Abstract
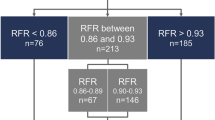
To develop a hybrid resting full-cycle ratio (RFR)- fractional flow reserve (FFR) decision-making approach for physiology-guided coronary revascularization in patients with non-ST elevation acute coronary syndrome (NSTE-ACS). This study comprised 253 NSTE-ACS patients (with 320 diseased vessels) who underwent invasive physiological evaluation at Cangzhou Central Hospital of Hebei Medical University between September 2021 and August 2023. The FFR threshold of ≤ 0.80 served as the reference standard for diagnosing functional coronary ischemia. Through exploratory analysis, a hybrid RFR-FFR method was developed to identify the “gray zones” of RFR measurements. The thresholds were set to reflect the upper boundary of high negative predictive values and the lower boundary of high positive predictive values, ensuring over 95.00% agreement with the FFR-alone methodology. Adenosine was employed solely for lesions with RFR values falling within these predefined thresholds, while the proportion of cases that could avoid adenosine in the hybrid model was quantified. When the concordance rate between the hybrid RFR-FFR model and the FFR-alone model reached 95.31%, adenosine use decreased significantly, showing a 56.56% reduction in vasodilator administration, coupled with positive and negative predictive values of 96.28% and 93.33%, respectively. As the zone requiring adenosine broadened, the correlation between the hybrid and FFR-alone strategies was strengthened, though the proportion of adenosine-free diseased vessels showed a corresponding decrease. The width of the adenosine requirement zone was 0.04 RFR points (0.89–0.92) and 0.07 RFR points (0.87–0.93) at the 90% and 95.31% agreement (concordance rate with FFR-only classification) levels, respectively. The hybrid RFR-FFR decision-making approach has the potential to reduce adenosine dependence in some patients while maintaining a high degree of consistency with the FFR alone decision-making approach. With the expansion of the adenosine requirement zone, the correlation between the hybrid strategy and the FFR-alone strategy further improved.
Similar content being viewed by others
Introduction
Non-ST elevation acute coronary syndrome (NSTE-ACS), an important subtype of acute coronary syndrome, primarily comprises unstable angina (UA) and non-ST elevation myocardial infarction (NSTEMI)1. Epidemiological data indicate that NSTE-ACS is linked to substantial morbidity and mortality on a global scale2. Patients diagnosed with this condition often present with intricate lesion profiles and a heightened risk of cardiovascular events3, which underscores the importance of accurately assessing the functional relevance of coronary stenoses. In this regard, the fractional flow reserve (FFR) has become a fundamental tool in coronary physiology, measuring the impact of coronary narrowing on blood flow4. FFR evaluates the pressure ratio between the site of stenosis and the aorta during a state of maximum hyperemia, providing an accurate assessment of coronary artery constriction. This evaluation assists in determining the need for interventional therapy at the lesion site during percutaneous coronary intervention (PCI)5, thus facilitating the refinement of therapeutic strategies. However, despite its established role in clinical practice, FFR use requires the administration of vasodilators (typically adenosine or its precursor adenosine triphosphate, ATP) to induce maximal hyperemia. Adenosine activates vascular receptors, causing potent microcirculatory vasodilation that minimizes resistance variability and is essential for standardized pressure gradient assessment. This process, while physiologically necessary, can lead to patient discomfort and increase both the procedural complexity and its associated costs6,7.
To address the limited application of physiologic assessments in revascularization guidance, there has been increasing interest in non-hyperemic pressure ratios (NHPRs). Key NHPRs include: Pd/Pa, the resting distal coronary-to-aortic pressure ratio, reflecting baseline hemodynamics without vasodilation8,9 and the instantaneous wave-free ratio (iFR)10,11. These methods offer the benefit of providing an initial assessment of coronary pressure during rest, thus avoiding the need for pharmacological induction. The resting full-cycle ratio (RFR) is a novel adenosine-free index for assessing the functional significance of coronary stenosis, defined as the minimum ratio of distal to aortic pressure (Pd/Pa) over the entire cardiac cycle12. It has been demonstrated that RFR is closely aligned with FFR, making it a reliable non-hyperemic marker for evaluating the severity of physiologic lesions12,13. Although several studies have examined the agreement between RFR and FFR, the limited number of investigations and the slow progress in this domain have prevented a definitive validation of RFR’s clinical utility. Therefore, additional research is critically needed. This study seeks to establish a hybrid RFR-FFR decision-making strategy for physiology-guided coronary revascularization in individuals with NSTE-ACS.
Methodologies
Study population
This prospective, single-center diagnostic accuracy study was conducted at Cangzhou Central Hospital between September 2021 and August 2023. The protocol received ethical approval from the Institutional Review Board of Hebei Medical University (Approval #2023-144-02), and all participants provided written informed consent. Inclusion criteria required: (1) Age ≥ 18 years; (2) Confirmed NSTE-ACS diagnosis; (3) Angiographically documented stenosis (30–90% diameter reduction); (4) Willingness to undergo invasive coronary function evaluation. Exclusion criteria: (1) Severe bronchial asthma; (2) Documented adenosine intolerance; (3) Second-degree or higher atrioventricular block; (4) Cardiogenic shock; (5) Inability to perform simultaneous RFR and FFR measurements or the occurrence of data drift.
A total of 267 consecutive patients with NSTE-ACS undergoing coronary angiography and invasive physiological assessment were initially enrolled, involving 337 diseased vessels. Following screening, 14 patients (17 vessels) meeting exclusion criteria were excluded: 13 patients (16 vessels) due to incomplete RFR assessment and 1 patient (1 vessel) due to significant FFR data drift. The final analytical cohort comprised 253 patients with 320 evaluable vessels.
Physiological assessment of coronary artery
All patients were subjected to CAG via radial artery access in compliance with current guidelines. During the coronary physiology assessment, the extent of coronary artery stenosis was first visually assessed by two experienced interventional cardiologists, independently performed visual assessments while blinded to each other’s interpretations. In cases of discrepancy, consensus was reached through joint re-evaluation and discussion, enabling consensus-based determination of invasive evaluation need according to clinical context. To mitigate the risk of coronary spasms, 200 µg of nitroglycerin was routinely administered before the procedure. The PressureWire™ x 0.014 pressure wire (Abbott, Santa Clara, CA, USA) was then positioned distal to the lesion site. Resting Pd/Pa and RFR values were initially recorded under non-hyperemic conditions. RFR is specifically defined as the minimum ratio of Pd/Pa measured over the entire cardiac cycle, capturing natural hemodynamic fluctuations without pharmacological provocation. This adenosine-free approach is feasible because RFR utilizes intrinsic pressure variations during resting conditions, avoiding the need for artificial hyperemia induction. Maximal hyperemia was then induced by intravenous ATP administered via median cubital vein at a weight-adjusted dosage of 167 µg/kg/min, calculated based on each patient’s actual body weight, thereby measuring the FFR value and accurately assessing the impact of stenosis on blood flow.
Hybrid RFR-FFR decision-making strategy
An RFR-FFR hybrid strategy is formulated through an exploratory analysis aimed at identifying the RFR “gray zone”: diagnostic uncertainty range requiring confirmatory FFR. This process establishes an upper limit, where the negative predictive value (NPV; probability of true non-ischemic lesions) exceeds 90%, thereby excluding lesions with an FFR above 0.80 (deferred RFR: medical management indicated). Simultaneously, a lower boundary is defined, characterized by a positive predictive value (PPV; probability of true ischemic lesions) surpassing 90%, to accurately ascertain lesions with an FFR of 0.80 or less (treatment RFR: revascularization indicated). In addition, the hybrid RFR-FFR method must achieve an overall agreement rate of no less than 95.00% when compared to the FFR-alone approach. For lesions with RFR values situated between the deferred and treatment thresholds, ATP will be administered to facilitate the standard FFR-based classification of the lesion. This hybrid approach transforms clinical decision pathways by: (1) Providing immediate treatment guidance for definitive RFR cases; (2) Targeting hyperemic testing to physiologically ambiguous lesions; (3) Minimizing unnecessary adenosine exposure while preserving diagnostic accuracy.
Adenosine requirement zone in the hybrid RFR-FFR decision-making strategy
Within the hybrid RFR-FFR strategy, the proportion of stenoses falling outside the adenosine requirement zone where ATP administration was deemed unnecessary-was calculated to evaluate the overall agreement with the FFR-alone strategy. In contrast to the FFR-alone approach, which mandates ATP administration for every diseased vessel, the adenosine requirement zone in the hybrid RFR-FFR strategy was defined by the deferred RFR value and the treatment RFR value. The magnitude of this zone was determined in increments of 0.01 RFR, indicating the range of RFR values for which ATP was necessary to perform FFR assessment.
Statistical analysis
Statistical analyses were executed utilizing SPSS version 26.0 and R version 4.3.3. The Kolmogorov-Smirnov test was applied to assess the normality of continuous variables. For normally distributed variables, data were reported as mean ± standard deviation, while non-normally distributed variables were denoted as median and interquartile range (IQR). Categorical variables were expressed as percentages. A cross-tabulation was performed to compare the overall classification concordance between the RFR-FFR strategy and the FFR-alone strategy. The potential reduction in adenosine use was evaluated by determining the proportion of stenoses within a specific range of RFR values. Additionally, the size of the adenosine-requiring region was calculated by assessing the range of RFR values for which adenosine administration was necessary. Consistency between the hybrid RFR-FFR strategy and FFR-alone classification was quantified using overall agreement rate, PPV, and NPV. 95% confidence intervals (CI) for these proportions were calculated via the Clopper-Pearson exact method to quantify estimation precision. Continuous variables were compared using Pearson correlation analysis to quantify linear relationships. Bland-Altman analysis assessed agreement between continuous physiological indices (RFR and FFR), with bias defined as the mean difference (RFR-FFR) and limits of agreement calculated as bias ± 1.96 × standard deviation.
Results
Population characteristics
The baseline clinical characteristics of the patients are presented in Table 1. The average age of the study population was 62.40 (56.50–69.00) years, with females comprising 41.50% (105 cases). The prevalence of hypertension, hyperlipidemia, and diabetes mellitus was 58.89% (149 cases), 14.23% (36 cases), and 24.51% (62 cases), respectively. Angiographic characteristics, patient physiologic assessment information is as follows, 203 (63.44%), 39 (12.19%), and 78 (24.38%) were left anterior descending artery, left circumflex, and right coronary artery lesions, respectively, and the stenosis degree of 287 (89.69%) vessels was ≥ 70% on angiography, which is commonly evaluated by FFR in standard clinical settings. The mean FFR was 0.83 ± 0.09, with 76.88% of the stenoses falling within the 0.60 to 0.90 range, while only 9.38% exhibited an FFR ≤ 0.70.
Correlation between RFR and FFR
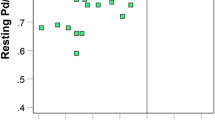
The correlation between RFR and FFR values was strong and statistically significant (Pearson r = 0.79, 95% CI: 0.74–0.83, P < 0.001). Bland-Altman analysis (Fig. 1) showed a mean bias of 0.09 (RFR-FFR) with 95% limits of agreement from − 0.03 to 0.20.
Overall concordance between hybrid RFR-FFR decision-making strategy and FFR-alone strategy
The hybrid revascularization strategy combining RFR and FFR has been shown to significantly reduce the requirement for adenosine in clinical practice. This method achieved a PPV of 96.28% (92.86%,98.43%) and a NPV of 93.33%. (87.29%,96.78%) Moreover, the hybrid approach demonstrated a 95.31% (92.27%,97.40%) concordance with the FFR-alone strategy, reducing the use of vasodilators by 56.56% (50.98%,61.98%).
The RFR gray zone was identified between values of 0.87 and 0.93. For RFR values below 0.87, PCI was advised, while conservative medical management was suggested for values exceeding 0.93. The comparison of the hybrid RFR-FFR strategy with the FFR-alone approach is illustrated in Fig. 2, where green represents concordant results, red indicates points of discordance, and the gray dots within the gray zone represent stenoses that require classification via FFR following adenosine administration.
Decrease in adenosine use with the hybrid RFR-FFR decision-making strategy
The implementation of the hybrid RFR-FFR strategy led to a substantial reduction in the number of patients requiring adenosine administration. The overall classification concordance between the RFR-FFR hybrid strategy and the FFR-alone method reached 95.31%, with a 56.56% reduction in the need for adenosine (Figs. 2 and 3). At concordance rates of 84.69%, 90.00%, and 99.38%, the predicted proportions of stenoses not requiring adenosine were 87.81%, 74.69%, and 17.50%, respectively (Figs. 3 and 4).
Effect of different sizes of adenosine requirement zones on overall concordance and proportion of adenosine-free patients: the larger the RFR range for adenosine administration, the greater the diagnostic concordance with the FFR-alone strategy (Panel B), but the smaller the proportion of adenosine-free patients (Panel A).
Overall concordance and adenosine-free ratios in different adenosine requirement zone
An expansion in the adenosine requirement zone is associated with a higher overall concordance between the hybrid RFR-FFR decision-making approach and the FFR-alone strategy, while simultaneously reducing the proportion of adenosine-free stenoses (Fig. 4). For the hybrid RFR-FFR strategy to achieve 90.00% and 95.31% concordance with the FFR-alone approach, the width of the adenosine requirement zone was found to be 0.04 RFR points (0.89–0.92) and 0.07 RFR points (0.87–0.93), respectively.
Discussion
FFR has become widely adopted as a standard tool for PCI assessment due to its accuracy and validation14,15,16. However, its reliance on adenosine-induced hyperemia increases procedural complexity, side effects, and costs17,18, limiting routine adoption.
NHPRs, particularly iFR and RFR, offer adenosine-free alternatives for revascularization guidance. iFR quantifies the distal-to-proximal coronary pressure ratio specifically during the wave-free period of diastole, when microvascular resistance is minimal19. A key hybrid iFR-FFR study20 demonstrated 94.70% classification accuracy using FFR adjudication for iFR gray-zone lesions (0.86–0.93), and 61% of patients avoiding adenosine administration. Diagnostic equivalence between iFR and RFR is well-established.
Svanerud et al.21 were the first to validate RFR, showing that RFR values ≤ 0.89 closely correspond to iFR values ≤ 0.89. Several studies have also indicated that RFR maintains a high level of concordance with FFR in most cases13. Retrospective data demonstrated that RFR achieved a diagnostic accuracy of 81.3% relative to FFR using a single cutoff method (RFR ≤ 0.89)21. Our team’s pre-study findings showed a strong correlation between RFR and FFR (r = 0.787, p < 0.001), with a diagnostic concordance of 80.8% and an area under the ROC curve of 0.883 for RFR predicting FFR ≤ 0.8022.
However, the diagnostic accuracy of RFR may be compromised when relying solely on a binary cutoff (RFR ≤ 0.89), limiting its standalone clinical utility. This necessitates the hybrid RFR-FFR strategy, which synergizes RFR’s simplicity with FFR’s precision to reduce adenosine use while improving diagnostic performance. In this model, RFR serves as an initial screening tool to exclude most non-significant stenoses, while those with RFR values falling within a “gray zone” require further assessment with FFR. This approach has already been applied in the context of iFR23, with iFR thresholds established at 0.86 and 0.93.
In the present study, the gray zone for the mixed RFR-FFR strategy was determined to be 0.87–0.93. The PPV was 96.28%, and the NPV was 93.33%, with a concordance with FFR of 95.31% and a reduction in vasodilator usage of 56.56%. These observations align with those of Casanova-Sandoval et al.24 in a prospective RFR versus FFR study, although they reported a gray zone of 0.86–0.92. At 90% concordance, the proportion of adenosine-free patients would increase to 74.69%, with RFR values below 0.89 and above 0.92 being considered for deferral and treatment, respectively, and if a 99% concordance level were selected, 17.5% of patients would still be adenosine-free.
The hybrid RFR-FFR strategy evaluates the severity of coronary stenosis by selectively administering adenosine within a specific range of RFR values, referred to as the adenosine requirement zone. The findings indicate that as the adenosine requirement zone expands (i.e., the RFR range increases), the classification concordance between the hybrid RFR-FFR strategy and the FFR-alone approach is enhanced. For instance, when the adenosine requirement zone spanned 0.04 RFR points (0.89–0.92), the concordance rate of the hybrid strategy reached 90%. Expanding the zone to 0.07 RFR points (0.87–0.93) further improved agreement to 95.31%. This suggests that a broader adenosine requirement zone more closely mirrors the decision-making process of the FFR-alone approach, thereby enhancing consistency.
However, this improvement in consistency comes at the expense of a lower proportion of adenosine-free stenosis cases. In other words, a wider adenosine requirement zone increases the number of cases requiring adenosine, which reduces one of the primary benefits of the hybrid strategy-minimized adenosine use compared to the FFR-alone approach. Therefore, while a broader adenosine requirement zone enhances overall concordance in the hybrid RFR-FFR strategy, a balance must be struck between achieving consistency and minimizing adenosine use.
For example, when the adenosine requirement zone expands from 0.04 RFR points (0.89–0.92) to 0.07 RFR points (0.87–0.93), although diagnostic concordance increases from 90% to 95.31%, the proportion of lesions requiring adenosine assessment also rises accordingly. Expanding the adenosine requirement zone reduces decision-making uncertainty associated with RFR-based classification, particularly for lesions with RFR values near the gray zone, thereby lowering the risk of misclassification. This is especially critical for high-risk patients. Additionally, each lesion requiring adenosine assessment adds procedural time, including guidewire preparation, drug infusion, and hemodynamic stabilization.
Therefore, in clinical practice, the width of the adenosine requirement zone should be tailored to specific scenarios. Narrower zones may be selected for stable, straightforward lesions such as focal stenosis in stable angina to optimize procedural efficiency, while broader zones are strongly recommended for high-risk lesions including proximal left anterior descending artery lesions to prioritize diagnostic accuracy. Notably, the agreement between RFR and FFR may vary across specific patient subgroups. For instance, recent evidence suggests reduced correlation in patients with concomitant aortic stenosis (AS), potentially due to altered coronary flow dynamics and microvascular dysfunction25. Further research is necessary to explore and optimize this balance in order to achieve more accurate and efficient coronary stenosis evaluation. Beyond pharmacologic hyperemia, emerging techniques like contrast-induced FFR and saline-induced hyperemia offer adenosine-free alternatives for physiological assessment26. While these methods require further validation, they represent promising pathways toward eliminating vasodilator dependency entirely in future clinical practice.
Pharmacologic alternatives such as papaverine, a potent coronary vasodilator acting via phosphodiesterase inhibition, provide viable options for achieving hyperemia in adenosine-contraindicated patients (e.g., high-grade atrioventricular block or severe asthma). Importantly, our hybrid strategy’s adenosine-sparing benefit extends to institutions utilizing such alternatives, as they achieve comparable maximal hyperemia for definitive FFR measurement27.
Limitations
This study has several limitations that should be carefully considered when interpreting the findings. First, this study utilized the same cohort for both developing RFR thresholds (gray zone 0.87–0.93) and validating the hybrid strategy. Although analysis protocols were prospectively defined, this approach carries inherent risks of overfitting, reduced external validity, and lacks independent validation. The single-center design with limited sample size (253 patients/320 vessels) further constrains generalizability. Additionally, the study used a single cohort to both develop and validate the RFR cut-off points, which, while providing initial evidence of the potential utility of RFR, is subject to the risk of overfitting. Furthermore, the lack of an independent validation cohort is a significant limitation. All lesions were tested both with and without adenosine, which may not accurately reflect the real-world scenario where RFR would be used to decide whether to administer adenosine. Therefore, while our findings suggest that RFR could potentially reduce the need for adenosine in some patients, these results need to be validated in a larger, independent patient population to confirm their robustness and clinical applicability. Second, left anterior descending (LAD) artery lesions represented 63.4% of the cases. The large area of myocardial perfusion in the LAD region could have contributed to variations between RFR and FFR measurements, potentially affecting the study’s results. Third, ATP was employed as a vasodilator in this study, in contrast to the frequently employed adenosine. This difference in vasodilators may have influenced myocardial perfusion and coronary blood flow, possibly impacting the link between RFR and FFR. Fourth, the results of this study are mainly applicable to patients with NSTE-ACS, especially in the ‘grey area’ of RFR and FFR. In patients with ST-elevation myocardial infarction (STEMI), particularly in the acute phase, these results may need to be applied with caution. Fifth, no vessel size description in terms of diameter is provided in this study. Major trials of complete revascularization typically exclude vessels smaller than 2.5 mm due to their different hemodynamic characteristics and the potential for increased variability in physiological measurements. The inclusion of smaller vessels in our study may have influenced the results and their generalizability to other populations. Sixth, direct comparison with Pd/Pa was not performed, though literature suggests similar NHPR performance28. Future studies should address these limitations by using larger, independent patient populations and exploring the long-term clinical outcomes associated with hybrid RFR and FFR-guided revascularization compared to FFR-guided revascularization.
Conclusions
This study demonstrates that the hybrid RFR-FFR strategy reduces adenosine requirements for physiological assessment in patients with NSTE-ACS while maintaining high concordance with FFR-based stenosis classification. By integrating RFR as an initial screening tool and reserving FFR for lesions within the RFR gray zone (0.87–0.93), this approach preserves diagnostic reliability and may facilitate broader adoption of physiology-guided revascularization (Fig. 5). Future research should validate these findings in multicenter cohorts and assess long-term clinical outcomes to establish standardized implementation protocols.
Data availability
The primary information substantiating the findings of this investigation will be provided by the researchers without unnecessary delay or restriction. Data are available upon request from the corresponding author.
References
Hedayati, T., Yadav, N., Khanagavi, J. & Non -ST-Segment Acute Coronary Syndromes. Cardiol. Clin., 36(1):37–52. doi: https://doi.org/10.1016/j.ccl.2017.08.003 (2018).
Sanchis-Gomar, F., Perez-Quilis, C., Leischik, R. & Lucia, A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann. Transl Med. 4 (13), 256. https://doi.org/10.21037/atm.2016.06.33 (2016).
Pilgrim, T. et al. Risk and timing of recurrent ischemic events among patients with stable ischemic heart disease, non-ST-segment elevation acute coronary syndrome, and ST-segment elevation myocardial infarction. Am. Heart J. 175, 56–65. https://doi.org/10.1016/j.ahj.2016.01.021 (2016).
Elbadawi, A. et al. Contemporary use of coronary physiology in Cardiology. Cardiol. Ther. 12 (4), 589–614. https://doi.org/10.1007/s40119-023-00329-2 (2023).
Shantouf, R. S. & Mehra, A. Coronary fractional flow reserve. AJR Am. J. Roentgenol. 204 (3), W261–W265. https://doi.org/10.2214/AJR.14.13933 (2015).
Feng, J. & Wu, X. [Research progress in fractional flow Reserve]. Zhongguo Yi Liao Qi Xie Za Zhi. 44 (2), 179–184. https://doi.org/10.3969/j.issn.1671-7104.2020.02.017 (2020).
Terentes-Printzios, D. et al. Angiography-based Estimation of coronary physiology: A frame is worth a thousand words. Trends Cardiovasc. Med. 32 (6), 366–374. https://doi.org/10.1016/j.tcm.2021.07.004 (2022).
Piroth, Z. et al. Correlation and relative prognostic value of fractional flow reserve and Pd/Pa of nonculprit lesions in ST-Segment-Elevation myocardial Infarction. Circ. Cardiovasc. Interv. 15 (2), e10796. https://doi.org/10.1161/CIRCINTERVENTIONS.121.010796 (2022).
Leone, A. M. et al. The Multi-center evaluation of the accuracy of the contrast medium induced Pd/Pa ratio in predicting FFR (MEMENTO-FFR) Study. EuroIntervention 12 (6), 708–715. https://doi.org/10.4244/EIJV12I6A115 (2016).
Davies, J. E. et al. Use of the instantaneous Wave-free ratio or fractional flow reserve in PCI. N Engl. J. Med. 376 (19), 1824–1834. https://doi.org/10.1056/NEJMoa1700445 (2017).
Gotberg, M. et al. Instantaneous Wave-free ratio versus fractional flow reserve to guide PCI. N Engl. J. Med. 376 (19), 1813–1823. https://doi.org/10.1056/NEJMoa1616540 (2017).
Malmberg, S., Lauermann, J., Karlstrom, P., Gulin, D. & Barmano, N. Resting Full-Cycle ratio versus fractional flow reserve: A SWEDEHEART-Registry-Based comparison of two physiological indexes for assessing coronary stenosis Severity. J. Interv Cardiol. 2023, 6461691. https://doi.org/10.1155/2023/6461691 (2023).
Ohashi, H. et al. Clinical feasibility of resting full-cycle ratio as a unique non-hyperemic index of invasive functional lesion assessment. Heart Vessels. 35 (11), 1518–1526. https://doi.org/10.1007/s00380-020-01638-5 (2020).
Paolucci, L. et al. Fractional flow Reserve-Guided coronary revascularization: evidence from randomized and Non-Randomized Studies. Diagnostics (Basel). 12 (11). https://doi.org/10.3390/diagnostics12112659 (2022).
Tonino, P. A. et al. TVM,. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med, 360(3):213–224. (2009). https://doi.org/10.1056/NEJMoa0807611
De Bruyne, B. et al. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl. J. Med. 367 (11), 991–1001. https://doi.org/10.1056/NEJMoa1205361 (2012).
Shah, T. et al. Fractional flow reserve to guide surgical coronary revascularization. J. Thorac. Dis. 9 (Suppl 4), S317–S326. https://doi.org/10.21037/jtd.2017.03.55 (2017).
Gotberg, M. et al. The evolving future of instantaneous Wave-Free ratio and fractional flow Reserve. J. Am. Coll. Cardiol. 70 (11), 1379–1402. https://doi.org/10.1016/j.jacc.2017.07.770 (2017).
Sen, S. et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine vasodilator independent stenosis Evaluation) study. J. Am. Coll. Cardiol. 59 (15), 1392–1402. https://doi.org/10.1016/j.jacc.2011.11.003 (2012).
Harle, T., Bojara, W., Meyer, S. & Elsasser, A. Comparison of instantaneous wave-free ratio (iFR) and fractional flow reserve (FFR)--first real world experience. Int. J. Cardiol. 199, 1–7. https://doi.org/10.1016/j.ijcard.2015.07.003 (2015).
Svanerud, J., Ahn, J. M., Jeremias, A., van Gore, T. V. M. & Maehara, A. Validation of a novel non-hyperaemic index of coronary artery stenosis severity: the resting Full-cycle ratio (VALIDATE RFR) study. EuroIntervention 14 (7), 806–814. https://doi.org/10.4244/EIJ-D-18-00342 (2018).
Lei, Y. et al. Correlation and consistency between resting full-cycle ratio and fractional flow reserve in assessing coronary artery function in a Chinese real-world cohort with non-ST-segment elevation acute coronary syndrome: a retrospective observational study. BMJ Open. 14 (8), e82913. https://doi.org/10.1136/bmjopen-2023-082913 (2024).
Petraco, R. et al. Hybrid iFR-FFR decision-making strategy: implications for enhancing universal adoption of physiology-guided coronary revascularisation. EuroIntervention 8 (10), 1157–1165. https://doi.org/10.4244/EIJV8I10A179 (2013).
Casanova-Sandoval, J. et al. Usefulness of the hybrid RFR-FFR approach: results of a prospective and multicenter analysis of diagnostic agreement between RFR and FFR-The RECOPA (REsting Full-Cycle ratio comparation versus fractional flow reserve (A prospective Validation)) Study. J Interv Cardiol, 2021,2021:5522707. https://doi.org/10.1155/2021/5522707
Gallinoro, E. et al. Effect of TAVI on epicardial functional indices and their relationship to coronary microvascular Function. Circ. Cardiovasc. Interv. 18 (6), e14940. https://doi.org/10.1161/CIRCINTERVENTIONS.124.014940 (2025).
Gallinoro, E. et al. Saline-induced coronary hyperemia with continuous intracoronary thermodilution is mediated by intravascular hemolysis. Atherosclerosis 352, 46–52. https://doi.org/10.1016/j.atherosclerosis.2022.05.011 (2022).
De Bruyne, B. et al. Intracoronary and intravenous adenosine 5’-triphosphate, adenosine, papaverine, and contrast medium to assess fractional flow reserve in humans. Circulation 107 (14), 1877–1883. https://doi.org/10.1161/01.CIR.0000061950.24940.88 (2003).
Van, T. V. M. et al. Comparison of different diastolic resting indexes to iFR: are they all equal? J. Am. Coll. Cardiol. 70 (25), 3088–3096. https://doi.org/10.1016/j.jacc.2017.10.066 (2017).
Funding
This work was supported by the Natural Science Foundation of Hebei Province, China (H2021110008).
Author information
Authors and Affiliations
Contributions
H.L, You.W, Y.M, and Li.Y were involved in conceptualizing the study, analyzing the data, and drafting the manuscript. S.F, X.L, M.J, and M.C aided in research design and provided feedback on the paper. N.G, Yun.W, J.Y and Lei Y helped with material preparation, data collection, and manuscript review. Y.M and Li.Y serve as guarantors, overseeing the overall content. All authors contributed to the article and gave their approval for the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki, and the research involving human subjects was evaluated and endorsed by the Ethics Committee at Cangzhou Central Hospital, affiliated with Hebei Medical University, which sought to sanction the study protocol (2023-144-02). Every patient and participant supplied written informed consent prior to their involvement in this investigation.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Liu, H., Wang, Y., Fang, S. et al. Physiology guided coronary revascularization using a hybrid RFR-FFR strategy for Non ST elevation acute coronary syndrome. Sci Rep 15, 36667 (2025). https://doi.org/10.1038/s41598-025-20563-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-20563-z