviation of the great toe at the metatarsophalangeal joint was more than 15 degrees 20. In assessing the knee alignment, a distance of more than 3cm between the two knees in a standing position was considered genu varus, and a distance of 4cm between the two medial malleoli was considered genu valgus 21. In addition, knee extension of more than 5 degrees in the standing position was considered as genu rectum 22,23. In assessing the spinal alignment, thoracic kyphosis greater than 45 degrees was considered hyperkyphosis, and lumbar lordosis greater than 42 degrees was considered hyperlordosis 24,25. In addition, cervical lordosis greater than 40 degrees was defined as cervical hyperlordosis 26. If scoliometer measurements were positive namely an angle greater than 7 degrees, scoliosis was diagnosed 27. Exclusion criteria included a history of physical therapy up to 2 months before participating in clinical trial, participation in championship and recreational sports, surgery history, upper and lower limbs malalignment, lower limb length discrepancy, history of balance problems, vestibular and vision disorders, patella instability, left foot dominant, PFP in the left knee and pain in other joints. Of note, anatomic leg length discrepancy is defined as the anatomical difference between the lengths of the anterior superior iliac spine (ASIS) and the medial malleolus 28,29. Patients were asked to lie supine. Then, the assessor measured the distance between the ASIS and the medial malleolus using a tape measure 28,29. In addition, we obtained information about the history of falls, imbalance in daily life, education level, etc. through a comprehensive questionnaire. With the confidence of diagnosing PFP and having eligibility criteria, patients were invited to the sports rehabilitation laboratory. Before data collection, all patients signed informed consent for voluntary participation in this clinical trial.
Interventions
The rehabilitation program was designed for 8 weeks with 6 sessions per week. The exercise program was under the supervision of two physiotherapists in the rehabilitation center of the university. The rehabilitation protocol included 1) foot-knee exercises and 2) gait retraining based on the forefoot strike pattern, each of which was supervised by a separate physiotherapist.
Safety considerations
Regarding safety considerations, in each session pay attention to exercise-related side effects (e.g. pain, disability signs). The assessment of side effects was done individually. The researchers planned to modify the exercises if the severity of pain and disability increased compared to the previous session or to eliminate the exercise that exacerbated the clinical symptoms. Of note, no adverse events occurred during the intervention.
Foot-knee exercises
The foot-knee exercises were according to previous clinical trials 2,30. The foot-knee strengthening exercises were designed for 8 weeks, 3 times a week and each session lasted 60 min (even days). The foot exercises included posterior tibia strengthening, heel raises, and short foot 2. These exercises as isolation strengthen the intrinsic foot muscles. The knee exercises were focused on isolation strengthening of the quadriceps muscles. The knee exercises consisted of straight-leg raises in the supine position, supine terminal knee extensions (from 10° of flexion to full extension), and a mini-squat (45° of flexion) with the back supported against the wall 30. The foot-knee exercise program was matched in dosage and progression. The initial dosage was 3 sets of 10 repetitions for all exercises, with progression to a maximum of 3 sets of 20 repetitions 2,30. Each repetition was performed dynamically over 2 to 3 s, with a 2-s pause between repetitions 30. The exercise dosage was planned once a week by the physiotherapist according to the level of performance and personal progress. A dosage was chosen in which the last repetitions were difficult while still allowing the patient to maintain high-quality movement control throughout the entire program 30.
Foot strike pattern
The gait retraining was designed for 8 weeks, 3 times a week and each session lasted for the first 15 min, and with progress, it increased to 30 min (odd days) 31. First, patients were taught by verbal instructions to strike with the forefoot while walking on the treadmill, and rear-foot contact after foot strike was optional after the first contact 31. Furthermore, feedback was provided to the patient through a mirror and text expressions such as “walking on your toes” or “walking on the balls of your foot” 17. A physical therapist visually confirmed that the patients were using a forefoot strike. During weeks 1–4, continuous feedback was provided to the patients, and from weeks 4–8, the feedback was gradually removed. The patients wore their shoes during the gait retraining sessions and walking velocity was set similar to the daily activities. This velocity was set throughout walking on a treadmill. At the end of each session, patients reported the level of effort to execute and the naturalness of the forefoot strike pattern on a 10-point scale as changing to a forefoot strike during walking is not a normal strike pattern and people may find this unnatural (“1” very hard/abnormal and “10” easy/normal execution) 17.
Quality control
The exercise program was under the supervision of four physiotherapists who have 8 years of clinical experience.; these physiotherapists were responsible for exercise and supervision. Two physiotherapists provided an exercise program for participants in the rehabilitation center of the university. After the participants fully mastered the exercises, two other physiotherapists who had received an advanced exercise program took charge of the group to continue to administer training and supervise the implementation of the exercise plan. The physiotherapists provided weekly guidance to ensure that participant movements were standardized and that the desired exercise intensity was reached. The measurements and medical advice were all free. Sometimes, we gave some small gifts (clothes, towels, etc.) to encourage the participants to adhere to the continued participation in treatment sessions.
Outcome measures
Outcome measures were assessed before (baseline) and after 8 weeks (post-intervention) by three physiotherapists (> 8 years of experience) in the sports rehabilitation laboratory of Bu-Ali Sina University, Hamedan.
Primary outcome
The primary outcome was self-reported pain that was assessed with a VAS (10 cm) (ICC = 0.91) 32, where 0 corresponds to no pain and 10 corresponds to the worst imaginable pain. Patients were asked to indicate the average pain experienced over the last week on the VAS scale. A minimal clinically important difference (MCID) for pain reduction of 2 points was reported 13.
Secondary outcome
The secondary outcome was rear-foot eversion, DKV, pelvic drop, muscle strength of hip extensor, hip abductor, and knee extensor. Two-dimensional video was recorded with a Sony Handycam digital camera (DCR-HC37) with a 40 Hz sampling rate and 10 optical zoom. Two-dimensional motion analysis is acceptable for measuring lower-extremity alignment 33. A digital video camera was placed at a distance of 3 m from the front and another camera was placed at a distance of 3 m behind the patient.
Markers were attached to the ASIS on both sides, the center of the patella, the center of the malleolus, and the center of the insertion of the Achilles tendon. Patients perform squats in 5 s with a standard velocity at 60° of knee flexion 34. Of note, we used a counter and a flexible electro-goniometer to control the time and knee joint angle, respectively. The first count was for the start of the squat, the third count was for the lowest point of the squat, and the fifth count was for the return to the starting position 34. Trials were accepted if patients squatted at 60° of knee flexion and maintained balance. A 2-min rest was considered to minimize fatigue 35. We set a flexion angle of 60 ◦ for data collection for several reasons. Firstly, high patellofemoral joint stress occurs between angles of 0 ◦ to 60 ◦ of knee flexion, and at 70° to 110° of knee flexion patellofemoral joint stress is very little 36. Secondly, 60 ◦ of knee flexion has been highlighted as a pertinent angle in PFP pathology, and the significance of this angle was underlined by functional motion analysis 37. Thirdly, and eventually, most of the daily activities are performed at the knee flexion angle between 20◦ to 60 ◦ 37.
The rear-foot eversion angle, DKV, and pelvic drop were calculated with Quinoa software (ICC = 0.99) 38 version 33 at 60 ◦ of knee flexion. Quinoa is a valid and reliable software method that measures in an accurate way at distances up to 5 m from the subject with an angle range of 45◦ – 90◦ 38. The angle subtended between the lines that formed the insertion of the Achilles tendon to the vertical line was recorded as the rear-foot eversion angle 39 (Fig. 1). The angle subtended between the lines formed between the markers at the ASIS and middle of the tibiofemoral joint and that formed from the markers on the middle of the tibiofemoral joint to the middle of the malleolus was recorded as the DKV angle 34 (Fig. 1). Pelvic drop angle was calculated as 90° minus the angle between the pelvis and the hip segment 40 (Fig. 1). Previous studies reported MCID for foot pronation at 4.71°, knee valgus at 2.76° 41, and pelvic drop at 5° 42,43.
We used the Nicholas Hand Held dynamometer (NHHD) (ICC = 0.89–0.94) 37 model 01,163 Lafayette instrument to measure muscle strength of the hip abductor, hip extensor, and knee extensor. Hip abductor strength was measured when the patient was placed in a side-lying position on the treatment table with the testing limb on top. A pillow was placed between the legs to provide a neutral position on the hip 37. The assessor placed a dynamometer on the lateral femoral condyle, and the patient performed the maximum voluntary isometric contraction (MVIC) 37. Hip extensor strength was measured when the patient was placed in a prone position and the knee was at 90° flexion 44. The assessor placed a dynamometer on the distal part of the hip 2 cm above the femoral epicondyle and the patient performed the MVIC 13.
The quadriceps strength was measured when the patient was sitting and the hip and knee were in the resting position (the hip and knee flexed to 90˚). The assessor placed the dynamometer in the midpoint of the malleolus and the patient performed the MVIC 37. The assessor provided verbal encouragement to the patient to maintain the MVIC initially showed during the trial. For all muscle strength trials, the patient performed 3 MVIC for 5 s, with 2 min of rest between each trial, and 5 min of rest was considered between the tests 13,37. The average force from 3 trials was normalized according to the body mass of the patient (strength (N)/body mass (kg) × 100).
Sample size
We used the free Power*G software version 3.1.9.2 (https://gpower.macupdate.com) to calculate an a priori power analysis with the F-test family (ANCOVA: fixed effects, main effects, and interactions) and the effect size of a related study that examined the effect of foot-knee exercises on the rear-foot eversion in patients with PFP. Power analysis was calculated with an assumed Type I error of 0.05, Type II error of 0.20 (statistical power of 80%), and effect size of 0.85 12. The analysis showed that 31 participants are required. However, with a dropout probability of 30% and increased statistical power, we recruited 40 women with PFP (age: 39.17 ± 3.78 years, height: 169.68 ± 4.68 cm, weight: 59.18 ± 3.96kg, BMI: 20.61 ± 1.89).
Randomization and blinding
Randomization and blinding were conducted by two physiotherapists who were not involved in data collection and were not aware of the study design. First, a physiotherapist generated random codes (block size of 4) and put them inside sealed and opaque envelopes. Another physiotherapist who was blind to the codes randomly selected the sealed envelopes and delivered them to the patients. As a result, patients with a ratio of 1:1 were assigned to the experimental (n = 20) and control (n = 20) groups. To ensure blinding, patients were instructed not to provide any information to the assessors.
Statistical analysis
All data were sent for analysis to another researcher who was blinded to the study design. To prevent bias, all information was coded so that the researcher was not aware of the details of the study. First, the normal distribution of the data and the homogeneity of the variances were checked with the Shapiro–Wilk and t-test, respectively. Analysis of covariance (ANCOVA) was used to compare results between groups. Using parietal eta squared (η2) data, the effect size was interpreted as small (d < 0.20), medium (d = 0.21–0.79), and large (d > 0.80) 45. Moreover, within-group effect sizes were calculated by determining the difference between pretest and posttest means, divided by the pretest SD, and interpreted according to a scale previously proposed by Rhea 46. All statistical analyses were performed with SPSS version 26 software and the significance level was set at p < 0.05.
Results
Patients characteristics
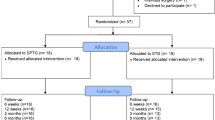
Overall, 40 eligible patients were recruited for clinical trials and assigned to two experimental (n = 20) and control groups (n = 20). The experimental group received the rehabilitation protocol (forefoot strike pattern with foot-knee exercises) for 8 weeks, while the control group did not receive any intervention (Fig. 2). Generally, Patients’ adherence to the research framework was 100%. More detailed, all patients in the experimental group completed 24 sessions of foot-knee strengthening exercises and 24 sessions of gait retraining (100%). As a result, all patients completed 48 intervention sessions by the research design, indicating high patient adherence to the research design. In contrast, all the patients assigned to the control group completely adhered to the study control group framework (100%). Hence, patients showed very high compliance in adherence to the research framework. In the experimental group, at the end of each session, the researchers provided information about the rehabilitation protocol to the patients. This information became progressively more specialized with each session and encouraged them to attend treatment sessions regularly and to avoid using other treatments that could contaminate the results.
In the control group, we contacted patients weekly and asked them to report the average pain experienced over the last week. We encouraged patients to refrain from any therapeutic intervention for 8 weeks. After 8 weeks, the control group patients also received the same therapeutic intervention under the supervision of a physiotherapist as the experimental group. Of note, we presented gifts (T-shirts, towels, sports bags) to the subjects during three phases (weeks 2, 4, and 6), encouraging them to continue adherence to the research framework and cooperating with the research team. All demographic characteristics displayed normal distribution according to the Shapiro–Wilk test (Table 1).
Primary outcome
Table 2. showed that there was a significant difference in the self-reported pain (p < 0.001; η2 = 0.884). The experimental group compared to the control group (within-group effect sizes (control: + 2.07 vs. experimental:—2.98) showed a decrease in self-reported pain (Table 2, Fig. 3, Fig. 4).
Secondary outcome
Table 2. showed that there was a significant difference in the rear-foot eversion angle (p < 0.001; η2 = 0.880), DKV (p < 0.001; η2 = 0.740), and pelvic drop (p < 0.001; η2 = 0.540), the hip abductor strength (p < 0.001; η2 = 0.770), the hip extensor strength (p < 0.001; η2 = 0.743), and knee extensor strength (p < 0.001; η2 = 0.811). The experimental group compared to the control group showed a decrease in the rear-foot eversion angle (within-group effect sizes control: + 0.95 vs. experimental:—4.32), DKV (within-group effect sizes control: + 1.77 vs. experimental: -3.44), and pelvic drop (within-group effect sizes control: + 0.88 vs. experimental: -0.25) (Table 2, Fig. 3, Fig. 4). In addition, the experimental group compared to the control group showed an improvement in the strength muscles of the hip extensor (within-group effect sizes control: -1.01 vs. experimental: + 1.71), hip abductor (within-group effect sizes control: -1.20 vs. experimental: + 1.79), and knee extensor (within-group effect sizes control: -0.90 vs. experimental: + 1.64) (Table 2, Fig. 3, Fig. 4).
Minimal clinically important difference
The MCID for self-reported pain of 3.1, rear-foot eversion of 5.1, DKV of 3.3, and pelvic drop of 1.67 was obtained. Therefore, in the experimental group clinical importance was received for the rear-foot eversion, self-reported pain, and DKV. Of note, despite the significant difference in the reduction of pelvic drop, the clinical importance of pelvic drop was not observed.
Discussion
This randomized clinical trial investigated the effects of altering walking foot strike pattern in combination with lower extremity strengthening on lower limb alignment in females with PFP. We hypothesized that after 8 weeks of a rehabilitation program, self-reported pain, rear-foot eversion, DKV, and pelvic drop would decrease and muscle strength of hip extensor, hip abductor, and knee extensor would increase. After 8 weeks the lower limb strengthening and changes in foot strike during walking led to reduced self-reported pain and changes in lower limb kinematics including angle reduction of rear-foot eversion, DKV, and pelvic drop were decreased during a single leg squat. In addition, the strength muscles of the hip extensor, hip abductor, and knee extensor were increased. Therefore, the hypothesis proposed in this clinical trial was supported. The findings of our study are in agreement with previous similar clinical trials 2,12,17,18,31. Therefore, we conclude that adding a forefoot strike pattern to foot-knee strengthening exercises can have clinical importance for improving lower limb dynamic alignment in women with PFP. Of note, women with PFP show a different movement pattern compared to men. The different movement pattern in the women population includes increased Q-angle, increased dynamic knee valgus, increased hip internal rotation, hip adduction moment, and knee abduction moment, decreased knee flexion angle as well as greater ankle flexion/extension 47,48. Therefore, gender is a confounding factor 49. Meanwhile, we only recruited women with PFP.
The foot pronation and the subsequent internal rotation of the tibia and hip lead to the DKV and the dynamic Q angle, which increases the distance of the lever arm between the center of the hip joint and the knee 3,10,50. As a result, the capacity of hip abductor muscles to produce moment decreases 3. The GMED has the largest physiological cross-sectional area of the hip abductor muscles and provides a stabilizer for the hip and pelvic 51. Overall, during the standing phase, the force of gravity moves the pelvis to the adduction position. The GMED and the upper part of the GMAX on the same side contract eccentrically and prevent the pelvic drop against the varus moment caused by the force of gravity 52. Meanwhile, despite the significant difference in the reduction of pelvic drop, no clinical importance was observed, which may be due to not focusing the exercise program on isolated strengthening of the GMED and GMAX muscles, which play an important role in controlling pelvic stability.
Several studies have shown that persons with PFP have delayed onset of GMED activation compared with healthy persons 53,54,55. Importantly, Aminaka et al. (2011) reported patients with PFP showed both delayed GMED onset and increased knee abduction moment compared with healthy subjects 54. Of note, knee abduction moment correlates with patellofemoral joint stress rate and is a risk factor for PFP 56. A meta-analysis showed that patients with PFP had a higher knee abduction moment than healthy subjects (SMD = 0.75; 95% CI = [0.47 to 1.02]) 3. Meanwhile, Kim et al. (2016) showed that improved GMED feedforward activation decreased knee abduction moment 51. Given the above knowledge, the reduction of rear-foot eversion after rehabilitation helps to explain how exercises focused on the foot can improve lower limb alignment.
Mølgaard et al. (2018) argued that distal interventions can have kinematic effects on the lower limb of patients with PFP 2. In other words, it seems that reducing foot pronation through lower extremity coupling has reduced DKV and patellofemoral joint stress and improved knee pain 2. On the other hand, reported that loading rate has correlated with pain intensity and PFP 49. The knee and patellofemoral joint loading depends on force dissipation and plantar loading 5. Since muscle activation plays an important role in load absorption, strengthening the intrinsic foot muscles can improve the stability, and ability to absorb shock 57. As a result, the vertical ground loading rate in the patellofemoral joint decreases, and pain improves. Yalfani et al. (2024) reported that PFP can cause the neuromuscular biomechanics of lower limb deficits and, the stabilizing muscles activation decreases and increases the lower limb movement in the frontal plane 15. These researchers recommended clinical trials are needed to investigate the effect of strategies focused on reducing patellofemoral joint stress during painful tasks on clinical symptoms of patients with PFP 15. In this line, we used a forefoot strike pattern to reduce patellofemoral joint stress.
The forefoot strike pattern can increase ankle plantar flexion and decrease the knee extensor demand and knee flexion. This change in joint angle redistributes mechanical load away from the patellofemoral joint and toward the ankle and calf muscle finally resulting in efficient energy transfer which can effectively reduce patellofemoral joint stress 18,58. Besides the above point, the forefoot strike pattern would produce a greater plantar–flexion moment and the center of pressure moved to the front of the foot, which would contribute to the horizontal distance between the ground reaction force line and increase the center of the ankle joint 18. Therefore, the increased plantarflexion moment and horizontal distance may increase ankle energy absorption and reduce knee energy absorption, thereby reducing the patellofemoral joint stress 18,58. As a result, it seems that using a forefoot strike pattern and subsequently reducing patellofemoral joint stress leads to control of the excessive medial movement of the lower extremity and subsequently, the activity of the stabilizing muscles of the lower extremities improves. In this line, Santos et al. (2019) showed that a forefoot strike led to patellofemoral joint stress decreased by 27% and pain reduction by 75% at a 6-month follow-up 16,31. In addition, Wei et al. (2024) showed that a reduction in knee abduction angle and moment after a forefoot strike pattern may help reduce the patellofemoral joint stress 18.
Overall, subjects with foot pronation show decreased muscle activity in the abductor hallucis, medial gastrocnemius, and VMO 59. The foot exercises of the present study focused on strengthening the intrinsic foot muscles. The abductor hallucis, flexor digitorum brevis, and quadratus plantae are intrinsic foot muscles that have been identified to contribute to postural control of the foot during weight bearing 60. Among the intrinsic muscles, specifically the abductor hallucis has been identified to contribute to stabilization and eccentric control of medial longitudinal arch descent during loading 60. It has been demonstrated that completing a short foot exercise during standing in individuals with PFP who have a pronated foot was the most effective method for increasing abductor hallucis muscle activity 10. In this regard, Lee et al. (2017) in an electromyography study showed that short foot exercises increased the activity of the abductor hallucis in patients with PFP 10. Overall, the intrinsic foot muscle exercise can elevate the medial longitudinal arch through a closed kinetic chain mechanism, potentially correcting foot pronation and altering foot biomechanics 61. More specialized, the subtalar joint is the functional unit connecting the foot and shank and its position influences the function of the foot and lower limb biomechanical alignment 62. The orientation of the subtalar joint axis links rear-foot eversion with lower limb internal rotation 63. These findings are in agreement with previous studies correlating foot position with tibial rotation, the interaction with the knee joint, and patellofemoral alignment and their reliance on rear-foot eversion angle 64,65. Moreover, these changes in foot mechanics may have a kinematic impact on the entire lower extremity through joint coupling, potentially reducing internal tibial rotation and hip adduction 63. This, in turn, may lead to a decrease in internal femoral rotation, thereby reducing lateral compressive forces on the patella and improving knee pain 61. Therefore, it is logical to hypothesize that reduced foot pronation may influence the biomechanics of the lower limb 63. Furthermore, they reported that VMO and vastus lateralis (VL) activation was relatively increased and decreased, respectively 10. Also, Hertel et al. (2005) showed that controlling foot pronation increased VMO and GMED activity in patients with PFP during single-leg squats 66. Of note, VMO/VL muscle imbalance are effective factor in increasing the patellofemoral joint stress and PFP pathogenesis 10.
Adding the medial intrinsic foot muscles exercises to a proximal lower limb (e.g., squats) can increase activation of GMAX, GMED, and quadriceps muscles which play an important role in controlling lower limb alignment during single-limb stance tasks 67. Consistent with our findings, Kısasık et al. (2021) reported that hip extensor strength improved after 8 weeks of combined foot and knee in patients with PFP 12. It seems that the improvement in muscle activity is due to the facilitation of the neuromuscular control of the lower limb 12. Foot pronation cause imposes higher pressure on the muscle spindles and tendons of the talocalcaneal joint, which leads to a defect in the proprioception feedback of the foot 59. In this regard, it has been reported that intrinsic foot muscle strengthening can improve muscle activation by facilitating plantar proprioceptive and increasing afferent impulses to the spinal cord 12.
Study limitations
The limitations of the present clinical trial should be acknowledged. First, only women volunteers participated in this trial. Therefore, since women with PFP show a different movement pattern than men, our findings cannot be generalized to male patients. Second, only PFP patients with rear-foot eversion participated in the clinical trial. Therefore, our results cannot be generalized to PFP patients with natural foot posture. Third, the follow-up period was limited to 8 weeks, preventing us from determining whether the effects of the intervention would be sustained in the long term. The outcome measures were limited to foot, knee, and pelvic alignment. Therefore, other kinematic (spatiotemporal characteristics) and kinetic variables (electromyography) should be investigated.
Conclusion
Eight weeks the lower limb strengthening and changes in foot strike during walking can have clinical importance in reducing self-reported pain, rear-foot eversion, DKV, and pelvic drop during a single leg squat.
Data availability
The datasets used and analyzed during the current study available from the corresponding author on reasonable request.
References
Yalfani, A. A. M. Patients with patellofemoral pain exhibiting decrease vertical ground reaction force compared to healthy individuals during weight bearing tasks: A systematic reviews and meta-analysis. Iran J Public Health. 52(2), 254–264 (2023).
Mølgaard, C. M. et al. Foot exercises and foot orthoses are more effective than knee focused exercises in individuals with patellofemoral pain. J. Sci. Med. Sport 21(1), 10–15 (2018).
Yalfani, A., Ahmadi, M. & Asgarpoor, A. The effect of kinetic factors of dynamic knee valgus on patellofemoral pain: A systematic review and meta-analysis. J. Bodyw. Mov. Ther. 1(37), 246–253 (2024).
Luz, B. C. et al. Relationship between rearfoot, tibia and femur kinematics in runners with and without patellofemoral pain. Gait Posture 1(61), 416–422 (2018).
Rathleff, M. S. et al. Increased medial foot loading during drop jump in subjects with patellofemoral pain. Knee Surgery, Sport Traumatol Arthrosc. 22(10), 2301–2307 (2014).
Dierks, T. A., Manal, K. T., Hamill, J. & Davis, I. S. Proximal and distal influences on hip and knee kinematics in runners with patellofemoral pain during a prolonged run. J Orthop Sports Phys Ther. 38(8), 448–456 (2008).
Neal, B. S. et al. Foot posture as a risk factor for lower limb overuse injury: A systematic review and meta-analysis. J Foot Ankle Res. 7(1), 1–13 (2014).
Aliberti, S., Costa, M. S., Passaro, A. C., Arnone, A. C. & Sacco, I. C. Medial contact and smaller plantar loads characterize individuals with patellofemoral pain syndrome during stair descent. Phys. Ther. Sport 11(1), 30–34 (2010).
Graci, V. & Salsich, G. B. Trunk and lower extremity segment kinematics and their relationship to pain following movement instruction during a single-leg squat in females with dynamic knee valgus and patellofemoral pain. J. Sci. Med. Sport 18(3), 343–347 (2015).
Lee, J., Yoon, J. & Cynn, H. Foot exercise and taping in patients with patellofemoral pain and pronated foot. J. Bodyw. Mov. Ther. 21(1), 216–222 (2017).
Kayll, S. A. et al. Do biomechanical foot-based interventions reduce patellofemoral joint loads in adults with and without patellofemoral pain or osteoarthritis? A systematic review and meta-analysis. Br J Sports Med. 57(13), 872–881 (2023).
Klsaclk, P. et al. Short foot exercises have additional effects on knee pain, foot biomechanics, and lower extremity muscle strength in patients with patellofemoral pain. J Back Musculoskelet Rehabil. 34(6), 1093–1104 (2021).
Sheikhi, B., Rabiei, P., Letafatkar, A. & Rossettini, G. Is adding education to trunk and hip exercises beneficial for patellofemoral pain? A randomized controlled trial. Arch. Phys. Med. Rehabil. 105(2), 217–226 (2024).
Sahrmann, S., Azevedo, D. C. & Van, D. L. Diagnosis and treatment of movement system impairment syndromes. Brazilian J Phys Ther. 21(6), 391–399 (2017).
Yalfani, A., Ahadi, F., Ahmadi, M. & Asgarpoor, A. Relationship between exacerbating patellofemoral pain and dynamic knee valgus in females with patellofemoral pain after a patellofemoral joint loading protocol: A cross-sectional. Phys. Ther. Sport 1(67), 13–18 (2024).
Davis, I. S., Tenforde, A. S., Neal, B. S., Roper, J. L. & Willy, R. W. Gait retraining as an intervention for patellofemoral pain. Curr Rev Musculoskelet Med. 13(1), 103–114 (2020).
Roper, J. L. et al. The effects of gait retraining in runners with patellofemoral pain: A randomized trial. Clin Biomech. 35, 14–22 (2016).
Wei, Z., Hou, X., Qi, Y. & Wang, L. Influence of foot strike patterns and cadences on patellofemoral joint stress in male runners with patellofemoral pain. Phys. Ther. Sport 1(65), 1–6 (2024).
Nakhaee, Z., Rahimi, A., Abaee, M., Rezasoltani, A. & Kalantari, K. K. The relationship between the height of the medial longitudinal arch (MLA) and the ankle and knee injuries in professional runners. Foot 18(2), 84–90 (2008).
Gur, G. et al. Effects of corrective taping on balance and gait in patients with hallux valgus. Foot Ankle Int. 38(5), 532–540 (2017).
Soheilipour, F. et al. The prevalence of genu varum and genu valgum in overweight and obese patients: Assessing the relationship between body mass index and knee angular deformities. Acta Bio Medica: Atenei Parmensis. 91(4), e2020121 (2020).
Seo, S. S. et al. Outcomes of total knee arthroplasty in degenerative osteoarthritic knee with genu recurvatum. Knee 25(1), 167–176 (2018).
Lee, H. J. et al. Risk factors of hyperextension and its relationship with the clinical outcomes following mobile-bearing total knee arthroplasty. Arch. Orthop. Trauma Surg. 1(139), 1293–1305 (2019).
Vaughn, D. W. & Brown, E. W. The influence of an in-home based therapeutic exercise program on thoracic kyphosis angles. J. Back Musculoskelet. Rehabil. 20(4), 155–165 (2007).
Bozorgmehr, A. et al. Effect of posterior pelvic tilt taping on abdominal muscle thickness and lumbar lordosis in individuals with chronic low back pain and hyperlordosis: A single-group. Repeated-Measures Trial. J Chiropr Med. 19(4), 213–221 (2020).
McAviney, J., Schulz, D., Bock, R., Harrison, D. E. & Holland, B. Determining the relationship between cervical lordosis and neck complaints. J. Manipulative Physiol. Ther. 28(3), 187–193 (2005).
Penha, P. J. et al. Posture alignment of adolescent idiopathic scoliosis: photogrammetry in scoliosis school screening. J. Manipulative Physiol. Ther. 40(6), 441–451 (2017).
Khamis, S. & Carmeli, E. A new concept for measuring leg length discrepancy. J Orthop. 14(2), 276–280 (2017).
Khamis, S. & Carmeli, E. Relationship and significance of gait deviations associated with limb length discrepancy: A systematic review. Gait Posture 1(57), 115–123 (2017).
Hott, A. et al. Effectiveness of isolated hip exercise, knee exercise, or free physical activity for patellofemoral pain: A randomized controlled trial. Am J Sports Med. 47(6), 1312–1322 (2019).
Dos Santos, A. F. et al. Effects of three gait retraining techniques in runners with patellofemoral pain. Phys. Ther. Sport 1(36), 92–100 (2019).
Chaharmahali, L., Gandomi, F., Yalfani, A. & Fazaeli, A. The effect of self-reported knee instability on plantar pressure and postural sways in women with knee osteoarthritis. J Orthop Surg Res. 16(1), 1–10 (2021).
Belyea BC, Lewis E, Gabor Z, Jackson J, King DL. Validity and intrarater reliability of a 2-dimensional motion analysis using a handheld tablet compared with traditional 3-dimensional motion analysis. Journal of sport rehabilitation. 2015 Nov 1;24(4).
Herrington, L. Knee valgus angle during single leg squat and landing in patellofemoral pain patients and controls. Knee. 21(2), 514–517 (2014).
Gwynne, C. R. & Curran, S. A. Two-dimensional frontal plane projection angle can identify subgroups of patellofemoral pain patients who demonstrate dynamic knee valgus. Clin. Biomech. 1(58), 44–48 (2018).
Salem, G. J. & Powers, C. M. Patellofemoral joint kinetics during squatting in collegiate women athletes. Clin Biomech. 16(5), 424–430 (2001).
Ahmadi, M., Yalfani, A., Gandomi, F. & Rashid, K. The effect of twelve-week neurofeedback training on pain, proprioception, strength and postural balance in men with patellofemoral pain syndrome: A double-blind randomized control trial. Journal of Rehabilitation Sciences & Research. 7(2), 66–74 (2020).
Dawood, R. S., Abdelraouf, O. R., Mehmed, S., Moubarak, E. E. & Elborady, A. A. Assessment of core endurance and shoulder proprioception in dental students with and without forward head posture. Bulletin of Faculty of Physical Therapy. 28(1), 19 (2023).
Kagaya, Y., Fujii, Y. & Nishizono, H. Association between hip abductor function, rear-foot dynamic alignment, and dynamic knee valgus during single-leg squats and drop landings. J. Sport Health Sci. 4(2), 182–187 (2015).
Pain, W. P. & Scholtes, S. A. A dynamic valgus index that combines hip and knee angles: assessment of utility in females with patellofemoral pain. Int J Sports Phys Ther. 12(3), 333–340 (2017).
Sinclair, J. et al. Effects of a 4-week intervention using semi-custom insoles on perceived pain and patellofemoral loading in targeted subgroups of recreational runners with patellofemoral pain. Phys. Ther. Sport 1(34), 21–27 (2018).
Wilken, J. M., Rodriguez, K. M., Brawner, M. & Darter, B. J. Reliability and minimal detectible change values for gait kinematics and kinetics in healthy adults. Gait Posture. 35(2), 301–307 (2012).
Bangerter, C. et al. What are the biomechanical consequences of a structural leg length discrepancy on the adolescent spine during walking?. Gait Posture 1(68), 506–513 (2019).
Goto, S., Aminaka, N. & Gribble, P. A. Lower-extremity muscle activity, kinematics, and dynamic postural control in individuals with patellofemoral pain. J Sport Rehabil. 27(6), 505–512 (2018).
Cohen J. Statistical Power Analysis for the Behavioral Sciences. 1988.
Rhea, M. R. Determining the magnitude of treatment effects in strength training research through the use of the effect size. The Journal of Strength & Conditioning Research. 18(4), 918–920 (2004).
Yalfani, A., Ahadi, F. & Ahmadi, M. Effects of pain exacerbation on postural control in women with patellofemoral pain during single leg squat: A cross-sectional study. J. Orthop. Surg. Res. 19(1), 462 (2024).
Jafarnezhadgero, A., Alavi-Mehr, S. M. & Granacher, U. Effects of anti-pronation shoes on lower limb kinematics and kinetics in female runners with pronated feet: The role of physical fatigue. PLoS ONE 14(5), e0216818 (2019).
Briani, R. V., Pazzinatto, M. F., Waiteman, M. C., de Oliveira, S. D. & de Azevedo, F. M. Association between increase in vertical ground reaction force loading rate and pain level in women with patellofemoral pain after a patellofemoral joint loading protocol. Knee 25(3), 398–405 (2018).
Levinger, P. & Gilleard, W. Relationship Between Static Posture and Rearfoot Motion During Walking in Patellofemoral Pain Syndrome. J Am Podiatr Med Assoc. 96(4), 323–329 (2006).
Kim, D., Unger, J., Lanovaz, J. L. & Oates, A. R. The Relationship of Anticipatory Gluteus Medius Activity to Pelvic and Knee Stability in the Transition to Single-Leg Stance. PM R. 8(2), 138–144 (2016).
Neumann, D. A. Kinesiology of the hip: A focus on muscular actions. J Orthop Sports Phys Ther. 40(2), 82–94 (2010).
Cowan, S. M., Crossley, K. M. & Bennell, K. L. Altered hip and trunk muscle function in individuals with patellofemoral pain. Br J Sports Med. 43(8), 584–588 (2009).
Aminaka, N., Pietrosimone, B. G., Armstrong, C. W., Meszaros, A. & Gribble, P. A. Patellofemoral pain syndrome alters neuromuscular control and kinetics during stair ambulation. J Electromyogr Kinesiol. 21(4), 645–651 (2011).
Willson, J. D., Kernozek, T. W., Arndt, R. L., Reznichek, D. A. & Scott, S. J. Gluteal muscle activation during running in females with and without patellofemoral pain syndrome. Clin Biomech. 26(7), 735–740 (2011).
Waiteman, M. C. et al. Relationship between knee abduction moment with patellofemoral joint reaction force, stress and self-reported pain during stair descent in women with patellofemoral pain. Clin. Biomech. 1(59), 110–116 (2018).
Pabón-Carrasco, M. et al. Randomized clinical trial: The effect of exercise of the intrinsic muscle on foot pronation. Int J Environ Res Public Health. 17(13), 1–11 (2020).
Zhang, X., Fu, B., Li, Y., Deng, L. & Fu, W. Effects of habitual foot strike patterns on patellofemoral joint and Achilles tendon loading in recreational runner. Gait Posture 1(117), 121–128 (2025).
Arachchige, S. N., Chander, H. & Knight, A. Flatfeet: Biomechanical implications, assessment and management. Foot 1(38), 81–85 (2019).
Baellow, A. et al. Intrinsic foot muscle size and quality in a single leg weight bearing position across foot posture types in individuals with patellofemoral pain compared to healthy. Phys. Ther. Sport 1(54), 58–64 (2022).
Kamel, A. M., Ghuiba, K., Abd Allah, D. S., Fayaz, N. A. & Abdelkader, N. A. Effect of adding short foot exercise to hip and knee focused exercises in treatment of patients with patellofemoral pain syndrome: A randomized controlled trial. J. Orthop. Surg. Res. 19(1), 1–9 (2024).
Khamis, S. & Yizhar, Z. Effect of feet hyperpronation on pelvic alignment in a standing position. Gait Posture. 25(1), 127–134 (2007).
Resende, R. A., Deluzio, K. J., Kirkwood, R. N., Hassan, E. A. & Fonseca, S. T. Increased unilateral foot pronation affects lower limbs and pelvic biomechanics during walking. Gait Posture. 41(2), 395–401 (2015).
Klingman, R. E., Liaos, S. M. & Hardin, K. M. The effect of subtalar joint posting on patellar glide position in subjects with excessive rearfoot pronation. J Orthop Sports Phys Ther. 25(3), 185–191 (1997).
Stergiou, N. & Bates, B. T. The relationship between subtalar and knee joint function as a possible mechanism for running injuries. Gait Posture. 6(3), 177–185 (1997).
Hertel, J., Sloss, B. R. & Earl, J. E. Effect of foot orthotics on quadriceps and gluteus medius electromyographic activity during selected exercises. Arch Phys Med Rehabil. 86(1), 26–30 (2005).
Utsahachant, N., Sakulsriprasert, P., Sinsurin, K., Jensen, M. P. & Sungkue, S. Effects of short foot exercise combined with lower extremity training on dynamic foot function in individuals with flexible flatfoot: A randomized controlled trial. Gait Posture 1(104), 109–115 (2023).
Acknowledgements
We gratefully thank patients for volunteered participation in this study.
Funding
The current study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FA initiated the study. MA and FA collected and analyzed the data. FA and MA wrote the manuscript under the supervision of AY. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The present clinical trial was approved by the ethics committee of Bu-Ali Sina University (R.BASU.REC.1402.012). The trial was registered in the Clinical Trials Registry Iran (IRCT20230425057991N1) on 08/06/2023. All methods were performed in accordance with the relevant guidelines and regulations. Also, this study was adhered to the ethical principles of the 2013 Declaration of Helsinki.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yalfani, A., Ahadi, F. & Ahmadi, M. Effects of altering walking foot strike pattern in combination with lower extremity strengthening on lower limb alignment in females with patellofemoral pain: a randomized controlled trial. Sci Rep 15, 31687 (2025). https://doi.org/10.1038/s41598-025-17000-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17000-6