Abstract
Atrial electromechanical coupling time (AEMCT) can be used to evaluate atrial electrical remodeling and early structural remodeling. This study explores the predictive role of AEMCT in postoperative new-onset AF (POAF) after off-pump isolated coronary artery bypass grafting (OPCAB). A total of 116 patients who underwent OPCAB and left atrial diameter (LAD)<44 mm were analyzed. According to 7-day continuous telemetry and Holter monitoring after OPCAB, the patients were divided into POAF group and non- POAF group. Patients were divided into two groups according to whether new-onset POAF occurred, namely, POAF group (38, 32.7%) and non-POAF group (78, 67.3%). There was no significant difference in LAD between two group. Multivariate analysis found that P-ALA ( P wave on ECG to the starting point of A´wave on tissue Doppler imaging (TDI) spectrum at the left atrial lateral wall of the mitral annulus), TLA (AEMCT in the left atrium) and HbA1c (glycosylated hemoglobin) in POAF group were significantly higher than that in non-POAF group, that is, higher HbA1c, prolonged P-ALA and TLA were independent risk factors for POAF after OPCAB. P-ALA had the highest diagnostic predicting value. The AUC of HbA1c, P-ALA and TLA with Cut -off was 0.766, 95% CI: 0.67–0.86, P < 0.001. In OPCAB patients without significant LAD enlargement, when P-ALA ≥ 96. 50 ms, there is more than 90% probability of POAF. The combination of HbA1c, P-ALA and TLA has the highest predictive value of POAF. AEMCT measured with TDI has the advantages of low cost and high repeatability.
Clinical Trial Registry Registration Number: ChiCTR2200056127.
Similar content being viewed by others
Introduction
New-onset postoperative atrial fibrillation (POAF) is a common complication after cardiac surgery1,2,3. Among patients undergoing isolated coronary artery bypass grafting (CABG), the incidence of new-onset POAF is 20% to 40%4, and this rate increases to 40% to 50% for patients undergoing surgical aortic valve replacement5. POAF increases the risk of congestive heart failure, embolic events and prolonged intensive care6,7,8,9. Patients without a history of atrial fibrillation (AF) develop new-onset POAF after coronary artery bypass grafting, and their risk of stroke and death is significantly increased10,11,12,13. POAF is the highest postoperative complication in cardiac surgery4. Therefore, the establishment of POAF prediction model can identify high-risk patients with AF before surgery and take preventive strategies, which is very important for improving the prognosis and life quality of CABG patients14,15.
Atrial electromechanical coupling time (AEMCT) is the interval time between atrial electrical signal and atrial mechanical motion, which can be used to evaluate atrial electrical remodeling and early structural remodeling16. Migraine is associated with subclinical atrial conduction disturbances, as evidenced by elevated P-wave dispersion and atrial electromechanical delay17. The Echocardiographic Atrial Strain and conduction Evaluation (EASE) score offers noninvasive risk prediction in paroxysmal atrial fibrillation ablation18. Early on, AEMCT was measured by invasive electrophysiological studies. To reduce invasive procedures and improve patient compliance, echocardiographic tissue Doppler imaging (TDI) was introduced to measure AEMCT16,19,20. TDI derived AEMCT has advantages in predicting POAF and AF recurrence21. Left atrial size, P wave dispersion of ECG, left atrial wall strain22 and Doppler velocity of left atrial appendage23 are closely related to POAF. The purpose of this study is to investigate the correlation between AEMCT and new-onset POAF in patients undergoing off-pump coronary artery bypass grafting (OPCAB), as well as the predictive value of AEMCT for new-onset POAF.
Results
Analysis of clinical data (Table 1)
The enrolled patients are all unstable angina patients with a left ventricular ejection fraction of over 50%. All the data were collected before surgery, and data analysis was conducted on the results. The patient received treatments such as heart rate control, blood pressure control, lipid-lowering, and anticoagulation. The level of age and HbA1c, and the proportion of diabetes of POAF group were higher than those of non-POAF group, P < 0.05. There was no significant difference between the two groups in sex, hypertension, hyperlipidemia, smoking, drinking, classification of coronary artery stenosis, other blood biochemical indexes and preoperative medication, P > 0.05.
Preoperative ultrasound data (Table 2)
All the data were collected before surgery, and data analysis was conducted on the results
All the selected cases were patients with LAD < 44 mm, and there was no significant difference in LAD between POAF group and non-POAF group, P > 0.05. The Ei’ and Ai’ of POAF were significantly lower than those of non-POAF, P < 0.05. The comparison of Electromechanical Coupling Time of Two Groups of Patients was shown in Fig. 1A. The time of P-ALA and TLA of POAF were significantly prolonged than that of non-POAF, P < 0.05. There was no significant difference between POAF and non-POAF in LAD, Em/Am, LVEF, HR and PASP.
Analysis of intraoperative and postoperative observation indicators
There was no significant difference between the two groups in terms of operation duration, intraoperative blood loss, length of time in ICU, the use of IABP, postoperative infection rate, aspirin and low molecular weightheparin usage rate, and the number of bridging vessels, P > 0.05.
Characteristics of New-onset POAF
37 patients (37/38, 97.4%) in POAF group had rapid AF (the fastest heart rate was more than 100 bpm). Only one patient developed slow AF (the fastest heart rate was less than 100 bpm). Characteristics of POAF were shown in Table 3.
Multivariate logistics analysis (Table 4)
Because of the interference between diabetes history and HbA1c in multivariate regression analysis, continuous variable HbA1c was selected for regression analysis. Since TLA is a component of P-ALA, these two factors were modeled and analyzed separately to avoid interference between them when included in multivariate analysis. Found that the HbA1c level in the POAF group was significantly higher than that in the non POAF group, and both models showed statistical significance. In their respective models, P-ALA and TLA in POAF group were significantly longer than those in non-POAF group.
ROC curve analysis
Diagnostic predicting value of P-ALA and TLA were shown in Fig. 1B. Among them, P-ALA had the highest diagnostic predicting value, and the AUC of P-ALA was 0.709, 95%CI: 0.60–0.82, P < 0.001(Cut-off = 96.50ms, Sensitivity = 42.10%, Specificity = 92.3%,Youden index = 34.4%). The AUC of HbA1c was 0.668, 95%CI: 0.57–0.77, P = 0.003(Cut-off = 6.79%, Sensitivity = 47.40%, Specificity = 80.8%, Youden index = 28.2%). The AUC of TLA was 0.693, 95%CI: 0.60–0.79, P = 0.001(Cut-off = 17.50ms, Sensitivity = 76.32%, Specificity = 59.0%, Youden index = 35.32%). The AUC of P-ALA and TLA with Cut -off was 0.732, 95% CI: 0.63–0.84, P < 0.001. The combination of HbA1c, P-ALA, and TLA has the greatest value in predicting POAF. The AUC of HbA1c, P-ALA and TLA with Cut -off was 0.766, 95% CI: 0.67–0.86, P < 0.001. Other evaluation parameters for P-ALA, TLA and HbA1c are shown in Table 5.
Correlation analysis between AEMCT and HbA1c
We found that although AEMCT and HbA1c were independent risk factors for POAF in OPCAB patients with no significant enlargement of the left atrium, there was no obvious correlation between them, in Table 6.
Inter- and intra-observer variability of analysis
Intra- and inter-observer variability did not differ significantly in measuring
Ultrasound Data, P > 0.05. P-ALA and TLA measured with special intelligent Doppler spectrum analysis software, and the intra- and inter-observer variability did not differ significantly, P > 0.05. Intra- and inter-observer agreement was well above 0.90 (P < 0.001) for all measures.
Discussion
Electrical remodeling, structural remodeling, electromechanical remodeling and autonomic nerve remodeling complement each other and are closely related to AF occurrence and development24,25,26. The most used method to evaluate the degree of atrial remodeling is to measure LA size, volume and strain, but these indicators have limited role in predicting the AF risk. The LA obvious enlargement indicates that LA structural remodeling has occurred, and patients with LA anteroposterior diameter > 44 mm were more likely to develop AF27. This study focuses on OPCAB patients with no significant enlargement of the left atrium, in order to identify the risk factors for POAF in patients without significant structural remodeling.
AEMCT is the time interval between the action potential generated by the excitation of atrial myocytes and the mechanical movement of atrial tissue15,16. The disordered anisotropic propagation of atrial electrical activity is manifested by the prolongation of AEMCT, which increases the risk of atrial arrhythmias. At present, research has found that patients with POAF already have ion channel abnormalities before surgery, namely electrical remodeling28.29. The abnormal transmission of electrical signals to mechanical activity, including local conduction delay and non-uniformity, known as electro-mechanical remodeling, is a key factor in the formation and maintenance of the atrial fibrillation return pathway. This study selected OPCAB patients with no significant LA enlargement as the study subjects, explored the correlation between AEMCT and new-onset POAF in OPCAB patients.
P-ALA refers to the conduction time of the electrical signal P wave to the atrial motion at the annulus of the lateral wall of the mitral valve, and TLA refers to the electromechanical coupling conduction time (T) in the left atrium (TLA) was calculated, that is, TLA=(P-ALA)-(P-AIAS). We found that AEMCT has predictive value for POAF in OPCAB patients, significant prolongation of P-ALA and TLA could be used as independent predictors of POAF after OPCAB. Since TLA is a component of P-ALA, these two factors were modeled and analyzed separately to avoid interference between them when included in multivariate analysis. We found that patients with significantly prolonged P-ALA are more likely to develop POAF.
We also found that the increase of HbA1c is an independent risk factor for newly developed AF after OPCAB. This indicates that poor control of diabetes is an independent risk factor for POAF and the increase of HbA1c may be associated with atrial electrical remodeling. Electrical remodeling caused by diabetes has the characteristics of prolonged atrial conduction time, increased dispersion of atrial effective refractory period, and prolonged duration of action potential, which will increase the susceptibility to AF24. The combination of HbA1c, P-ALA, and TLA has the greatest value in predicting POAF. The AUC of HbA1c, P-ALA and TLA with Cut -off was 0.766, 95% CI: 0.67–0.86, P < 0.001. Atrial electrical remodeling is the early pathophysiological basis of atrial fibrillation. How to measure atrial electrical remodeling in patients has been paid attention to clinically, and AEMCT prolongation is one of the manifestations of atrial electrical remodeling. Measuring atrial electromechanical conduction can relate the atrial microelectrical environment to macroatrial motion.
Microenvironment disorder is one of the causes of POAF in patients. Our team found in previous research that preoperative oral administration of Berberine can effectively reduce the incidence of POAF30, which may be related to changes in gut microbiota. It indicates that the patient is more prone to POAF in a certain special state, where the threshold for atrial fibrillation occurrence is relatively low. The degree of increase in HbA1c can reflect the blood glucose control level of diabetes for three months. We found that elevated HbA1c is an independent risk factor for new-onset AF after OPCAB. A significant increase in HbA1c indicates that the patient faces a heavier blood glucose load, which may cause more severe atrial electromechanical remodeling. However, no significant correlation between AEMCT and HbA1c was found in this study. It indicates that there may be another mechanism for patients with higher HbA1c to develop POAF, and further research is needed.
Diabetes can lead to atrial structural remodeling, electromechanical remodeling, autonomic neuropathy, endothelial dysfunction, inflammation, activation of renin angiotensin system, etc.24,31,32. Diabetes is independently related to myocardial fibrosis33,34. AEMCT of type 2 diabetes patients is longer than that of healthy people35. The changes of myocardial structure, oxidative stress and inflammation slow down the conduction between electrical and mechanical activities. The reduction of inflammation and oxidative stress in diabetes patients and the improvement of blood sugar can improve atrial remodeling, which is conducive to reducing the incidence of AF in diabetes patients36. Therefore, it is necessary to strengthen the blood glucose management of perioperative patients to reduce the occurrence of POAF.It shows that diabetic patients are prone to POAF, which may be the combined effect of many factors. It is necessary to strengthen the blood glucose management of patients during perioperative period to reduce the occurrence of POAF.
The atrium consists of overlapping cardiomyocytes, which gather in the form of myocardial fibers to form the atrial wall. Sinoatrial node is in the RA. When the current is generated, it propagates in a non-uniform and anisotropic way, depolarizing the RA and the LA successively. Compared with the RA, the arrangement of myocytes in the LA is relatively irregular from a histological point of view37, and the current conduction in the left atrium is relatively more irregular. Electrical remodeling promotes the occurrence of AF by altering the expression and/or function of ion channel proteins. The longer AEMCT means the more uneven atrial transmission pulses, reflecting the degree of atrial remodeling38, and is significantly related to the prolongation of the maximum P wave duration, the increase of P wave dispersion and histopathological changes. AEMCT can be used as one of the clinical indicators of early atrial remodeling. If the patient’s AEMCT is found to be prolonged, it means that the patient has prolonged electromechanical conduction time of each wall of the atrium and increased conduction heterogeneity, which is prone to POAF. Therefore, it is necessary to strengthen personalized treatment for these patients in advance to avoid the occurrence of POAF.
TDI imaging technology utilizing Doppler principle can measure the mechanical motion of myocardial segments and cardiac structures. The AEMCT measurement derived from this can be used as a non-invasive evaluation index for atrial conduction heterogeneity39,40, and the electromechanical coupling time of the left atrial sidewall of the mitral annulus can be an important predictive indicator for identifying patients with paroxysmal AF16. We investigated risk factors for POAF in patients with OPCAB without significant left atrial enlargement and found that preoperative AEMCT of the left atrial wall at the lateral annulus of the mitral valve, namely P-ALA, could serve as an independent predictor of POAF after OPCAB.The measurement of AEMCT using echocardiography Doppler technology is a non-invasive method for predicting POAF and has clinical practicality.When P-ALA ≥ 96.50ms, the sensitivity and specificity of POAF after OPCAB were 42.10% and 92.30% respectively, and when TLA ≥ 17.50ms, the sensitivity and specificity of POAF after OPCAB were 76.30% and 59.00%, respectively. Among them, P-ALA had stronger predictive value for POAF patients after OPCAB, AUC was 0.709, 95% CI was 0.60–0.82, P < 0.001.
In univariate analysis of clinical data, we found that the newly diagnosed POAF in OPCAB patients was significantly correlated with age and diabetes (P = 0.010 and 0.017 respectively). In the multivariate analysis, we found that the increase of HbA1c is an independent risk factor for newly developed AF after OPCAB. In this group of cases, when HbA1c ≥ 6.79%, the sensitivity and specificity for diagnosing newly diagnosed AF after OPCAB were 47.40% and 80.80%, respectively. The reduction of inflammation and oxidative stress in diabetes patients and the improvement of blood sugar can improve atrial remodeling, which is conducive to reducing the incidence of AF in diabetes patients36. In patients with poor glycemic control, intensive glycemic control before surgery may reduce the incidence of POAF.
The incidence of POAF is high in both cardiac surgery and non-cardiac surgery, and preoperative measurement of AEMCT may have high clinical predictive value. In future studies, routine measurement of AEMCT needs to be carried out, grouped according to different etiologies, and then stratified by atrial size. Clinical trials need to be designed with POAF as one of the observation endpoints, in order to define the normal range of AEMCT in different patients and provide practical guidance for preoperative, intraoperative and postoperative treatment.
Limitations
The sensitivity of TLA, P-ALA, and HbA1c in predicting POAF was low in the results of this study. In future research designs, it is necessary to expand the sample size to further improve the predictive value and add indicators such as glomerular filtration rate to increase clinical practical value.
Conclusion
In OPCAB patients without significant LAD enlargement, when P-ALA ≥ 96. 50 ms, there is more than 90% probability of POAF. The combination of HbA1c, P-ALA and TLA has the highest predictive value of POAF. AEMCT measured with TDI has the advantages of low cost and high repeatability.
Materials and methods
Study design
This is a prospectively case-control study. The protocol was approved by the Ethics Committee of the General Hospital of Northern Theater Command, No. Y (2020) 055, and registered in the Chinese Clinical Trial Registry (registration number: ChiCTR2200056127, registration date 2022-02-01). Manuscripts reporting results of a clinical trial conform to CONSORT 2010 guidelines. Referring to our previous research21, POAF was defined as any atrial tachyarrhythmia lasting longer than 30 s within one week after surgery:, detected by any of the following modalities: 12-lead ECG, continuous telemetry or 7-day Holter monitoring. (Shanghai Yueguang Medical Technology Co., Ltd., China). The clinical trial is observational and prospective, and has obtained informed consent from patients. All the methods were in accordance with relevant guidelines and regulations.
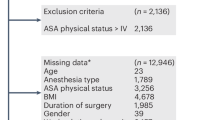
Study population
116 patients who underwent OPCAB between February 2022 and July 2022 were prospectively selected. Clinical data were collected for all consecutive patients, including preoperative medical history, complications, biochemical indicators, New York Heart Association (NYHA) functional classification, smoking and alcohol consumption, and coronary artery stenosis grade. Exclusion criteria: (1) previous AF or paroxysmal AF; (2) patients with moderate or severe mitral regurgitation caused by ischemia should be treated at the sametime; (3) left atrial anteroposterior diameter ≥ 44 mm; (4) patients with significantly reduced left ventricular ejection fraction (LVEF) ≤ 0.40, Simpson’s biplane; (5) patients with preoperative thyroid insufficiency, electrolyte disorder and chronic obstructive pulmonary disease; (6) long-term Holter monitoring duration ≤ 5 days; (7) postoperative wound infection or pericardial infection; (8) patient-related data were missing or died after operation.The study flow chart is provided in Fig. 2.
Measurement
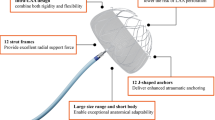
All patients were examined by echocardiography with Philips iE33 and 5 − 1 MHz transducer within 2 days before operation. The measurement and calculation of cardiac ultrasound are recommended according to the guidelines of the American Society of Echocardiography41. The interval time from the starting point of P wave on ECG to the starting point of A´ wave on TDI spectrum was measured successively, and the P- A of atrium was obtained (As shown in Fig. 3A. Pulse-wave tissue Doppler imaging (PW-TDI) synchronously connected ECG was used to measure the early diastolic, late diastolic, and systolic peak velocities at the lateral wall of the mitral annulus (Em´, Am ´ and Sm´), the interatrial septal annulus (Ei´, Ai´ and Si´), and the lateral wall of the tricuspid annulus (Et´, At´ and St´) in the Four-chamber view (As shown in Fig. 3B). The AEMCT were measured at the left atrial lateral wall of the mitral annulus (P-ALA), the interatrial septal annulus (P-AIAS), the right atrial lateral wall of the tricuspid annulus (P-ARA), respectively. And, the electromechanical coupling conduction time (T) in the left atrium (TLA) and the right atrium (TRA) was calculated, that is, TLA=(P-ALA)-(P-AIAS), TRA=(P-AIAS)-(P-ARA). Two sonographers measured and averaged each Doppler spectrum image three times every other day in a single blind state.
By measuring the interval from the start of the P wave in the electrocardiogram to the start of the A´ wave in the TDI spectrum, the electromechanical coupling time can be obtained (A). The three arrows from right to left respectively represent the positions of the lateral wall of the mitral annulus, the interatrial septal annulus, and the lateral wall of the tricuspid annulus in the Four-chamber view (B).
Surgery
All operations were performed by the same cardiac anesthesiologist and surgical team. Endotracheal intubation with combined intravenous anesthesia, median sternotomy, off-pump coronary artery bypass grafting, the descending branch before internal mammary artery anastomosis and the great saphenous vein anastomosis with other vessels were preferred.
Statistical power consideration
Ana priori power calculation was not conducted prior to patient enrollment. However, a post-hoc power analysis was performed upon study completion to assess the robustness of the statistical comparisons. Given the final group sizes (n = 38 and n = 78), an observed mean difference of 13.0 (Previous studies reported that patients with or without POAF had atrial electromechanical coupling times of 75 ms and 62 ms, respectively), and a common standard deviation of 23.0, the achieved statistical power was calculated to be 80.9% for a two-sided two-sample t-test at a significance level (alpha) of 0.05. This indicates that the study possessed sufficient sensitivity to detect the reported inter-group difference.
Statistical analysis
Patients were divided into two groups according to whether new-onset POAF occurred, namely, POAF group (38, 32.7%) and non-POAF group (78, 67.3%). Quantitative variables, which were in the normal distribution, were reported as mean and standard deviation analyzed by T-test, or median and quartiles analyzed by Mann - Whitney U test, to compare the difference between groups. Qualitative variables were reported by number (proportion) and analyzed by Chi-square test or Fisher’s exact test between groups. Multivariate logistic regression was used to analyze the variables with P < 0.05. ROC curves were used to evaluate the predictive/classification performance ability of the significant statistical factors. Spearman’s correlations analysis were used to analyze the correlation between AEMCT and HbA1c. Intraclass correlation coefficients to evaluate intra- and inter-observer agreement of the measured variables. All data were analyzed by SPSS 26. P < 0.05 was considered to be statistically significant.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Caldonazo, T. et al. Atrial fibrillation after cardiac surgery: A systematic review and meta-analysis. J. Thorac. Cardiovasc. Surg. 165, 94–103e124 (2023).
Shah, S., Chahil, V., Battisha, A., Haq, S. & Kalra, D. K. Postoperative Atrial Fibrillation: A Review, Biomedicines, 12 (2024).
Kongpakwattana, K., Dilokthornsakul, P., Dhippayom, T. & Chaiyakunapruk, N. Clinical and economic burden of postsurgical complications of high-risk surgeries: a cohort study in Thailand. J. Med. Econ. 23, 1046–1052 (2020).
Bessissow, A., Khan, J., Devereaux, P. J., Alvarez-Garcia, J. & Alonso-Coello, P. Postoperative atrial fibrillation in non-cardiac and cardiac surgery: an overview. J. Thromb. Haemostasis: JTH. 13 (Suppl 1), S304–312 (2015).
Indja, B., Woldendorp, K., Vallely, M. P. & Grieve, S. M. New onset atrial fibrillation following transcatheter and surgical aortic valve replacement: A systematic review and Meta-Analysis. Heart Lung Circ. 29, 1542–1553 (2020).
Sihombing, R. S., Muhadi, M., Mansjoer, A. & Rinaldi, I. The influence of New-Onset atrial fibrillation after coronary artery bypass grafting on Three-Year survival. Acta Med. Indones. 52, 125–130 (2020).
Goyal, P. et al. Post-operative atrial fibrillation and risk of heart failure hospitalization. Eur. Heart J. 43 (31), 2971–2980 (2022).
Westerman, S. & Wenger, N. Gender differences in atrial fibrillation: A review of Epidemiology, Management, and outcomes. Curr. Cardiol. Rev. 15, 136–144 (2019).
Schnabel, R. B. et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham heart study: a cohort study. Lancet (London England). 386, 154–162 (2015).
Lin, M. H. et al. Perioperative/Postoperative atrial fibrillation and risk of subsequent stroke and/or mortality. Stroke 50, 1364–1371 (2019).
Yao, X. et al. Association of surgical left atrial appendage occlusion with subsequent stroke and mortality among patients undergoing cardiac surgery. Jama 319, 2116–2126 (2018).
Min, J. J. et al. Does the type of anesthetic technique affect In-Hospital and One-Year outcomes after Off-Pump coronary arterial bypass surgery? PloS One. 11, e0152060 (2016).
Conen, D. et al. New-Onset perioperative atrial fibrillation after coronary artery bypass grafting and Long-Term risk of adverse events: an analysis from the CORONARY trial. J. Am. Heart Association. 10, e020426 (2021).
Zhang, Y. et al. E/Em’and E/(Em’ × Sm’) in tissue doppler imaging for the evaluation of heart failure after coronary artery bypass grafting [J]. Clin. J. Med. Offic. 49 (08), 844–847 (2021).
Zhang, X. et al. Evaluation of P wave dispersion and tissue doppler imaging for predicting paroxysmal atrial fibrillation in patients with hypertension. Heart Surg. Forum. 21, E054–e058 (2018).
Akamatsu, K. et al. Usefulness of tissue Doppler-derived atrial electromechanical delay for identifying patients with paroxysmal atrial fibrillation. Cardiovasc. Ultrasound. 18, 22 (2020).
Sarıkaya, C., Salkın, F. Ö. & Sarıkaya, C. P-Wave dispersion and atrial conduction abnormalities in migraine: implications for cardiovascular risk. Acta Neurol Belg. (2025). https://doi.org/10.1007/s13760-025-02876-y. Epub ahead of print. PMID: 40856982.
Cacciapuoti, F. et al. Left atrial mechanics and remodeling in paroxysmal atrial fibrillation: introducing the EASE score for Pre-Ablation risk prediction. Med. Sci. (Basel). 13 (3), 131. https://doi.org/10.3390/medsci13030131 (2025). PMID: 40843753; PMCID: PMC12372132.
Yuasa, T. & Imoto, Y. Usefulness of tissue doppler Imaging-Derived atrial conduction time for prediction of atrial fibrillation. Circulation Journal: Official J. Japanese Circulation Soc. 80, 58–59 (2016).
Dons, M. et al. Systolic and diastolic function by tissue doppler imaging predicts mortality in patients with atrial fibrillation. J. Atr. Fibrillation. 8, 1241 (2015).
Ari, H. et al. Predictive value of atrial electromechanical delay for atrial fibrillation recurrence. Cardiol. J. 20, 639–647 (2013).
Sánchez, F. J., Pueyo, E. & Diez, E. R. Strain echocardiography to predict postoperative atrial fibrillation. Int. J. Mol. Sci., 25(23), 1355 (2022).
Sarin, K. et al. Relationship between perioperative left atrial appendage doppler velocity estimates and new-onset atrial fibrillation in patients undergoing coronary artery bypass graft surgery with cardiopulmonary bypass. Ann. Card. Anaesth. 20, 403–407 (2017).
Wang, A., Green, J. B., Halperin, J. L. & Piccini, J. P. Atrial fibrillation and diabetes mellitus: JACC review topic of the week. J. Am. Coll. Cardiol. 74(8), 1107–1115 (2019).
Yue, F., Jin, Y. & Wang, H. Diagnostic characteristics of atrial functional atrioventricular valve regurgitation [J]. Chin. J. Cardiovasc. Med. 18 (12), 1130–1133 (2020).
GuoQ., LiuX. & ShiY. Mechano-electric feedback and atrial fibrillation. Sheng Wuyi Xue gong. Cheng Xue Za zhi = J. Biomedical Eng. = Shengwu Yixue Gongchengxue Zazhi. 33, 801–805 (2016).
Menichelli, D. et al. Atrial fibrillation pattern, left atrial diameter and risk of cardiovascular events and mortality. A prospective multicenter cohort study. Int. J. Clin. Pract. 75, e13771 (2021).
Heijman, J. et al. Atrial myocyte NLRP3/CaMKII nexus forms a substrate for postoperative atrial fibrillation. Circ. Res. 127 (8), 1036–1055 (2020).
van Schie, M. S. et al. Characterization of pre-existing arrhythmogenic substrate associated with de Novo early and late postoperative atrial fibrillation. Int. J. Cardiol. 363, 71–79 (2022).
Zhang, J. et al. Preventive effect of Berberine on postoperative atrial fibrillation. Circ. Arrhythm. Electrophysiol. 15 (10), e011160 (2022).
Şerban, R. C. & Scridon, A. Data linking diabetes mellitus and atrial Fibrillation-How strong is the evidence? From epidemiology and pathophysiology to therapeutic implications. Can. J. Cardiol. 34, 1492–1502 (2018).
Prídavková, D. et al. Type 2 Diabetes, Atrial Fibrillation, and Direct Oral Anticoagulation, Journal of diabetes research, 5158308. (2019).
Russo, I. & Frangogiannis, N. G. Diabetes-associated cardiac fibrosis: cellular effectors, molecular mechanisms and therapeutic opportunities. J. Mol. Cell. Cardiol. 90, 84–93 (2016).
GrangerC.B. & MahaffeyK.W. Preventing atrial fibrillation with treatments for diabetes mellitus. Circulation 141, 1235–1237 (2020).
Demir, K. et al. Assessment of atrial electromechanical delay and P-wave dispersion inpatients with type 2 diabetes mellitus. J. Cardiol. 67, 378–383 (2016).
ZelnikerT.A. et al. Effect of Dapagliflozin on atrial fibrillation in patients with type 2 diabetes mellitus: insights from the DECLARE- TIMI 58 trial. Circulation 141, 1227–1234 (2020).
Hari, K. J., Nguyen, T. P. & Soliman, E. Z. Relationship between P-wave duration and the risk of atrial fibrillation. Expert Rev. Cardiovasc. Ther. 16, 837–843 (2018).
Maffè, S. et al. Prognostic value of total atrial conduction time measured with tissue doppler imaging to predict the maintenance of sinus rhythm after external electrical cardioversion of persistent atrial fibrillation. Echocardiography (Mount Kisco N Y). 32, 420–427 (2015).
Rago, A. et al. The role of the atrial electromechanical delay in predicting atrial fibrillation in beta- thalassemia major patients. J. Interventional Cardiac Electrophysiology: Int. J. Arrhythm. Pacing. 48, 147–157 (2017).
Müller, P. et al. Den Uijl, Echocardiography-derived total atrial conduction time (PA-TDI duration): risk stratification and guidance in atrial fibrillation management. Clin. Res. Cardiol. 110, 1734–1742 (2021).
Nishimura, R. A. & Carabello, B. Operationalizing the 2014 ACC/AHA guidelines for valvular heart disease: A guide for clinicians. J. Am. Coll. Cardiol. 67, 2289–2294 (2016).
Acknowledgements
The authors thank Yachuan Pu and Yuji Zhang for assistance with analysis of Long Range Dynamic Electrocardiogram. Two anonymous reviewers provided helpful and constructive comments that improved the manuscript substantially.
Funding
This study was supported by the National Natural Science Foundation of China (No.81771833). Natural Science Foundation of Liaoning Province, 2024JH2/102,600,300.
Author information
Authors and Affiliations
Contributions
Yan Jin proposed the project design, experimental methods, and participated in the writing, review and revision of the article. Fengjie Yue wrote of the original draft and conducted the experiments. Yong Zhang participated in the review and revision of the article. Fangran Xin conducted statistical analysis on the experiment. Yang Zhao, Yuji Zhang and Huishan Wang conducted the experiments. All authors contributed to the article and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The Ethics Number of General Hospital of Northern Theater Command: No. Y (2020)055.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, Y., Yue, F., Zhang, Y. et al. Case-control study on atrial electromechanical coupling time in patients with new-onset postoperative atrial fibrillation. Sci Rep 15, 40479 (2025). https://doi.org/10.1038/s41598-025-24316-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-24316-w