Abstract
Ischemic preconditioning (PreC), remote perconditioning (PerC), and postconditioning (PostC) are known to reduce myocardial infarct size, but their relative efficacy and potential additive effects remain unclear. This study compared the individual and combined effects of PreC, PerC, and PostC on infarct size and cardiac troponin I (cTnI) levels in a rat model of myocardial ischemia–reperfusion. Fifty-four male Sprague–Dawley rats underwent 40 min of coronary occlusion followed by 2 h of reperfusion. They were randomized into six groups: Control, PreC, PerC, PostC, PerC + PostC, or PreC + PerC + PostC. Infarct size was measured using Evans blue/TTC staining, and cTnI levels were assessed. All conditioning strategies significantly reduced infarct size and cTnI levels compared to control (p < 0.001). PreC and PreC + PerC + PostC were the most effective, while PostC was the least. No additive benefit was seen when combining PreC with other strategies (p = 0.9) or PerC with PostC (p = 0.9). These findings suggest that PreC provides the greatest cardioprotection, and combining conditioning strategies does not enhance outcomes, possibly due to overlapping protective mechanisms.
Similar content being viewed by others
Introduction
Ischemic conditioning is a promising cardioprotective strategy aimed at mitigating ischemia–reperfusion injury by inducing brief, non-lethal ischemic episodes that enhance tissue resistance to subsequent prolonged ischemia1,2,3. Based on the timing relative to the index ischemic event, ischemic conditioning is categorized into three main types: preconditioning (PreC) before ischemia, perconditioning (PerC) during ischemia, and postconditioning (PostC) at the onset of reperfusion1,3.
Among these, ischemic preconditioning—first described in a canine model in 1986—remains the most extensively studied and consistently effective strategy4,5. It significantly reduces infarct size across various animal models, including rodents, pigs, and primates5,6. However, its reliance on pre-ischemia application limits clinical feasibility in acute unpredictable settings.
To overcome this limitation, alternative strategies applicable during or after ischemia—such as remote perconditioning and ischemic postconditioning—have been explored7,8,9,10,11. While preclinical studies, particularly in large animals, support their cardioprotective potential, results in rodent models and clinical trials have been inconsistent, with variable effects on infarct size and myocardial salvage3,10,11,12,13,14,15,16,17,18,19,20.
Given the variability, combining PerC and PostC— the two strategies applicable in acute settings—has been proposed to enhance cardioprotection. However, findings remain inconsistent, highlighting the need for further investigation10,11.
In this study, we systematically evaluate the cardioprotective efficacy of PreC, PerC, and PostC—both individually and in combination—in a rat model of ischemia–reperfusion injury by assessing their impact on infarct size and plasma troponin I levels21.
Methods and materials
Rats
Fifty-four male Sprague–Dawley rats (6–8 weeks old, 250–350 g) were obtained from Janvier Labs (Le Genest-Saint-Isle, France). The rats were acclimatized for one week at the Laboratory for Experimental Biomedicine (Gothenburg, Sweden) prior to the experiment. They were housed in standard cages under controlled conditions (21 °C, 12-h light/dark cycle) with ad libitum access to standard laboratory chow and water. All procedures were conducted in compliance with institutional and national guidelines for animal research and were approved by the Gothenburg Animal Ethics Committee (Dnr 5.8.18–11,014/2023) and performed in accordance with ARRIVE guidelines.
Ischemia–reperfusion model
Surgeries was performed as previously described2. Anesthesia was induced with an intraperitoneal injection of ketamine (120 mg/kg) and xylazine (5 mg/kg). To maintain anesthesia, an intravenous infusion of ketamine (0.125 mg/mL) and xylazine (3 mg/mL) in Ringer’s solution was administered via a lateral tail vein cannula and continued until euthanasia following the 2-h reperfusion period. End-tidal CO₂ levels were continuously monitored using CapStar-100 (CWE Inc.) and maintained between 5–6%. Additionally, body temperature, heart rate, oxygen saturation, and respiratory parameters were continuously recorded throughout the procedure.
A left thoracotomy was performed through the fourth intercostal space to access the heart. The left anterior descending (LAD) artery was ligated 3–4 mm distal to its origin using a 6.0 silk suture (Ethicon Inc., NJ, USA). LAD occlusion was confirmed by (i) left ventricular blanching, (ii) ECG changes, and (iii) regional akinesia on echocardiography. Reperfusion was initiated by loosening the suture.
Remote ischemic perconditioning was induced by temporary ligation of the left femoral artery with a 6.0 silk suture. This consisted of four cycles of 5-min occlusion followed by 5-min reperfusion. Effective occlusion was visually confirmed by the absence of distal blood flow.
Study design
This study evaluated the cardioprotective effects of pre-, post- and per-conditioning on myocardial infarction in a rat model. All rats underwent 40 min-index ischemia followed by 2 h of reperfusion. In addition, rats were randomized to the three types of conditioning as well as to combinations of the conditioning types. Specifically, fifty-four rats were randomly assigned to the following six experimental groups (n = 9 per group): (A) Control group: No conditioning intervention; (B) PreC: Two cycles of 5-min LAD ischemia and 5-min reperfusion were applied before index ischemia; (C) PerC: Four cycles of left femoral artery occlusion (5 min) and reperfusion (5 min) during the index ischemia; (D) PostC: Six cycles of 10-s LAD ischemia and 10-s reperfusion were initiated immediately after the index ischemia; (E) PerC + PostC: Both PerC and PostC; (F) PreC + PerC + PostC: A combination of all three ischemic conditioning strategies. A schematic representation of the experimental protocol is provided in Fig. 1.
Experimental protocols for ischemia–reperfusion and ischemic conditioning interventions. All groups underwent 40 min of left anterior descending artery (LAD) occlusion followed by 120 min of reperfusion. (A) Control group: LAD occlusion and reperfusion without any ischemic conditioning. (B) Ischemic preconditioning (PreC): Two cycles of 5 min LAD occlusion/reperfusion before ischemia. (C) Remote ischemic perconditioning (PerC): Four cycles of 5 min femoral occlusion/reperfusion during ischemia. (D) Ischemic postconditioning (PostC): Six cycles of 10 s LAD occlusion/reperfusion at reperfusion onset. (E) PerC + PostC: Combination of PerC and PostC. (F) PreC + PerC + PostC: Combination of all three conditioning strategies. Infarct size was assessed using TTC staining, and myocardial injury was evaluated by troponin I measurement. Black bars represent LAD occlusion, gray bars femoral artery occlusion, and white bars reperfusion.
Infarct size assessment
Myocardial infarct size was determined using Evans blue and 2,3,5-triphenyltetrazolium chloride (TTC) double staining, as previously described2. At the end of the 2-h reperfusion period, the LAD was re-occluded, and 5% Evans blue dye was administered via the lateral tail vein to demarcate non-ischemic myocardium. Hearts were rapidly excised, rinsed in saline, and transversely sectioned into five 2-mm-thick slices from apex to base. Slices were incubated in 1% TTC solution at 37 °C for 10 min in the dark to distinguish viable (red) from infarcted (white) myocardium, then fixed in 10% neutral-buffered formalin and immersed in phosphate buffer (pH 7.4) for 10 min. Digital images of each slice were acquired using a flatbed scanner (Seiko Epson, Japan). Image analysis was performed using ImageJ (v1.34, NIH, USA) to quantify infarcted, viable, and non-ischemic regions. Infarct size was expressed as a percentage of the area at risk , excluding the Evans blue–stained non-ischemic zones. All measurements were performed by two independent, blinded investigators. In cases of discrepancy, consensus was reached through evaluation by a third blinded reviewer.
Troponin I analysis
Plasma samples were stored at -80 °C until analysis. Cardiac troponin I (cTnI) levels were determined using the Abbott Alinity assay, with a LoB of 1 ng/L, an LoQ of 5.1 ng/L, an analytical CV of 10%, and a 99th percentile reference value of 26 ng/L.
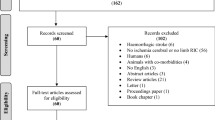
Exclusion criteria
Animals were excluded based on predefined criteria: (1) failure to position the LAD suture within two attempts; (2) excessive post-occlusion bleeding (≥ 3-soaked cotton swabs); (3) sustained heart rate < 250 bpm; (4) sustained end-tidal CO₂ > 7.5%; or (5) incomplete or technically inadequate TTC staining. Group allocation was randomized, and infarct size analysis was performed by an investigator blinded to treatment groups22.
Statistical analysis
Data were analyzed using R software (v4.2.0). All figures were generated using R, with additional formatting and design adjustments completed in Affinity Designer. Normality was tested using the Shapiro–Wilk test. Group comparisons were performed using one-way ANOVA, followed by Tukey’s post hoc test for pairwise comparisons. Results are expressed as mean ± SD, with significance set at p < 0.05.
Results
Baseline physiological characteristics
Physiological parameters—including age, body weight, temperature, heart rate, end-tidal CO₂, and oxygen saturation—did not differ significantly between experimental groups (Table 1). All rats survived the surgery and no procedural mortality was observed.
Infarct size
Infarct size, expressed as a percentage of the area at risk, differed significantly between experimental groups. The control group exhibited the largest infarct size (50.6% ± 4.9%), significantly larger than in all other groups (p < 0.001). The smallest infarcts were observed in the PreC group (28.6% ± 3.9%) and the PreC + PerC + PostC group (29.4% ± 2.5%). These two groups had statistically significantly smaller infarct size than all other groups with no significant difference between them (p = 0.9). Infarct size in the PerC group (35.6% ± 3.3%) was significantly smaller than in the PostC group (42% ± 2.7%, p < 0.01). While combined PerC and PostC (36.6% ± 2.3%) conferred greater protection than PostC (p < 0.01), it did not differ compared to PerC alone (p = 0.9). These findings are illustrated in Fig. 2.
Infarct size across experimental groups. (A) Infarct size, expressed as a percentage of the area at risk (AAR), was significantly higher in the control group compared to all other groups (p < 0.001). The smallest infarcts were observed in the PreC and PreC + PerC + PostC groups, with no significant difference between them (p = 0.9). PerC and PerC + PostC significantly reduced infarct size compared to PostC (p < 0.01), but the combination of PerC + PostC did not provide additional benefit over PerC alone (p = 0.9). Each dot represents one rat (n = 9 per group). Yellow circles indicate group means, and error bars represent standard deviation. Statistical comparisons were performed using one-way ANOVA followed by Tukey’s post hoc test. ** = p < 0.01, *** = p < 0.001. (B) Representative images of whole hearts stained with triphenyltetrazolium chloride (TTC). Dark blue regions indicate myocardium not subjected to ischemia. The bright red and white areas represent the area at risk (AAR), with bright red indicating viable myocardium and white indicating necrotic tissue.
Troponin I levels
Plasma cardiac troponin I (cTnI) levels were highest in the control group (49 723 ± 3 765 ng/L), significantly exceeding all other groups (p < 0.001). Similar to the histological infarction size, cTnI levels were significantly lower in the PreC (20 386 ± 4 796 ng/L) and PreC + PerC + PostC (18 625 ± 2 517 ng/L) groups than other groups, with no significant difference between them (p = 0.9). Among the other groups, PerC and PerC + PostC resulted in significantly lower cTnI levels than PostC (p < 0.001 for both), with no significant difference between PerC alone and PerC + PostC. These findings are shown in Fig. 3.
Troponin I levels across experimental groups. Troponin I (cTnI) levels were highest in the control group, and significantly higher than in all other groups (p < 0.001). The lowest levels were observed in the PreC and PreC + PerC + PostC groups, with no significant difference between them (p = 0.9). PerC and PerC + PostC reduced cTnI levels more than PostC (p < 0.001), but the combination of PerC + PostCdid not provide additional benefit over PerC alone (p = 0.18). Each dot represents one rat (n = 9 per group). Yellow circles indicate group means, and error bars represent standard deviation. Statistical analysis was performed using one-way ANOVA followed by Tukey’s post hoc test. *** = p < 0.001.
Discussion
The most important findings of our study is that in a controlled experimental setting (i) PreC, PerC, and PostC all significantly reduce histological infarct size and cTnI release after myocardial ischemia–reperfusion, with the most pronounced reduction in infarct size observed with PreC and the least pronounced effect observed with PostC; and (ii) there were no additive effect of PostC to PerC or PostC and PerC to PreC suggesting a potential ceiling effect when combining conditioning types.
Both PostC and PerC have reduced infarct size in preclinical models, though PostC has shown more variable efficacy10,11. This inconsistency may stem from protocol-dependent factors, such as the number, duration, and timing of ischemia–reperfusion cycles. Shorter cycles or delayed initiation have been shown to reduce protective effects3,10. Conversely, PerC has demonstrated consistent efficacy in large animal models but remains inconsistent in rodent studies, where species-specific metabolic and vascular differences, as well as protocol variations, may contribute to variability11,15.
In clinical settings, the efficacy of PostC and PerC remains inconclusive. While some studies report PostC-induced infarct size reduction in STEMI patients, as measured by Single-Photon Emission Computed Tomography and cardiac biomarkers (CK-MB, troponin I), others show no improvement in myocardial salvage or infarct size3,12,13,14. Similarly, PerC trials have demonstrated reductions in injury markers and improved myocardial salvage, but without significant impact on final infarct size, raising questions about the clinical significance of these improvements17,18,19.
In this study, both PostC and PerC conferred cardioprotection by reducing infarct size compared to the control group. However, PerC proved more effective than PostC, while neither approach matched the superior efficacy of ischemic preconditioning. Troponin I release closely paralleled infarct size reduction across groups. The inconsistencies in both experimental and clinical studies call into question the reliability of PostC and PerC as standalone interventions, prompting research into their combined application for enhanced cardioprotection.
A rat study identified an optimized PerC + PostC protocol—consisting of four cycles of 5-min unilateral limb occlusion (PerC) during ischemia, followed by six cycles of 10-s occlusion-reperfusion (PostC) at reperfusion onset—which yielded maximal infarct size reduction11. However, a subsequent study failed to replicate these findings, with the only methodological difference being the use of bilateral rather than unilateral limb occlusion10. Clinical trials have shown similarly inconsistent outcomes. The RIPOST-MI trial found that adding PostC to PerC in STEMI patients failed to enhance cardioprotection, as assessed by CK-MB release19. In contrast, the LIPSIA trial reported a significantly higher myocardial salvage index (MSI) in the PerC + PostC group compared to conventional PCI, though this did not translate into reduced infarct size or improved long-term outcomes13.
In our study, we applied the same unilateral optimized protocol as Xin et al.11 but observed no added benefit of combining PerC and PostC over PerC alone. Likewise, triple conditioning (PreC + PerC + PostC) did not further reduce infarct size or cTnI levels over PreC alone, suggesting no cumulative benefit from combining strategies. Although combining PerC and PostC is theoretically appealing, both animal and human studies have failed to demonstrate consistent additive effects.
Pushing the Protective Ceiling of Ischemic Conditioning.
One plausible explanation for this ceiling effect is the extensive convergence of cardioprotective signaling cascades23,24. IPC, IPost, and RIPerC differ in their temporal windows and initiating mechanisms.
-
IPC triggers protection before ischemia through early activation of PKC-ε, Akt, ERK1/2, and STAT3, followed by a delayed transcriptional phase involving JAK–STAT and p38 MAPK signaling25,26,27.
-
IPost acts exclusively at reperfusion, rapidly engaging Akt, ERK1/2, eNOS, and STAT3 via autacoid signaling, but without a delayed phase27,28,29.
-
RIPerC, initiated during ongoing ischemia, relies on remote neural and humoral inputs, with robust STAT3 phosphorylation often driven by circulating cytokines30,31.
Despite these upstream differences, all three strategies converge on the RISK (PI3K–Akt, ERK1/2) and SAFE (JAK–STAT3) pathways and downstream effectors including nitric oxide (NO), PKG activation, and inhibition of mitochondrial permeability transition pore (mPTP) opening. This convergence may impose a ceiling effect, beyond which additional stimuli yield no further benefit27,28, as illustrated in Fig. 4.
Mechanisms of cardioprotection in ischemic conditioning. Ischemic pre-, per-, and post-conditioning activate pro-survival signaling cascades—primarily the RISK (PI3K–Akt–eNOS, ERK1/2, PKC, GSK-3β) and SAFE (TNF-α–JAK2–STAT3) pathways—which converge on mitochondria to inhibit mPTP opening, stabilize membrane potential, reduce oxidative stress and calcium overload, and enhance anti-apoptotic signaling. Created by BioRender.
The variability observed in both preclinical and clinical studies reflects a broader limitation in the field: the lack of systematic optimization of conditioning algorithms. Most studies, including ours, rely on legacy protocols developed in early proof-of-concept experiments, which—while offering consistency and comparability—may not represent optimal configurations32,33. The absence of additive protection in our study may therefore result not only from pathway saturation but also from suboptimal algorithm selection (timing, duration, or cycle number). Rational, head-to-head algorithmic design studies are warranted to systematically map protocol parameters and identify configurations that maximize efficacy.
Further, incomplete engagement of other molecular regulators may contribute to the variability of cardioprotection. Redox signaling plays a dual role: while moderate ROS levels promote pro-survival pathways—PKC and ERK1/2 activation-, sustained oxidative stress can impair signaling fidelity and exacerbate injury34. Mitochondrial dysfunction, in turn, activates the NLRP3 inflammasome, driving pyroptotic cell death. Targeting mitochondrial ROS or NLRP3 pharmacologically has been proposed as a way to reinforce cardioprotection35,36. Moreover, mitophagy, via PINK1/Parkin or BNIP3-dependent pathways, maintains mitochondrial integrity and restrains inflammation; impaired mitophagy, particularly in the context of metabolic syndrome, may blunt the efficacy of conditioning. Interventions that fine-tune mitophagic flux may further enhance the efficacy of ischemic conditioning37.
Together, these insights support a multidimensional optimization framework: future studies should (1) explore the combinatorial space of conditioning parameters and (2) integrate targeted modulation of redox homeostasis, mitochondrial quality control, and inflammasome signaling. This integrative strategy may help advance ischemic conditioning toward more robust, reproducible, and clinically translatable cardioprotection.
Conclusion
Our study demonstrated that PreC, PerC, and PostC each independently reduced infarct size and troponin I release, with PreC providing the most pronounced reductions. Neither combining PerC and PostC nor combining PreC, PerC, and PostC conferred additional cardioprotection, suggesting a ceiling effect due to overlapping mechanism.
Limitations
Only male Sprague–Dawley rats were used, which may limit the generalizability of the findings to female subjects. Given that sex differences in ischemic tolerance and cardioprotection are well documented38, future studies should investigate sex-specific responses to ischemic conditioning, as hormonal and metabolic differences may influence cardioprotective efficacy.
This study focused on acute outcomes—namely infarct size and troponin I levels—which, although established markers of myocardial injury, do not capture long-term functional consequences. Future research should incorporate echocardiographic evaluations to determine parameters such as left ventricular remodeling and systolic function. Invasive hemodynamic measurements were not performed. Future studies should incorporate such assessments to further elucidate the functional consequences of different conditioning strategies.
This study was conducted in healthy rats, appropriate for controlled mechanistic evaluation as outlined in the IMPACT criteria39, but not reflective of the clinical profile of myocardial infarction patients. It is well established that comorbidities such as diabetes, aging, and hyperlipidemia, and commonly used medications including opioids, antiplatelets, and anesthetics can attenuate or abolish cardioprotective signaling40,41,42,43. Incorporating these confounders into future preclinical models is essential to assess the true translational potential of candidate cardioprotective strategies.
Data availability
The datasets generated during and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PreC:
-
Ischemic preconditioning
- PerC:
-
Remote ischemic perconditioning
- PostC:
-
Ischemic postconditioning
- LAD:
-
Left anterior descending artery
- cTnI:
-
Cardiac troponin I
- TTC:
-
2,3,5-Triphenyltetrazolium chloride
References
Bulluck, H. & Hausenloy, D. J. Ischaemic conditioning: Are we there yet?. Heart 101, 1067–1077 (2015).
Elmahdy, A. et al. Ischemic preconditioning affects phosphosites and accentuates myocardial stunning while reducing infarction size in rats. Front. Cardiovasc. Med. 11, 1376367 (2024).
Hausenloy, D. J. & Yellon, D. M. Ischaemic conditioning and reperfusion injury. Nat. Rev. Cardiol. 13, 193–209 (2016).
Murry, C. E., Jennings, R. B. & Reimer, K. A. Preconditioning with ischemia: A delay of lethal cell injury in ischemic myocardium. Circulation 74, 1124–1136 (1986).
Donato, M., Bin, E. P. & V DA, Gelpi RJ,. Myocardial remote ischemic preconditioning: From cell biology to clinical application. Mol. Cell Biochem. 476, 3857–3867 (2021).
Kharbanda, R. K. et al. Transient limb ischemia induces remote ischemic preconditioning in vivo. Circulation 106, 2881–2883 (2002).
Zhao, Z. Q. et al. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: Comparison with ischemic preconditioning. Am. J. Physiol. Heart. Circ. Physiol. 285, H579-588 (2003).
Kin, H. et al. Postconditioning attenuates myocardial ischemia-reperfusion injury by inhibiting events in the early minutes of reperfusion. Cardiovasc. Res. 62, 74–85 (2004).
Schmidt, M. R. et al. Intermittent peripheral tissue ischemia during coronary ischemia reduces myocardial infarction through a KATP-dependent mechanism: First demonstration of remote ischemic perconditioning. Am. J. Physiol. Heart Circ. Physiol. 292, H1883-1890 (2007).
Sachdeva, J., Dai, W., Gerczuk, P. Z. & Kloner, R. A. Combined remote perconditioning and postconditioning failed to attenuate infarct size and contractile dysfunction in a rat model of coronary artery occlusion. J. Cardiovasc Pharmacol. Ther. 19, 567–573 (2014).
Xin, P. et al. Combined local ischemic postconditioning and remote perconditioning recapitulate cardioprotective effects of local ischemic preconditioning. Am. J. Physiol. Heart Circ. Physiol. 298, H1819-1831 (2010).
Lønborg, J. et al. Cardioprotective effects of ischemic postconditioning in patients treated with primary percutaneous coronary intervention, evaluated by magnetic resonance. Circ. Cardiovasc Interv. 3, 34–41 (2010).
Eitel, I. et al. Cardioprotection by combined intrahospital remote ischaemic perconditioning and postconditioning in ST-elevation myocardial infarction: The randomized LIPSIA CONDITIONING trial. Eur. Heart J. 36, 3049–3057 (2015).
Freixa, X. et al. Ischaemic postconditioning revisited: Lack of effects on infarct size following primary percutaneous coronary intervention. Eur. Heart J. 33, 103–112 (2012).
Zhao, W., Hausenloy, D. J., Hess, D. C., Yellon, D. M. & Ji, X. Remote ischemic conditioning: Challenges and opportunities. Stroke 54, 2204–2207 (2023).
White, S. K. et al. Remote ischemic conditioning reduces myocardial infarct size and edema in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 8, 178–188 (2015).
Bøtker, H. E. et al. Remote ischaemic conditioning before hospital admission, as a complement to angioplasty, and effect on myocardial salvage in patients with acute myocardial infarction: A randomised trial. Lancet 375, 727–734 (2010).
Rentoukas, I. et al. Cardioprotective role of remote ischemic periconditioning in primary percutaneous coronary intervention: Enhancement by opioid action. JACC Cardiovasc Interv. 3, 49–55 (2010).
Prunier, F. et al. The RIPOST-MI study, assessing remote ischemic perconditioning alone or in combination with local ischemic postconditioning in ST-segment elevation myocardial infarction. Basic Res. Cardiol. 109, 400 (2014).
Wei, M. et al. Repeated remote ischemic postconditioning protects against adverse left ventricular remodeling and improves survival in a rat model of myocardial infarction. Circ. Res. 108, 1220–1225 (2011).
Espinosa, A. S. et al. Differences between cardiac troponin I vs. T according to the duration of myocardial ischaemia. Eur. Heart J. Acute Cardiovasc. Care 12, 355–363 (2023).
Bøtker, H. E. et al. Practical guidelines for rigor and reproducibility in preclinical and clinical studies on cardioprotection. Basic Res. Cardiol. 113, 39 (2018).
Ryabov, V. V. et al. The signaling mechanism of remote postconditioning of the heart: Prospects of the use of remote postconditioning for the treatment of acute myocardial infarction. Cells 12, 1622 (2023).
Rosenberg, J. H., Werner, J. H., Moulton, M. J. & Agrawal, D. K. Current modalities and mechanisms underlying cardioprotection by ischemic conditioning. J. Cardiovasc. Transl. Res. 11, 292–307 (2018).
Hausenloy, D. J., Mocanu, M. M. & Yellon, D. M. Cross-talk between the survival kinases during early reperfusion: Its contribution to ischemic preconditioning. Cardiovasc. Res. 63, 305–312 (2004).
Tong, C. & Zhou, B. Cardioprotective strategies in myocardial ischemia-reperfusion injury: Implications for improving clinical translation. J. Mol. Cell Cardiol. Plus 11, 100278 (2025).
Davidson, S. M. et al. Multitarget strategies to reduce myocardial ischemia/reperfusion injury: JACC review topic of the week. J. Am. Coll. Cardiol. 73, 89–99 (2019).
Heusch, G. Myocardial ischaemia-reperfusion injury and cardioprotection in perspective. Nat. Rev. Cardiol. 17, 773–789 (2020).
Boengler, K. et al. Cardioprotection by ischemic postconditioning is lost in aged and STAT3-deficient mice. Circ. Res. 102, 131–135 (2008).
Basalay, M. et al. Remote ischaemic pre- and delayed postconditioning—Similar degree of cardioprotection but distinct mechanisms. Exp. Physiol. 97, 908–917 (2012).
Heusch, G. Molecular basis of cardioprotection: Signal transduction in ischemic pre-, post-, and remote conditioning. Circ. Res. 116, 674–699 (2015).
Skyschally, A. et al. Ischemic postconditioning: Experimental models and protocol algorithms. Basic Res. Cardiol. 104, 469–483 (2009).
Hausenloy, D. J. et al. Ischaemic conditioning and targeting reperfusion injury: A 30 year voyage of discovery. Basic Res. Cardiol. 111, 70 (2016).
Pagliaro, P. & Penna, C. Redox signalling and cardioprotection: Translatability and mechanism. Br. J. Pharmacol. 172, 1974–1995 (2015).
Chen, L. et al. Myocardial ischemia-reperfusion injury: The balance mechanism between mitophagy and NLRP3 inflammasome. Life Sci. 355, 122998 (2024).
Yu, J. W. & Lee, M. S. Mitochondria and the NLRP3 inflammasome: Physiological and pathological relevance. Arch. Pharm. Res. 39, 1503–1518 (2016).
Gao, T. et al. Interplay between chromosomal alterations and gene mutations shapes the evolutionary trajectory of clonal hematopoiesis. Nat. Commun. 12, 338 (2021).
Pylova, T. et al. Associations between female sex hormones, estrous cycle, ischemic preconditioning and myocardial infarct size after ischemia-reperfusion injury. Basic Res. Cardiol. 120(2), 321–333 (2025).
Lecour, S. et al. IMproving preclinical assessment of cardioprotective therapies (IMPACT) criteria: Guidelines of the EU-CARDIOPROTECTION COST Action. Basic Res. Cardiol. 116, 52 (2021).
Kleinbongard, P., Bøtker, H. E., Ovize, M., Hausenloy, D. J. & Heusch, G. Co-morbidities and co-medications as confounders of cardioprotection-Does it matter in the clinical setting?. Br. J. Pharmacol. 177, 5252–5269 (2020).
Ferdinandy, P. et al. Interaction of cardiovascular nonmodifiable risk factors, comorbidities and comedications with ischemia/reperfusion injury and cardioprotection by pharmacological treatments and ischemic conditioning. Pharmacol. Rev. 75, 159–216 (2023).
Heusch, G. & Gersh, B. J. Is cardioprotection salvageable?. Circulation 141, 415–417 (2020).
Heusch, G. & Kleinbongard, P. Cardioprotection research has left its comfort zone. Eur. Heart J. 45, 1568–1570 (2024).
Funding
Open access funding provided by University of Gothenburg. This project has received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation programme (grant agreement no 948665), the Swedish Heart–Lung Foundation [20180555], The Swedish Research Council (2020–00732), ALF, the Swedish Society of Medical Research [181015], and Konung Gustaf V:s och Drottning Victorias Stiftelse. These funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Ahmed Elmahdy conceptualized, designed the study, analyzed the data, and drafted the manuscript. Ahmed Elmahdy, Maryna Krasnikova, Tetiana Pylova, Abhishek Jha, Aaron Shekka Espinosa, Ermir Zulfaj, and Mana Kalani, performed in vivo experiments and image analyses. Aditi Banerjee and Ola Hammarsten conducted troponin analysis. Erik Axel Andersson and Elmir Omerovic revised the initial draft of the manuscript. Björn Redfors supervised all aspects of the study and obtained funding.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All experiments were approved by the Gothenburg Animal Ethics Committee (Dnr 5.8.18–11014/2023) and performed after the ARRIVE guidelines and in accordance with the local legislation and institutional requirements.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Elmahdy, A., Krasnikova, M., Jha, A. et al. Individual and combined effects of ischemic conditioning strategies on infarct size after myocardial ischemia reperfusion. Sci Rep 15, 32006 (2025). https://doi.org/10.1038/s41598-025-17442-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17442-y