Abstract
Lung squamous cell carcinoma (LSCC) is among the most prevalent and deadly malignancies in arsenic‐exposed populations, yet effective targeted therapies remain elusive. Cross-Reactive Material (CRM197), a non‐toxic mutant of diphtheria toxin that binds heparin‐binding EGF‑like growth factor (HB‑EGF), has demonstrated anti‑tumor activity, but its efficacy against arsenic‐induced LSCC has not been characterized. In this study, we assessed CRM197’s effects on proliferation (CCK‑8 and colony‑formation assays), cell‑cycle progression (flow cytometry), comparing its activity to cetuximab and afatinib in arsenic‑transformed BEAS‑2B cells obtained by 6-month treatment on human bronchial epithelial cells BEAS-2B with low-dose sodium arsenite (As‑T) and lung cancer cells(NCI‑H226 and PC‑9). Next, we evaluated in vivo efficacy in nude mice bearing As‑T and NCI‑H226 xenografts treated daily with CRM197 (5 mg/kg) or afatinib. Finally, tandem‑mass‑tag proteomics and network pharmacology identified 179 upregulated proteins in As‑T cells and 11 overlapping CRM197 targets—including AKR1B1, PTPN1, PPARA, and SERPINE1—which were validated by molecular docking and 100‑ns dynamics simulations. CRM197 markedly inhibited cell proliferation, induced G₀/G₁ arrest, and outperformed cetuximab and matched or exceeded afatinib in vitro; in vivo, CRM197 reduced tumor volume and weight more effectively than afatinib, with extensive necrosis. These data establish CRM197 as a potent, multi‑targeted inhibitor of arsenic‑driven LSCC and highlight novel therapeutic targets for further drug development.
Similar content being viewed by others
Introduction
Lung squamous cell carcinomas (LSCCs) account for approximately 30% of newly diagnosed cases of non-small cell lung cancer (NSCLC)1,2. This type of the cancer offers limited treatment options in advanced stages3. LSCC exhibits unique epidemiological, clinicopathological, and molecular characteristics4. It is primarily caused by the destruction of bronchial mucosal epithelial cells, loss of cilia, and squamous metaplasia of basal cells due to prolonged exposure to harmful substances. The mutation rate of the epidermal growth factor receptor (EGFR) in LSCC is relatively low5,6, often resulting in suboptimal responses to commonly used chemotherapy regimens.
Arsenic is a well-known environmental toxicant that has been linked to various human malignancies, including LSCC 7,8. Long-term exposure to arsenic, whether through contaminated drinking water or occupational environments, can result in genomic instability 5, abnormal gene expression, and epigenetic alterations in lung epithelial cells. Mechanistically, arsenic-induced oxidative stress initiates a series of intracellular signaling cascades. For instance, it can activate mitogen-activated protein kinases (MAPKs)9, which subsequently regulate the expression of proto-oncogenes and tumor suppressor genes involved in cell proliferation, apoptosis, and differentiation10.
Given the established association between arsenic exposure and LSCC, it is urgent to elucidate the mechanism of arsenic- induced malignant transformation of cells in order to find effective prevention, diagnosis, and treatment targets for lung squamous cell carcinoma. Arsenic‑transformed BEAS‑2B cells were obtained by 6-month treatment on human bronchial epithelial cells BEAS-2B with low-dose sodium arsenite (As‑T) to identify abnormal expression of proteins in As-T cells for finding effective prevention, diagnosis, and treatment targets for lung squamous cell carcinoma. CRM197, a non-toxic mutant of diphtheria toxin, has emerged as a promising candidate. Previous studies have demonstrated its anti-tumor activity across multiple cancer models, although its precise mechanism of action remains incompletely understood11,12. Preliminary evidence suggests that CRM197 may disrupt the growth and survival pathways of cancer cells by regulating key signaling molecules and inducing cell cycle arrest or apoptosis13. The aim of this study is to elucidate the inhibitory effect and targets of CRM197 on LSCC. This research not only contributes to a better understanding of the disease’s pathogenesis but also lays the groundwork for the development of more effective therapies against LSCC.
Materials and methods
Cell culture
Human bronchial epithelial BEAS-2B (BEAS-2B) and As-T cells were established and cultured in DMEM medium mixed with 10% heat-inactivated fetal bovine serum (FBS), 100 units/mL penicillin G, and 100 μg/mL streptomycin. The NCI-H226 and PC9 cells were purchased from EK-bioscience Biotechnology Company and cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum (FBS), 100 units/mL penicillin G and 100 μg/mL streptomycin. The CRM(197) used in this experiment was purchased from Jicang Biotech (Chongqing,China).
Cell proliferation assay
After adjusting the cell densities of each group of lung cancer NCI-H226, PC9, and As-T cells to 1 × 104 cells/mL, 200 μL of the cell suspension was taken from each and added to a 96-well plate respectively. Then, the cells were cultured at 37 °C for 0, 24 h, 48 h, 72 h, and 96 h. Subsequently, 10 µL of CCK-8 solution was added to each well. After incubation at 37 °C for 2 h, the absorbance (OD) value at a wavelength of 450 nm was detected using a microplate reader.
Flow cytometry analysis of cell cycle
The cells were cultured and transfected with the corresponding plasmids for 48 h, and then transferred into collection tubes. The cells were fixed in 1 mL of 70% cold ethanol for 2 h, washed with ice-cold PBS three times, and suspended in 100 μL of PBS containing 0.5 mL of PI/RNase Staining Buffer (BD Biosciences, USA) at room temperature for 15 min in the dark. Flow cytometry analysis was performed within 24 h after PI staining. Finally, the cell cycle distribution was determined using a flow cytometer (Beckman Coulter, USA).
Western blot experiment
Protein samples were isolated from cells and animal tissues, and then separated by SDS polyacrylamide gel electrophoresis and transferred onto a 0.2 μm PVDF membrane (Sigma, USA). The blots were blocked with Tris-buffered saline containing 5% BSA at room temperature for 2 h and immunoblotted with appropriate primary antibodies overnight at 4 °C. The next day, the blots were incubated with secondary antibodies at room temperature for 1 h.
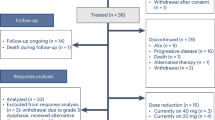
Animal experiments
Male BALB/c nude mice (4 weeks old) were purchased from the Animal Center of Nanjing Medical University (Nanjing, China). A total of 45 BALB/c mice were housed under controlled temperature (23 ± 2 °C) and a 12-h light–dark cycle, with free access to food and water. The mice were fed a standard diet (5.1% fat, 55.3% carbohydrates, 23.1% protein).
The 45 mice were divided into 3 major groups (n = 15 per group). Each group received a subcutaneous injection of 5 × 105–2 × 10⁶ cells/100 μL into the lower dorsum, with the following cell lines: As-T cells、NCI-H226 cells、PC-9 cells.
Tumor growth was monitored starting on Day 14 post-inoculation. On Day 14, each major group was further subdivided into 3 subgroups (n = 5 per subgroup) and treated daily from Day 14 to Day 25 via intramuscular injection with:100 μL PBS (control)、100 μL 5 mg/kg CRM197、100 μL 5 mg/kg afatinib. Tumor volume was measured daily using a vernier caliper. All mice were euthanized on Day 25 for endpoint analysis.
In animal experiments, we used 2.5% (w/v) Avertin as the anesthetic, administered via intraperitoneal injection at a dose of 0.2 mL/10 g of body weight in mice. Once the anesthesia took effect and the animals reached a deep anesthetic state, euthanasia was performed by cervical dislocation or other ethically approved methods to ensure a pain-free and humane endpoint.
Animal handling and experimental procedures were carried out in accordance with the Guidelines for the Care and Use of Laboratory Animals of Nanjing Medical University.
Molecular docking
The compounds with the top 10° values in SJZD active ingredient-target network were selected as ligands, and we used the PubChem database to search the three-dimensional structure of these compounds. The targets with the top 5° value were selected in the drug-disease common target PPI network and the main pathway-target point network. In addition, we add the other 2 identified CRC targets by consulting the literature. All above obtained targets were entered in the Protein Data Bank database (PDB, https://www.rcsb.org/), the refining conditions were limited by following conditions: the source organism was Homo sapiens, the experimental method was X-ray diffraction, the resolution was ≤ 3, and the release years was ≤ 10, then we selected the target protein as receptors which were suitable for docking from the remaining search results. Then the results were imput into AutoDock. AutoDock is an open source software for molecular modeling and simulation and one of the most accurate docking tools. It can effectively perform protein–ligand docking. AutoDock Tools can determine the binding sites of molecules by setting the three-dimensional coordinates of the receptor protein pockets to increase the accuracy of the results. Then we used Autodock Tools to add polar hydrogen, add charge and adjust Grid box size. At last the qdbpt formats were output for preparing docking.
Target prediction and, construction of PPI network
This study employed a network pharmacology approach to predict potential targets of the compound CRM197 and analyze its protein–protein interaction (PPI) network. First, the canonical SMILES structure of CRM197 was obtained from the PubChem database. Target prediction was performed using dual platforms, SwissTargetPrediction (https://www.swisstargetprediction.ch/) and SuperPred (https://prediction.charite.de/). The compound’s SMILES was submitted to both platforms, with SwissTargetPrediction configured for the species Homo sapiens and retaining targets with a significant *p*-value < 0.05. Results from both platforms were integrated, redundant entries were removed, and gene names were standardized using the UniProt ID mapping tool. Subsequently, the final target list was imported into the STRING database (https://string-db.org/) to construct a PPI network, with parameters set to Homo sapiens species and an interaction confidence score > 0.7. The network data were exported in TSV format, followed by further topological analysis using Cytoscape 3.9.1.
Statistical analysis
All experiments were repeated three times. The data were analyzed by Microsoft Excel 2022, and the correlations were analyzed by GraphPad Prism 9.0. Statistical evaluation of the data was performed using the t-test. A P-value of less than 0.05 was considered statistically significant. *P < 0.05, **P < 0.01, ***P < 0.001, ns, not significant.
Results
Construction of As-T cell lines and proteomics of As-T and B2B
To verify that arsenic and its compounds can induce the malignant transformation of lung epithelial cells, Arsenic-transformed cells (As-T) were obtained through continuous treatment human lung epithelial cells BEAS-2B with arsenic for 6 months, as described previously14. Following the acquisition of As-T and its control of BEAS-2B treated with PBS for 6 months (B2B), we investigated the role of arsenic and its molecular mechanisms in inducing the malignant transformation of lung epithelium by comparing the characteristics of B2B with those of As-T cells. To verify whether the arsenic-transformed cells As-T have the malignant phenotype of tumor cells, after obtaining the arsenic-transformed cells As-T, the proliferation levels of B2B cells and As-T cells were detected by the CCK8 proliferation assay. The experimental results showed that the proliferation level of the arsenic-transformed cells As-T was significantly higher than that of B2B cells (Fig. 1A). Meanwhile, we further verified using the cell colony formation assay. The number of colonies formed by the arsenic-transformed cells As-T was significantly greater than that of B2B cells, while B2B cells rarely or hardly formed colonies (Fig. 1B). All the above results indicate that treatment with arsenic significantly promoted the proliferation level and colony formation of human lung epithelial B2B cells, suggesting that arsenic is involved in the process of the malignant transformation of lung epithelial cells by promoting the excessive proliferation of lung epithelial cells.
Arsenic-induced malignant transformation of human bronchial epithelial cells BEAS-2B (B2B) and its molecular mechanisms. (A) Cell proliferation assessed by CCK-8 assay. The proliferation of arsenic-transformed cells (As-T) and normal B2B cells was measured at 24, 48, 72, 96 h. Data are presented as mean ± SD of independent experiments. ****p < 0.0001 compared to B2B cells. (B) Colony formation assay. The colony-forming ability of As-T cells and B2B cells was evaluated. Representative images and quantitative analysis of colony numbers are shown. **p < 0.01 compared to B2B cells. (C) A total of 179 upregulatedly expressed proteins were identified in As-T cells compared to B2B cells. (D) Functional enrichment analysis of differentially expressed proteins. TMT-based proteomics analysis identified 179 upregulatedly expressed proteins between As-T and B2B cells, which were enriched in pathways such as cell cycle, PI3K-AKT signaling pathway, and the p53 signaling pathway and apoptosis. (E) Heatmap of key genes in enriched pathways. Expression levels of key genes in the enriched pathways were significantly upregulated in As-T cells compared to B2B cells. (F) Western blot analysis of EGFR, p-EGFR, and HB-EGF expression. Protein levels of EGFR, phosphorylated EGFR (p-EGFR), and HB-EGF were detected in As-T and B2B cells. Results showed decreased EGFR and increased p-EGFR and HB-EGF levels in As-T cells, suggesting rapid activation of EGFR by HB-EGF.
To investigate the molecular mechanisms by which arsenic promotes the malignant transformation of lung epithelial cells, we conducted a proteomic analysis on B2B cells and As-T cells using the tandem mass tag (TMT) labeling technique, and conducted protein identification and quantification by liquid chromatography-tandem mass spectrometry (LC–MS/MS). 179 upregulated-expressed proteins were identified (Fig. 1C). These proteins were respectively enriched in signaling pathways such as the cell cycle, PI3K-AKT signaling pathway, and the p53 signaling pathway (Fig. 1D), and the key proteins within these pathways were significantly upregulated in the arsenic treatment group (Fig. 1E and 1F). These findings suggest that arsenic may induce the malignant transformation of lung epithelial cells through the modulation of these signaling pathways, but the results still need further exploration.
3.2 The inhibitory effect of CRM197 on As-T growth is superior to cetuximab and afatinib at certain time points, but its inhibitory effect on NCI-H226 and PC-9 growth is weaker than afatinib.
Heparin-binding EGF-like growth factor (HB-EGF) is an EGFR ligand and may be a potential therapeutic target for lung cancer. CRM197 is a well-known inhibitor of HB-EGF and induced significant cell apoptosis and marked suppression of tumorigenicity in As-T cells and lung cancer cells12,15. However, there are few reports on the effect of CRM197 on LSCC. NCI-H226 without EGFR mutation is an important model for studying LSCC and has been reported for studying the roles of EGFR, PI3K/AKT, MAPK and other pathways in lung cancer16,17. PC-9 cell originates from human lung adenocarcinoma tissue and carries an EGFR exon 19 deletion mutation, which is one of the common EGFR activation mutations in lung adenocarcinoma. This mutation leads to sustained activation of the EGFR signaling pathway, promoting tumor growth, making PC-9 highly sensitive to EGFR tyrosine kinase inhibitors such as gefitinib and erlotinib18. Afatinib is not only a first-line treatment for EGFR mutation positive lung adenocarcinoma, particularly effective against common EGFR mutations such as exon 19 deletion and exon 21 L858R point mutation19,20 but also approved for second-line treatment of advanced lung squamous cell carcinoma, especially after platinum based chemotherapy failure21,22. Cetuximab-based therapy is suitable for squamous cell of lung cancer with EGFR high copy number according to the report27.
We detected the effect of CRM197 on the proliferation of As-T and NCI-H226, and compared its efficacy with two clinical anti-tumor drugs, cetuximab and afatinib, on As-T, NCI-H226 and PC-9. According to the literature, the inhibitory effects of CRM197 at a concentration of 10 μg/ml, cetuximab at 10 μg/ml, and afatinib at 5 μg/ml were compared. The results indicated that CRM197, cetuximab, and afatinib all inhibited the proliferation of tumor cells. Notably. CRM197 demonstrated superior inhibitory activity on As-T cells at certain time points (Fig. 2A), Flow cytometry was employed to assess the cell cycle distribution of As-T, NCI-NCI-H226 and PC-9 cells treated with the drugs CRM197and afatinib to analyze their proliferation status. The results indicated that in the control group of As-T cells, the proportion of cells in the G0/G1 phase was 57.66%, the proportion of S-phase cells was 27.88%, and the proportion of G2/M-phase cells was 14.57%. This suggests that under normal physiological conditions, the cell population maintains a relatively stable proliferative state. Most cells are in the G0/G1 phase, which is crucial for material preparation and growth regulation, while only a certain proportion of cells progress to the S phase for DNA synthesis and the G2/M phase for mitotic preparation and cell division processes. After treatment with CRM197, the cell cycle distribution of As-T cells changed significantly. The proportion of cells in the G0/G1 phase increased to 60.97%, and the proportion of S-phase cells rose to 30.91%. Conversely, the proportion of G2/M-phase cells decreased significantly to 8.12%, and the proportion of apoptotic cells was 9.03%. In contrast, the cell cycle changes in As-T cells treated with afatinib were not significant. This result suggests that CRM197 causes a greater number of As-T cells to be arrested in the S phase, inhibiting the transition of cells from the S phase to the G2/M phase. Consequently, this reduces the number of cells entering the DNA synthesis stage and slows down the proliferation rate of tumor cells to some extent. In NCI-H226 and PC-9 cells, afatinib exhibited a more pronounced inhibitory effect on cell proliferation (Fig. 2B). In summary, the findings of this study indicate that CRM197 can effectively alter the cell cycle distribution of As-T cells and significantly inhibit their proliferation, providing a crucial experimental foundation for further exploration of the mechanisms underlying the action of CRM197 in cellular biological behaviors.
Effects of CRM197, cetuximab, and afatinib on the proliferation and cell cycle distribution of arsenic-transformed cells (As-T) and lung cancer cells, and proteomic analysis of CRM197-treated As-T cells. (A) Cell proliferation assessed by CCK-8 assay. The inhibitory effects of CRM197 (10 µg/mL), cetuximab (10 µg/mL), and afatinib (5 µg/mL) on the proliferation of As-T, H226, and PC-9 cells were measured at 24, 48, 72, 96 h. Data are presented as mean ± SD of independent experiments. ****p < 0.0001 compared to the cetuximab group. CRM197 showed superior inhibitory activity on As-T cells at certain time points. (B) Cell cycle analysis by flow cytometry. The cell cycle distribution of As-T, H226, and PC-9 cells treated with CRM197 or afatinib was analyzed. In As-T cells, CRM197 treatment increased the proportion of cells in G0/G1 phase (60.97%) and S phase (30.91%), while significantly decreasing the proportion in G2/M phase (8.12%) and inducing apoptosis (9.03%). Afatinib showed more pronounced effects on H226 and PC-9 cells. (C) Functional enrichment analysis of differentially expressed proteins. KEGG pathway analysis revealed that the differentially expressed proteins were significantly enriched in pathways such as anti-apoptosis, cell cycle, PI3K-AKT signaling, and p53 signaling. These results suggest that CRM197 may inhibit the proliferation of As-T cells through these pathways. (D) Heatmap of key genes in enriched pathways. After CRM197 treatment, the expression levels of key proteins in the enriched pathways were significantly downregulated.
The tandem mass tag (TMT) labeling technique was employed to conduct a proteomic analysis on arsenic-transformed lung cancer As-T cell samples, as well as on those treated with the CRM197 drug. Protein identification and quantification were performed using liquid chromatography-tandem mass spectrometry (LC–MS/MS). A total of 132 differentially expressed proteins were identified between the CRM197treatment group and the control group. Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses23,24 revealed that the differentially expressed proteins following CRM197 treatment were significantly enriched in pathways related to anti-apoptosis, the cell cycle (Fig. 2C, D). These findings suggest that CRM197 may inhibit the proliferation of arsenic-transformed lung cancer cells through these pathways.
Network pharmacology reveals the targets of CRM197
To further investigate the mechanism by which CRM197 inhibits the proliferation of lung cancer cells, we predicted the targets of CRM197. The chemical structure of CRM197 is illustrated in Fig. 3A. The SwissTargetPrediction website suggested that the functions of CRM197 may include acting as a protease and a surface antigen, among other roles (Fig. 3B). We utilized SwissTargetPrediction and SuperPred to identify 102 and 242 potential targets, respectively, which may serve as the pharmacological targets of CRM197. Subsequently, we cross-referenced the 102 and 242 targets predicted by SwissTargetPrediction and SuperPred with the 179 upregulated protein targets mentioned earlier, resulting in 11 overlapping targets: MME, ERAP2, AKR1B1, FPR1, NTSR2, CTSD, PTPN1, SERPINE1, PTPN2, CYSLTR2, and PPARA (Figs. 3C and 3D). These overlapping targets may represent potential therapeutic targets of CRM197 for arsenic-induced malignant transformation in lung cancer. We conducted a protein–protein interaction (PPI) network analysis of the genes corresponding to these 11 overlapping targets (Fig. 3E), identified the key hub proteins within this network, and performed KEGG pathway enrichment analyses on these key hub proteins (Fig. 3F and 3G). The expression levels of CCND1, p-AKT, and AKT were significantly decreased by western blotting, indicating that CRM197 inhibited the PI3K-AKT pathway in vivo, which aligned with the predictions made by network pharmacology (Fig. 3H). According to the results of the KEGG pathway enrichment analyses, CRM197 may exert its anti-tumor effects by activating pathways such as the PI3K-AKT signaling pathway and the p53 signaling pathway.
Prediction of CRM197 functional targets and analysis of potential therapeutic mechanisms in arsenic-transformed lung cancer cells. (A) Chemical structure of CRM197. The molecular structure of CRM197 is shown. (B) Functional prediction of CRM197. SwissTargetPrediction analysis suggested potential functions of CRM197, including protease and surface antigen activities. (C) Venn diagram of predicted and upregulated protein targets. A total of 11 overlapping targets (MME, ERAP2, AKR1B1, FPR1, NTSR2, CTSD, PTPN1, SERPINE1, PTPN2, CYSLTR2, PPARA) were identified from the intersection of targets predicted by SwissTargetPrediction (102 targets), SuperPred (242 targets), and the 179 upregulated proteins in As-T cells. (D) List of 11 overlapping targets. The 11 overlapping targets are listed, which may represent potential therapeutic targets of CRM197 in arsenic-transformed lung cancer. (E) Protein–protein interaction (PPI) network analysis of the 11 overlapping targets. Key hub proteins in the PPI network were identified and analyzed. (F–G) KEGG pathway enrichment analysis of key hub proteins. Enriched pathways included PI3K-AKT signaling, p53 signaling, and others, suggesting that CRM197 may exert its anti-tumor effects through these pathways. (H) Western blot analysis of cell cycle-related proteins and PI3K/AKT signaling pathway. CRM197 treatment significantly downregulated the expression of CCND1, p-AKT, and AKT, indicating inhibition of the PI3K-AKT pathway, consistent with network pharmacology predictions.
Molecular docking simulates the docking of drugs with targets
The AlphaFold3 molecular docking software was utilized to simulate the binding of CRM197 target proteins to proteins associated with LSCC. The results indicated that CRM197 target proteins exhibited strong binding affinities with several disease-related proteins, including CTSD-SERPINE1, SERPINE1-PPARA, PPARA-AKR1B1, AKR1B1-PTPN1, PTPN1-PPARA, and PTPN1-PTPN2, thereby providing molecular-level evidence for the pharmacological effects of CRM(197) (Fig. 4A, B, C). According to the molecular docking results, the binding strength between proteins increases as the binding free energy decreases, with the PTPN1-PPARA complex demonstrating the lowest binding energy, indicating the most favorable docking conformation.
Molecular docking and molecular dynamics simulation analysis of CRM197 target proteins and their interactions with lung squamous cell carcinoma-related proteins. (A–C) Molecular docking results. CRM197target proteins (CTSD, SERPINE1, PPARA, AKR1B1, PTPN1, PTPN2) showed strong binding affinities with disease-related proteins, as demonstrated by their low binding free energies. The best docking conformation was observed between PTPN1 and PPARA, which exhibited the lowest binding energy. (D) Root mean square deviation (RMSD) analysis. The RMSD values of the PTPN1-PPARA complex stabilized after 50 ns, indicating a stable binding conformation. (E) Radius of gyration (Rg) analysis. The Rg curve stabilized after 20 ns, suggesting a tightly folded and stable complex structure. (F) Solvent accessible surface area (SASA) analysis. The SASA curve reached equilibrium after 50 ns, with an average value of 460 nm2, indicating stable solvent interactions. (G) Hydrogen bond (H-bond) analysis. The stable hydrogen bond patterns between PTPN1 and PPARA further confirmed the strong binding affinity of the complex. (H–I) Root mean square fluctuation (RMSF) analysis. The RMSF values indicated that the overall structure of the complex was stable, with residual flexibility observed in the protein regions 100–200. These results demonstrate the dynamic interactions and stability of CRM197 with its target proteins, providing molecular-level evidence for its pharmacological effects.
We utilized the GROMACS molecular dynamics simulation software to perform a binding simulation between PTPN1 and PPARA. The calculations yielded results for RMSD (Root Mean Square Deviation), RMSF (Root Mean Square Fluctuation), Rg (radius of gyration), SASA (solvent-accessible surface area), and hydrogen bonds (H-bonds). RMSD is employed to assess the relative stability of the binding system. The results presented in Fig. 4D indicate that the complex exhibits reduced fluctuations and tends to stabilize after 50 ns, suggesting a strong binding interaction between PTPN1 and PPARA. The RMSF values provide insight into the structural stability of the protein, atomic mobility, and residual flexibility during interactions. The data shown in Figs 4H and I reveal that the overall structure of the complex remains relatively stable, with two notable peaks in protein residues 100–200 exhibiting greater residual flexibility compared to other regions. The Rg (radius of gyration) can be used to characterize the surface compression or expansion trend of the binding system. The result in Fig. 4E shows that after a brief fluctuation from 0-20 ns, the radius of gyration curve is almost stable, indicating that the complex conformation is stable and tightly folded. SASA (solvent-accessible surface area) is used to calculate the surface area of molecules such as proteins in contact with the solvent and analyze the interaction with the solvent. The result in Fig. 4F shows that the SASA curve tends to be in equilibrium after 50 ns, with an average SASA value of 460 nm2. H-bond (hydrogen bond) represents the binding strength between the ligand and the protein. The result in Fig. 4G shows that the docked complex has a stable hydrogen-bond pattern.
The results indicate that molecular dynamics simulation analysis was conducted to study the dynamic interactions between CRM197 and disease targets, thereby verifying its stability.
CRM197 inhibited the tumor growth of As-T, NCI-H226 and PC-9 In vivo
To further investigate the effect of CRM197 on tumor growth in vivo, As-T cells, NCI-H226 cells, and PC-9 cells were injected subcutaneously into nude mice to establish a LSCC (LUSC) model in BALB/c mice. Seven days later, the mice were treated daily with 5 mg/kg CRM197, 5 mg/kg afatinib, or PBS for 10 consecutive days. As shown in the figures, CRM197 has a more significant inhibitory effect on As-T than afatinib, but its inhibitory effect on NCI-H226 and PC-9 is was not as good as afatinib (Figs. 5A, B, C). The results of hematoxylin and eosin (HE) staining demonstrated that CRM197 inhibited the malignant progression of tumors (Fig. 5D). In summary, these data suggest that the inhibition of cell proliferation induced by CRM197 is associated with the induction of cell cycle arrest and the blockade of the PI3K/AKT signaling pathway.
In vivo anti-tumor effects of CRM197 and its mechanisms in a lung squamous cell carcinoma (LUSC) mouse model. (A–C) Tumor growth inhibition by CRM197. As-T, H226, and PC-9 cells were subcutaneously injected into BALB/c mice to establish LUSC models. Mice were treated daily with 5 mg/g CRM197, 5 mg/g afatinib, or PBS for 10 days. CRM197 significantly inhibited tumor growth in As-T cells compared to the control and afatinib groups, as shown by reduced tumor volume. (D) HE staining of tumor tissues. HE staining results demonstrated that CRM197 suppressed tumor malignancy progression. These findings suggest that CRM197 inhibits tumor growth by inducing cell cycle arrest and blocking the PI3K/AKT signaling pathway.
Discussion
LSCC is associated with high mortality and limited targeted therapies 3. Chronic arsenic exposure is more likely to induce squamous cell carcinoma in the human, especially skin and lung cancer25. Studying the expression of protein levels during arsenic-induced cellular malignant transformation can help people identify signaling molecules that play a key role in Arsenic-induced- transformation process, providing a basis for early diagnosis and treatment targets of LSCC. In this study, we employed proteomic techniques to sequence the As-T cells and control B2B cells, identified differential gene expression, and conducted bioinformatics analysis to screen for proteins that exhibit changes in the early stages of lung cancer. These potential biomarkers may provide new targets and insights for the early diagnosis of lung cancer, thereby addressing the current challenges associated with early detection. Proteomics results of As-T and B2B showed 179 proteins including RRM2 and PRKDC overexpressed in As-T cells. Moreover, according to some reports, RRM2 and PRKDC are highly expressed in lung cancer and play important roles in the proliferation, prognosis, and drug resistance of lung cancer suggesting that they may play an important role in arsenic- induced malignant transformation of cells and serve as a prognostic marker and potential therapeutic target but further research is needed25.
Approximately 45% and 40% of patients with non-small cell lung cancer (NSCLC) are positive for epidermal growth factor receptor (EGFR) exon 19 deletions and exon 21 L858R mutations, respectively 26,27. These mutations are predictive of treatment benefit from small molecule EGFR tyrosine kinase inhibitors (TKIs) such as erlotinib, gefitinib, and afatinib, However, most patients develop resistance to these small-molecule EGFR TKIs after the first 8 to 16 months28. Lung squamous cell carcinoma is characterized by a low mutation rate of EGFR29, which often limits the efficacy of traditional EGFR-targeted therapies. In pursuit of alternative and effective treatment strategies, we focused on inhibiting HB-EGF using its specific inhibitor CRM197 because Arsenic activated EGFR through HB-EGF and more likely induce lung squamous cell carcinoma30.
CRM197 binds to HB-EGF with high affinity and blocks its interaction with receptors like EGFR and HER4, thereby suppressing HB-EGF-mediated signaling and inducing significant apoptosis of ovarian, breast, bladder, and gastric cancer cells harboring HB-EGF expression31. HB-EGF is highly expressed in EGFR-mutated lung adenocarcinoma cell lines PC14, RERF-LC-A1 and NCI-H1975 compared with lung adenocarcinoma cells without EGFR mutation. Therefore, CRM197 induces cell apoptosis by inhibiting HB-EGF and significantly suppresses the tumorigenic ability of lung adenocarcinoma cells with EGFR single or double mutations 28,32. In this study, we examined the antitumor effects of CRM197 on As-T, squamous carcinoma NCI-H226 cells without EGFR mutation and PC9 cells with EGFR mutations (ex 19 del + T790M of EGFR) to assess the validity of CRM197 as a therapeutic target for LSCCs. We selected Cetuximab and Afatinib of lung cancer drugs as comparative subjects, because Afatinib is a second-line treatment option in LSCC based on its survival advantage over erlotinib for treating LSCC26,27 and Cetuximab-based therapy is suitable for squamous cell of lung cancer with EGFR high copy number together with high EGFR protein expression according to the report28. The results showed that CRM197 inhibited tumor cell growth less potently than afatinib. Our results showed 10 μg/ml CRM197 has a better growth inhibitory effect on As-T cells, but not as good as the effect of Afatinib on NCI-H226 compared to 10 μ g/ml cetuximab and 5 μ g/ml afatinib subsequently confirmed by the results of tumorigenic experiments in vivo. The inhibitory effect of CRM197 on the growth of As-T, NCI-H226, and PC-9 is significantly better than that of cetuximab. In addition, the results of cell cycle analysis by flow cytometry showed that CRM197 inhibited transition from the S phase to the G2/M phase and induced apoptosis of As-T, NCI-H226 and PC-9 cells. CRM197 significantly inhibited the expressions of CCND1 which is a key regulator of cell cycle and the overexpression rate of CCND1 in LSCC is relatively high, about 30–60% which is one of the important molecular features of LSCC. CCND1 promotes tumor progression, and is an important prognostic marker and therapeutic target. The treatment strategy targeting the CCND1/CDK4/6 pathway provides new hope for patients with LSCC29,30. Our findings provide a theoretical basis for the development of CRM197 as a therapeutic drug for Arsenic-transformed cells and lung squamous cell carcinoma.
In addition, our results demonstrated that whether the expression of HB-EGF was suppressed by CRM197 or not, CRM197 significantly inhibited the growth and induced apoptosis of As-T, squamous carcinoma NCI-H226 cells without EGFR mutation and PC9 cells with EGFR mutations (ex 19 del + T790M of EGFR). This result indicated that CRM197 inhibited cell growth not only through the HB-EGF/EGFR pathway. We employed a comprehensive approach that combined network pharmacology, molecular docking and molecular dynamics simulations to thoroughly explore the mechanisms of arsenic-induced cells transformation, and CRM197 inhibiting tumor growth. We successfully constructed a target network for CRM197 in the treatment of arsenic-induced cell transformation using network pharmacology methods. 11 potential targets including AKR1B1, PTPN1, PPARA and SERPINE1 were predicted. These targets are significantly enriched in signaling pathways, including apoptosis and the PI3K-AKT pathway. These pathways play a critical role in processes such as cell proliferation, apoptosis and metabolism which are closely associated with the occurrence and progression of LSCC33,34. Especially the relationship between AKR1B1 (member B1 of the aldehyde ketone reductase family) and lung cancer is currently one of the research hotspots. In lung cancer, high expression of AKR1B1 is associated with poor prognosis and may promote lung cancer progression by regulating oxidative stress and inflammatory response35,36. In addition, PTPN1 is a protein tyrosine phosphatase involved in regulating cell signaling, metabolism, and growth. In lung cancer, high expression of PTPN1 is associated with poor prognosis and may promote lung cancer progression by regulating cell proliferation and apoptosis 37,38. The relationship between PPARA (peroxisome proliferator activated receptor alpha) and lung cancer is currently unclear, but previous studies have explored its role in cancer. There are indications that PPARA may affect the development of lung cancer by regulating metabolism and inflammation39,40. The relationship between SERPINE1 (plasminogen activator inhibitor-1, PAI-1) and lung cancer is currently another of the research hotspots. Multiple studies have shown that SERPINE1 is highly expressed in non-small cell lung cancer (NSCLC) and small cell lung cancer (SCLC), and is significantly associated with tumor staging, metastasis, and poor prognosis41,42. According to the reports and our prediction results, it is suggested that AKR1B1, PTPN1, PPARA and SERPINE1may play important role in Arsenic-induced transformation and CRM197 inhibited the growth of As-T and NCI-H226, but he mechanisms of AKR1B1, PTPN1, PPARA and SERPINE1 in lung cancer still need further research and their potential as a therapeutic target deserve attention.
In conclusion, we have established a foundation for future research focused on enhancing the diagnosis, treatment, and prevention of this lethal disease. Although certain achievements have been made in this study, relying solely on database technology has limitations and is not sufficiently comprehensive or in-depth. Future exploration that combines this technology with clinical practice is necessary.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Chaudhuri, M. R. Primary pulmonary cavitating carcinomas. Thorax 28(3), 354–366 (1973).
Travis, W. D. et al. The 2015 World Health Organization Classification of Lung Tumors: Impact of Genetic, Clinical and Radiologic Advances Since the 2004 Classification. J Thorac Oncol 10(9), 1243–1260 (2015).
Kwon, J. et al. USP13 drives lung squamous cell carcinoma by switching lung club cell lineage plasticity. Mol Cancer 22(1), 204 (2023).
Ono, K. et al. Clinicopathological and molecular characteristics of endometrial neuroendocrine carcinomas reveal preexisting endometrial carcinoma origin. Pathol Int 71(8), 491–499 (2021).
Marsden, C. G. et al. Mouse Embryonic Fibroblasts Isolated From Nthl1 D227Y Knockin Mice Exhibit Defective DNA Repair and Increased Genome Instability. DNA Repair (Amst) 109, 103247 (2022).
Pastan, I. et al. Immunotoxin therapy of cancer. Nat Rev Cancer 6(7), 559–565 (2006).
Qu, G., et al., PINK1/Parkin-Mediated Mitophagy Partially Protects against Inorganic Arsenic-Induced Hepatic Macrophage Polarization in Acute Arsenic-Exposed Mice. Molecules, 2022. 27(24).
Yang, W. et al. Nuclear PKM2 regulates β-catenin transactivation upon EGFR activation. Nature 480(7375), 118–122 (2011).
Lin, Q., et al., Effect and underlying mechanism of a photochemotherapy dual-function nanodrug delivery system for head and neck squamous cell carcinoma.
Park, S. et al. Inhibition of MAGEA2 regulates pluripotency, proliferation, apoptosis, and differentiation in mouse embryonic stem cells. J Cell Biochem 121(11), 4667–4679 (2020).
Duan, Z. L. et al. Wumei Wan attenuates angiogenesis and inflammation by modulating RAGE signaling pathway in IBD: Network pharmacology analysis and experimental evidence. Phytomedicine 111, 154658 (2023).
Giubellino, A. et al. Characterization of two mouse models of metastatic pheochromocytoma using bioluminescence imaging. Cancer Lett 316(1), 46–52 (2012).
Hirsch, F. R. et al. Lung cancer: Current therapies and new targeted treatments. Lancet 389(10066), 299–311 (2017).
He, J. et al. Chronic arsenic exposure and angiogenesis in human bronchial epithelial cells via the ROS/miR-199a-5p/HIF-1α/COX-2 pathway. Environ Health Perspect 122(3), 255–261 (2014).
Liu, X. et al. Histone deacetylase 3 expression correlates with vasculogenic mimicry through the phosphoinositide3-kinase / ERK-MMP-laminin5γ2 signaling pathway. Cancer Sci 106(7), 857–866 (2015).
Acheampong, F. et al. Estrone analogs as potential inhibitors targeting EGFR-MAPK pathway in non-small-cell lung cancer. Chem Biol Drug Des 101(6), 1356–1366 (2023).
Li, C. et al. Nuclear EGFR contributes to acquired resistance to cetuximab. Oncogene 28(43), 3801–3813 (2009).
Zhao, B., et al., Macrophage renewal modes affect acquired resistance to gefitinib in EGFR‑mutant lung cancer PC‑9 cells. Oncol Rep, 2023. 49(2).
Sequist, L. V. et al. Phase III Study of Afatinib or Cisplatin Plus Pemetrexed in Patients With Metastatic Lung Adenocarcinoma With EGFR Mutations. J Clin Oncol 41(16), 2869–2876 (2023).
Kutsuzawa, N. et al. Successful Treatment of a Patient with Lung Adenocarcinoma Harboring Compound EGFR Gene Mutations, G719X and S768I, with Afatinib. Tokai J Exp Clin Med 45(3), 113–116 (2020).
Vavalà, T. Role of afatinib in the treatment of advanced lung squamous cell carcinoma. Clin Pharmacol 9, 147–157 (2017).
Cobo, M. et al. Afatinib in patients with squamous cell carcinoma of the lung: Current context and the option of oral treatment. Med Clin (Barc) 146(Suppl 1), 25–29 (2016).
Kanehisa, M. et al. KEGG as a reference resource for gene and protein annotation. Nucleic Acids Res 44(D1), D457–D462 (2016).
Kanehisa, M. & Goto, S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res 28(1), 27–30 (2000).
Martinez, V. D. et al. Induction of human squamous cell-type carcinomas by arsenic. J Skin Cancer 2011, 454157 (2011).
Rosell, R. et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol 13(3), 239–246 (2012).
Sequist, L. V. et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 31(27), 3327–3334 (2013).
Yotsumoto, F. et al. HB-EGF Is a Promising Therapeutic Target for Lung Cancer with Secondary Mutation of EGFR(T790M). Anticancer Res 37(7), 3825–3831 (2017).
Cheung, A. H. et al. EGFR mutation exists in squamous cell lung carcinoma. Pathology 52(3), 323–328 (2020).
Wang, L. et al. HB-EGF Activates the EGFR/HIF-1α Pathway to Induce Proliferation of Arsenic-Transformed Cells and Tumor Growth. Front Oncol 10, 1019 (2020).
Mitamura, T. et al. Diphtheria toxin binds to the epidermal growth factor (EGF)-like domain of human heparin-binding EGF-like growth factor/diphtheria toxin receptor and inhibits specifically its mitogenic activity. J Biol Chem 270(3), 1015–1019 (1995).
Hsieh, C. H. et al. A targetable HB-EGF-CITED4 axis controls oncogenesis in lung cancer. Oncogene 36(21), 2946–2956 (2017).
Derman, B. A. et al. Treatment of advanced squamous cell carcinoma of the lung: A review. Transl Lung Cancer Res 4(5), 524–532 (2015).
Zhang, Q. & Wang, Y. MiR-210-3p targets CELF2 to facilitate progression of lung squamous carcinoma through PI3K/AKT pathway. Med Oncol 39(11), 161 (2022).
Li, Q. et al. Molecular profiling of human non-small cell lung cancer by single-cell RNA-seq. Genome Med 14(1), 87 (2022).
Kang, M. W. et al. AKR1B10 is associated with smoking and smoking-related non-small-cell lung cancer. J Int Med Res 39(1), 78–85 (2011).
Wang, C.C., et al., Novel Potential Therapeutic Targets of PTPN Families for Lung Cancer. J Pers Med, 2022. 12(12).
Kostrzewa, T. et al. Inhibitors of Protein Tyrosine Phosphatase PTP1B With Anticancer Potential. Anticancer Res 39(7), 3379–3384 (2019).
Wu, L. et al. PPARα ligand, AVE8134, and cyclooxygenase inhibitor therapy synergistically suppress lung cancer growth and metastasis. BMC Cancer 19(1), 1166 (2019).
Ye, G. et al. Aryl hydrocarbon receptor mediates benzo[a]pyrene-induced metabolic reprogramming in human lung epithelial BEAS-2B cells. Sci Total Environ 756, 144130 (2021).
Kong, H. J. et al. Crosstalk between YAP and TGFβ regulates SERPINE1 expression in mesenchymal lung cancer cells. Int J Oncol 58(1), 111–121 (2021).
Ou, J. et al. SERPINE1 and SERPINB7 as potential biomarkers for intravenous vitamin C treatment in non-small-cell lung cancer. Free Radic Biol Med 209(Pt 1), 96–107 (2023).
Acknowledgements
This work was supported by National Natural Science Foundation of China (82373314).
Author information
Authors and Affiliations
Contributions
Z.X.Y. Conception and design, Writing—Original Draft;S.S.Y.:Validation; T.J.Q.:Analysis and interpretation; Z.K.N.,Z.X.,M.J.,B.X.M.,S.H., S.D.M.,W.M.: Project Administration, Resources, Supervision, Final approval of the article. Project Administration, Resources, Supervision, Final approval of the article.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical approval
All animal studies were performed according to the guidelines established by the Research Animal Care Committee of Nanjing Medical University, China (Permit Number: IACUC-NJMU 1710015), and the study adhered to the guidelines set by this committee. Additionally, this study conforms to the ARRIVE guidelines (https://arriveguidelines.org) — all animal experiments were approved by the aforementioned Research Animal Care Committee of Nanjing Medical University (Permit Number: IACUC-NJMU 1710015) and conducted in compliance with institutional animal welfare policies.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, X., Song, S., Tang, J. et al. The inhibitory effect and targets of CRM197 on tumor growth in arsenic-transformed cells and lung cancer cells. Sci Rep 15, 40081 (2025). https://doi.org/10.1038/s41598-025-23832-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-23832-z