Abstract
The demand for remote assessment tools has increased, yet there is a lack of standardized adaptations for remote administration. This pilot study investigates the equivalency of in-person and remote cognitive assessments using the NIH Toolbox Cognition Battery (NIHTB-CB) among children aged 7 to 17 years. Forty-seven children (51.1% female; Mage = 12.26, SDage= 3.23) were assessed in two formats: in-person at a study site and remotely from home, with the order of assessments counterbalanced. The NIHTB-CB was used for in-person evaluations, while a newly developed version, the NIH Toolbox Participant/Examiner (NIHTB-P/E) App, was used for remote assessments through built-in teleconferencing features. The results showed considerable consistency between in-person and remote scores across all NIHTB-CB tests. Certain differences were noted, including longer test durations for remote assessments and potential practice effects on some measures. Overall, preliminary findings from this pilot study support thefeasibility of administering the NIHTB-CB remotely using the NIHTB-P/E App, providing a viable option to traditional in-person cognitive assessments in pediatric populations.
Similar content being viewed by others
Introduction
Cognitive assessment is vital to evaluating cognitive functioning1. It is particularly critical during childhood due to its essential role in tracking healthy development, identifying any developmental delays, making accurate and timely diagnoses, and evaluating the effectiveness of treatments and interventions2,3,4,5,6. In that respect, cognitive assessments have significant implications for children, ranging from treatment decisions to eligibility for access to resources3. Additionally, cognitive abilities have been consistently associated with real-world outcomes, such as social functioning7 and physical and mental health8as well as educational outcomes including school readiness, early academic skills, language comprehension, reading, vocabulary acquisition, and mathematics9,10,11. Cognitive assessments are also used in research studies to compare outcomes between intervention groups. Therefore, it is crucial to have reliable, valid, and age-appropriate standardized measures to evaluate children’s cognitive functioning, as these tools ensure the quality and accuracy of the assessment process.
Traditional methods of cognitive assessment in pediatric populations often involve direct interaction between an examiner and a participant, typically conducted in a clinical, research, or educational setting using standardized paper-and-pencil or computerized tests12,13,14. The COVID-19 pandemic, however, interrupted these traditional in-person approaches due to social distancing requirements and restrictions on face-to-face interaction15,16,17 and led researchers to explore alternative assessment strategies. Remote assessment, in which the participant and examiner are in separate locations, has proven to offer several benefits to both researchers and participants. Benefits for researchers include increased efficiency of data collection, increased sample size and diversity, higher generalizability and ecological validity, and cost-effectiveness18,19. Benefits for participants include eliminating barriers to participation, such as travel costs and long travel hours, which is particularly helpful for participants residing in remote or hard-to-reach areas20,21. Remote testing can reduce attrition in longitudinal studies by increasing the likelihood of participation at multiple time points21. Remote assessment can even aid the recruitment of participants living with limited mobility (e.g., physical disabilities) who are underserved when in-person assessment strategies are applied22.
Despite numerous benefits, remote assessment is not without its limitations. First, it can be challenging to achieve the same level of standardization remotely as in traditional lab settings23,24 because researchers have less control over the testing environment (e.g., distraction). Second, depending on the level of monitoring, participants may engage in dishonest practices, such as taking notes, capturing screenshots, or seeking assistance from third parties. Third, if the remote assessments are administered on participants’ own devices, the assessment can be interrupted by phone calls, notifications, or text messages. Fourth, additional challenges to data safety and transfer exist, especially when Personally Identifiable Information (PII) is involved25,26.
The COVID-19 pandemic has also increased interest in the feasibility of remote cognitive assessment in pediatric populations27,28. A majority of the feasibility studies focused on the psychometric equivalency between remote and in-person cognitive assessments by using either intelligence scales such as the Wechsler Intelligence Scale for Children, Fifth Edition29 or other cognitive tests27,28,30,31. Additionally, some recent studies investigated remote cognitive assessment in special populations. In children with specific learning disabilities, for example, remote and in-person assessments of learning skills revealed similar results32. Likewise, remote administration of processing speed measures was feasible in children with chronic medical conditions33indicating its potential for broader use in clinical practice.
In the current pilot study, we investigate the equivalency of in-person and remote cognitive assessments in healthy children by examining a newly developed application - the NIH Toolbox Participant/Examiner (NIHTB-P/E) App, which leverages the NIH Toolbox for Assessment of Neurological and Behavioral Function Cognition Battery (NIHTB-CB; www.nihtoolbox.org). The NIHTB-CB is a well-established iPad-based measurement system currently deployed in over 1,100 institutions across the world34,35,36,37,38. It is used in several large-scale longitudinal studies such as Environmental influences on Child Health Outcomes (ECHO)39 and HEALthy Brain and Child Development (HBCD)40 is further used in clinical samples, including children with congenital heart defects (CHD)41 and those with Pompe disease (PD)42. Therefore, providing the remote option of the NIHTB-CB is an important contribution to the field by expanding accessibility, reducing barriers to participation, and enabling more frequent and flexible monitoring of cognitive development in pediatric populations.
Tests within the NIH Toolbox Cognition Battery (NIHTB-CB) span a diverse array of cognitive domains, including working memory, processing speed, language, attention, executive functioning, and episodic memory (see Table 1 for constructs, their definitions, corresponding tests, age ranges, and test durations), These tests have been proven useful for predicting cognitive performance across diverse childhood samples43,44,45,46. The NIHTB-CB measures were designed to be interactive, engaging, and developmentally appropriate and have previously been shown to be reliable and valid compared to similar gold-standard assessments in this age range45,47. NIHTB-CB measures have typically been administered in-person; however, they can now be administered remotely via the newly developed NIHTB-P/E app. This app is an iPad-to-iPad assessment system allowing for testing when the examiner and participant are in different locations. Critically, it includes a built-in bi-directional video-conferencing feature (see Figs. 1 and 2) that allows the administration to be experimenter-guided and fully monitored. This supervised remote cognitive assessment is similar to in-person testing due to the real-time interactions between the examiner and the participant through videoconferencing48.
In this pilot study, we tested the equivalency of in-person cognitive assessment by using the NIHTB-CB and remote cognitive assessment via the NIHTB-P/E app. Children ages 7–17 completed the NIHTB-CB tests on an iPad, guided and monitored by a trained examiner using the NIHTB-P/E app. With the support of the bi-directional communication system, we expected no significant differences in test scores between remote cognitive assessment at home by using the NIHTB-P/E app and in-person assessment at the study site utilizing the NIHTB-CB.
Method
Participants
Child-caregiver dyads were recruited across six study sites throughout the United States (i.e., Orlando, FL; Houston, TX; Nashville, TN; Atlanta, GA; Baltimore, MD; and Dallas, TX) as part of a larger study49 with specific age, gender, race/education, and mother education targets to ensure demographic diversity (e.g., maximum 60% of each sex, at least 20% of mothers/caregivers with less than a college degree). Participants were screened by a market panel research company based on predetermined inclusion and exclusion criteria. Specifically, the inclusion criteria were: children aged 7–17 years, fluency in English, self-reported adequate internet access, and caregiver willingness to assist with the remote setup. Exclusion criteria, on the other hand, included a current positive COVID-19 test in the child, limited English proficiency in either the caregiver or the child, or a lack of access to an iPad-compatible internet connection. Children with physical impairments that would interfere with the ability to interact with the iPad (e.g., limited upper limb mobility preventing touchscreen use) were not included in this pilot study. A total of 58 child participants between 7 and 17 years old were recruited (48.3% female; Mage = 11.88, SDage = 3.31). Of these participants, 47 (51.1% female; Mage = 12.26, SDage = 3.23) completed both the in-person and remote cognitive batteries a few days apart (M = 3.15; SD = 3.06). While a small number of participants did not complete both sessions, there was no evidence of differential dropout by age group, sex, or mode of test administration. Demographic characteristics of the final sample are displayed in Table 2. Caregivers signed informed consent forms and received $225 for participating in both remote and in-person assessments. Their travel expenses were reimbursed for in-person site visits. The study protocol was approved by the WIRB-Copernicus Group (WCG) Institutional Review Board (IRB Approval #20231258). In addition, the study was conducted in accordance with the Declaration of Helsinki and applicable institutional/national ethical guidelines. Finally, written informed consent was obtained from all participants or their legally authorized representatives prior to study enrollment.
Measures
The NIH toolbox cognition battery (NIHTB-CB)
The NIH Toolbox for Assessment of Neurological and Behavioral Function (NIHTB; www.nihtoolbox.org) is a comprehensive set of computerized measures with four batteries: cognition, emotion, motor, and sensation37,50. NIHTB is designed for use across the lifespan (i.e., ages 3 to 85) and has been reported to be a valid and reliable tool in different age groups and populations ranging from healthy adults to patients with neurological disorders50,51,52. The NIHTB-CB is designed to measure a broad range of cognitive abilities, including attention, episodic memory, language (i.e., oral reading and vocabulary), working memory, executive function, and processing speed. All tests in the NIHTB-CB are psychometrically validated and normed50. Each cognitive test in the battery is further described individually below.
The NIH toolbox participant/examiner app (NIHTB-P/E)
NIH Toolbox Participant/Examiner App (NIHTB-P/E) is a newly developed iPad-to-iPad assessment system that allows for remote cognitive testing when the examiner and participant are in different locations. The NIHTB-P/E app leverages the NIHTB described above. The NIHTB-P/E app was designed for monitored, experimenter-guided assessment and, as such, includes a built-in bi-directional video-conferencing feature. The examiner can observe the participant completing the assessment at all times and has full control over the assessment, including pausing the assessment, terminating the assessment, and moving to a new measure. In turn, the participant is able to complete all measures directly on the iPad in front of them and, if necessary, can communicate with the examiner. Figures 1 and 2 show screenshots of the NIHTB-P/E app, captured during a sample testing session for the Dimensional Change Card Sort Test and the Flanker Inhibitory Control and Attention Test, respectively.
The NIHTB-P/E was designed to be adaptable to various iPad models, and as such, testing stimuli are fixed to the stimuli size of the NIHTB-CB, regardless of iPad screen size of either the examiner or participant. Additionally, scores are recorded and calculated locally on the participant’s device after each item (e.g., in a computer adaptive paradigm), maximizing data capture. The NIHTB-CB and NIHTB-P/E app offer parallel versions of standardized normed measures, with the only difference being the remote functionality of the latter system.
Cognitive tests in the NIHTB-CB and the NIHTB-P/E app
NIH Toolbox Dimensional Change Card Sort Test (DCCS). NIH Toolbox Dimensional Change Card Sort Test53 measures cognitive flexibility, which is the ability to adaptively shift between sorting rules for identical stimuli. The original version of DCCS was developed by Zelazo and colleagues54 for the first version of the NIHTB-CB. This test is a measure of fluid ability, which is the capacity to acquire new knowledge and to adapt to unfamiliar circumstances. In DCCS, participants are shown two images side by side at the bottom of the screen. In each trial, participants see a cue word - either “shape” or “color” - at the center of the screen, followed by a bivalent target image, which participants sort based on the cued dimension. The sorting rule alternates between “color” and “shape” in a pre-determined order that appears to be pseudo-random. Participants respond by tapping one of the two visual images based on the dimension specified by the presented cue word (see Fig. 1). Scoring is based on both accuracy and reaction time.
NIH Toolbox Flanker Inhibitory Control and Attention Test (Flanker). The NIH Toolbox Flanker Inhibitory Control and Attention Test (Flanker) is a version of the Eriksen Flanker Task55 designed to measure attention and inhibitory control36,53. Like the DCCS test, Flanker is also considered a measure of fluid ability. In this test, each trial starts with a fixation star in the center of the screen, followed by a blank screen. Next, a row of five stimuli (fish or arrows) appears, pointing left or right (see Fig. 2). Participants are instructed to tap one of two buttons on the bottom of the screen that matches the target stimulus’s direction (the middle fish or arrow). Scoring is based on both accuracy and reaction time.
NIH Toolbox List Sorting Working Memory Test (LSWM). The NIH Toolbox List Sorting Working Memory Test (LSWM) is a sequencing task developed to measure working memory56. In this test, which is a measure of fluid ability, participants engage in immediate recall and sequencing of different stimuli presented visually and orally. A set of pictures of different animals and foods are presented with an accompanying audio recording and written text (e.g., dog, apple). The participants are then asked to say the items back in size order (smallest to largest) in two formats, first within a single dimension (either animals or foods, called 1-List) and then in two dimensions (foods, then animals, called 2-List). Scoring is based on the total number of items correct.
NIH Toolbox Pattern Comparison Processing Speed Test (PCPS). The NIH Toolbox Pattern Comparison Processing Speed Test (PCPS) is a measure of fluid ability and developed to assess the speed of processing. It measures how accurately participants can decide whether two side-by-side pictures are the same51. When the presented patterns are not identical, they vary on one of three dimensions (i.e., color, quantity, and presence/absence of an image or image component). Participants respond to whether or not the patterns are identical by pressing a “yes” or “no” button. Scoring is based on the total number of items correct.
NIH Toolbox Picture Sequence Memory Test (PSM). The NIH Toolbox Picture Sequence Memory Test (PSM) measures episodic memory by asking participants to recall the order of thematically related pictures of objects and activities57,58. It is also considered as a measure of fluid ability. At the beginning of each trial, a fixed spatial order of pictures is displayed in the center of the screen, with an auditory description of an activity that can be described with all the pictures. Immediately following the presentation of a sequence of pictures, the participants are instructed to re-order the stimuli from memory. Participants are asked to recall each sequence twice. The number of presented pictures in a sequence varies between 6 and 18 depending on the age of the participant. Participants are given credit for each adjacent pair of pictures they correctly place (i.e., if pictures in locations 7 and 8 are placed in that order and adjacent to each other anywhere, such as slots 1 and 2, one point is awarded), up to the maximum value for the sequence, which is one less than the sequence length. Scoring is based on an IRT-based score where the number of correct adjacent pairs is transformed into a latent (theta) score, which is then scaled to a normed score.
NIH Toolbox Oral Reading Recognition Test (OR). The NIH Toolbox Oral Reading Recognition Test (OR) employs a Computer Adaptive Testing59,60 methodology, requiring active administrator involvement for scoring60,61. It measures crystallized abilities, which develop with age and education and increase during childhood before becoming stable in adulthood. The examiner first identifies the educational level of the participant in order to set the appropriate starting point. Respondents are then provided with a word on the screen. The difficulty level of the words is set according to the participant’s age and adaptively increases or decreases in difficulty based on the participant’s performance. Participants are asked to pronounce each word to the best of their ability. Examiners are trained with audio recordings for the word list and a printed pronunciation guide before administering the test. The trained examiner scores the participants’ responses as either “correct” or “incorrect” based on pronunciation accuracy. Pronunciations that did not match the respelling pronunciation guide were evaluated as incorrect. Scoring is based on a combination of correct responses and the difficulty of each item, and a latent (theta) score is produced that is then scaled to normed scores.
NIH Toolbox Picture Vocabulary Test (PVT). The NIH Toolbox Picture Vocabulary Test (PVT) assesses general vocabulary knowledge60 using CAT. This test is a measure of crystallized abilities. The examiner first identifies the educational level of the participant in order to set the appropriate starting point. During the test, the participant is presented with four photographic images on the screen and an audio recording that matches one of the four images. Participants are provided as much time as they need to respond and are asked to select the picture that matches most closely based on the recording. The difficulty level of the words is set according to the participant’s age and adaptively increases or decreases in difficulty based on the participant’s performance. Scoring is based on a combination of correct responses and the difficulty of each item, and a latent (theta) score is produced that is then scaled to normed scores.
Procedure
Prior to data collection, examiners were trained and certified to administer both the in-person and remote versions of the NIHTB-CB. The order of remote and in-person cognitive assessment sessions was counterbalanced, with half of the participants (randomly selected) first completing the assessments remotely and the other half completing them in person.
For the remote assessments participants were shipped a study kit that included a study iPad pre-loaded with the NIHTB-P/E app, an iPad charger, printed instructions for setup and use, and paper copies of data collection forms to be completed during the remote session. Caregivers were provided with step-by-step instructions on how to enter a meeting code on the NIHTB-P/E app that would connect them to the examiner. Once connected with the examiner on the app, caregivers followed the examiner’s live instructions through the app’s communication system to assist with the final setup process (e.g., adjusting the volume on the iPad).
The setup process on the participant’s end typically took less than five minutes, not including the time to charge the iPad, which families were instructed to do in advance. Once the set-up process was complete, caregivers were instructed not to assist their child with any tests. However, they were allowed to help with technical difficulties, such as connection issues or iPad malfunctions. The examiner could note any deviations from the administration, though there were none recorded regarding the administration of the current reported study. Caregivers were also given the examiner’s contact information in case the examiner was disconnected during the test and needed to rejoin the app. After completing the assessments, participants could return the iPad either in person at the study site or by using a prepaid return shipping label provided in the kit.
Statistical analyses
Individual and composite test scores
Individual test scores were obtained from each of the seven tests in the NIHTB-CB. Composite scores were derived from a specific combination of individual test scores, resulting in three categories: fluid composite (FC), crystallized composite (CC), and total composite (TC) test scores34,62. Specifically, the FC test score includes Flanker, Dimensional Change Card Sort, Picture Sequence Memory, List Sorting, and Pattern Comparison Tests while the CC test score includes the Picture Vocabulary and Reading Tests. These composite scores were calculated by averaging the standard scores of the individual tests. Finally, the TC test score is the average of the FC and CC test scores. These composites were empirically derived in prior validation studies of the NIH Toolbox Cognitive Battery and have been used in previous research involving children and adolescents63.
Age-corrected standard scores and uncorrected standard scores
For each test, we used two types of test scores: age-corrected standard scores and uncorrected standard scores. Age-corrected standard scores compare each participant’s score to those in the original NIHTB norming study of nationally representative individuals of the same age36. A score of 100 indicated performance at the national average for the participant’s age with an SD of 15. Uncorrected standard scores also use a standard score metric (normative mean = 100 and SD = 15), comparing the performance of the test-taker to those in the entire NIHTB normative sample, regardless of age or any other variable. In the present study, all analyses involving test scores were conducted separately for age-corrected and uncorrected standard scores for comparison purposes. Results based on uncorrected standard scores are presented in Table S1 and Table S2 in the supplementary materials.
Finally, analyses involving participants’ age used two age bands: 7- to 12-years and 13- to 17-years, consistent with previous research using the NIHTB-CB in child samples36,45,64. We also conducted the analyses by including age as a continuous covariate and obtained consistent results, indicating that our findings are robust regardless of how age is included in the analyses.
Group comparisons
Differences between remote and in-person cognitive assessment scores were compared by conducting a series of Repeated Measures ANOVAs. The mode of administration (remote vs. in-person) was the within-subjects while age group (7-to-12 vs. 13-to-17 years old) and administration order (remote first vs. in-person first) were between-subjects factors. Another series of Repeated Measures ANOVAs examined the within-subjects effect of mode of administration (remote vs. in-person) controlling for age group (7-to-12 vs. 13-to-17 years old) and administration order (remote first vs. in-person first), which were the between-subjects factors on test time in minutes. Bonferroni corrections65 were applied to adjust for multiple comparisons, with an alpha level of 0.017 for analyses involving the three composite test scores and 0.007 for analyses involving the seven individual test scores.
Analysis of overlap
To assess the similarity between the empirical distributions of each measure and composite when compared by administration mode (e.g., the percentage overlap in distribution between remote and in-person Pattern Comparison Processing Speed Test), we calculated the overlap between their respective kernel density estimates66. This analysis has been used in many contexts in many fields67,68is efficient to calculate, makes no assumptions of normality, and is straightforward to interpret. This analysis was done using the ‘overlapping’ package in R 4.2.269,70.
Results
Mode of administration by age group and administration order
Analyses on participants’ individual test scores revealed no significant differences between remote and in-person cognitive assessments (see Table 4). Age group and administration order had no significant effects on performance for individual test scores (see Table 4). However, there was a significant interaction between the mode of administration and the first mode for two of the individual tests: Pattern Comparison Processing Speed Test and Picture Sequence Memory. To be more specific, test scores for remote cognitive assessments were lowest for these two tests when the remote assessment was administered first, whereas they were highest when the in-person cognitive assessment was administered first (see Table 3). As seen in Table 4, no other significant interaction between the mode of administration and the first mode was observed for the remaining individual test scores. Finally, the three-way interaction between mode of administration, age group, and first mode was not significant for individual test scores (see Table 4). Results of the separate analyses for composite test scores are provided in the Supplementary Materials. Specifically, Table S1 presents the means and standard deviations of age-corrected composites test scores by mode of administration, age and first mode and Table S2 presents mean square error (MSE), F and p values together with the effect sizes of the Repeated Measures ANOVAs. As seen in Table S2, results for composite scores generally followed the same pattern observed in individual test scores with significant Mode*First Mode interactions for both the fluid and total composites, suggesting higher remote scores when remote testing was the second administration (see Supplementary Table S1).
Test duration by mode of administration, age group, and administration order
Results indicated a significant main effect of mode of administration on test duration for Dimensional Change Card Sort Test, List Sorting Working Memory, and Picture Sequence Memory tests: Participants took longer to complete these tests in remote administration compared to in-person administration (see Tables 5 and 6). Mode of administration had no effect on the remaining tests of Flanker, Pattern Comparison Processing Speed Test, Oral Reading Recognition, and Picture Vocabulary (see Table 6). Age group had a main effect on test duration for the Pattern Comparison Processing Speed Test, with younger participants completing the test faster than their older counterparts (see Tables 5 and 6). The interaction between the mode of administration and administration order was significant for Pattern Comparison Processing Speed Test and Picture Vocabulary tests (see Table 6). For the Pattern Comparison Processing Speed Test, children completed the test faster in the first administration. More specifically, in-person testing had shorter duration than remote testing when it was conducted first while remote assessment was shorter than in-person one when it was administered first. For the Picture Vocabulary test, duration was the longest when the cognitive assessment was completed remotely as the first measurement. However, remote Picture Vocabulary testing displayed the shortest duration when the first administration mode was in-person. No other significant effects or interactions were observed (see Table 6).
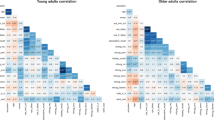
Analysis of overlap
The percentage overlap between remote and in-person distributions of each NIHTB-CB test ranged between 96.61% and 84.21%, indicating the highest overlap for the Flanker test and the lowest for the List Sorting Working Memory test. The mean percentage overlap for all seven tests was 90.72%. The percentage overlap for the fluid, crystallized, and total composite scores was 89.5%, 94.27%, and 95%, respectively. Density plots with the percentage overlap between in-person and remote assessments are presented in Fig. 3 for composite test scores. For individual test scores, density with the percentage overlap between in-person and remote assessments are displayed in Figure S1 in the supplementary materials.
Discussion
Results of this pilot study show equivalency between in-person and remote test scores, indicating that the NIHTB-P/E app is a feasible option for remote cognitive assessment in children aged 7–17. Introducing standardized remote cognitive assessment methods is critical, as remote assessment has endured in the post-pandemic era71,72 and offers a range of potential benefits, including increased diversity and representativeness of research subjects. Increasing sample diversity is essential for research with children as developmental processes can vary depending on geographical location, ethnicity, and socioeconomic status73,74,75. Through remote assessment, children who would otherwise be excluded from studies, such as those living in rural areas, face lower barriers to participation, all of which can help improve the ecological validity of research studies. In addition to these benefits, remote tools like the NIHTB-P/E app can enhance the feasibility of decentralized clinical trials (DCTs)76,77 by reducing reliance on in-person site visits. Thus, the remote administration of the NIHTB-CB will support future studies including the decentralized ones.
The lack of significant differences between in-person and remote scores held across age groups (7–12 and 13–17 years old) and, for the most part, regardless of the order in which the testing modes were administered. Indeed, for five out of the seven tests, no significant differences were observed in scores across the two formats. However, the interaction between the mode of administration and the order of remote versus in-person assessments revealed practice effects for two individual tests: the Pattern Comparison Processing Speed and Picture Sequence Memory tests. More specifically, taking these tests in-person first led to higher scores on the second (remote) session. Interestingly, when the remote assessment was administered first, we did not see an increase in performance in the second (in-person) session. It is important to note that practice effects on these tests may not be specific to this context since previous studies have also reported practice effects for both Pattern Comparison Processing Speed51 and Picture Sequence Memory58. These effects may be related to familiarity with stimuli and may have more to do with the relatively short time between the remote and in-person administrations in the current study. Overall, current findings indicate that the NIHTB-P/E app, in general, offers a way to reliably assess cognitive abilities in decentralized protocols. It is important to note that this analysis was focused on group-level equivalency between in-person and remote testing, often used in cross-sectional research designs, for example, rather than individual-level measurement agreement. As such, while preliminary findings of our pilot study support the comparability of in-person and remote testing at the group level, future research is needed to investigate whether individuals obtain consistent scores across administrations.
Additionally, we found that test duration was impacted by the mode of administration, with participants taking significantly longer to complete specific tests (i.e., Dimensional Change Card Sort, List Sorting Working Memory, and Picture Sequence Memory) remotely compared to in-person. Age differences affected only the Pattern Comparison Processing Speed test, which was completed faster by younger participants than older ones. The Picture Vocabulary test had the longest duration when administered remotely first and shortest when remote testing followed in-person administration. The Pattern Comparison Processing Speed test, on the other hand, had a shorter duration in the first administration than the second, independent of the mode of administration. These differences, however, had very small effect sizes. Overall, these findings suggest that both administration mode and order have nuanced effects on test duration for the Pattern Comparison Processing Speed and Picture Vocabulary tests, highlighting the importance of considering these factors when interpreting remote versus in-person testing results.
One limitation of the NIHTB-P/E app is that it requires sufficient internet bandwidth and the availability of required technological devices: in this case, an iPad. While these limitations may be an issue by introducing selection bias, systematically excluding individuals lacking access to internet services, technological devices, and technological literacy78,79we note that there are many solutions to overcome these challenges. For instance, researchers can send participants iPads with built-in internet service or connect users to locations with adequate internet access, such as libraries. Certainly, our study addressed this limitation by screening participants for internet access and providing iPads for home use. However, these requirements may present significant challenges for larger, multi-site, or national studies involving hundreds or thousands of participants.
Another limitation to note is that although our study demonstrated equivalency between the remotely applied NIHTB-P/E app and the in-person NIHTB-CB, the norm-referenced scores available for the NIHTB are based on data from in-person testing. This creates future opportunities to harmonize assessments across both modes of administration. Finally, the moderate sample size, consistent with the pilot nature of the study, limits the generalizability of the current findings and requires further research with larger samples. While the study provides important preliminary evidence supporting remote administration of the NIHTB-CB, the findings should be interpreted with caution. Larger studies are needed to confirm these results and explore variability across different subgroups and settings.
In conclusion, the NIHTB-P/E app provides a feasible and standardized method for remote administration of the NIHTB-CB to children in varied environments. Although this pilot study had a small sample size that may limit statistical power to detect subtle differences, the findingssuggest that scores obtained remotely are generally comparable to those from traditional in-person methods These preliminary results support the potential utility of the app for remote cognitive assessment with minimal impacts on test duration or performance. This pilot study supports the NIHTB-P/E app’s potential to expand the scope of cognitive assessment research, reducing participant burden.
Data availability
The data that support the findings of this study are available from the corresponding author (BE) upon reasonable request.
References
Lezak, M. D., Howieson, D. B., Bigler, E. D. & Tranel, D. Neuropsychological Assessment (Oxford University Press, 2012).
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. (American Psychiatric Association. https://doi.org/10.1176/appi.books.9780890425596 (2013).
Ellingsen, K. M. Standardized assessment of cognitive development: instruments and issues. In Early Childhood Assessment in School and Clinical Child Psychology (ed. Garro, A.) 25–49 (Springer New York, 2016). https://doi.org/10.1007/978-1-4939-6349-2_2.
Farmer, C., Golden, C. & Thurm, A. Concurrent validity of the differential ability scales, second edition with the Mullen scales of early learning in young children with and without neurodevelopmental disorders. Child. Neuropsychol. 22, 556–569 (2016).
Riccio, C. A., Sun, L. H. & Gonzalez, A. Understanding typical and atypical neurodevelopment in children and adults. In Understanding the Biological Basis of Behavior (eds D’Amato, R. C. et al.) 71–106 (Springer International Publishing, 2021). https://doi.org/10.1007/978-3-030-59162-5_4.
Sternberg, R. J. & Kaufman, S. B. The Nature of Human Intelligence (Cambridge University Press, 2018).
Racz, S. J., Putnick, D. L., Suwalsky, J. T. D., Hendricks, C. & Bornstein, M. H. Cognitive abilities, social adaptation, and externalizing behavior problems in childhood and adolescence: specific cascade effects across development. J. Youth Adolesc. 46, 1688–1701 (2017).
Der, G., Batty, G. D. & Deary, I. J. The association between IQ in adolescence and a range of health outcomes at 40 in the 1979 US National longitudinal study of youth. Intelligence 37, 573–580 (2009).
Blair, C. & Razza, R. P. Relating effortful control, executive function, and false belief Understanding to emerging math and literacy ability in kindergarten. Child. Dev. 78, 647–663 (2007).
Espy, K. A. et al. The contribution of executive functions to emergent mathematic skills in preschool children. Dev. Neuropsychol. 26, 465–486 (2004).
Ursache, A., Blair, C. & Raver, C. C. The promotion of Self-Regulation as a means of enhancing school readiness and early achievement in children at risk for school failure. Child. Dev. Perspect. 6, 122–128 (2012).
Kaufman, A. S. & Kaufman, N. L. Kaufman Assessment Battery for Children (American Guidance Service, 2015).
Reynolds, C. R. & Fletcher-Janzen, E. (eds) Handbook of Clinical Child Neuropsychology (Springer, 2019).
Sattler, J. M. & Hoge, R. D. Assessment of Children: Cognitive Applications (Sattler, Publisher, Inc., 2006). Jerome M.
Farmer, R. L. et al. Teleassessment with children and adolescents during the coronavirus (COVID-19) pandemic and beyond: practice and policy implications. Prof. Psychol. Res. Pract. 51, 477–487 (2020).
Omary, M. B. et al. The COVID-19 pandemic and research shutdown: staying safe and productive. J. Clin. Invest. 130, 2745–2748 (2020).
Sheskin, M. et al. Online developmental science to foster innovation, access, and impact. Trends Cogn. Sci. 24, 675–678 (2020).
Gold, M. et al. Digital technologies as biomarkers, clinical outcomes assessment, and recruitment tools in alzheimer’s disease clinical trials. Alzheimers Dement. Transl Res. Clin. Interv. 4, 234–242 (2018).
Rhodes, M. et al. Advancing developmental science via unmoderated remote research with children. J. Cogn. Dev. 21, 477–493 (2020).
Hensen, B. et al. Remote data collection for public health research in a COVID-19 era: ethical implications, challenges and opportunities. Health Policy Plan. 36, 360–368 (2021).
Hodge, M. A. et al. Literacy assessment via telepractice is comparable to Face-to-Face assessment in children with reading difficulties living in rural Australia. Telemed E-Health. 25, 279–287 (2019).
Graham, F., Boland, P., Grainger, R. & Wallace, S. Telehealth delivery of remote assessment of wheelchair and seating needs for adults and children: a scoping review. Disabil. Rehabil. 42, 3538–3548 (2020).
Germine, L., Reinecke, K. & Chaytor, N. S. Digital neuropsychology: challenges and opportunities at the intersection of science and software. Clin. Neuropsychol. 33, 271–286 (2019).
Koo, B. M. & Vizer, L. M. Examining mobile technologies to support older adults with dementia through the lens of personhood and human needs: scoping review. JMIR MHealth UHealth. 7, e15122 (2019).
Kaissis, G. A., Makowski, M. R., Rückert, D. & Braren, R. F. Secure, privacy-preserving and federated machine learning in medical imaging. Nat. Mach. Intell. 2, 305–311 (2020).
Mayer, A. H., Costa, D., Righi, R. & C. A. & D. R. Electronic health records in a blockchain: A systematic review. Health Inf. J. 26, 1273–1288 (2020).
Harder, L. et al. Home-Based pediatric teleneuropsychology: A validation study. Arch. Clin. Neuropsychol. 35, 1266–1275 (2020).
Wright, A. J. Equivalence of remote, digital administration and traditional, in-person administration of the Wechsler intelligence scale for children, fifth edition (WISC-V). Psychol. Assess. 32, 809–817 (2020).
Wechsler, D. Wechsler Intelligence Scale for Children (Pearson, 2014).
Hamner, T., Salorio, C. F., Kalb, L. & Jacobson, L. A. Equivalency of In-Person versus remote assessment: WISC-V and KTEA-3 performance in clinically referred children and adolescents. J. Int. Neuropsychol. Soc. 28, 835–844 (2022).
Hodge, M. A. et al. Agreement between telehealth and face-to-face assessment of intellectual ability in children with specific learning disorder. J. Telemed Telecare. 25, 431–437 (2019).
Lampis, V. et al. Comparing remote versus in-person assessment of learning skills in children with specific learning disabilities. Digit. Health. 10, 20552076241254453 (2024).
Peterson, R. K. & Ng, R. The feasibility of remote administration of oral processing speed measures in children with chronic medical conditions. Clin. Neuropsychol. 1–13. https://doi.org/10.1080/13854046.2025.2469337 (2025).
Akshoomoff, N. et al. VIII. NIH TOOLBOX COGNITION BATTERY (CB): COMPOSITE SCORES OF CRYSTALLIZED, FLUID, AND OVERALL COGNITION. Monogr. Soc. Res. Child. Dev. 78, 119–132 (2013).
Casaletto, K. B. et al. Demographically corrected normative standards for the english version of the NIH toolbox cognition battery. J. Int. Neuropsychol. Soc. 21, 378–391 (2015).
Casaletto, K. B. et al. Demographically corrected normative standards for the Spanish Language version of the NIH toolbox cognition battery. J. Int. Neuropsychol. Soc. 22, 364–374 (2016).
Gershon, R. C. et al. NIH Toolbox for Assessment of Neurological and Behavioral Function. Neurology 80, (2013).
Gershon, R. C. et al. The NIH toolbox: overview of development for use with Hispanic populations. J. Int. Neuropsychol. Soc. 26, 567–575 (2020).
Price, J. C., Lee, J. J., Saraiya, N., Lei, S. & Mintz, C. D. An update on NIH programs relevant to child brain health research: ECHO, ABCD, HBCD, and MIRA. J. Neurosurg. Anesthesiol. 35, 119–123 (2023).
Deoni, S. C. L. et al. Remote and at-home data collection: considerations for the NIH healthy brain and cognitive development (HBCD) study. Dev. Cogn. Neurosci. 54, 101059 (2022).
Wallace, J. et al. Psychometric properties of the NIH toolbox cognition and emotion batteries among children and adolescents with congenital heart defects. Child Neuropsychol. 30, 967–986 (2024).
Spiridigliozzi, G. A. et al. Exploring the use of the National institutes of health toolbox cognition battery with children and adolescents with Pompe disease: preliminary findings. Mol. Genet. Metab. 144, 109043 (2025).
Anokhin, A. P. et al. Age-related changes and longitudinal stability of individual differences in ABCD neurocognition measures. Dev. Cogn. Neurosci. 54, 101078 (2022).
Chadwick, L. et al. Cognitive outcomes in children with mild traumatic brain injury: an examination using the National institutes of health toolbox cognition battery. J. Neurotrauma. 38, 2590–2599 (2021).
Kabundula, P. P. et al. Validation of the National Institute of health toolbox cognition battery (NIHTB-CB) in children and adolescents with and without HIV infection in lusaka, Zambia. AIDS Behav. 26, 3436–3449 (2022).
Karcher, N. R. et al. Replication of associations with Psychotic-Like experiences in middle childhood from the adolescent brain cognitive development (ABCD) study. Schizophr Bull. Open. 1, sgaa009 (2020).
Shields, R. H. et al. Validation of the NIH toolbox cognitive battery in intellectual disability. Neurology 94, e1229–e1240 (2020).
Chuey, A. et al. Moderated online Data-Collection for developmental research: methods and replications. Front. Psychol. 12, 734398 (2021).
Ho, E. et al. (ed, H.) Remote assessment of pediatric anthropometrics. Pediatrics e2024067663 https://doi.org/10.1542/peds.2024-067663 (2025).
Weintraub, S. et al. Cognition assessment using the NIH toolbox. Neurology 80, S54-64 (2013).
Carlozzi, N. E., Beaumont, J. L., Tulsky, D. S. & Gershon, R. C. The NIH toolbox pattern comparison processing speed test: normative data. Arch. Clin. Neuropsychol. 30, 359–368 (2015).
Heaton, R. K. et al. Reliability and validity of composite scores from the NIH toolbox cognition battery in adults. J. Int. Neuropsychol. Soc. 20, 588–598 (2014).
Weintraub, S. et al. I. NIH TOOLBOX COGNITION BATTERY (CB): INTRODUCTION AND PEDIATRIC DATA. Monogr. Soc. Res. Child. Dev. 78, 1–15 (2013).
Zelazo, P. D. The dimensional change card sort (DCCS): a method of assessing executive function in children. Nat. Protoc. 1, 297–301 (2006).
Eriksen, B. A. & Eriksen, C. W. Effects of noise letters upon the identification of a target letter in a nonsearch task. Percept. Psychophys. 16, 143–149 (1974).
Tulsky, D. S. et al. V. NIH TOOLBOX COGNITION BATTERY (CB): MEASURING WORKING MEMORY. Monogr. Soc. Res. Child. Dev. 78, 70–87 (2013).
Bauer, P. J. et al. III. NIH TOOLBOX COGNITION BATTERY (CB): MEASURING EPISODIC MEMORY. Monogr. Soc. Res. Child. Dev. 78, 34–48 (2013).
Dikmen, S. S. et al. Measuring episodic memory across the lifespan: NIH toolbox picture sequence memory test. J. Int. Neuropsychol. Soc. 20, 611–619 (2014).
Weiss, D. J. & Kingsbury, G. G. APPLICATION OF COMPUTERIZED ADAPTIVE TESTING TO EDUCATIONAL PROBLEMS. J. Educ. Meas. 21, 361–375 (1984).
Weiss, D. J. & Şahin, A. Computerized Adaptive Testing: from Concept To Implementation (The Guilford Press, 2024).
Gershon, R. C. et al. IV. NIH TOOLBOX COGNITION BATTERY (CB): MEASURING LANGUAGE (VOCABULARY COMPREHENSION AND READING DECODING). Monogr. Soc. Res. Child. Dev. 78, 49–69 (2013).
Gershon, R. C. et al. NIH Toolbox Oral Reading Recognition Test. (2017). https://doi.org/10.1037/t63740-000
Akshoomoff, N. et al. VIII. NIH TOOLBOX COGNITION BATTERY (CB): COMPOSITE SCORES OF CRYSTALLIZED, FLUID, AND OVERALL COGNITION. Monogr. Soc. Res. Child. 78 (4), 119–132 (2013).
Taylor, B. K. et al. Reliability of the NIH toolbox cognitive battery in children and adolescents: a 3-year longitudinal examination. Psychol. Med. 52, 1718–1727 (2022).
Dunn, O. J. Multiple comparisons among means. J. Am. Stat. Assoc. 56, 52–64 (1961).
Pastore, M. & Calcagnì, A. Measuring distribution similarities between samples: A distribution-Free overlapping index. Front. Psychol. 10, 1089 (2019).
Kuperman, V., Schroeder, S. & Gnetov, D. Word length and frequency effects on text reading are highly similar in 12 alphabetic languages. J. Mem. Lang. 135, 104497 (2024).
Rohde, L. E. et al. Associations between new York heart association classification, objective measures, and Long-term prognosis in mild heart failure: A secondary analysis of the PARADIGM-HF trial. JAMA Cardiol. 8, 150 (2023).
Pastore, M. Overlapping: a R package for estimating overlapping in empirical distributions. J. Open. Source Softw. 3, 1023 (2018).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2022).
Brugnaro, B. H. et al. Exploration of the feasibility of remote assessment of functioning in children and adolescents with developmental disabilities: parents’ perspectives and related contextual factors. Int. J. Environ. Res. Public. Health. 19, 15101 (2022).
Buzhardt, J. & Meadan, H. Introduction to the special issue: A new era for remote early intervention and assessment. J. Early Interv. 44, 103–109 (2022).
Bradley, R. H. & Corwyn, R. F. Socioeconomic status and child development. Annu. Rev. Psychol. 53, 371–399 (2002).
Quintana, S. M. et al. Race, ethnicity, and culture in child development: contemporary research and future directions. Child. Dev. 77, 1129–1141 (2006).
Xiao, Y. et al. Patterns of social determinants of health and child mental health, cognition, and physical health. JAMA Pediatr. 177, 1294 (2023).
Dorsey, E. R., Kluger, B. & Lipset, C. H. The new normal in clinical trials: decentralized studies. Ann. Neurol. 88, 863–866 (2020).
Khozin, S. & Coravos, A. Decentralized trials in the age of Real-World evidence and inclusivity in clinical investigations. Clin. Pharma Ther. 106, 25–27 (2019).
Grootswagers, T. A primer on running human behavioural experiments online. Behav. Res. Methods. 52, 2283–2286 (2020).
Whitehead, L., Talevski, J., Fatehi, F. & Beauchamp, A. Barriers to and facilitators of digital health among culturally and linguistically diverse populations: qualitative systematic review. J. Med. Internet Res. 25, e42719 (2023).
Richardson, J. T. E. Eta squared and partial Eta squared as measures of effect size in educational research. Educational Res. Rev. 6 (2), 135–147 (2011).
Acknowledgements
The authors would like to thank Patricia Bucko for her expert support with data visualization and Magdalena E. Kupczyk for her diligent project management that ensured the study’s smooth execution.
Funding
This work was supported by the Environmental Child Health Outcomes Study (1U24OD023319-01); Admin Supplement #(3U24OD023319-05S1).
Author information
Authors and Affiliations
Contributions
BE: Conceptualization, Methodology, Validation, Data Curation, Formal analysis, Investigation, Resources, Software, Writing - Original draft, Visualization EHH: Conceptualization, Methodology, Validation, Investigation, Resources, Writing - Review & Editing, Supervision, Funding acquisition ZT: Data curation, Formal analysis, Investigation, Project administration, Resources, Software, Validation, Writing - Review & Editing MAN: Writing - Review & Editing SG: Data curation, Formal analysis, Software, Visualization AZ: Data curation, Formal analysis, Software, Visualization VU: Investigation, Project administration, Resources CWH: Writing - Review & Editing RG: Conceptualization, Supervision, Funding acquisition.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ece, B., Ho, E.H., Tuladhar, Z. et al. A pilot study of remote cognitive assessment in children using the NIH toolbox participant/examiner app. Sci Rep 15, 36204 (2025). https://doi.org/10.1038/s41598-025-20256-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-20256-7