Abstract
Despite the fund of literature on patient satisfaction post penile implants across the Western world, to the best of our knowledge, there are no studies investigating this phenomenon at the Middle East and North Africa levels. Therefore, we aimed to examine patient satisfaction after penile prosthesis at a regional center in Jordan. This cross-sectional study was conducted on patients undergoing penile implant surgery between 2018 and 2023. Patient satisfaction was measured using the Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) survey. Included patients were either implanted with malleable (36.0%) or hydraulic penile prosthesis (64.0%). All surgical operations were performed by a single surgeon. Mean differences in EDITS score were analyzed using SPSS version 27.0. A total of 100 patients from 8 different countries were included in the final analysis. Included patients were characterized by a mean age of 57.9 ± 9.7 years, mean BMI of 27.2 ± 3.9 kg/m2, and a mean erectile dysfunction duration of 6.0 ± 4.2 years. Only 33.0% of patients were medically free. Participants who were medically free were 2.7 times (95% CI 1.103–6.466; p = 0.027) less likely to report early complications and 2.2 times (95% CI 1.018–6.107; p = 0.022) less likely to report late complications compared to those with comorbidities. Mean EDITS score for the entire sample was 75.14 ± 22.78. Patients who did not report early or late complications had significantly higher EDITS scores (p = 0.001 and p < 0.001, respectively). EDITS score did not significantly differ across age, BMI, country of residence, or type of penile implant. Our study contributes to the expanding body of evidence that supports the effectiveness of penile implant surgery in managing refractory ED, with high satisfaction rates and clinical efficacy.
Similar content being viewed by others
Introduction
Erectile dysfunction (ED) is defined as the consistent or recurrent inability to attain and maintain an erection sufficient for satisfactory sexual performance1,2. It is the most common form of male sexual dysfunction, predominantly affecting males beyond 40 years of age, and it significantly impacts their quality of life2. By 2025, it is estimated that ED will affect about 322 million men on a global scale3. The prevalence of ED is positively associated with age and increases significantly in the presence of other co-morbidities4. Its most commonly significant risk factors include cardiovascular disease, diabetes, hyperlipidemia, hypertension, or any pathology that affects circulatory elements, hormones, or vessel histology5.
Due to the multi-factorial nature of the disease, the treatment of ED is complex to navigate as it involves both physiological and psychological factors6. Current treatment modalities start with mere lifestyle modifications, which are considered the safest and most beneficial, and range from less-intrusive, non-surgical options to purely surgical options7. Medical, less-intrusive modalities are considered first line to ED refractory to lifestyle modifications and include PDE-5 inhibitors, testosterone supplementation, vacuum devices, intraurethral PGE-1, and intracavernosal injections2. When the aforementioned are contraindicated or fail to be satisfactory or ineffective, penile prosthesis is a valid third-line therapeutic modality with very high satisfaction rate per the guidelines of the European Association of Urology1,8. However, with proper preoperative counselling, penile prosthesis may be considered as first-line therapy9.
It should be noted that sexual health and erectile quality are not only important for the patient’s quality of life, but also their partner’s mental, emotional, and physical well-being10. The American Urological Association (AUA) recommends the use of psychiatric care as adjunctive therapy as a means to improve adherence to and effectiveness of provided treatment options11,12. The literature shows high satisfaction in response to penile implants. Jorissen et al.’s, cohort of Belgian patients who underwent the implementation of a 3-piece inflatable penile prosthesis, demonstrated high satisfaction rates alongside their partners1. Akin-Olugbade et al., demonstrated that penile prosthesis resulted in significantly better post-operative satisfaction rates among the general population and even those with anatomical (i.e., Peyronie’s disease) and medical risk factors (i.e., BMI > 30)13. Finally, in their Greek cohort, Vakalopoulos et al., showed that inflatable penile prostheses are significantly associated with higher posttreatment satisfaction for both patients and their respective partners14. The study also found that the correlation between patient and partner satisfaction exhibits a linear pattern.
Despite the fund of literature on patient satisfaction post penile implants across the Western world, to the best of our knowledge, there are no studies investigating this phenomenon in the Middle East and North Africa. Therefore, we aimed to examine patient satisfaction after penile prosthesis at a regional center in Jordan, which hosts patients from a wide range of Middle Eastern nations, including Saudi Arabia, Iraq, Oman, Qatar, and the United Arab Emirates, among others. This study provides a glimpse into the general attitudes of patients regarding penile implants in a conservative community, in which, sexual health and its associated matters are considered extremely private matters, and at times, taboo.
Methods
Study design and population
This cross-sectional study included patients who underwent penile implant surgery at Abdali Hospital between 2018 and 2023. Patients who underwent more than one penile prosthesis implantation, had conducted any penile surgery outside of our center, or had refused to participate in the study were excluded. Moreover, participants who failed to complete the study’s questionnaire or had missing answers totaling more than 10% of variables were also removed from the final analysis.
Study tool
We implemented a data collection tool that was developed after an extensive literature review. The self-administered tool is composed of 29 items distributed across three domains. The first domain included patients’ sociodemographic and clinical characteristics, which included age, marital status, number of children, plans to have other children, educational level, country of residence, follow-up period, anthropometric measures, past medical history, duration of erectile dysfunction, number of preoperative consultations, previous non-surgical treatments used, number of implant surgeries, implant type, and smoking status.
The second domain recorded patients’ self-reported early and late treatment complications and outcomes. Early and late complications were defined as any event that occurred during the initial 4 weeks or beyond 4 weeks after the surgery, respectively. These events included infections, pain, hematoma, mechanical failure, altered penile sensation, floppy glans syndrome, disfigurement, scrotal swelling, and implant instability. Outcomes were defined as unfavorable changes to penile width or length.
The third domain is directly adopted from the Erectile Dysfunction Inventory of Treatment Satisfaction (EDITS) survey. The EDITS is an 11-item validated tool to evaluate treatment satisfaction and probability of treatment continuation in patients with ED15. A number of items were modified to ensure cultural acceptability, taking into account the conservative nature of Middle Eastern societies. The EDITS tool was translated into Arabic and tested for validity per the recommendations of translation by the World Health Organization (i.e., forward translation, back translation, expert consensus of bi- and mono-linguals)16.
The reliability of the questionnaire was ensured through conducting a pilot study on 20 patients who were not included in the final analysis of the study. The Cronbach’s alpha value for the EDITS tool was 0.938. The English version of the data collection tool is presented as Supplementary material.
Data collection procedure
Participants conforming to our inclusion criteria were contacted via WhatsApp and asked to fill out our self-administered tool. The tool was implemented through Google Forms. Aside from age, the tool was strictly anonymous with no collection of any identifying information. The study was conducted in accordance with the guidelines set by the declaration of Helsinki and was granted ethical approval by the Abdali Research and Ethics Committee (NO# 032400003). Informed written consent was obtained from all the patients.
Surgical protocol
Prior to the operation, a comprehensive informed consent form was received from all patients, which included detailed information on the procedure and its risks. The type of prosthesis to be placed was determined based on the patients’ medical history and their socioeconomic status. Patients were either implanted with the Coloplast (Minneapolis, MN, USA) Titan inflatable penile prosthesis or the Coloplast (Minneapolis, MN, USA) Genesis malleable penile prosthesis.
The patients were provided with information on possible complications that may occur during and after the surgery. In the perioperative period, the penoscrotal area was cleansed mechanically using chlorhexidine alcohol. Penoscrotal vertical incision was used for all procedures. The administration of Clindamycin was continued for a duration of two weeks following the patient’s discharge from the hospital. The patients had instructions on how to use the prosthetic after a duration of one month and were then granted permission to start using the prosthesis after a period of six weeks. All conducted operations were performed by a single surgeon (A.Y).
Statistical analysis
All data were entered into Microsoft Excel software, where they were recorded, cleaned and polished. The data were described using variability analysis in the form of means ± standard deviation. The sociodemographic factors were calculated and provided as frequencies (percentages). Pearson’s chi-square test and Fisher’s exact test were used to assess the association between categorical variables. The data was checked for normal distribution. Mann–Whitney U test was used to assess the mean difference between the hydraulic and malleable penile regarding several continuous variables. Differences in mean EDITS score across self-perceived unfavorable outcomes were examined using the Kruskal Wallis test. Spearman’s rank correlation was used to test the correlation between BMI and total satisfaction score. SPSS version 27.0 (Chicago, USA) was used for the analysis. All variables with a p < 0.05 were considered statistically significant.
Results
Demographic characteristics
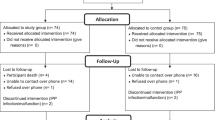
From 117 eligible patients, a total of 100 patients from 8 different countries who underwent hydraulic or malleable penile implant surgery were included in the study. Only 17 patients were excluded from the final analysis (n = 4 had more than one penile implant, n = 11 had penile implants outside of our center, and n = 2 did not complete the questionnaire). The mean age of the participants was 57.91 ± 9.68 years, ranging from 29 to 75 years. All of the participants were married, with an average marriage duration of 28.54 ± 12.33 years. Almost three quarters (72%) of the patients had a higher education. The mean number of children reported by the participants was 5.10 ± 2.76. Most of the participants were residing in Jordan (30.0%), followed by Saudi Arabia (24%) and Kuwait (23%). Table 1 demonstrates the participants’ sociodemographic characteristics.
Clinical characteristics
For included participants, the mean duration of erectile dysfunction before surgery of 6.02 ± 4.16 years (range 1–30). In addition, patients had a mean of 2.54 ± 2.52 (range 0–20) medical visits before deciding to have the operation with 86% of the patients had tried other conservative treatments before have the operations. Moreover, only 20.0% of the patients in the study were planning to have more children.
Among the included patients, 33.0% were medically free. On the other hand, the most common chronic conditions among their counterparts were diabetes (44.0%), hypertension (31.0%), and ischemic heart disease (5.0%). Only one patient had Peyronie’s disease. Additionally, 34% of the patients were smokers. The mean height measured 177.57 ± 6.10 centimeters, while weight mean 85.43 ± 10.17 kg, resulting in a mean BMI of 27.19 ± 3.90 kg/m².
Prosthesis type and self-reported complications
Regarding the type of penile implant received, the majority of patients were treated with hydraulic penile implants (64.0%), while 36.0% received malleable penile implants. Participants who were medically free were 2.7 times (95% CI 1.103–6.466; p = 0.027) less likely to report early complications and 2.2 times (95% CI 1.018–6.107; p = 0.022) less likely to report late complications compared to those with comorbidities.
Less than half of the included cohort (46.0%) reported early-term complications. These complications included pain (21.0%), scrotal swelling (13.0%), altered penile sensation (12.0%). On the other hand, only 28.0% of patients experienced long term complications, which included chronic pain (9.0%), penile disfigurement (8.0%), implant instability (8.0%), and altered penile sensation (6.0%). Table 2 summarizes all the early and late-term complications after the implant surgery.
Treatment satisfaction
Analysis of the EDITS scores revealed a mean score of 75.14 ± 22.78 for the entire cohort. When categorized, 89% of participants reported being satisfied, while 11% expressed dissatisfaction. Table 3 represent the detailed responses of erectile dysfunction inventory of treatment satisfaction.
When comparing the two types of implant surgery, there was no significant difference in the total EDITS score (p = 0.148). Similarly, EDITS score did not significantly differ per age (p = 0.420), country of residence (p = 0.228), BMI (p = 0.088), or presence of chronic disease (p = 0.497). On the other hand, patients who did not experience early or late complications had significantly higher EDITS scores (p = 0.001 and p < 0.001, respectively). Table 4 demonstrate the EDITS score for the included cohort stratified per their sociodemographic and clinical characteristics. In terms of self-perceived unfavorable outcomes, EDITS score was significantly different across both the early and late timepoints (p = 0.033 and p = 0.004, respectively) (refer to Fig. 1).
Discussion
The results of our study indicate high patient satisfaction rates with penile implant surgery. This finding is consistent with previous research on the topic1,17,18,19,20. However, we found no significant difference in satisfaction rates between malleable and hydraulic implants, contradicting several studies that suggest higher satisfaction rates with hydraulic implants13,19,21,22. This discovery indicates that the choice of prosthesis type may not be the sole factor determining treatment satisfaction. Instead, it highlights the importance of tailoring treatment approaches to individual patient preferences and clinical considerations. Therefore, it is crucial to consider individual differences in treatment expectations and experiences, as factors like socioeconomic status, preoperative counseling, postoperative support, and psychosocial aspects can influence satisfaction levels. It should also be noted that differences within the literature could also be attributed to differences in meta-characteristics such as sampling frame, target population, design differences, or even methodological biases.
While penile prosthetic surgery can be a valuable treatment option for patients with medication-refractory ED, it does carry some potential complications23. Our investigation revealed a decrease in size as the most common early complication following penile implant surgery. Studies on the impact of this surgery on penile length have shown conflicting results24. Some found no significant changes in penile length after the surgery25. Conversely, other studies observed a significant decrease in erect penile length; however, this did not affect treatment efficacy26. Montague et al., highlighted the importance of effectively managing patient expectations, particularly regarding penile size, as patient dissatisfaction often arises from unmet size expectations27. Some papers suggested that aggressive cylinder sizing and postoperative rehabilitation could potentially assist in maintaining or even increasing penile length28. Moreover, our study also highlighted pain as a frequently encountered complication associated with penile implant surgery. Pain management following this surgical procedure is essential to patient care29.
Despite the potential for complications, including postoperative pain, the satisfaction rates among patients and their partners following penile implant surgery are generally high. Patients often report experiencing psychological benefits, such as enhanced self-esteem, despite their concerns regarding pain and other mechanical issues30. However, it should be noted that the EDITS tool, while properly translated into Arabic, was not psychometrically validated across such a population. Therefore, its threshold for high satisfaction could change in light of comparative normative data. Moreover, the limited range of items within the EDITS tool may not have captured the essence of “satisfaction” among our Arab patients.
A range of studies have explored patient complaints following penile implant surgery. One study found that mechanical failure, penile length loss, postoperative pain, and altered sensation were the main reasons for patient dissatisfaction1. Others have found that the most frequent postoperative problems include infection, bleeding, and device malfunction31. Nevertheless, these issues can be mitigated by employing a consistent technique, adhering to standard protocols, and utilizing innovative antibiotic coatings. The effectiveness of conservative treatment methods, such as antibiotic therapy, in managing localized infections after penile implant surgery has been well documented32. Additionally, surgical penile lengthening procedures performed during penile prosthesis insertion have been proven to be safe and effective for patients with penile shortening and severe erectile dysfunction33. Additionally, the risk of complications can be reduced through proper patient selection, preoperative assessment, and the implementation of specific intraoperative and postoperative protocols34.
Direct comparisons between our results and those of the existing literature are quite challenging. Firstly, the majority of studies reporting outcomes or complications lack standardized reporting, exhibit heterogenous methodologies, and inconsistent inclusion criteria35. While the PHOENIX multicentric registry reported an overall early complication rate of 4.6%, Italian and German reports showcase a postoperative complication rate of 20% with extremely high infection and mechanical failure rates36,37,38. On the other hand, an assessment of 605 worldwide patients implanted with Rigicon demonstrated a revision rate of 0.9% due to complications39. Each of the aforementioned studies reported its own set of complications, and at times, only those affecting reoperation. Secondly, since all patients self-reported their complications, these claims were not clinically validated. Thirdly, wildly different sample sizes on top of heterogenous methodologies render raw numeric comparisons between centers meaningless.
In our study, many patients had no underlying medical conditions, resulting in a significantly lower likelihood of experiencing both early and late complications compared to those with comorbidities. The most prevalent comorbidities identified were diabetes mellitus, hypertension, and ischemic heart disease. This suggests a plausible association between individuals’ overall health status and surgical interventions’ outcomes. These results underscore the importance of conducting comprehensive preoperative diagnoses and administering appropriate treatment for comorbid disorders to enhance surgical outcomes and mitigate complications.
The primary focus of research on penile implant surgery has been on the technical aspects and patient selection40. Szabo et al., have stressed the importance of preoperative planning and patient preparation to minimize complications41. However, there is a lack of specific research on the impact of penile implant surgery on fertility and the ability to have children. Our study indicated that 20% of our participants were planning to have children. Further research is required to investigate this aspect and offer guidance to individuals considering both penile implant surgery and parenthood.
Our research revealed a predominantly overweight population. Obesity poses a significant risk for ED and can influence the results of penile implant surgery. Saavedra-Belaunde et al., further emphasize the link between obesity and ED, often resulting in penile implant surgery42. It is also important to mention that nearly one-third of our patients are smokers, putting them at an increased risk of postoperative complications43. Collectively, these studies indicate that lifestyle factors can complicate penile implant surgery and may necessitate additional considerations for successful outcomes.
The duration of ED among the participants in our study was found to be quite lengthy, which is consistent with the systematic review conducted by Bajic et al.44. Their review revealed that men who underwent inflatable penile prosthesis placement had an average duration of 56 months, while those who received malleable penile prostheses had an average duration of 72 months. Furthermore, diabetic patients who underwent inflatable penile prosthesis placement had an average ED duration of 75 months. These findings underscore the variability in the duration of ED prior to penile implant surgery, with diabetic patients and individuals opting for malleable penile prostheses experiencing the longest durations. Acknowledging this condition’s chronic nature and its significant impact on patients’ quality of life is essential.
Despite our study’s encouraging findings, some limitations must be acknowledged. Firstly, the study was conducted as a descriptive cross-sectional study, which cannot establish causality or temporal relationships. Secondly, there was a lack of data on partner satisfaction, which plays a vital role in overall satisfaction with the sexual and psychological aspects of the relationship. Thirdly, this study relied on patients’ self-reported data. Complications or adverse events were not verified through clinical or any other objective examination. This is particularly relevant for variables, such as penile length or width, where patient perceptions do not always align with objective postoperative findings. Finally, recruitment of patients through WhatsApp using a Google Forms-based questionnaire could’ve introduced selection bias with participation skewed towards technologically savvy patients. Our study also has a few strengths; our study included patients from a wide range of countries in the Middle East. This provides a glimpse into the general attitudes of patients regarding penile implants in a conservative community. The surgical procedures were performed by a single doctor for all patients, ensuring consistency in surgical techniques and reducing the possibility of confounding factors that may impact patient outcomes.
Further research is essential to address important questions and uncertainties. Longitudinal studies with larger sample sizes and extended follow-up periods are necessary to evaluate the long-term satisfaction rates and durability of penile implants across diverse patient populations. Comparative studies on the effectiveness and patient satisfaction associated with different types and models of penile implants could help optimize surgical outcomes and improve patient experience. Qualitative research on patients’ subjective experiences, psychosocial impact, and factors influencing satisfaction post-penile implant surgery could provide valuable insights for tailored care delivery. Additionally, we identified the need for further research on the effects of penile implant surgery on fertility and the ability to have children. By addressing the limitations and building on the strengths of previous research, future studies can further progress our comprehension of this therapeutic approach and enhance patient outcomes and quality of life. The latter is of significant importance as it influences both the patient and the partner. Adjunctive psychiatric care should be examined within the context of risk factors affecting sexual health and erection quality.
Conclusion
To summarize, our study contributes to the expanding body of evidence that supports the effectiveness of penile implant surgery in managing refractory ED, with high satisfaction rates and clinical efficacy. Patients without underlying medical conditions had significantly lower risks of complications compared to those with comorbidities like diabetes, hypertension, and heart disease. Early complications, such as decreased size, pain, and decreased width, were common, while late complications often involved chronic pain and further size and width reduction. Most patients explored alternative treatments before surgery, highlighting the importance of informed decision-making. The prevalence of smoking and overweight status among participants underscores the need for lifestyle changes to optimize outcomes. These findings collectively emphasize the need for personalized preoperative assessments and comprehensive perioperative care to ensure favorable outcomes and enhance patient satisfaction in the management of erectile dysfunction.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jorissen, C., De Bruyna, H., Baten, E. & Van Renterghem, K. Clinical outcome: patient and partner satisfaction after penile implant surgery. Curr. Urol. 13 (2), 94–100 (2019).
Leslie, S. W. & Sooriyamoorthy, T. Erectile Dysfunction. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2024. Available from: http://www.ncbi.nlm.nih.gov/books/NBK562253/
Ayta, I. A., McKinlay, J. B. & Krane, R. J. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 84 (1), 50–56 (1999).
Shamloul, R. & Ghanem, H. Erectile dysfunction. Lancet Lond. Engl. 381 (9861), 153–165 (2013).
Matsui, H., Sopko, N. A., Hannan, J. L. & Bivalacqua, T. J. Pathophysiology of erectile dysfunction. Curr. Drug Targets. 16 (5), 411–419 (2015).
Krzastek, S. C., Bopp, J., Smith, R. P. & Kovac, J. R. Recent advances in the understanding and management of erectile dysfunction. F1000Research. 8, F1000 Faculty Rev. (2019). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC6348436/
Maiorino, M. I., Bellastella, G. & Esposito, K. Lifestyle modifications and erectile dysfunction: what can be expected? Asian J. Androl. 17(1):5. (2014). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC4291878/
Hatzimouratidis, K. et al. Guidelines on male sexual dysfunction: erectile dysfunction and premature ejaculation. Eur. Urol. 57 (5), 804–814 (2010).
Trost, L. W., Baum, N. & Hellstrom, W. J. G. Managing the difficult penile prosthesis patient. J. Sex. Med. 10 (4), 893–906 (2013). quiz 907.
Wassersug, R. & Wibowo, E. Non-pharmacological and non-surgical strategies to promote sexual recovery for men with erectile dysfunction. Transl. Androl. Urol. 6(Suppl 5),S776 (2017). Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5715194/
Burnett, A. L. et al. Erectile dysfunction: AUA guideline. J. Urol. 200 (3), 633–641 (2018).
Kukula, K. C., Jackowich, R. A. & Wassersug, R. J. Eroticization as a factor influencing erectile dysfunction treatment effectiveness. Int. J. Impot. Res. 26 (1), 1–6 (2014).
Akin-Olugbade, O., Parker, M., Guhring, P. & Mulhall, J. Determinants of patient satisfaction following penile prosthesis surgery. J. Sex. Med. 3 (4), 743–748 (2006).
Vakalopoulos, I. et al. High patient satisfaction after inflatable penile prostheses implantation correlates with female partner satisfaction. J. Sex Med. 10(11), 2774–81 (2013). Available from: https://www.sciencedirect.com/science/article/pii/S1743609515301739
Althof, S. E. et al. EDITS: development of questionnaires for evaluating satisfaction with treatments for erectile dysfunction. Urology 53 (4), 793–799 (1999).
World Health Organization. WHOQOL-BREF: Translation Methodology. Available from: https://www.who.int/tools/whoqol/whoqol-bref/docs/default-source/publishing-policies/whoqol-100-guidelines/translation-methodology
Carson, C. C. Penile prosthesis implantation: surgical implants in the era of oral medication. Urol. Clin. North. Am. 32 (4), 503–509 (2005). vii.
Bozkurt, I. H. et al. Patient and partner outcome of inflatable and semi-rigid penile prosthesis in a single institution. Int. Braz J. Urol. Off J. Braz Soc. Urol. 41 (3), 535–541 (2015).
Habous, M. et al. Predictors of satisfaction in men after penile implant surgery. J. Sex. Med. 15 (8), 1180–1186 (2018).
Levine, L. A. et al. Penile prosthesis surgery: current recommendations from the international consultation on sexual medicine. J. Sex. Med. 13 (4), 489–518 (2016).
Vakalopoulos, I. et al. High patient satisfaction after inflatable penile prostheses implantation correlates with female partner satisfaction. J. Sex. Med. 10 (11), 2774–2781 (2013).
Bernal, R. M. & Henry, G. D. Contemporary patient satisfaction rates for three-piece inflatable penile prostheses. Adv. Urol. 2012, 707321 (2012).
Sadeghi-Nejad, H. & Fam, M. Penile prosthesis surgery in the management of erectile dysfunction. Arab. J. Urol. 11 (3), 245–253 (2013).
Habous, M. et al. Penile length is preserved after implant surgery. BJU Int. 123 (5), 885–890 (2019).
Deveci, S., Martin, D., Parker, M. & Mulhall, J. P. Penile length alterations following penile prosthesis surgery. Eur. Urol. 51 (4), 1128–1131 (2007).
Wang, R. et al. Prospective and long-term evaluation of erect penile length obtained with inflatable penile prosthesis to that induced by intracavernosal injection. Asian J. Androl. 11 (4), 411 (2009).
Montague, D. K. Penile prosthesis implantation: size matters. Eur. Urol. 51 (4), 887–888 (2007).
Henry, G. D., Carrion, R., Jennermann, C. & Wang, R. N. Prospective evaluation of postoperative penile rehabilitation: penile length/girth maintenance 1 year following Coloplast Titan inflatable penile prosthesis. J. Sex. Med. 12 (5), 1298–1304 (2015).
Ellis, J. L., Higgins, A. M. & Simhan, J. Pain management strategies in penile implantation. Asian J. Androl. 22 (1), 34–38 (2019).
Tiefer, L., Pedersen, B. & Melman, A. Psychosocial follow-up of penile prosthesis implant patients and partners. J. Sex. Marital Ther. 14 (3), 184–201 (1988).
O’Rourke, T. K., Erbella, A., Zhang, Y. & Wosnitzer, M. S. Prevention, identification, and management of post-operative penile implant complications of infection, hematoma, and device malfunction. Transl. Androl. Urol. 6 (Suppl 5), S832–S848 (2017).
Habous, M. et al. Conservative therapy is an effective option in patients with localized infection after penile implant surgery. J. Sex. Med. 13 (6), 972–976 (2016).
Tran, H., Goldfarb, R., Ackerman, A. & Valenzuela, R. J. Penile lengthening, girth, and size preservation at the time of penile prosthesis insertion. Sex. Med. Rev. 5 (3), 403–412 (2017).
Cayetano-Alcaraz, A. A. et al. Penile implant surgery-managing complications. Fac. Rev. 10, 73 (2021).
Trost, L., Wanzek, P. & Bailey, G. A practical overview of considerations for penile prosthesis placement. Nat. Rev. Urol. 13 (1), 33–46 (2016).
Van Renterghem, K. et al. Early complications after penile prosthesis surgery: findings from the PHOENIX multicenter registry. Int. J. Impot. Res. 1–7 (2025).
Pozza, D., Marcantonio, A., Mosca, A. & Pozza, C. Penile prosthesis and complications: Results from 577 implants. Arch. Ital Urol. E Androl. 92(4). (2020). Available from: https://www.pagepressjournals.org/aiua/article/view/aiua.2020.4.302
Natali, A., Olianas, R. & Fisch, M. Penile implantation in europe: successes and complications with 253 implants in Italy and Germany. J. Sex. Med. 5 (6), 1503–1512 (2008).
Wilson, S. K. et al. Safety outcomes of the first Rigi10™ malleable penile prostheses implanted worldwide. Int. J. Impot. Res. 36 (8), 833–837 (2024).
Selvaggi, G., Branemark, R., Elander, A., Liden, M. & Stalfors, J. Titanium-bone-anchored penile epithesis: preoperative planning and immediate postoperative results. J. Plast. Surg. Hand Surg. 49 (1), 40–44 (2015).
Szabo, D. & Jenkins, L. C. Preparation and operative setup of penile prosthesis surgery. J. Vis. Surg. 6(0). (2020). Available from: https://jovs.amegroups.org/article/view/31926
Saavedra-Belaunde, J., Clavell Hernandez, J. & Wang, R. Epidemiology regarding penile prosthetic surgery. Asian J. Androl. 22, 2–7 (2019).
Miller, J. A. & Bennett, N. E. Comparing risk factors for adverse outcomes in Virgin inflatable penile prosthesis implantations and revisions: a retrospective cohort study. Sex. Med. 8 (3), 388–395 (2020).
Bajic, P. et al. Etiology of erectile dysfunction and duration of symptoms in patients undergoing penile prosthesis: a systematic review. Sex. Med. Rev. 8 (2), 333–337 (2020).
Funding
This work did not receive funding from any private or public institutions.
Author information
Authors and Affiliations
Contributions
Conceptualization: Yaman Altal, Leen Al-Huneidy. Formal analysis: Abdulrahman Karam, Rand Al-huneidy. Writing—original draft: Yaman Altal, Leen Al-Huneidy, Abdulrahman Karam, Rand Al-Huneidy, Morad Bani-Hani, Jad Alsmadi, Hassan Alkhatatbeh. Writing—review and editing: Yaman Altal, Leen Al-Huneidy, Abdulrahman Karam, Rand Al-Huneidy, Morad Bani-Hani, Jad Alsmadi, Hassan Alkhatatbeh.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethical approval and consent to participate
This study was approved by the Abdali Research and Ethics Committee (NO# 032400003). All methods were carried out in accordance with guidelines and regulations of the aforementioned bodies. All participants read and signed an online informed consent form before continuing to complete the questionnaire. The informed consent form included the participants’ right to anonymity, confidentially of their data, right to leave the study, and reassurance that their participation is completely voluntary, is not associated with any kind of short-term benefit or rewards and does not affect the quality of their received care.
Consent for publication
Not applicable.
Use of artificial intelligence tools
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Altal, Y., Al-Huneidy, L., Karam, A. et al. Patients’ satisfaction rate after penile implant surgery: a cross-sectional investigation from the middle east. Sci Rep 15, 34410 (2025). https://doi.org/10.1038/s41598-025-17391-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17391-6