Abstract
Dry eye is among the most prevalent complications following refractive surgery, significantly impacting the training and daily lives of recruits. While recent years we have witnessed some advancements in understanding the occurrence and progression of dry eye, the specific effects of refractive surgery on this condition remain unclear. This study aims to investigate the impact of refractive surgery on dry eye among 300 army recruits. A series of examinations specific to dry eye were conducted on the subjects using the OSDI questionnaire and the ocular surface comprehensive analyzer. The correlation between refractive surgery and dry eye was analyzed in conjunction with dry eye symptoms and related data. Additionally, optical coherence tomography (OCT) was employed to observe fundus changes in dry eye patients, comparing those with low to moderate myopia against patients with high myopia prior to surgery. The morphology of the meibomian glands in the upper eyelid was assessed using the Keratograph 5M ocular surface analyzer, where the area of meibomian gland loss was calculated and scored, facilitating an exploration of the relationship between meibomian gland loss and dry eye. Furthermore, the dry eye detection rates of Non-Invasive Break-Up Time (NIBUT), Lipid Layer Thickness Measurement (LTMH), and basal Schirmer secretion (SIT) were calculated, and the diagnostic differences among these three methods for dry eye were analyzed. According to the OSDI questionnaire, 117 (39%) patients opted for SMILE, 60 (20%) for F-LASIK, and 123 (41%) for LASIK. Among the recruits, 78 (26%) were diagnosed with dry eye following refractive surgery. Single factor and multiple logistic regression analyses indicated that LASIK may serve as an independent risk factor for the development of dry eye after refractive surgery. Furthermore, the incidence of leopard-pattern fundus was significantly higher in recruits with high myopia compared to those with low to moderate myopia. Keratograph5M assessments revealed that 52.6% of patients exhibited no meibomian gland loss; 45.5% had meibomian gland loss of less than 1/3; 1.9% experienced meibomian gland loss ranging from 1/3 to 2/3; and no patients had meibomian gland loss exceeding 2/3. These results suggest that there is no direct relationship between dry eye and meibomian gland loss following refractive surgery. Additionally, the dry eye detection rate using non-invasive tear break-up time (NIBUT) was 92.6%, while the detection rate for LTMH dry eye was 91.0%. The basal Schirmer test (SIT) yielded a dry eye detection rate of 78.2%, indicating that non-invasive tear assessment methods have a higher detection rate for dry eye. The incidence of dry eye among recruits following excimer laser corneal refractive surgery is significantly higher than that observed with other surgical methods, suggesting that it may represent an independent risk factor for dry eye post-refractive surgery. Consequently, we do not recommend the use of laser in situ keratomileusis for refractive surgery.
Similar content being viewed by others
Introduction
With the advent of the new era, an increasing number of aspiring young individuals are actively joining the army. The reform of the military service system, along with the enhancement of the military service culture, has led to a higher detection rate of myopia1,2. According to the latest data released by the National Health Commission in 2023, the overall myopia rate among children and adolescents in China stands at 52.7%. This includes rates of 35.6% among primary school students, 71.1% among junior high school students, and 80.5% among senior high school students. Recent trends indicate that the age of high incidence of myopia has shifted from 8 to 12 years to 6–10 years3,4. To meet the vision standards required for military service, there has been a significant increase in the number of recruits undergoing refractive surgery to correct myopia1. However, studies indicate that the eyeball remains fragile following such surgery, leading to potential complications such as dry eye, glare, loss of night vision, and a gradual decline in distance vision5. During the intense military training, these visual impairments are more likely to manifest, thereby affecting combat readiness6. Consequently, ensuring the safety and health of recruits post-refractive surgery has become a critical component of eye health protection.
Dry eye is one of the most common complications following refractive surgery. Symptoms of dry eye include redness, dryness, a foreign body sensation, fatigue, discomfort, excessive blinking, and blurred vision, which often improves after blinking7. Research indicates that dry eye symptoms can manifest as early as the first day post-surgery, with an incidence rate ranging from 69 to 85% within 7–14 days7. Patients with a history of dry eye symptoms tend to experience more severe manifestations, which may persist for up to six months post-surgery and can even progress to chronic dry eye8. For recruits undergoing myopia correction, the demanding training schedules during the initial training period may hinder continuous observation and targeted treatment, resulting in a higher likelihood of experiencing dry eye symptoms. This condition can adversely affect both the physical and mental well-being of soldiers and may even impede their training9. Consequently, early prevention, detection, and treatment of dry eye are crucial for enhancing the quality of life for soldiers and improving the combat effectiveness of military units.
This paper will explore the impact of refractive surgery on dry eye syndrome. We will first conduct a series of dry eye-specific tests on the study subjects using the OSDI questionnaire and other equipment, such as the ocular surface analyzer. We will combine dry eye symptoms and related data to analyze the correlation between refractive surgery and dry eye syndrome. Additionally, we will utilize OCT to observe the progression of Fundus tessellation (FT) in dry eye patients and compare the fundi of pre-operative low-to-moderate myopic patients with those of pre-operative high myopic patients. Furthermore, we will employ the infrared meibomian gland photography function of the Keratograph 5M corneal surface analyzer to document the morphology of the upper eyelid meibomian gland, calculate the area of meibomian gland deficiency, and assign scores. This will allow us to explore the relationship between meibomian gland deficiency and the occurrence of dry eye. Finally, we will conduct a statistical analysis of the dry eye detection rates of NIBUT, LTMH, and SIT, respectively, to assess the differences in dry eye diagnosis among these three tear assessment methods.
Materials and methods
Study population and questionnaire survey
A total of 1017 OSDI questionnaires were collected from new recruits who underwent a series of health check-ups at the Fragrant Hill outpatient department of the Eighth Medical Center of the PLA (Chinese People’s Liberation Army)General Hospital from March 5, 2024 to March 22, 2024.The questionnaires were administered by professional ophthalmologists, who first informed the recruits that the survey was unrelated to discharge, thereby ensuring the reliability and authenticity of the results.The study was approved by the Ethical Review Board of the People’s Liberation Army General Hospital (approval ID:309202410535013290) and conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice Guidelines. All participants gave informed consent.All participants gave their oral consent before filling out the questionnaire.The questionnaire was filled out voluntarily by the participant, and if the participant completed the questionnaire, it was proved that he had given informed consent. The questionnaire included the following sections: (1) General demographic information, which encompassed name, gender, age, education level, preoperative myopia degree, and surgical methods. (2) Dry eye symptoms, which included eye redness, dryness, foreign body sensation, fatigue, discomfort, excessive blinking, and blurred vision (which improves after blinking) and (3) Additional factors, such as contact lens use, smoking history, Systemic health history (including Sjogren’s syndrome, rheumatoid arthritis, etc.), and medication history (including antidepressants and eye drops).
Research methods
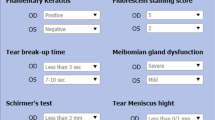
Using the Keratograph5M (The ocular surface analyzer, also known as the “dry eye detector”, is a kind of non-invasive ocular surface examination instrument with automatic imaging and analysis functions. It has many examination and analysis functions, such as tear meniscus height measurement, non-contact tear film break-up time examination, lipid layer examination, meibomian gland imaging and so on), we measured non-invasive first tear film break-up time (NIBUTf), non-invasive average tear film break-up time (NIBUTav), and lower tear meniscus height (LTMH) in survey subjects who had undergone LASIK surgery. The results were then correlated with Schirmer I test (SIT) scores, corneal fluorescein staining (CFS) scores, and subjective symptom scores for dry eye.
-
(1)
Perform the Oculus Eye Surface Analysis System (Oculus Keratograph 5M; JENVIS Pro, JP) assessments, including Non-Invasive Break-Up Time (NIBUTf), Average Non-Invasive Break-Up Time (NIBUTav), automatic dry eye grading, and the Lateral Tear Meniscus Height (LTMH) examination. Instruct the patient to position their lower jaw on the chin rest and press their forehead against the forehead strap. The patient should keep their eyes naturally open and focus on the central red dot after the Placido disk, which contains 22 red concentric circles, is projected onto their cornea. Once the patient successfully focuses, instruct them to blink twice and then maintain their eyes open until the next blink. The instrument will automatically present the tear film image and display the measurement values, including the automatic dry eye grading. The results were measured twice and the mean value was calculated. The LTMH measurement reflects the amount of tear secretion, with a value greater than 0.2 mm considered normal. The Oculus Eye Surface Analysis System can determine the non-invasive LTMH and will automatically present the tear river image. For a more intuitive assessment of tear river continuity and secretion, manually measure the length of the tear river between the upper and lower extremes, ensuring more objective results. Measure twice and calculate the average value.
-
(2)
CFS: Apply 5 g/L levofloxacin eye drops to the sodium fluorescein strips, then insert the strips into the lower conjunctival sac of the subject. Instruct the subject to blink fully and maintain a steady gaze. Under the slit lamp, observe the condition of the CFS and assign a score.
-
(3)
SIT: Position the tear film test paper on the inner third of the lower conjunctival sac of the subject, and measure the wet length of the filter paper after 5 min.
Observing indicators
NIBUTf, NIBUTav, LTMH, CFS, SIT, and dry eye SSS were observed. Non-invasive tear film break-up time was measured using the Oculus ocular surface analyzer, followed by SIT and CFS assessments, with an interval exceeding 30 min.
Diagnostic criteria for dry eye
According to the “2020 Expert Consensus on the Clinical Diagnosis and Treatment of Dry Eye,” patients exhibiting symptoms such as dryness, foreign body sensation, burning sensation, fatigue, discomfort, vision fluctuation, and other subjective ocular surface symptoms were diagnosed with dry eye if their tear break-up time (BUT) was less than or equal to 5 s or their Schirmer’s test (SIT) was less than or equal to 5 mm over 5 min. Additionally, patients presenting with one of the aforementioned subjective ocular surface symptoms, a BUT greater than 5 s but less than or equal to 10 s, or a SIT greater than 5 mm over 5 min but less than or equal to 10 mm over 5 min, and a positive corneal staining score (CFS10), were also diagnosed with dry eye10.
Classification of dry eye severity
Mild: There are no obvious signs of ocular surface damage, with corneal fluorescein staining spots fewer than 5 and a break-up time (BUT) of 2 s or more. Moderate: The extent of corneal damage observed under the slit lamp microscope did not exceed 2 quadrants, and/or the number of corneal fluorescein staining spots ranged from 5 to fewer than 30, with a BUT of 2 s or more. Severe: Corneal damage involved 2 quadrants or more, and/or there were 30 or more fluorescent staining spots, with a BUT of less than 2 s. The fluorescein staining spots in the cornea coalesced into thick spots, sheets, or filaments11,12.
CFS scoring criteria
Corneal epithelial staining was assessed and scored following fluorescein sodium staining. The cornea was divided into three quadrants based on the pupil area, and each quadrant was scored independently. Corneal fluorescence staining (CFS) : The CFS was scored using a 12-point scale: the cornea was divided into 4 quadrants, each quadrant was 0–3 points, 0 points: no staining; 1 point: 1–30 punctate staining; 2 points: > 30 spots stained but not fused; Score 3: corneal punctate pigmentation fusion, filamentous matter and ulceration. The sum of the four quadrant scores was equal to the corneal fluorescein staining score.The scoring system for the Corneal Fluorescein Staining (CFS) is as follows: 0 points for no punctate staining; 1 point for 1–5 punctate stains.2 points for 6–10 punctate stains, and 3 points for more than 10 punctate or patchy staining. The scores from the three quadrants were summed to obtain a total score ranging from 0 to 9 points13.
Statistical analysis
SPSS 20.0 and Graphpad Prism 5.0 were used for statistical analysis. Quantitative data were expressed as mean ± standard deviation. The two-tailed student T test was used to analyze the differences between the two groups. Classification data were evaluated by χ2 test. P < 0.05 was considered statistically significant. All experiments were repeated three times.
Results
Results of questionnaire survey
A total of 1017 questionnaires were distributed, and all 1017 valid questionnaires were returned, resulting in an effective response rate of 100%. Among the respondents, 300 individuals (29.4%) reported having undergone refractive surgery. Specifically, 117 (39%) underwent small incision lenticule extraction (SMILE), 60 (20%) underwent femtosecond laser-assisted laser in situ keratomileusis (F-LASIK), and 123 (41%) underwent conventional laser in situ keratomileusis (LASIK). The postoperative uncorrected visual acuity was recorded as ≥ 4.9.
Correlation between occurrence of dry eye and clinical features
To investigate the relationship between dry eye syndrome and clinical data, we conducted a single-factor correlation analysis involving subjects who had undergone refractive surgery (see Table 1). Our findings indicate that the diagnosis of dry eye syndrome post-refractive surgery was not correlated with gender, age, education level, or history of eye diseases. However, it was significantly correlated with the surgical method and preoperative myopia. Notably, the positive rate of dry eye in patients with low and moderate myopia prior to refractive surgery was lower than that in patients with high myopia. Additionally, dry eye was found to be more prevalent in individuals undergoing traditional laser in situ keratomileusis (LASIK).
Furthermore, multivariate logistic regression analysis revealed that dry eye was significantly associated with surgical procedures (p = 0.001, odds ratio [OR] = 2.467, 95% confidence interval [CI] 1.392–5.286). Therefore, we speculate that conventional laser in situ keratomileusis (LASIK) may represent an independent risk factor for the development of dry eye following refractive surgery.
Comparison of preoperative fundus observations between recruits with low to moderate myopia (< 600°) and recruits with high myopia (≥ 600°)
It has been reported in the literature that myopia can significantly impact the fundus14. To analyze the effect of preoperative myopia on the fundus, we conducted an Optical coherence tomography(OCT) examination on 78 new recruits (156 eyes) with dry eye. The recruits included those with low to moderate myopia (< 600°) and high myopia (≥ 600°) prior to surgery. Fundus tessellation (FT) can be categorized into four grades: none, mild, moderate, and severe, based on the visibility of choroidal vessels in the retina15,16,17. The results indicated that the likelihood of fundus tessellation was significantly higher in recruits with high preoperative myopia compared to those with low to moderate preoperative myopia. Among recruits with low to moderate preoperative myopia, fundus tessellation was observed in only 2 of 18 eyes, yielding a probability of 11.1%, both of which exhibited mild changes, as illustrated in Fig. 1. In contrast, OCT results for recruits with high myopia prior to surgery revealed varying degrees of fundus tessellation in 34 of 138 eyes, resulting in a total probability of 24.6%, as shown in Table 2; Fig. 2. The severity of fundus tessellation was greater in recruits with high preoperative myopia than in those with low to moderate preoperative myopia.
Analysis of meibomian gland loss in dry eye patients
Severe dysfunction and loss of meibomian glands have been identified as significant factors contributing to dry eye syndrome18. To investigate the extent of meibomian gland loss and its associated factors in patients diagnosed with dry eye, a total of 78 patients (156 eyes) were enrolled in this study. The infrared meibomian gland photography capability of the Keratograph 5M ocular surface analyzer was utilized to capture the morphology of the meibomian glands in the upper eyelid. All examination items were conducted and scored by the same ophthalmologist at our hospital. The scoring criteria were as follows: no meibomian gland loss was assigned a score of 0; meibomian gland loss of less than 1/3 received 1 point; loss between 1/3 and 2/3 was scored as 2 points; and meibomian gland loss greater than 2/3 was given a score of 319. The results indicated that 52.6% of the patients exhibited no meibomian gland loss, while 45.5% had less than 1/3 loss, and 1.9% had loss ranging from 1/3 to 2/3. Notably, there were no cases of meibomian gland loss exceeding 2/3, as shown in Table 3; Fig. 3. Furthermore, the findings suggest that dry eye resulting from refractive surgery is not directly correlated with meibomian gland loss.
Comparison of three tear assessment methods in the diagnosis of dry eye
Three tear eye assessment methods commonly used in clinical practice for the diagnosis of dry eye include NIBUT, LTMH and SIT20,21. Due to variations in regional and economic development, not all medical institutions are equipped to implement comprehensive examination methods for patients. Therefore, it is essential to investigate the differences among NIBUT, LTMH, and SIT in diagnosing dry eye, aiming to provide a quick, simple, and efficient examination method for clinical diagnosis. A total of seventy-eight patients (156 eyes) diagnosed with dry eye were selected for this study. The differences in the diagnostic performance of NIBUT, LTMH, and SIT were analyzed. The detection rate for dry eye using NIBUT was found to be 92.6%, while the detection rate for LTMH was 91.0%, and for SIT, it was 78.2% (see Table 4). These findings indicate that non-invasive tear eye evaluation methods demonstrate a high detection rate for dry eye, suggesting that such methods should be prioritized in medical institutions with limited resources when comprehensive dry eye examination methods are not feasible.
Discussion
Dry eye is a chronic ocular surface disease that arises from multiple factors. It is characterized by tear film instability and an imbalance in the ocular surface microenvironment, which are attributable to qualitative, quantitative, and kinetic abnormalities of the tears. This condition may be accompanied by ocular surface inflammation, tissue damage, and nerve abnormalities, leading to a range of ocular discomfort symptoms and potential visual dysfunction22,23. The interplay between ocular surface microenvironment imbalance and tear film instability is reciprocal24. Ocular surface or systemic inflammation can precipitate dry eye, while persistent dry eye and unresolved tear film instability can further exacerbate ocular surface inflammation. Thus, dry eye and inflammation are mutually causal25. This article primarily examines the relationship between refractive surgery and dry eye, along with its clinical characteristics.
In this study, we utilized the OSDI questionnaire to assess the degree of dry eye in recruits, revealing that the incidence of dry eye following myopic surgery was 26%. Among the factors examined, gender, age, education, and a history of eye diseases appeared to have minimal impact on dry eye incidence. In contrast, surgical methods, preoperative myopia, and exceeding 2 h of daily screen time post-surgery significantly influenced dry eye outcomes. Our findings indicated that the incidence of dryness after conventional laser in situ keratomileusis (LASIK) was notably higher compared to that of full femtosecond laser small incision lenticule extraction and femtosecond laser-assisted LASIK.The primary contributors to dry eye syndrome post-LASIK are as follows: (1) Corneal epithelial cell damage: The damage inflicted on corneal epithelial cells by the negative pressure suction ring and lamellar knife impairs tear film function and disrupts its stability. (2) Disruption of corneal sensation: The nasal and temporal branches of the ciliary nerve are severed during LASIK surgery, resulting in a significant reduction in corneal sensation in the early postoperative period, which adversely affects the tear secretion reflex. (3) Changes in ocular surface contour: LASIK surgery reduces the regularity of the corneal surface, which is crucial for maintaining a stable tear film. An irregular corneal epithelial surface can lead to tear film rupture26,27. Furthermore, our data analysis revealed a significant correlation between the occurrence of dry eye and LASIK, leading us to speculate that conventional LASIK may represent an independent risk factor for dry eye following refractive surgery.Although the number of high myopia patients with preoperative myopia exceeding 600 degrees was greater, and the proportion of patients experiencing severe dry eye was higher among those with dry eye, this factor did not emerge as an independent predictor in the variable analysis. This lack of significance may be attributed to the limited sample size. In the future, we intend to validate these findings by collecting samples from a larger number of clinical research centers. It has been reported that 30%-40% of patients have different degrees of meibomian gland dysfunction before refractive surgery. Therefore, it should be paid attention to before surgery. Physical therapy such as meibomian gland massage before surgery is helpful to reduce the occurrence of dry eye after surgery28,29. Literature review reveals that our research findings are consistent with existing results and clinical observations, indicating that dry eye is the most common complication following LASIK, with an incidence rate of 47–52%. FS-LASIK follows with an incidence rate of approximately 8%, while SMILE is the least frequent. The underlying causes include corneal nerve damage, alterations in corneal surface regularity, injury to the corneal and conjunctival epithelium, reduction in goblet cells, postoperative inflammatory responses, the toxic effects of preservatives in local anesthetics and perioperative medications, and photodamage from the surgical microscope26,27.
Fundus tesselation (FT) is the initial manifestation of fundus changes associated with high myopia. As axial length elongates and the eyeball expands, the ocular wall tissue becomes thinner in cases of high myopia. This thinning is characterized by degeneration of choroidal vessels, progressive thinning and atrophy of the retinal pigment epithelium (RPE), and the formation of early FT30. Studies indicate that the vascular diameter and thickness measured by micrometry reveal significant variability in the vascular wall of individuals with high myopia, which may ultimately lead to choroidal vascular thrombosis and retinal vascular occlusion31. Furthermore, research has shown that the incidence of FT is as high as 85.7% among individuals with diopters exceeding − 10.00 DS32. In conclusion, FT frequently occurs in high myopia and serves as a critical feature in the diagnosis of retinochoroidal diseases. Therefore, early screening for FT is essential for the diagnosis and treatment of related fundus diseases.
Normal meibomian glands are arranged in parallel without loss. The loss of meibomian glands is a typical sign of meibomian gland dysfunction.Morphological changes in the meibomian glands can lead to dysfunction, resulting in a series of pathophysiological changes33. Meibomian gland secretion, known as meibum, is released through the opening of the skin-mucosa junction at the eyelid margin, facilitated by the extrusion that occurs during eyelid closure with each blink. Meibum evenly coats the outermost layer of the tear film, forming the lipid layer, which plays a crucial role in preventing the rapid evaporation of tears. When meibomian gland function is impaired, the quality and quantity of meibomian ester secretion are reduced, leading to a thinning of the lipid layer of the tear film and an acceleration of the evaporation of the aqueous layer. This dysfunction results in symptoms such as dryness, itching, and stinging34,35,36. It has been reported that there is a close relationship between contact lens wearing and meibomian gland dysfunction, which is mainly reflected in the following aspects: chronic irritation and obstruction. Long-term contact lens wearing may produce chronic irritation to the meibomian glands, leading to meibomian gland opening obstruction and gland reduction. This can affect the normal secretion of lipids (meibum) from the meibomian glands, thereby destroying the stability of the tear film and causing dry eye and other problems. With abnormal tear film and dry eye, contact lenses can interfere with tear distribution and cause the tear film to evaporate too quickly. In meibomian gland dysfunction, insufficient lipid secretion can not effectively lock water, and aggravate dry eye symptoms, which are manifested as dry eyes, foreign body sensation, visual acuity fluctuations, etc. Inflammation and discomfort, contact lenses may cause ocular surface inflammation, further affecting meibomian gland function. Patients with meibomian gland dysfunction are often accompanied by chronic inflammation, which is manifested as eye redness, eye itching and other symptoms. Wearing contact lenses may aggravate these discomfort. Studies have shown that daily contact lenses can reduce sediment accumulation and improve ocular surface health; Eyelid cleaning (such as hot compress and massage) can help to relieve meibomian gland dysfunction and reduce the discomfort of wearing37,38,39.
In conclusion, our findings indicate that while the visual acuity of recruits post-LASIK was within normal limits and the recovery time was relatively short, most recruits underwent surgery 2–3 months prior to recruitment. These recruits were subsequently subjected to high-intensity training in a challenging environment, which may exacerbate the ocular damage associated with dry eye. Dry eye has emerged as a prevalent complication among recruits following LASIK, significantly impacting both their daily lives and training capabilities. Consequently, we do not recommend the use of laser in situ keratomileusis in refractive surgery.
Data availability
Data are available upon reasonable request.
Abbreviations
- 5M:
-
Oculus Keratograph 5M
- JP:
-
JENVIS Pro
- PLA:
-
Chinese People’s Liberation Army
- NIBUTf:
-
Non-invasive break-up time
- NIBUTav:
-
Average non-invasive break-up time
- LTMH:
-
Automatic dry eye grading, and the lateral tear meniscus height
- SIT:
-
Schirmer I test
- CFS:
-
Corneal fluorescein staining
- SSS:
-
subjective symptom scores
- BUT:
-
Break-up time
- SMILE:
-
Small incision lenticule extraction
- F- LASIK:
-
Femtosecond laser-assisted laser in situ keratomileusis
- LASIK:
-
Conventional laser in situ keratomileusis
- FT:
-
Fundus tessellation
- RPE:
-
Retinal pigment epithelium
- OCT:
-
Optical coherence tomography
References
Xu, Y., Mao, Z., Yan, Y., Chen, X. & Zhou, W. Vision criteria for recruits after PRK and LASIK. J. Third Mil. Med. Univ. 27(9), 884887 (2005).
Liu, Y. Research progress of training injuries in recruits during entrainment training. Sporting Goods Technol. 16(16), 133–134 (2021).
Chen, Y., Han, X. & He, M. New enlightenment of epidemiological study on the prevention and control of myopia in Chinese adolescents. Chin. J. Ophthalmol. Vis. Sci. 25(10), 721–725 (2023).
Yang, F., Li, T., Gao, Z., Zhang, X., Xu, S., Tao, S. & Wu, X. The distribution of poor vision and screening myopia among children and adolescents in six provinces of China in 2023. China Health Educ. 40(6), 483–486498 (2024).
Wilson, S. E. Biology of keratorefractive surgery-PRK, PTK, LASIK, SMILE, inlays and other refractive procedures. Exp. Eye Res. 198, 108136 (2020).
Hua, L., Hong, J. & Li, H. Investigation and analysis of corneal refractive surgery in recruits of a certain army in 2022. Southeast Def. Med. 25(2), 216–218 (2023).
Nair, S., Kaur, M., Sharma, N. & Titiyal, J. S. Refractive surgery and dry eye: An update. Indian J. Ophthalmol. 71(4), 1105–1114 (2023).
Randleman, J. B. The state of refractive surgery: 2021 and beyond. J. Refract. Surg. 37 (1), 6 (2021).
Du, G., Li, Z., Song, M., Liu, X. & Huang, Y. Investigation and analysis of ocular refractive surgery in navy recruits. Chin. J. Nauti. Med. Hyperb. Med. 24(2), 97–99 (2017).
Asian Dry Eye Society China Branch; Ocular Surface and Tear Disease Group, Ophthalmology Committee, Cross-Straits Medical and Health Exchange Association. Chinese expert consensus on dry eye: Definition and classification. Chin. J. Ophthalmol. 56(6), 418–422 (2020).
Chen, Y., Liu, M., Wei, M., Gu, H. & Ji, M. The role of tear osmolarity in the pathogenesis of dry eye and progress in its diagnosis and treatment. Int. J. Ophthalmol. 23(1), 84–89. (2023).
Rodriguez-Garcia, A. et al. A practical approach to severity classification and treatment of dry eye disease: A proposal from the Mexican dry eye disease expert panel. Clin. Ophthalmol. 16, 1331–1355 (2022).
Cai, P. Effects of cyclosporine A combined with sodium hyaluronate on tear film break-up time, dry eye symptom score, and corneal fluorescein staining score in the treatment of dry eye. J. Contemp. Med. 21(4), 100–102 (2023).
Miyake, M. et al. Analysis of fundus shape in highly myopic eyes by using curvature maps constructed from optical coherence tomography. PLoS One 9(9), e107923 (2014).
Lyu, H. et al. Characteristics of fundal changes in fundus tessellation in young adults. Front. Med. (Lausanne). 8, 616249 (2021).
Yan, Y. N. et al. Fundus tessellation: Prevalence and associated factors: The Beijing eye study 2011. Ophthalmology 122(9), 1873–1880 (2015).
Badian, R. A., et al. Meibomian gland dysfunction is highly prevalent among first-time visitors at a Norwegian dry eye specialist clinic. Sci. Rep. 11(1), 23412 (2021).
Chan, T. C. Y., Chow, S. S. W., Wan, K. H. N. & Yuen, H. K. L., update on the association between dry eye disease and meibomian gland dysfunction. Hong Kong Med. J. 25(1), 38–47 (2019).
Moreno, I., Verma, S., Gesteira, T. F. & Coulson-Thomas, V. J. Recent advances in age-related meibomian gland dysfunction (ARMGD). Ocul Surf. 30, 298–306 (2023).
Qi, Y., Zhang, C., Zhao, S., Huang, Y. & Yang, R. A novel noninvasive ocular surface analyzer for the assessment of dry eye with meibomian gland dysfunction. Exp. Ther. Med. 13(6), 2983–2988 (2017).
Wang, J. et al. Evaluation of tear film function by oculus keratograph 5M and IDRA ocular surface analyser. Int. Ophthalmol. 44(1), 403 (2024).
Huang, R. et al. Dry eye syndrome: Comprehensive etiologies and recent clinical trials. Int. Ophthalmol. 42(10), 3253–3272 (2022).
Qian, L. & Wei, W. Identified risk factors for dry eye syndrome: A systematic review and meta-analysis. PLoS One 17(8), e0271267. (2022).
Hashemi, H. et al. Prevalence of dry eye syndrome in an adult population. Clin. Exp. Ophthalmol. 42(3), 242–248 (2014).
Marshall, L. L. & Roach, J. M. Treatment of dry eye disease. Consult Pharm. 31(2), 96–106 (2016).
Toda, I. Dry eye after LASIK. Invest. Ophthalmol. Vis. Sci. 59(14), Des109–Des115 (2018).
Raoof, D. & Pineda, R. Dry eye after laser in-situ keratomileusis. Semin Ophthalmol. 29(5–6), 358–362 (2014).
Kim, K. Y. et al. Changes in ocular surface and meibomian gland after penetrating keratoplasty. BMC Ophthalmol. 21(1), 85 (2021).
Spierer, O. et al. The effect of meibomian gland dysfunction on laser-assisted in situ keratomileusis in asymptomatic patients. Ophthalmol. Ther. 12(1), 281–291 (2023).
He, H. L. et al. Fundus tessellated density of pathologic myopia. Asia Pac. J. Ophthalmol. (Phila). 12(6), 604–613 (2023).
Chen, X. Y., He, H. L., Xu, J., Liu, Y. X. & Jin, Z. B. Clinical features of fundus tessellation and its relationship with myopia: A systematic review and meta-analysis. Ophthalmol. Ther. 12(6), 3159–3175 (2023).
Yoshihara, N., Yamashita, T., Ohno-Matsui, K. & Sakamoto, T. Objective analyses of tessellated fundi and significant correlation between degree of tessellation and choroidal thickness in healthy eyes. PLoS One 9(7), e103586 (2014).
Vu, C. H. V. et al. Influence of meibomian gland dysfunction and friction-related disease on the severity of dry eye. Ophthalmology 125(8), 1181–1188 (2018).
Hom, M. M., Martinson, J. R., Knapp, L. L. & Paugh, J. R. Prevalence of meibomian gland dysfunction. Optom. Vis. Sci. 67(9), 710–712 (1990).
Eom, Y. et al. Comparison of meibomian gland loss and expressed meibum grade between the upper and lower eyelids in patients with obstructive meibomian gland dysfunction. Cornea 33(5), 448–452 (2014).
Dogan, A. S., Kosker, M., Arslan, N. & Gurdal, C. Interexaminer reliability of meibography: Upper or lower eyelid?? Eye Contact Lens. 44(2), 113–117 (2018).
Ifrah, R., Quevedo, L. & Gantz, L. Topical review of the relationship between contact lens wear and meibomian gland dysfunction. J. Optom. 16(1), 12–19 (2023).
Gantz, L., Weissman, B. A. & Ifrah, R. Complications and compliance in professionally-managed and self-managed contact lenses compared with non-contact lens wearers. PLoS One 19(9), e0308538 (2024).
Arita, R., Fukuoka, S. & Morishige, N. Meibomian gland dysfunction and contact lens discomfort. Eye Contact Lens 43(1), 17–22 (2017).
Acknowledgements
We acknowledge the assistance from the Eighth Medical Center of Chinese PLA General Hospital.
Funding
This study was supported by The Eighth Medical Center project of PLA General Hospital(2021MS011).
Author information
Authors and Affiliations
Contributions
Fang He and Chao Wang led study design and prepared the manuscript; Ruofei He carried out the experiments and performed statistical analysis; Qian Wang performed data analysis and interpretation; Fangchong Du, Sijin Cheng and Yuanyuan Fang assisted in questionnaire survey collection; Ze Zhao provided data collection. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved by the Ethical Review Board of the People’s Liberation Army General Hospital (approval ID: 309202410535013290) and conducted in accordance with the principles of the Declaration of Helsinki and Good Clinical Practice Guidelines.All participants gave informed consent.All participants gave their oral consent before filling out the questionnaire.The questionnaire was filled out voluntarily by the participant, and if the participant completed the questionnaire, it was proved that he had given informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
He, R., Wang, Q., Du, F. et al. Clinical analysis of dry eye after refractive surgery in army recruits in 2024. Sci Rep 15, 31798 (2025). https://doi.org/10.1038/s41598-025-17572-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-17572-3