Abstract
Given the increasing attention on unplanned readmissions among paediatric haematopoietic stem cell transplant patients, studies on prevalence and modifiable risk factors are essential for improving transplant outcomes. We analysed the prevalence and risk factors for unplanned readmissions in paediatric patients after haematopoietic stem cell transplantation, the impact of unplanned readmission on overall survival, and how to identify high-risk children and develop intervention strategies. We retrospectively analysed the data and status of unplanned readmissions (within 30 days of discharge) among 548 children who underwent haematopoietic stem cell transplantation at a specialised hospital in Chongqing (June 2013–August 2023). We used logistic regression analysis to identify unplanned readmission risk factors, and Kaplan–Meier survival curves and log-rank tests to analyse survival data. Our findings reveal that 139 children (25.36%) experienced unplanned readmissions and the factors influencing these readmissions include cytomegalovirus serological status before transplantation (OR = 66.324, p < 0.001), conditioning regimen (OR = 2.479, p = 0.036), infection during hospitalisation (OR = 11.914, p = 0.011), and length of hospitalisation (OR = 2.907, p = 0.005). Within the 1-year follow-up, 85 children (15.51%) died. Unplanned readmission significantly reduced survival rates (χ2 = 17.37, p < 0.05). Medical staff should manage unplanned readmissions, particularly among patients with the identified risk factors, and use a targeted comprehensive intervention strategy to improve long-term survival.
Similar content being viewed by others
Introduction
Haematopoietic stem cell transplantation (HSCT) is an important method used to treat malignant or non-malignant haematological and genetic metabolic diseases in children, bringing hope for a cure to thousands of children worldwide every year. According to statistics1, the 5-year and 10-year survival rates of patients undergoing HSCT are 86% and 76%, respectively. Although early and long-term efficacies have significantly improved, the issue of unplanned readmissions in these patients has become increasingly prominent owing to the impact of transplant complications such as chemotherapy toxicity, infection, and organ damage2. Unplanned readmission is an event in which a patient is readmitted to a hospital within a specific time interval after discharge and is largely related to deficiencies in the quality of medical care3. Some previous studies have found that the all-cause incidence of unplanned readmission within 30 days ranges from 27.29 to 39.60% in paediatric transplant cohorts4,5. A high readmission rate not only increases the psychological pressure on children and their families after trauma and the burden of care but also consumes medical resources and induces medical disputes6. It is reported that 12–75% of unplanned readmissions are avoidable3, highlighting the importance of addressing preventable unplanned readmissions.
However, most current studies on paediatric patients undergoing HSCT focus on drug and symptom management after transplantation7 and the prediction and intervention of complications8,9,10. Little attention has been paid to the impact of peri-transplantation status on the transition period after discharge, and there is a lack of accurately understanding the factors influencing unplanned readmission and survival rates. Although some scholars have explored the factors affecting unplanned readmission, the sample size in those studies was small, and they were conducted long ago11. In addition, there are some differences in treatment plans and management models between adult and paediatric patients undergoing HSCT12,13; therefore, the findings focused on adult patients may not be applicable to children undergoing HSCT. Pre-assessment and intervention for potential risks during hospitalisation can effectively reduce the risk of unplanned readmission and improve prognosis. Therefore, this study aimed to investigate the current situation and factors influencing the unplanned readmission of children after HSCT. Moreover, we aimed to explore the impact of unplanned readmission on the survival rate to provide a reference for clinical medical staff to identify high-risk children as early as possible and formulate management programs to prevent unplanned readmissions.
Methods
Design and ethical considerations
This retrospective case-control study was approved by the Ethics Committee of the Children’s Hospital of Chongqing Medical University (approval number: 2024 − 393) and was conducted in accordance with the Declaration of Helsinki. Due to the retrospective nature of the study, the Institutional Review Board waived the need to obtain informed consent.
Participants selection
Children who underwent HSCT and regular follow-ups at a tertiary children’s specialised hospital in Chongqing between June 2013 and August 2023 were selected as participants. Inclusion criteria were: (1) children aged ≤ 18 years; (2) met the indications for allogeneic HSCT 14, received transplantation for the first time, and followed up for > 1 year; (3) met the discharge criteria and followed the doctor’s advice for discharge; and (4) unpredictable rehospitalisation for the same or related disease. The exclusion criteria were: (1) readmission to other hospitals or other departments within the same hospital after discharge; (2) previous hospitalisation in another hospital; (3) incomplete medical records or lost to follow-up; and (4) planned follow-up or re-examination.
Sample size calculation
Based on the literature search4,5,11, expert consultations, and group discussions, 15 factors were included in this study. According to the formula for calculating the sample size15, the sample size should be at least 5–10 times the factor. In addition, a previous study has reported that the incidence of unplanned readmission in patients undergoing HSCT is 27.29%4. After considering a 10% loss to follow-up, the required sample size for this study was 306–611, and 548 patients were included.
Data collection
All paediatric patients selected in this study received guidance on medication and precautions from haematology specialists before discharge and long-term follow-up after discharge. The children were divided into unplanned readmission and no-readmission groups according to whether the interval between the day of discharge and readmission was ≤ 30 days.
Based on a literature search4,5,11, expert consultation, and consideration of clinical practice, the research group discussed and referred to the opinions of senior medical staff of the Department of Haematology and Oncology. The items to be investigated were decided upon, and a uniform information questionnaire was designed. Data were collected from electronic medical and nursing records. Survival data of the children were obtained from outpatient follow-up records and telephone follow-ups. Data included three aspects: (1) demographic factors such as sex, age, and body mass index (BMI), medical insurance, and the education level of the caregiver; (2) disease related factors such as diagnosis, cytomegalovirus serologic status before transplantation, length of hospitalisation, infection during hospitalisation, and grade II to IV graft-versus-host disease; and (3) transplantation related factors such as degree of human leucocyte antigen matching, type of transplant donor, source of stem cells, and conditioning regimen.
In addition, the treatment outcomes (death or survival) of all children during the 1-year follow-up period, readmission time, and reasons for unplanned readmissions were collected. Before transplantation, all children and/or donors underwent weekly cytomegalovirus screening using antigen testing or quantitative polymerase chain reaction. Overall survival is defined as the time from the date of discharge after transplantation to death or the last follow-up. Infection during hospitalisation refers to any documented bacterial, viral, or fungal infection caused by specific microorganisms. Pneumonia, discovered both clinically and radiologically, is also considered an infection. Only the first readmission medical record data of each patient was selected for analysis.
Quality control
Before the start of the study, two transplant specialist nurses responsible for collecting data were trained and informed about the purpose and methods of the study. The inclusion and exclusion criteria were strictly adhered to. The researchers used a unified questionnaire and data entry method to collect and collate the data. Two researchers input the data, and two researchers checked the data. The collected data were periodically sampled and checked. Weekly feedback on the data collection results and corrections of unqualified statistical data were provided. To minimise bias and confounding effects as much as possible, only survival events that occurred after 30 days were considered.
Statistical analysis
SPSS software (version 26.0; IBM, USA) was used to analyse the data. The Shapiro–Wilk test was used to assess the normality of the measurement data. Measurement data with a normal distribution are expressed as mean ± standard deviation; otherwise, they are expressed as median and quartile (P25, P75). Count data are expressed as frequencies and percentages (%). The chi-square test was used to compare count data between the groups. Variables with p < 0.20 in the univariate analysis were included in the multivariate regression model to account for potential confounding or other factors that may obscure their statistical significance in the univariate analysis. Logistic regression analysis was used to screen for factors influencing unplanned readmissions within 30 days. Kaplan-Meier survival curves and log-rank tests were used to analyse survival data. The alpha value was set to 0.05.
Results
General information on children who underwent HSCT and the current situation of unplanned readmissions
In total, 548 children who underwent HSCT were included in this study. Their general information is shown in Table 1. Their average age was 3.6 (range, 2.1–7.3) years. The mean length of hospital stay during transplantation was 50 (46–54) days. Unplanned readmissions occurred approximately 10 days (2–29 days) after discharge. Among the 548 children who underwent HSCT, 139 (25.36%) experienced unplanned readmission within 30 days. In addition, 63% of patients were initially admitted because of fever, and 55% were eventually diagnosed with an infection. Thirty-two per cent of patients were admitted due to gastrointestinal-related issues, and 28% were diagnosed with acute or chronic graft-versus-host disease. The remaining patients were readmitted due to convulsions, recurrence, or abnormal coagulation function.
Analysis of factors influencing unplanned readmissions
As shown in Table 1, according to the results of the univariate analysis, diagnosis, BMI, cytomegalovirus serological status before transplantation, conditioning regimen, and infection during hospitalisation were significantly associated with unplanned readmissions (all p < 0.05).
The dependent variable was unplanned readmissions. Combined with practical experience; sex; age; length of hospitalisation; and variables with a p < 0.20 in the univariate analysis, such as cytomegalovirus serological status before transplantation, conditioning regimen, infection during hospitalisation, length of hospitalisation, diagnosis, BMI, and blood type of the donor and recipient, were independent variables in the multi factor logistic model.
As shown in Table 2, positive cytomegalovirus serological status before transplantation, myeloablative conditioning regimen, infection during hospitalisation, and length of hospitalisation ≥ 51 days were the factors influencing unplanned readmission of paediatric patients who underwent HSCT (all p < 0.05).
Survival analysis
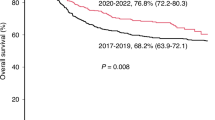
Among the 548 patients, 85 (15.51%) died during the 1-year follow-up period after discharge, with a median follow-up time of 12 months (range, 7–12). The proportion of deaths caused by grade III–IV acute graft-versus-host disease was 40.00% (34/85), severe pneumonia with respiratory failure accounted for 35.29% (30/85), bloodstream infection accounted for 12.94% (11/85), disease recurrence accounted for 4.71% (4/85), intracranial haemorrhage accounted for 2.35% (2/85), implantation dysfunction accounted for 2.35% (2/85), heart failure accounted for 1.18% (1/85), and others accounted for 1.18% (1/85). During the 1-year follow-up period, the mortality rate was 25.18% (35/139) in the unplanned readmission group and 12.22% (50/409) in the no-readmission group. According to the Kaplan–Meier survival curves, the 1-year overall survival was 73.87% (95% CI = 65.51–80.50%) and 86.53% (95% CI = 82.61–89.63%) in the readmission and no-readmission groups, respectively. The log-rank test indicated a significant difference in 1-year overall survival between the unplanned readmission and no-readmission groups (Fig. 1; χ2 = 17.37, p < 0.001).
Discussion
This study is exploratory in nature. Therefore, the observed associations should be regarded as hypothesis-generating rather than confirmatory. The findings of this study showed that the incidence of unplanned readmission in children after HSCT was 25.36%, with the highest incidence in those with acute leukaemia. This rate is much higher than that of international general paediatric patients (5.12%)6 and of children with cancer (9.80%)16, which may be attributed to the temporary suppression of the immune system and an increase in complications during the peri-transplantation period. However, the incidence found in this study was slightly lower than that in previous studies on patients who underwent transplantation4,5. This may be related to the longer hospitalisation time of patients in our centre, as well as the fact that they received discharge guidance from medical staff before discharge and follow-up after discharge, which made their condition more stable at discharge and provided them with certain coping abilities after discharge. In addition, the results showed that the most common reasons for unplanned readmission were infection (55%) and graft versus-host disease (28%), which is consistent with the findings of Shulman et al.11. Therefore, medical staff should pay close attention to unplanned readmissions of patients undergoing HSCT, develop targeted management plans for unplanned readmissions based on influencing factors, comprehensively improve their ability to cope after discharge, and reduce the incidence of unplanned readmissions.
Cytomegalovirus is a double-stranded DNA virus that increases the risk of bone marrow suppression, graft dysfunction, and invasive fungal disease, seriously affecting the prognosis of paediatric patients17. The results of univariate analysis showed that 65.45% of patients with positive cytomegalovirus before transplantation experienced unplanned readmission. Logistic regression analysis suggested that positive cytomegalovirus before transplantation was an important predictor of unplanned readmission in children after HSCT (OR = 66.324, p < 0.001), which was consistent with the results of a previous study18 about the relationship of cytomegalovirus infection and rehospitalization. This elevated risk of unplanned readmission likely stems from the latent-virus reactivation, higher complication rates, and antiviral toxicity—all demanding closer inpatient surveillance. Therefore, medical staff should learn from their experience in the management of adult cytomegalovirus infection based on expert consensus19, refer to clinical situations, and select donors with the same cytomegalovirus serological status before transplantation. Additionally, intensified antiviral prophylaxis and close follow-up are essential.
This study revealed that compared with non-myeloablative pre-treatment, children who underwent myeloablative conditioning regimens were more likely to experience unplanned readmissions (OR = 2.479, p = 0.036), which is consistent with the results of Spring et al.20 who studied the factors influencing readmission in 1,141 patients who underwent allogeneic HSCT. An explanation for this may be that the myeloablative conditioning regimen leads to a prolonged immune function recovery time, more related complications (such as infection and organ toxicity), and treatment-related mortality rates, significantly increasing the risk of transplantation and increasing the likelihood of readmission. A previous study in Brazil indicated that clinical pharmacists could provide professional services at all stages of HSCT, especially in detecting and preventing drug-related problems and reducing the risk of medication errors during the transition period21. Therefore, it is recommended that medical staff collaborate with pharmacists to continuously optimise pre-treatment and nursing plans to promote immune system reconstruction; using pharmaceutical monitoring to regularly monitor concentration and complications to adjust medication plans in a timely manner, helping improve short-term and long-term treatment outcomes for transplant patients.
Infection is one of the most common causes of transplant failure and non-recurrent death in children undergoing HSCT22. The results showed that recorded infections during hospitalisation could predict unplanned readmission in patients undergoing HSCT (OR = 11.914, p = 0.011), similar to that reported by Yamaguchi et al.23. Due to the lack of neutrophils and disruption of mucosal barrier integrity caused by conditioning regimens, bacteria, fungi, or other microorganisms enter the bloodstream and cause bloodstream infections. In addition, the application of immunosuppressive drugs (such as mycophenolate mofetil and cyclosporine) is complex and diverse, which can have a certain impact on the immune function of children and increase the infection rate. Some researchers have confirmed through clinical practice that removing the central venous catheter at discharge can reduce unplanned readmissions due to bacteraemia or sepsis24. Therefore, it is recommended that medical staff strengthen the prevention and management of various opportunistic infections in children with HSCT according to the guidelines22, implement necessary laboratory and imaging examinations, and apply other comprehensive infection prevention and control measures to reduce their readmission risk.
The results of this study demonstrated that the length of hospitalisation was one of the factors influencing unplanned readmission in children undergoing HSCT. The longer the length of hospitalisation, the higher the risk of unplanned readmission (OR = 2.907, p = 0.005) compared with a length of hospitalisation < 51 days (OR = 1.462, p = 0.308). This finding is consistent with the results of a real-world study in France25, which may be related to the fact that the conditioning regimen leads to bone marrow suppression and allogeneic reactions that cause malnutrition and a heavy burden of comorbidity, resulting in a high dependence on medical care and longer hospitalisation time. Nurse-led and evidence-based health education and proactive discharge support are effective ways to reduce the unplanned readmission rate of children undergoing HSCT4. Therefore, it is suggested that medical staff should pay special attention to children who have been hospitalised for a long time and dynamically evaluate changes in their condition. Based on the evaluation results, medical staff can provide targeted information on the identification, treatment, and medical process of related complications during health education. At the same time, it is necessary to use online and offline management platforms to maintain continuous access to medical support and consultation channels.
During the 1-year follow-up period after discharge, 15.51% (85/548) of children who underwent HSCT died. Mortality was 25.18% (35/139) in the unplanned-readmission group and 12.22% (50/409) in the no-readmission group. Kaplan–Meier analysis showed that 1-year overall survival was 73.87% (95% CI = 65.51–80.50%) for the unplanned-readmission group and 86.53% (95% CI = 82.61–89.63%) for the no-readmission group; the difference was statistically significant (log-rank p < 0.001), indicating that unplanned readmission is associated with lower post-transplant survival. This finding is similar to that of another study focusing on the impact of early readmission on the burden on the Canadian healthcare system26. This may be because these children have a variety of complications and physical dysfunction that can lead to life-threatening organ failure27. Therefore, early identification of high-risk groups for unplanned readmission among patients with HSCT is recommended, along with the implementation of targeted interventions, such as the development and expansion of high-quality transitional care services—to improve survival rates.
Study strengths and limitations
The main strength of our study is that it provides a systematic account of 30-day readmission rates and their determinants and compares 1-year overall survival between children who are and are not readmitted within one month of discharge, thereby providing a reference for preventing or reducing the occurrence of unplanned readmission. Nevertheless, this study is constrained by its single-centre, retrospective design and an early follow-up system that may have introduced selection bias and missing data. Restricting the analysis to disease-related factors precluded consideration of psychological status and family caregiving capacity. Moreover, definitions and patterns of unplanned readmission vary internationally and are influenced by local practices, physician judgment, and patient or family preferences. Therefore, prospective, multicentre studies are necessary to determine the incidence and risk factors of unplanned readmission. In future studies, we intend to add some indices, such as psychological and social variables, to explore the causal relationship.
Conclusion
Paediatric patients undergoing HSCT have a higher incidence of unplanned readmissions and mortality, which are influenced by the cytomegalovirus serological status before transplantation, conditioning regimen, infection during hospitalisation, and length of hospitalisation. Medical staff need to pay close attention to the management of unplanned readmission in children undergoing HSCT, especially for positive results for cytomegalovirus before HSCT, myeloablative conditioning regimen, documented infection during HSCT, and an extended length of hospitalisation. Targeted comprehensive intervention strategies should be provided to reduce the risk of unplanned readmission to enhance transplant outcomes and to improve long-term outcomes.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Grønvold, B. L. et al. Allogeneic stem cell transplant recipients surviving at least 2 years without relapse: outcome and risk factors. EJHaem 5, 117–124 (2024).
Kelkar, A. H., Antin, J. H. & Shapiro, R. M. Long-term health outcomes of allogeneic hematopoietic stem cell transplantation. Front. Oncol. 13, 1175794 (2023).
Moerschbacher, A. & He, Z. Building prediction models for 30-day readmissions among ICU patients using both structured and unstructured data in electronic health records. Proc. (IEEE Int. Conf. Bioinf. Biomed). 2023, 4368–4373 (2023).
West, M., Varnes, A. & Hudspeth, M. Standardization of pediatric hematopoietic stem cell transplant patient discharge to reduce readmission rates. J. Pediatr. Hematol. Oncol. Nurs. 40, 432–439 (2023).
Elsabbagh, E. M. & Elkaryoni, A. Thirty-day readmissions in hematopoietic stem cell transplantation recipients: insight from nationwide readmission database. Biol. Blood Marrow Transpl. 25, S220–S221 (2019).
AlKhalaf, H. et al. Identifying the prevalence and causes of 30-day hospital readmission in children: a case study from a tertiary pediatric hospital. Glob J. Qual. Saf. Healthc. 6, 101–110 (2023).
Zhou, X. M. et al. Changes in post-traumatic stress disorder status among children receiving hematopoietic stem cell transplantation: the influencing factors. J. Nurs. Sci. 38, 77–79 (2023). (in Chinese).
Campagna, B. R. et al. Acceleration of mobile health for monitoring post-transplant in the COVID-19 era: applications for pediatric settings. Pediatr. Transpl. 26, e14152 (2022).
Pan, X. R. et al. Establishment and validation of a risk prediction model for oral mucositis in children undergoing hematopoietic stem cell transplantation. Chin. J. Nurs. 58, 587–595 (2023). (in Chinese).
Shaw, A. M. et al. Totally excited about moving mobility and exercise (TEAM me): a successful multidisciplinary exercise quality improvement initiative for pediatric and young adult oncology and stem cell transplant inpatients. Child. (Basel). 9, 186 (2022).
Shulman, D. S., London, W. B., Guo, D., Duncan, C. N. & Lehmann, L. E. Incidence and causes of hospital readmission in pediatric patients after hematopoietic cell transplantation. Biol. Blood Marrow Transpl. 21, 913–919 (2015).
Bezinelli, L. M. et al. Salivary antioxidant enzymes associated with oral toxicity in Haematopoietic cell transplantation: an observational study. Eur. J. Clin. Investig. 51, e13379 (2021).
Gu, J. X. et al. Reliability and validity of the Chinese version of perception of protective isolation scale among patients with hematopoietic stem cell transplantation. Chin. Nurs. Manag. 23, 1806–1811 (2023). (in Chinese).
Chinese Society of Hematology, Chinese Medical Association. The consensus of allogeneic hematopoietic transplantation for hematological diseases in China (2014)——indication, conditioning regimen and donor selection. Zhonghua Xue Ye Xue Za Zhi. 35, 775–780 (2014). (in Chinese).
Wang, Y. et al. General well-being and its influencing factors in peer educators of breast cancer. Chin. J. Nurs. 59, 191–197 (2024). (in Chinese).
Sletvold, T. P., Boland, S., Schipmann, S. & Mahesparan, R. Quality indicators for evaluating the 30-day postoperative outcome in pediatric brain tumor surgery: A 10-year single-center study and systematic review of the literature. J. Neurosurg. Pediatr. 31, 109–123 (2023).
Wu, X. et al. The indirect effects of CMV reactivation on patients following allogeneic hematopoietic stem cell transplantation: an evidence mapping. Ann. Hematol. 103, 917–933 (2024).
Teschner, D., Knop, J., Piehl, C., Junker, S. & Witzke, O. Cytomegalovirus infection and rehospitalization rates after allogeneic hematopoietic stem cell and solid organ transplantation: a retrospective cohort study using German claims data. Infection 50, 1543–1555 (2022).
Stem Cell Application Group, Chinese Society of Hematology, Chinese Medical Association. The Chinese consensus on the management of cytomegalovirus infection in allogeneic hematopoietic stem cell transplantation patients (2022). Zhonghua Xue Ye Xue Za Zhi. 43, 617–623 (2022). (in Chinese).
Spring, L. et al. Risk factors for readmission after allogeneic hematopoietic stem cell transplantation and impact on overall survival. Biol. Blood Marrow Transpl. 21, 509–516 (2015).
Zanetti, M. O. B. et al. Impact of the insertion of the clinical pharmacist in the allogeneic hematopoietic stem cells transplantation team. J. Oncol. Pharm. Pract. 29, 375–385 (2023).
Lehrnbecher, T. et al. 8th European Conference on Infections in Leukaemia: 2020 Guidelines for the use of antibiotics in paediatric patients with cancer or post-haematopoietic cell transplantation. Lancet Oncol. 22, e270-e280 (2021).
Yamaguchi, K. et al. Characterization of readmission after allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 56, 1335–1340 (2021).
Garcia, M. E. L. et al. Risk factors associated with readmission following allogeneic hematopoietic cell transplantation (AlloHCT) among children. Transpl. Cell. Ther. 30, S349–S349 (2024).
Michonneau, D. et al. Clinical and economic burden associated with graft-versus-host disease following allogeneic hematopoietic cell transplantation in France. Bone Marrow Transpl. 58, 514–525 (2023).
Famure, O. et al. Outcomes of early hospital readmission after kidney transplantation: perspectives from a Canadian transplant centre. World J. Transpl. 13, 357–367 (2023).
Zinter, M. S. et al. Intensive care risk and long-term outcomes in pediatric allogeneic hematopoietic cell transplant recipients. Blood Adv. 8, 1002–1017 (2024).
Acknowledgements
We appreciate the cooperation of Children’s Hospital of Chongqing Medical University in granting us access to the medical records used in this study. Their support facilitated the smooth progress of our research. Moreover, especially we would like to thank Editage (www.editage.com) for English language editing.
Funding
Funding was provided by Children’s Hospital of Chongqing Medical University (grant number: CHCQMU2023.19) and Chongqing Municipal Natural Science Foundation General Project (grant number: CSTB2022NSCQ-MSX0082).
Author information
Authors and Affiliations
Contributions
X.R.P.and X.L.G. participated in the conceptualization, methodology, writing, and editing.M.L. participated in the invaluable counsel on the intricacies of the study design and the nuanced interpretation of the results. S.Q.Z, J.Y. and X.H.R. participated in the supervision, revision, and project administration. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pan, X., Guo, X., Mo, L. et al. Factors influencing unplanned readmissions after paediatric haematopoietic stem cell transplantation and effect on overall survival. Sci Rep 15, 35727 (2025). https://doi.org/10.1038/s41598-025-19447-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-19447-z