Abstract
Ultrasound-guided supra-inguinal fascia iliaca compartment block (FICB) is increasingly used for preoperative analgesia in elderly hip fracture patients. However, the median effective concentration (50% effective concentration, EC50) of ropivacaine required for supra-inguinal FICB for preoperative analgesia has not been determined. This study was designed to evaluate the EC50 of 30 mL ropivacaine to maintain preoperative analgesia for at least 24 h. Twenty-eight consecutive patients aged 75 years or older with acute hip fracture were enrolled. All patients received 30 mL ropivacaine for preoperative analgesia. Dixon’s up-and-down sequential method was used to determine the concentration of ropivacaine. The initial concentration was 0.35%. Successful analgesia was defined as a Numerical Rating Scale (NRS) score for pain less than 4 during movement within the first 24 h after the block. The concentration in each subsequent patient was determined by the response of the previous patient, and concentrations were adjusted at 0.025% intervals. The 50% and 95% effective concentrations (EC50, and EC95) of ropivacaine were calculated using probit regression. The EC50 and EC95 of 30 mL ropivacaine for at least 24-hours effective preoperative analgesia via ultrasound-guided supra-inguinal FICB were 0.248% (95% confidence interval [CI], 0.233–0.262%) and 0.276% (95% CI, 0.262–0.343%), respectively. No adverse events occurred. A single dose of ropivacaine was found to provide effective preoperative analgesia via ultrasound-guided supra-inguinal FICB in elderly patients with hip fracture. The EC50 (95% CI) of 30 mL ropivacaine for preoperative analgesia lasting at least 24 h was 0.248% (0.233–0.262%).
Trial Registration: This trial was registered on UMIN Center Clinical Trials Register (registration number UMIN000050676, date of first trial registration 25/03/2023).
Similar content being viewed by others
Background
Hip fractures are considered one of the most serious of musculoskeletal injuries and are common in elderly patients. The pain caused by hip fractures can be very intense, especially in the preoperative period when the fracture is unstable, and is exacerbated by changes in position including physical examination, treatment or transportation. Severe pain can trigger a range of systemic responses in patients, particularly in the elderly with multiple comorbidities, including stress response and hemodynamic changes, which can result in a series of adverse outcomes, such as delirium, cardio- and cerebrovascular complications, infection, and deep vein thrombosis1. Therefore, to improve the prognosis of these elderly patients, early and aggressive use of safe and effective analgesic treatments are essential.
In recent years, ultrasound-guided peripheral nerve block regional analgesic strategies have been considered superior to systemic analgesic regimens in terms of pain relief, opioid requirements, treatment-related adverse effects, and analgesic success rates2. The fascia iliaca compartment block (FICB) is a widely employed, safe and effective technique for acute pain management in patients with hip fracture. Administration of local anesthetics via the fascia iliaca compartment delivers rapid-onset, site-specific and reliable perioperative analgesia through concomitant blockade of the femoral nerve (FN) and lateral femoral cutaneous nerve (LFCN) and, in selected cases, the obturator nerve (ON)2,3. The FICB procedure is classified into supra- and infra-inguinal approaches based on the puncture site chosen. The supra-inguinal approach is a modified method for performing FICB. It enables easier and more consistent spreading of local anesthetic in a cranial direction than the conventional infra-inguinal approach. This increases the likelihood of achieving complete blockade of all three nerves and providing more effective analgesia1,4,5,6.
While serious complications during FICB procedure are uncommon, elderly patients are particularly vulnerable to adverse effects of local anesthetics (e.g. systemic toxicity, hypotension and arrhythmia). Therefore, it is crucial to determine the appropriate volume and concentration of local anesthetic for supra-inguinal FICB to minimize adverse effects7. Ropivacaine is the most commonly used long-acting local anesthetic for supra-inguinal FICB. Low concentrations of ropivacaine can provide comparable analgesia to higher concentrations while preserving motor function, thereby minimizing local anesthetic-related adverse events and perioperative complications in geriatric patients8. However, the median effective concentration (50% effective concentration, EC50) of ropivacaine required for ultrasound-guided supra-inguinal FICB for preoperative analgesia has not been determined. Thus, we conducted a prospective study to assess the EC50 of 30 mL ropivacaine to maintain preoperative analgesia for at least 24 h.
Methods
Ethics
The prospective study was conducted at Banan Hospital of Chongqing Medical University from April to October 2023, with approval from the Institutional Review Board of Banan Hospital of Chongqing Medical University in 2022 (BNLL-KY-2022-057). Written informed consent was obtained from each participant. This study was conducted in accordance with the principles of the Declaration of Helsinki. The trial was registered on UMIN Center Clinical Trials Register (registration number: UMIN000050676, principal investigator: J.C, date of first trial registration: 25/03/2023) before patient enrolment.
Inclusion and exclusion
Patients with acute hip fracture in American Society of Anesthesiologists (ASA) physical status I through III, aged 75 years or older, of either sex, were included in this study. Exclusion criteria comprised of (1) weight less than 35 kg, (2) any serious systemic disorder, including clinically manifest dysfunction of the heart, brain, lungs, liver, or kidneys, and hypertension refractory to pharmacologic control, (3) evidence of coagulopathy or anticoagulant therapy, (4) known hypersensitivity to ropivacaine, (5) history of chronic pain or chronic preoperative analgesic use, (6) infection at the injection site, (7) neurological or neuromuscular disease, and (8) dementia or evidence of significant visual, hearing, or cognitive impairment. Patients were also excluded from the final analysis if they underwent surgery within 24 h of receiving supra-inguinal FICB regional analgesia.
Blinding method
All blockades were performed by two experienced anesthetists, each of whom had performed at least 50 ultrasound-guided supra-inguinal FICB respectively. The procedural data and blockade efficacy were assessed and recorded by two anesthesiology residents who were not involved in the trial. The same two residents were also responsible for patient follow-up during the first 24 h after the supra-inguinal FICB.
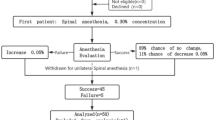
Up-and-Down sequential method
A volume of 30 mL ropivacaine was administered for supra-inguinal FICB. According to the previous study9,10 and our preliminary results, the initial concentration of ropivacaine was set at 0.35%. The interval concentration of ropivacaine in adjacent patients was set at 0.025%. Based on Dixon’s up-and-down sequential method (UDM)11, the result of the block in the previous patient determined the concentration of ropivacaine in the next patient. Successful analgesia was defined as a Numerical Rating Scale (NRS) score for pain less than 4 during movement within the first 24 h after the block. If analgesia was successful, the concentration of ropivacaine was reduced by 0.025% for the next patient. If analgesia failed (defined as a NRS score for pain of 4 or higher during movement within the first 24 h post-block), the concentration of ropivacaine for the subsequent patient was increased by 0.025%. The study was concluded when six or more crossovers (conversion from successful to unsuccessful analgesia or vice versa) were observed. Patients who failed to achieve analgesia were administered oral oxycodone and acetaminophen tablet as a rescue for preoperative analgesia.
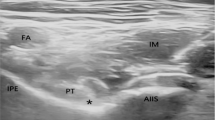
Nerve block technique
On the day of admission, appropriate supra-inguinal FICB was performed in the ward under sterile technique using a Wisonic Clover 50 ultrasound device (Huasheng Medical Technology Co., Ltd., Shenzhen, China). With the patient in the supine position, a high frequency (5–13 MHz) linear probe was placed longitudinally at the level of the anterior superior iliac spine (ASIS) and slid in a medial and caudal direction. After identifying the iliacus muscle (IM), abdominal muscles (AM) and fascia iliaca (FI), the cranial end of the probe was rotated slightly towards the umbilicus until the deep circumflex iliac artery was visualised on the screen. Using an in-plane technique, an 8-cm 22-gauge insulated block needle (Tuoren™, Tuoren Co. Ltd., Henan, China) was then inserted from the caudad side and directed cephalad, penetrating the fascia iliaca and injecting 3 mL of saline to separate the fascia iliaca from the iliac muscle. The predetermined concentration of 30 mL of ropivacaine was injected (Fig. 1). To avoid local anesthetic toxicity, the maximum dose of ropivacaine administered to all the participants was less than 3 mg/kg. Vital signs including heart, noninvasive blood pressure, respiratory rate and pulse oximetry were continuously monitored throughout the procedure.
Outcome assessments
Analgesia was assessed using an 11-point NRS immediately before the block and at 1, 6, 12, and 24 h post-blockade. The assessments were initially conducted at rest to determine the resting NRS pain score, and subsequently repeated with the affected limb passively elevated to 15° to determine the NRS pain score during movement. The higher the score, the more severe the pain. Successful supra-inguinal FICB was defined as a NRS pain score of less than 4 during movement at 1 h post-block. Successful analgesia was defined as a NRS pain score of less than 4 during movement at 6, 12, and 24 h following a successful supra-inguinal FICB. Oral oxycodone and acetaminophen tablet was administered if the patient complained of severe pain at rest within 24 h after successful supra-inguinal FICB. The patient was also declared analgesia unsuccessful. Complications within 24 h of the blockade were recorded, including arrhythmia, dizziness, nausea and vomiting, and hypotension (defined as a > 20% decrease from baseline blood pressure).
Data analysis
In most cases, the sample size of the UDM cannot be predicted in advance. Based on the study by Sebel et al.12, at least six pairs of failure-success crossovers are required to achieve 80% power with an alpha of 0.05 (two-tailed). In our study, we continued sampling until we had obtained six or more crossovers (conversion from successful analgesia to unsuccessful analgesia or vice versa) of concentration.
Statistical analysis was performed by SPSS version 25.0 (SPSS Inc, Chicago, Illinois, USA). Data were presented as mean ± standard deviation or median with upper and lower quartiles for numerical data and percentages for categorical data. Data were analysed with the average of the crossover midpoints and probit regression to calculate the EC50 for 30 mL of ropivacaine to successfully maintain analgesia for at least 24 h. The EC95 and the 95% confidence intervals of both values were also estimated by probit regression.
Results
From April to October 2023, thirty-nine patients with acute hip fracture were enrolled in the present study. Of these, eleven patients were excluded due to failure to meet the inclusion criteria (n = 9) and refusal to sign the informed consent (n = 2). None of the patients in this study underwent surgery within 24 h after FICB regional analgesia. Ultimately, a total of 28 elderly patients (10 males) were evaluated. A flowchart of participants recruitment is displayed in Fig. 2. The demographic characteristics and fracture type are shown in Table 1.
The successful analgesia was achieved in 16 patients and failed in 12 patients. The sequence of positive and negative block results for ultrasound-guided supra-inguinal FICB using 30 mL ropivacaine is graphed in Fig. 3.
The EC50 and EC95 of 30 mL ropivacaine for ultrasound-guided supra-inguinal FICB to provide effective analgesia for at least 24 h were 0.248% (95% confidence interval [CI], 0.233–0.262%) and 0.276% (95% CI, 0.262–0.343%), respectively (Fig. 4).
Concentration-response curve for ropivacaine plotted from probit analysis. The 50% effective concentration of 30 mL ropivacaine for supra-inguinal FICB was 0.248% (95% CI, 0.233–0.262%), and the 95% effective concentration was 0.276% (95% CI, 0.262–0.343%). CI: confidence interval, FICB: fascia iliaca compartment block.
No adverse effects of ropivacaine were observed during the 24-hours follow-up period.
Discussion
Previous studies10,13 have shown that administration of 0.5% ropivacaine significantly relieves pain in elderly hip fracture patients for 36 to 48 h. However, few trials had investigated the duration of effective analgesia and the optimal concentration of ropivacaine as study objectives. This study estimated, for the first time, the EC50 and EC95 of 30 mL ropivacaine to maintain preoperative analgesia for at least 24 h. The EC50 and EC95 (95% CI) values for 30 mL ropivacaine were 0.248% (0.233–0.262%) and 0.276% (0.262–0.343%), respectively.
The efficacy of the regional nerve block is affected by the concentration and volume of the local anesthetic solution, although the exact nature of this relationship is not yet fully understood. To achieve optimal supra-inguinal FICB effects, it is important to ensure sufficient diffusion of the local anesthetic in the lacuna. In clinical practice, the volume of ropivacaine used for supra-inguinal FICB typically ranges from 20 mL to 40 mL1,5,9,14,15. In their cadaver study, Kris Vermeylen et al.16 found that a volume of 20–30 mL was sufficient for staining FN and LFCN, but a volume of 40 mL was required to reach FN, LFCN, and ON. However, it is important to note that dyes diffuse differently than local anesthetic solutions due to their inherent viscosity and density17. Additionally, a pilot study had shown that passive muscle mobilization can facilitate the diffusion of local anesthetic solution within the fascia iliaca compartment in a cranial direction18. Xu et al.19 reported that the estimated volume of the fascia iliaca compartment in the cadavers was (23.4 ± 6.5) cm3. Therefore, a fixed volume of 30 mL of ropivacaine was chosen for this study. This volume was consistent with the amount of ropivacaine used in most previous supra-inguinal FICBs1,9,14.
It is important to note that the intensity of pain in older patients is very heterogeneous and depends on many factors. In fact, some older patients with hip fractures may not experience pain while at rest, even without analgesics, unless they are required to change positions for reasons such as physical examination, treatment, or transportation20. In the present study, we observed that approximately 25% of elderly patients had a NRS pain score of less than 4 at rest prior to undergoing a nerve block. The scenario is consistent with the report by Foss and colleagues2. Therefore, it is crucial to choose the suitable indicator to measure the effectiveness of nerve blocks in patients. Hogh et al.21 evaluated pain using sensory stimulation and hip flexion, while Foss et al.2 measured pain both at rest and in passive motion, in contrast to Monzon et al.22 who only assessed pain at rest. It can be argued that pain relief on hip movement or improvement in hip mobility is a better indicator of analgesic efficacy, which would eliminate confounding factors as positioning and immobilization is itself a method of pain relief. However, the use of NRS pain scores during movement may pose ethical challenges, particularly concerning whether it is ethical to induce pain by move the affected limb.
Early surgery was recommended for most hip fractures due to its association with better functional outcomes, shorter hospital stays, less pain, lower nonunion rates, and fewer postoperative complications23. Current guidelines24,25 indicated that surgery for hip fracture should be performed within 24–48 h of hospital admission. With the implementation of the early surgical quality indicator at our institution, surgery is now possible within 48 h of admission for the majority of patients. The average delay in surgery after admission was 39.7 ± 15.1 h (unpublished data). Therefore, the observation period for analgesic efficacy in this study protocol was 24 h. Participation in the trial did not affect the scheduling of patients’ surgical operations. We supported patients who had completed adequate preoperative preparation to undergo surgery at the earliest opportunity. Patients who underwent surgery within 24 h of receiving supra-inguinal FICB regional analgesia were excluded to avoid interruption of follow-up.
This study has several limitations. Firstly, this study was conducted at a single center. Compared with other populations (e.g., from the United States and Europe), the participants in this study had a smaller physical stature, with a mean height and body mass index (BMI) of 156.5 cm and 21.9 kg·m−2, respectively. The study findings may not be generalizable to other populations, as they only reflect the EC50 of ropivacaine in this specific population. Therefore, it is necessary to conduct further studies in populations with higher height and BMI. Secondly, for ethical reasons, we chose UDM for EC50 calculations to minimize the number of patients with analgesic failure. Although UDM had the advantage of simplicity and low sample size requirements26, it was less reliable for calculating small or large percentiles (e.g., EC95) in small sample size studies. Therefore, the determination of the EC95 in this study, which has a limited sample size, may not be accurate. In contrast, the biased-coin design sequential allocation method26, an improvement and upgrade of UDM, allows for the direct study of effective concentrations in any quartile. This enables accurate extrapolation of high quartile (e.g., EC95) effect concentrations of ropivacaine from the median points. Thirdly, our investigation only considered the EC50 of a fixed volume of 30 mL ropivacaine, limiting the generalizability of our findings. Future studies should explore the EC50 by varying the volume of local anesthetic.
Conclusions
A single 30-mL dose of ropivacaine provided effective preoperative analgesia via ultrasound-guided supra-inguinal FICB in elderly patients with hip fracture. The EC50 (95% CI) for preoperative analgesia lasting at least 24 h was 0.248% (0.233–0.262%). These data can guide the selection of ropivacaine concentration for preoperative analgesia. Further research is necessary to evaluate and refine preoperative analgesia strategies for hip fractures.
Data availability
The de-identified data for individual participants underlying our results can be accessed with approval from the corresponding author 6 months after publication. The study protocol, statistical analyses, and clinical study report will also be available.
References
Chen, L., Shen, Y., Liu, S., Cao, Y. & Zhu, Z. Ultrasound-guided supra-inguinal fascia Iliaca compartment block for older adults admitted to the emergency department with hip fracture: a randomized controlled, double-blind clinical trial. BMC Geriatr. 21, 669. https://doi.org/10.1186/s12877-021-02646-4 (2021).
Foss, N. B. et al. Fascia Iliaca compartment Blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology 106, 773–778 (2007).
Dolan, J., Williams, A., Murney, E., Smith, M. & Kenny, G. N. Ultrasound guided fascia Iliaca block: a comparison with the loss of resistance technique. Reg. Anesth. Pain Med. 33, 526–531 (2008).
Kumar, K. et al. Comparison of conventional infrainguinal versus modified proximal suprainguinal approach of fascia Iliaca compartment block for postoperative analgesia in total hip arthroplasty. A prospective randomized study. Acta Anaesthesiol. Belg. 66, 95–100 (2015).
Desmet, M. et al. A longitudinal supra-inguinal fascia Iliaca compartment block reduces morphine consumption after total hip arthroplasty. Reg. Anesth. Pain Med. 42, 327–333 (2017).
Vermeylen, K. et al. Supra-inguinal injection for fascia Iliaca compartment block results in more consistent spread towards the lumbar plexus than an infra-inguinal injection: a volunteer study. Reg. Anesth. Pain Med. https://doi.org/10.1136/rapm-2018-100092 (2019).
Fredrickson, M. J., Smith, K. R. & Wong, A. C. Importance of volume and concentration for ropivacaine interscalene block in preventing recovery room pain and minimizing motor block after shoulder surgery. Anesthesiology 112, 1374–1381 (2010).
Borgeat, A., Aguirre, J., Marquardt, M., Mrdjen, J. & Blumenthal, S. Continuous interscalene analgesia with ropivacaine 0.2% versus ropivacaine 0.3% after open rotator cuff repair: the effects on postoperative analgesia and motor function. Anesth. Analg. 111, 1543–1547 (2010).
Zhang, C., Dai, W. & He, K. 95% effective volume of ropivacaine for ultrasound-guided supra-inguinal fascia Iliaca compartment block. BMC Anesthesiol. 23, 98. https://doi.org/10.1186/s12871-023-02049-5 (2023).
Levente, B. Z., Filip, M. N., Romaniuc, N. & Gheorghe, S. Efficacy and duration of ultrasound guided fascia Iliaca block for hip fracture performed in the emergency departments. Rom J. Anaesth. Intensive Care. 24, 167–169 (2017).
Dixon, W. J. Staircase bioassay: the up-and-down method. Neurosci. Biobehav Rev. 15, 47–50 (1991).
Sebel, P. S. et al. Reduction of the MAC of desflurane with Fentanyl. Anesthesiology 76, 52–59 (1992).
Kumar, D., Hooda, S., Kiran, S. & Devi, J. Analgesic efficacy of ultrasound guided FICB in patients with hip fracture. J. Clin. Diagn. Res. 10, UC13–UC16 (2016).
Liang, L., Zhang, C., Dai, W. & He, K. Comparison between pericapsular nerve group (PENG) block with lateral femoral cutaneous nerve block and supra-inguinal fascia Iliaca compartment block (S-FICB) for total hip arthroplasty: a randomized controlled trial. J. Anesth. 37, 503–510 (2023).
Yamada, K., Inomata, S. & Saito, S. Minimum effective volume of ropivacaine for ultrasound-guided supra-inguinal fascia Iliaca compartment block. Sci. Rep. 10, 21859. https://doi.org/10.1038/s441598-020-79059-7 (2020).
Vermeylen, K. et al. The effect of the volume of supra-inguinal injected solution on the spread of the injectate under the fascia iliaca: a preliminary study. J. Anesth. 32, 908–913 (2018).
De Miguel Garcia, C., Whyte, M., St James, M. & Ferreira, T. H. Effect of contrast and local anesthetic on dye spread following transversus abdominis plane injection in dog cadavers. Vet. Anaesth. Analg. 47, 391–395 (2020).
Vermeylen, K. et al. The effect of passive muscle mobilization on the distribution of local anesthetics after supra-inguinal fascia Iliaca compartment block, a pilot case study. J. Clin. Anesth. 68 https://doi.org/10.1016/j.jclinane.2020.110100 (2021).
Xu, Z. et al. Fibrous configuration of the fascia Iliaca compartment: an epoxy sheet plastination and confocal microscopy study. Sci. Rep. 10, 1548. https://doi.org/10.1038/s41598-020-58519-0 (2020).
Pinson, S. Fascia Iliaca (FICB) block in the emergency department for adults with neck of femur fractures: a review of the literature. Int. Emerg. Nurs. 23, 323–328 (2015).
Hogh, A., Dremstrup, L., Jensen, S. S. & Lindholt, J. Fascia Iliaca compartment block by junior registrars as a supplement to pre-operative analgesia for patients with hip fracture. Strategies Trauma. Limb Reconstr. 3, 65–70 (2008).
Monzon, D. G., Vazquez, J., Jauregui, J. R. & Iserson, K. V. Pain treatment in post-traumatic hip fracture in the elderly: regional block vs. systemic non-steroidal analgesics. Int. J. Emerg. Med. 3, 321–325 (2010).
Kempenaers, K. et al. Are the current guidelines for surgical delay in hip fractures too rigid? A single center assessment of mortality and economics. Injury 49, 1169–1175 (2018).
O’Connor, M. I. & Switzer, J. A. AAOS clinical practice guideline summary: management of hip fractures in older adults. J. Am. Acad. Orthop. Surg. 30, e1291–e1296 (2022).
National Institute for Health and Care Excellence (NICE). NICE clinical guidelines, No.124, Hip fracture: management. London: National Institute for Health and Care Excellence (NICE). ; (2023). Retrieved from https://www.nice.org.uk/guidance/CG124. (Accessed October 29, 2023).
Pace, N. L. & Stylianou, M. P. Advances in and limitations of up-and-down methodology: a precis of clinical use, study design, and dose Estimation in anesthesia research. Anesthesiology 107, 144–152 (2007).
Acknowledgements
This study was conducted at Banan Hospital of Chongqing Medical University. We are extremely grateful to everyone who participated and cooperated in the surveys.
Funding
No funding was received by authors for this study.
Author information
Authors and Affiliations
Contributions
All authors made substantial contributions to the study. The study protocol was written by KQ, DJR, HWC and JC with support from the academic supervisory team of TYL, CHL, TZC and YC. Data collection and analysis was completed by KQ and DJR with support from TYL, CHL and JC. Statistical analysis was done by HWC and TZC with support from DJR and YC. The manuscript was drafted by KQ, DJR, HWC, YC and JC. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was reviewed and approved by the Institutional Review Board of Banan Hospital of Chongqing Medical University on 10th November 2022 (BNLL-KY-2022-057). The study was conducted according to the Declaration of Helsinki. Written informed consent was obtained from all participants prior to participation and they were all assured that they could withdraw their consent at any time without consequences.
Conflict of interest disclosure
All authors disclosed no financial relationships relevant to this publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Qian, K., Ruan, Dj., Chen, Hw. et al. Median effective concentration of ropivacaine for preoperative analgesia under ultrasound-guided supra-inguinal fascia Iliaca compartment block in hip fracture patients. Sci Rep 15, 33566 (2025). https://doi.org/10.1038/s41598-025-18616-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-18616-4