Abstract
Complete atrioventricular block (CAVB) is a largely intractable disease that leads to severe bradyarrhythmia. The only treatment is the implantation of a pacemaker device. Left untreated, CAVB patients experience QT prolongation and ventricular overload, increasing susceptibility to cardiac remodeling and heart failure, as well as potentially lethal tachyarrhythmias. Animal models of CAVB offer a direct avenue to investigate the disease and potential disease-modifying therapies. However, existing models have limitations due to phenotype instability and high attrition rate. We aimed to create an improved method for disease model creation and report beating rate and variability analysis of the model. We report a modified surgical model of CAVB in rats by adapting a clinical radiofrequency energy generator to ablate the atrioventricular node region of the rat heart. Compared to previous ablation methods that utilize sharp needle entry into the AV node (AVN) region, the modified method resulted in a significantly higher success rate with a lower attrition rate. The rat model of CAVB showed stable conduction block for at least four weeks after model creation, supporting their suitability as a preclinical model of severe bradyarrhythmia due to AV conduction block. Models showed severe beat-to-beat variability with decreased overall autonomic innervation. We present a rodent model of a complete and stable AV block, which enhances the rigor and reproducibility of the disease model and downstream applications.
Similar content being viewed by others
Introduction
Atrioventricular block, also referred to as heart block, is a defect in the cardiac conduction system and results in abnormally slow heart rate, bradyarrhythmia. Congenital heart block is a rare disease, occurring in one in every 20,000 live births1. Surgical repair of structural abnormalities can also create iatrogenic cardiac conduction defects such as complete atrioventricular block (CAVB). A multicenter study reported that the double switch operation, tricuspid valve replacement, mitral valve replacement, and atrial switch surgery all have > 5% occurrence of iatrogenic CAVB or second-degree block2. In adult patients without congenital abnormalities, CAVB can result from coronary ischemia and acute myocardial infarction3. Left untreated, CAVB patients can experience QT prolongation, which increases susceptibility to potentially fatal ventricular arrhythmias such as Torsades de Pointes4,5,6. Due to the life-threatening nature of the disease, symptomatic bradycardia is treated with implantation of a pacemaker.
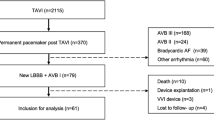
Animal models of CAVB offer opportunities to understand disease prognosis and to develop therapeutic strategies alternative to current device-dependent cardiac pacing7. We and others have developed porcine, ovine, and canine models of CAVB using catheter-based ablation of the atrioventricular node7,8,9,10,11. However, the need for clinical cardiac electrophysiology instrumentation and trained cardiac electrophysiologists limit their widespread use in these larger animal subjects. Transgenic mouse models of CAVB have been reported5,12,13,14, but phenotypic penetrance and longitudinal stability of the disease phenotype are variable. We have previously described a surgical model of CAVB in rats by sharp needle penetration of the AV node (AVN) region, followed by delivery of electrical current toward the interatrial septum near the aortic root for ablation of the AVN15. Although the model created stable and chronic CAVB in surviving rats, the attrition rate was high due to tissue perforation at the sharp needle electrode. In this study, we present a modified surgical model of CAVB in rats by epicardial application of radiofrequency ablation energy at the AVN area.
In addition, we sought to understand the beating rate and heart rate variability (HRV) parameters of this novel rodent model of CAVB. Long-term heart rate variability of CAVB patients is not widely studied due to the need for immediate pacemaker implantation. One study reported that the time-domain HRV parameters standard deviation of normal-to-normal intervals (SDNN), root mean square of successive differences (RMSSD), and the percentage of successive NN intervals differing by more than 50 ms (pNN50) were significantly reduced in patients with varying degrees of heart block compared to controls. It is also known that the sinoatrial node (SAN) is well-innervated with both sympathetic and parasympathetic arms16,17,18. We sought to understand comparative differences in the autonomic control of the junction escape rhythm from His bundle region upon AVN ablation by analyzing the heart rate variability of the sinus rhythm (SR) and the junction escape rhythm.
Materials and methods
Thoracotomy procedure to reach AVN ablation target
Female Sprague-Dawley rats (n = 50; Charles River Laboratories CD 001, aged 3–8 months) were sedated in an induction chamber using 5% isoflurane for 5 min, then subsequently intubated with an endotracheal tube consisting of an intravenous 14 G, 2-inch catheter. Following intubation, the animals were ventilated at 2% isoflurane and 2 L/min oxygen, with a 2.5mL tidal volume and 80 breaths per minute. A 3 cm area was shaved across the width of the subject’s lower back to provide a surface for the ground electrode return pad of the ablation system. The animals were administered 1.2 mg/kg buprenorphine polymer subcutaneously, 3 mg/kg meloxicam intramuscular, 1 mL saline intraperitoneally, and 1mL of 1 mg/kg lidocaine subcutaneously along the skin incision line prior to the first incision. Thoracic access was gained using a right-sided thoracotomy of the third intercostal space (Fig. 1A, Supplementary Video 1). For direct access to the heart, the lungs were covered with sterile gauze and the thymus was positioned away from the heart using the upper arm of a rib spreader. The pericardial sac was carefully dissected with forceps to expose the epicardium (Supplementary Video 2).
Clear illustration of the surgical procedure. (A) Diagram showing the surgical profile of the rodent during thoracotomy and ablation ((A,B) produced using Biorender). (B) Cartoon depicting the fat pad ablation target (RAA = right atrial appendage, RV = right ventricle). (C) In-vivo image of the fat pad (CTA = cotton-tipped applicator). (D) The radio-frequency ablation system with arrows indicating the flow of energy. (E) Epicardial ablation tip consisting of a 12-gauge copper wire and saline irrigation sheath. (F) Configuration from Medtronic ablation catheter to 12-gauge copper wire for the epicardial ablation electrode. (G) Diagram for new epicardial ablation method.
Subepicardial CAVB procedure for direct comparison
To directly compare the efficacy of our new method to our current method for creating CAVB in rat hearts15, animals were divided into epicardial (n = 26) and subepicardial (n = 24) groups and underwent identical surgical procedures except for the method of AVN ablation. Our previously established subepicardial ablation technique is performed by advancing the distal tip of a sharp needle into the AVN region by 2–3 mm (Supplementary 1 A-B) and passing electrical power through the proximal tip of the needle. RF energy was delivered at or less than 2 W for 30 s with a Bovie Aaron 950 High Frequency Desiccator as described previously15. Additional rounds of energy were delivered until CAVB confirmation. At higher than 2 W of energy, the incidence of significant bleeding was high due to myocardial tissue perforation around the subepicardial tip of the needle.
Telemeter implantation and recording
For continuous electrocardiogram recording (n = 5), model CTA-F40 telemeters (Data Sciences International™) were implanted into the abdominal cavity of the Sprague Dawley female rats at least 2 weeks before CAVB generation. The single lead biopotential telemeter wires were implanted in a lead II configuration. Animals were housed atop RPC-1 receiver pads (Data Sciences International™) in the Johns Hopkins University animal facility. Continuous electrocardiogram collection was conducted using the Physiotel Matrix 2.0 (Data Sciences International) communicator and Ponemah software. Data acquisition was performed using a 1 Hz sampling rate.
Autonomic nervous system Blockade
Atropine, a cholinergic muscarinic antagonist, and propranolol, a beta-adrenergic blocker, were administered to the animals. Thirty milligrams of powdered compounds were diluted in 10 mL of DPBS. 3 mg/kg of either or both drugs were administered to conscious subjects using intraperitoneal injections.
Electrocardiogram and heart rate variability analysis
Electrocardiograms were analyzed using the Ponemah electrocardiogram analysis module. Unless otherwise stated, ventricular beating rate analysis was performed using 1-minute logging intervals. Signal thresholds were adjusted between 0.1 mV to 0.3 mV on the low filter and 10 mV on the high filter to eliminate detection error due to poor signal. Heart rate variability was determined using the Variability Analysis module in LabChart 8 from ADInstruments. For frequency domain analysis, the very low-frequency lower and upper limits were set to 0.05 Hz and 0.25 Hz, respectively; low-frequency lower and upper limits were set to 0.25 Hz and 1.0 Hz, respectively; high-frequency lower and upper limits were set to 1 Hz and 3 Hz, respectively. The standard deviation of RR intervals (SDRR) was chosen in addition to SDNN due to the high occurrence of irregular beating patterns observed in CAVB models.
Animal housing
All subjects were housed in the Johns Hopkins University animal facilities and underwent 12-hour sleep-wake cycles. Subjects were transferred to the surgical station on the day of the procedure and immediately returned to the animal facility the same day upon completion. Subjects were housed in isolation for 7 days after telemeter implantation and 7 days after CAVB creation. After the 7-day recovery period, subjects were cohoused with a weight, sex, and species-matched partner.
Statement of ethics
This study was conducted under a protocol approved by the Johns Hopkins University Animal Care and Use Committee (ACUC) for the principal investigator, Dr. Hee Cheol Cho. All experiments in this study were conducted according to the approved protocol and all other guidelines and regulations laid out by the Johns Hopkins University ACUC. The authors complied with the ARRIVE Essential 10 guidelines.
Results
Creation of CAVB through epicardial ablation of the AVN
Upon right-sided thoracotomy (Supplementary Video 1), the fat pad at the atrioventricular groove was exposed by gently sliding the right atrial appendage (RAA) to the lateral right with a sterile cotton-tipped applicator (CTA) (Fig. 1A-C). While manipulating the RAA with one hand, the tip of a modified ablation wire was advanced to the epicardial fat pad with the other hand (Fig. 1B-C, Supplementary Vid. 3). The modified epicardial ablation apparatus consists of an insulated 12-gauge, 2.05 mm diameter copper wire connected to the radiofrequency (RF) power pin of a Medtronic ATAKR II catheter cable (Fig. 1D-F). RF energy was delivered to the epicardial surface for 15 s at 10 W with continuous saline irrigation (Fig. 1G). The RF delivery was administered using a foot pedal, allowing freedom of the surgeon’s hands to irrigate the ablation site via a 10mL syringe with saline attached to the irrigation catheter. Additional RF energy was delivered until CAVB was achieved (n = 26). Before each RF energy delivery, real-time surface ECG was examined for a minimum of one minute to confirm the creation and stability of CAVB. RF energy was increased up to 15 W if successful CAVB was not achieved after 3 ablation attempts at 10 W. No audible steam pops were observed during any of the ablations. Successful CAVB was determined by the complete dissociation of P waves from QRS complexes on surface ECG recordings. Additionally, the contractions of the ventricles and right atrium were observed while the chest cavity remained exposed to further confirm the CAVB. ECG recordings were monitored for 5 min before closing the chest cavity to ensure that the CAVB was permanent. Furthermore, 1-week and 4-week follow-up ECG recordings confirmed the longevity of the CAVB. Impedance for the novel epicardial ablation method averaged 185 ± 22 Ω. Compared with the previously established subepicardial ablation approach, the epicardial CAVB method required significantly greater average power (12.2 ± 0.4 W vs. 2.2 ± 0.1 W) but a significantly shorter total ablation time (81 ± 10 s vs. 96 ± 12 s) (Table 1).
Altered beating patterns of epicardial-ablated CAVB animals
To better understand the nature of the disease model, female subjects were studied with continuous ECG telemetry for two weeks before (n = 5) and after CAVB creation (n = 4), and once weekly, surface ECG recordings under 2% isoflurane were performed for four weeks after CAVB creation (Fig. 2A). CAVB was observed in all surviving animals at day 0, 7 and 28 post-op, indicating the disease model was stable (Fig. 2B-D; Table 1). We observed a polymorphic pattern of ventricular beats, including a dominant escape rhythm for an extended period (Fig. 2D), abrupt changes in QRS morphology and/or polarity suggesting competing foci of escape rhythm (Fig. 2E), irregularly occurring premature ventricular complexes (Fig. 2F), and highly irregular beat-to-beat intervals (Fig. 2G).
Disease model viability. (a) The study design indicates two weeks of ECG recordings before and after the CAVB model creation. ECG traces during pre-op (b), immediately post CAVB-ablation (c), and 28 days after model creation (d). Arrhythmias often appear on ECG as competing loci of escape rhythms (e), premature escape beats (f), and irregular escape rhythms (g). Blue-shaded areas identify the arrhythmia of interest.
Analysis of the 24-hour mean heart rates collected from telemetry demonstrates a significantly slow escape rhythm in CAVB animals (n = 4) compared to the animals’ sinus rhythm prior to CAVB (n = 5; Fig. 3A). The CAVB animals showed an initial increase in daily heart rate, rising from 112 ± 20 bpm at day 1 to 158 ± 14 bpm at day 3 (Fig. 3A). At day 14 after the ablation surgery, the CAVB animals’ mean heart rate was 131 ± 3 bpm compared to their sinus rhythm of 354 ± 12 bpm on the day before CAVB, a > 60% reduction in heart rate (Fig. 3A). Five-minute mean heart rates of sinus rhythm animals from day − 6 through day − 1 prior to CAVB exhibit daily fluctuations on average of 70 bpm, with a daily maximum of 405 ± 33 bpm and a daily minimum of 335 ± 27 bpm (Fig. 3B). These daily fluctuations are significantly increased when compared to these same animals under CAVB, whose 5-minute mean ventricular rates from day 9 through day 14 post-CAVB showed average daily fluctuations of 27 bpm, with a daily maximum of 151 ± 13 bpm and a daily minimum of 124 ± 12 bpm (Fig. 3C).
CAVB model beating rate trends. (a) Continuous beating rate averages 14 days before and after CAVB model creation using DSI telemetry, with standard deviation error bars (n = 5 SR; n = 4 CAVB). (b) Daily 5-minute beating rate averages for sinus rhythm for animals the 5 days leading up to CAVB creation and (c) CAVB animals 9–14 days post model creation. Note: Day 0 is the day of CAVB creation. The shaded segments (b,c) illustrate the 12-hour dark period, and the light segments represent the 12-hour light period in the animal facility. The dark line is the 5-minute heart rate average, and the blue lines represent their standard deviations.
Epicardial ablation significantly improves the long-term survival of CAVB animals
We compared the survival rates of CAVB animals created by epicardial ablation to that of the subepicardial needle electrode ablation technique15. For this study, female rats were weight-matched and randomly assigned to either surgical procedure with no difference in their heart rate before surgery (Table 1). Of the animals that underwent the subepicardial CAVB surgery, only 38% (n = 9 of 24) survived at 24 h post-op, which further decreased to 25% (n = 6) at 4 weeks (Fig. 4; Table 1). In contrast, 88% (n = 23 of 26) of the animals that underwent epicardial CAVB surgery survived 24 h and 77% (n = 20) survived to 4 weeks post-op (Fig. 4; Table 1). The significant improvement in the survival rate of epicardial ablation appears to correlate with minimizing incidences of severe blood loss (Table 1), which was significantly lower with the epicardial ablation method. Most deaths occurred during the first 7 days post-op (Fig. 4), suggesting that the CAVB animals could adapt to severe bradyarrhythmia if they survive the first week after the ablation surgery. There were no significant differences in the mean escape rhythm between the two CAVB models at days 0, 7, or 28 post-CAVB (Table 1), suggesting that the degree of AVN ablation and subsequent survival of slow pacemaker cells in the His bundle region was comparable between the two different methods.
Survivability of CAVB procedures. Kaplan-Meier curve comparing survival trends of CAVB models created using epicardial ablations and subepicardial ablations. A statistical difference between the Kaplan–Meier survival curves was evaluated using the log-rank (Mantel–Cox) test, which yielded p < 0.001.
Our previous study with subepicardial AVN ablation found that female rats survived the CAVB procedure much better than males15. For this study, we also attempted to perform our new epicardial CAVB procedure on male rats. Of the male animals that underwent the subepicardial CAVB surgery (n = 15), 67% (n = 10) survived at 24 h post-op, which further decreased to 33% (n = 5) at 2 weeks (Supplementary Fig. 3). When compared to the female rats that underwent the same procedure, the male rats experience a significantly decreased rate of long-term survival (Supplementary Table 1). Due to this high attrition rate in males, we decided to only use female rats for the additional studies that were performed in this study.
CAVB models exhibit altered heart rate variability
We examined heart rate variability parameters in female animals under normal sinus rhythm (n = 5) and after CAVB created with epicardial ablations (n = 4) by looking at 1-hour daytime intervals (light), from 12 pm to 1 pm and at 1-hour nighttime intervals (dark), from 12 am to 1 am. As expected with severe bradycardia, average daily RR intervals were significantly higher in CAVB animals than in wild-type animals at 461 ± 16 vs. 161 ± 4 ms, respectively (Fig. 5A; p < 0.001). RMSSD is generally used to report beat-to-beat variability and estimates vagal tone19. RMSSD was significantly higher in CAVB animals under escape rhythm than in control animals under sinus rhythm (Fig. 5B). This difference was preserved during the day and the night (Fig. 5B). SDRR and SDNN report generalized heart rate variability trends for a subject, with SDRR utilizing all beats including arrhythmic and polymorphic beats20. There was no significant change in the SDRR (Fig. 5C) or SDNN (Fig. 5D) for CAVB animals when compared to animals under sinus rhythm during the day and the night.
Poincaré plots visualize the relationship in RR intervals between success beats21. We created poincaré plots with corresponding standard deviation ellipses and delta RR histograms, utilizing the same 1-hour intervals previously described for animals (n = 4) under sinus rhythm and subsequently under CAVB (Fig. 6A). Mean SD1 values, which measures rapid changes in R–R intervals and is regarded as a measure for the faster-acting vagal effects of parasympathetic innervation22, were higher under CAVB escape rhythm than in sinus rhythm during the 1-hour light and 1-hour dark intervals analyzed (Fig. 6B left). Mean SD2 values, which measure the effects of both sympathetic and parasympathetic innervation22, were not changed under CAVB escape rhythm when compared to sinus rhythm for the 1-hour light period and the 1-hour dark period (Fig. 6C). SD1/SD2 values, which compares a subject’s short term variability against its long term variability22, were higher in CAVB models under escape rhythm than in animals under sinus rhythm for both the light and dark periods (Fig. 6D). These data indicate that our CAVB animals are subject to higher degrees of beat-to-beat short term variability while simultaneously losing a significant amount of long-term heart rate variability when compared to their sinus rhythms.
Poincare analysis for beat-to-beat variability. (a) Poincare plots and beat-to-beat ∆RR for 1-hour light and dark periods for animals (n = 4) before and after CAVB creation, day five post-surgery. Black traces on Poincare plots indicate SD1 and SD2 values for each plot. (b) SD1, (c) SD2, and (d) SD1/SD2 values for the animals (n = 4) before and after CAVB creation, day five post-surgery, with standard deviation error bars.
Differences in autonomic denervation between novel CAVB model and sinus rhythm
To better understand autonomic regulation of the sinus and CAVB rhythms, we recorded heart rate changes upon pharmacological blockade of the autonomic nervous system in ambulatory animals. In normal animals under sinus rhythm (n = 5), intraperitoneal atropine administration (3 mg/kg) led to a significant increase in their mean heart rate from 338 ± 27 to 443 ± 28 bpm (32 ± 8%, p < 0.001, Fig. 7A). In contrast, atropine administration did not impact the escape rhythm of CAVB rats (n = 4) with an average beating rate of 137 ± 8 bpm before administration and 139 ± 9 bpm after administration (1.6 ± 1.5%, p ≥ 0.05, Fig. 7A). We also analyzed the sinus rhythm of CAVB animals by examining their PP intervals to attain atrial beating rates. As expected, the atrial beating rate of the CAVB animals increased significantly upon atropine administration from 346 ± 12 to 414 ± 13 bpm (17 ± 3%, p < 0.001, Figs. 7A).
Effects of autonomic denervation on CAVB animals. One minute beating rate averages over time (n = 1), 10-minute mean heart rates before and after drug administration, and ∆ beating rates before and after administration of (A) 3 mg/kg atropine, (B) 3 mg/kg propranolol, or (C) 3 mg/kg atropine and 3 mg/kg propranolol in sinus rhythm (SR) (n = 5) and CAVB (n = 4) models. Bar graphs include standard error bars.
A day after the atropine experiment, the same animals were administered propranolol (3 mg/kg) for blockade of sympathetic innervation. Immediately after propranolol treatment, the sinus rhythm of control animals (n = 5) decreased significantly from 385 ± 35 to 323 ± 12 bpm (-16 ± 8%, p < 0.05, Fig. 7B). Propranolol administration decreased the escape rhythm of CAVB animals (n = 4) as well from 127 ± 8 to 108 ± 11 bpm (-15 ± 5%, p < 0.05, Fig. 7B). Likewise, the atrial beating rate of CAVB animals (n = 4) decreased from 352 ± 7 to 303 ± 11 bpm during the same time (-14 ± 4%, p < 0.05, Fig. 7B).
A day after the propranolol experiment, the same animals were administered atropine and propranolol to mimic a complete blockade of autonomic influence on the heart rate. The sinus rhythm of control animals (n = 5) trended lower from 326 ± 21 bpm before atropine and propranolol injection to 303 ± 17 bpm after the pharmacologic denervation; however, statistical significance was not reached (-7 ± 6%, p ≥ 0.05, Fig. 7C). In contrast, the escape rhythm of CAVB animals showed a significant decrease upon treatment from 127 ± 25 to 108 ± 24 bpm (-15 ± 7%, p < 0.05, Fig. 7C). Atrial beating rate of the CAVB animals trended lower upon the treatment from 335 ± 18 to 321 ± 9 bpm without reaching statistical significance (-4 ± 4% p ≥ 0.05, Fig. 7C). Taken together, the data suggests that CAVB ventricular beating rates are significantly influenced by sympathetic innervation and but not by parasympathetic innervation when compared to sinus rhythm.
Discussion
In this study, we present a highly effective surgical method for creating stable and chronic CAVB in female rats with a 77% survival rate at 4 weeks after the surgery (Fig. 4; Table 1). The total surgery time from sedation to repair of the thoracotomy was abbreviated by almost 30 min, from two hours with subepicardial ablation to 1.5 h with epicardial ablation (Table 1). The animals recovered from anesthesia significantly faster, within < 15 min, with epicardial ablations compared to > 1 h with subepicardial ablation (Table 1). The substantial improvement in surgical outcomes is likely due to less charring of the myocardium and minimal bleeding at the ablation site with epicardial ablation. With our previous surgical method of subepicardial ablation with a sharp needle, we observed frequent perforation of myocardial tissue at the needle electrode upon ablative energy delivery. This frequently caused incidences of significant bleeding (Table 1). Additionally, in earlier studies by Cho and colleagues, sham-operated animals that underwent only needle puncture without energy delivery exhibited 100% survival, indicating that postoperative mortality is attributable to the ablation procedure itself rather than the sham intervention. Epicardial ablation also negated the surgical skills required for orienting the ablation needle into the interatrial septum to locate the AVN region, further reducing the surgical duration and any likelihood of complications (Table 1). Our new method showed a lower survival rate for male subjects at 2 weeks post-surgery (33%), suggesting that female rats are better suited for longitudinal studies utilizing this disease model. There were no significant differences in CAVB ventricular beating rates from ECG recordings 1-week of 4-weeks post-op (Table 1), and no appreciable differences in arrhythmic behaviors were observed between groups at those times, suggesting the new epicardial method exhibits similar morphological patterns to the previously established subepicardial disease model.
The daily escape rhythm of our new rat model of CAVB was about 60% slower than their sinus rhythm throughout the study period (Fig. 3A; Table 1). Due to variability in ablation depth, the degree of atrioventricular block can differ, which in turn influences whether escape rhythms arise from the junctional area or more distally from the ventricles. Because surface ECG recordings in rats cannot definitively distinguish between junctional and ventricular foci, the precise source of these rhythms remains uncertain. The polymorphic morphology observed in our recordings supports the possibility of multiple sites of origin, and it cannot be excluded that a substantial proportion of these escape rhythms were junctional rather than ventricular in nature.
Since clinical cases of symptomatic CAVB are rarely left untreated, there is a lack of extensive data on HRV parameters of escape rhythms. This stable and CAVB rodent model provides an opportunity to examine potential differences in HRV parameters in CAVB compared to sinus rhythm. Our CAVB models showed significant increases in beat-to-beat HRV parameters RMSSD and SD1, suggesting these CAVB models have high short-term ventricular variability. This finding may be due to the escape rhythms being unstable at the individual level, including potential induced lower lower-junctional tachycardia from incomplete destruction of the AVN. Diverse origins of escape rhythms between animals, ranging from the ventricular conduction system to the lower AVN, create additional increases in HRV when compared to the highly specialized and innervated pacemaker cells of the SAN. Additionally, long-term HRV parameters SDNN, SDRR and SD2 suggest no change in CAVB animals compared to sinus rhythm; however, once normalized to mean RR, these parameters are significantly lower for the CAVB group (Supplementary Fig. 2A-B, E). This finding mirrors prior studies indicating a decreased HRV in human subjects with heart block, likely due to decreased autonomic innervation of the ventricular conduction system where the escape rhythm of the CAVB subjects likely originates23.
Pharmacologic blockade of the parasympathetic branch led to a significant acceleration of the sinus rhythm, but not the escape rhythm of the CAVB animals (Fig. 7A). Blockade of the sympathetic innervation decelerated the escape rhythm of the CAVB animals as well as the sinus rhythm of normal animals (Fig. 7B), suggesting that the escape rhythm of CAVB rats is dominated by sympathetic control. Combined treatment with both atropine and propranolol slowed the escape rhythm in CAVB animals. In contrast, the sinus rhythm of normal animals showed no significant effect, supporting sympathetic dominance of the escape rhythm in CAVB rats. These findings suggest that our CAVB models experience lower total autonomic innervation, with a shift towards sympathetic dominance at the basal rate. Although autonomic regulation was not systematically studied in the earlier subepicardial model, important procedural distinctions between the two approaches provide context for interpreting our findings. The subepicardial method primarily delivered lesions deeper within the atrioventricular junction, whereas the present epicardial approach creates additional superficial lesions that encompass epicardial ganglionic plexi24. This anatomical difference likely contributes to the autonomic profile observed in the epicardial CAVB model, in which escape rhythms were sustained predominantly by sympathetic drive with parasympathetic influence almost completely abolished. While direct comparative data is lacking, these considerations suggest that the epicardial technique may result in greater interruption of autonomic inputs than the prior subepicardial approach. Combining electrophysiological findings with the simplicity of our new approach highlights the rigor and reproducibility of this disease model and its usefulness as a platform to study the disease.
Supplies
Ablation system.
12-gauge copper wire | Southwire | 11,587,383 |
ATAKR II RF ablation system | Medtronic | Model 4803 |
Banana plug | Sumnacon | 4,330,119,086 |
Alligator clip | Sumnacon | ULSMC00391 |
ATAKR to RF catheter, sterile, 12’ (366 cm) | Medtronic | 05116 S |
Reusable ground plate | Bovie | A1204 |
Spectra 360 electrode gel | MFI Medical | PKR-12-08 |
Telemetry.
Physiotel implantable telemeters | Data Sciences International | CTA-F40 |
Telemetry recording system | Data Sciences International | MX2 |
Telemetry receivers for plastic cages | Data Sciences International | RPC-1 |
Surgical instruments and supplies.
Rib retractor | Miltex | MH11-14 |
Dissecting scissors | Cole-Palmer | UX-10818-00 |
Forceps | Sigma Aldrich | F4142 |
Scalpel handle | Surgical Design | 27,057 A |
Scalpel #10 blade | JMU Dental | 46,101,004 |
Needle driver | ProDent USA | 14-256TC |
Ethilon nylon suture 5 − 0 | Ethicon | 698G |
Coated Vicryl suture 4 − 0 | Ethicon | J304H |
Sterile alcohol prep pads | Fisher Scientific | 22-363-750 |
Povidone iodine prep pads | Med Pride | MPR-41,153 |
Non-woven sterile gauze | McKesson | 16-4224 |
Small animal ventilator | Harvard Apparatus | Model 683 |
Tabletop isoflurane anesthesia system | Harvard Apparatus | 72-6468 |
Sterile drapes | Cardinal Health | 7554 |
Drugs.
OstiLox Meloxicam (5 mg/mL) | MWI Animal Health | 501,080 |
Buprenorphine polymer (1 mg/mL) | Wedgewood Pharmacy | BUPREN-INJ011VC |
Atropine | Santa Cruz Biotechnology | sc-252,392 |
Propranolol hydrochloride | Millipore Sigma | P0884-25G |
Isospire (isoflurane) | MWI Animal Health | 119,932 |
DPBS | Gibco | 14,190,250 |
Analysis software.
OriginLab OriginPro |
ADInstruments Labchart Pro 8 |
DSI Ponemah 6.5x |
Biorender |
Data availability
All data will be made available upon reasonable request to the corresponding author, Dr. Hee Cheol Cho.
References
Wu, W., He, J. & Shao, X. Incidence and mortality trend of congenital heart disease at the global, regional, and National level, 1990–2017. Med. (Baltim). 99, e20593. https://doi.org/10.1097/MD.0000000000020593 (2020).
Liberman, L., Silver, E. S., Chai, P. J. & Anderson, B. R. Incidence and characteristics of heart block after heart surgery in pediatric patients: A multicenter study. J. Thorac. Cardiovasc. Surg. 152, 197–202. https://doi.org/10.1016/j.jtcvs.2016.03.081 (2016).
Knabben, V., Chhabra, L. & Slane, M. in StatPearls (2024).
Baruteau, A. E., Perry, J. C., Sanatani, S., Horie, M. & Dubin, A. M. Evaluation and management of bradycardia in neonates and children. Eur. J. Pediatr. 175, 151–161. https://doi.org/10.1007/s00431-015-2689-z (2016).
Bignolais, O. et al. Early ion-channel remodeling and arrhythmias precede hypertrophy in a mouse model of complete atrioventricular block. J. Mol. Cell. Cardiol. 51, 713–721. https://doi.org/10.1016/j.yjmcc.2011.07.008 (2011).
Bordachar, P. et al. Pathophysiology, clinical course, and management of congenital complete atrioventricular block. Heart Rhythm. 10, 760–766. https://doi.org/10.1016/j.hrthm.2012.12.030 (2013).
Wolfson, D. W. et al. Transient pacing in pigs with complete heart block via myocardial injection of mRNA coding for the T-box transcription factor 18. Nat. Biomed. Eng. 8, 1124–1141. https://doi.org/10.1038/s41551-024-01211-9 (2024).
Farraha, M. et al. Development of a sheep model of atrioventricular block for the application of novel therapies. PLoS One. 15, e0229092. https://doi.org/10.1371/journal.pone.0229092 (2020).
Fisher, V. J., Lee, R. J., Christianson, L. C. & Kavaler, F. Production of chronic atrioventricular block in dogs without thoracotomy. J. Appl. Physiol. 21, 1119–1121. https://doi.org/10.1152/jappl.1966.21.3.1119 (1966).
Hu, Y. F., Dawkins, J. F., Cho, H. C., Marban, E. & Cingolani, E. Biological pacemaker created by minimally invasive somatic reprogramming in pigs with complete heart block. Sci. Transl Med. 6, 245ra294. https://doi.org/10.1126/scitranslmed.3008681 (2014).
Cingolani, E. et al. Biological pacemaker created by percutaneous gene delivery via venous catheters in a Porcine model of complete heart block. Heart Rhythm. 9, 1310–1318. https://doi.org/10.1016/j.hrthm.2012.04.020 (2012).
Baruscotti, M. et al. Deep bradycardia and heart block caused by inducible cardiac-specific knockout of the pacemaker channel gene Hcn4. Proc. Natl. Acad. Sci. U S A. 108, 1705–1710. https://doi.org/10.1073/pnas.1010122108 (2011).
Donoghue, M. et al. Heart block, ventricular tachycardia, and sudden death in ACE2 Transgenic mice with downregulated connexins. J. Mol. Cell. Cardiol. 35, 1043–1053. https://doi.org/10.1016/s0022-2828(03)00177-9 (2003).
Nakamura, K. et al. Complete heart block and sudden death in mice overexpressing calreticulin. J. Clin. Invest. 107, 1245–1253. https://doi.org/10.1172/JCI12412 (2001).
Kim, N. K., Wolfson, D., Fernandez, N., Shin, M. & Cho, H. C. A rat model of complete atrioventricular block recapitulates clinical indices of bradycardia and provides a platform to test disease-modifying therapies. Sci. Rep. 9, 6930. https://doi.org/10.1038/s41598-019-43300-9 (2019).
Hanna, P. et al. Innervation and neuronal control of the mammalian sinoatrial node a comprehensive atlas. Circ. Res. 128, 1279–1296. https://doi.org/10.1161/CIRCRESAHA.120.318458 (2021).
Quan, K. J. et al. Characterization of sinoatrial parasympathetic innervation in humans. J. Cardiovasc. Electrophysiol. 10, 1060–1065. https://doi.org/10.1111/j.1540-8167.1999.tb00278.x (1999).
Pauza, D. H. et al. Innervation of sinoatrial nodal cardiomyocytes in mouse. A combined approach using immunofluorescent and electron microscopy. J. Mol. Cell. Cardiol. 75, 188–197. https://doi.org/10.1016/j.yjmcc.2014.07.016 (2014).
McCraty, R. & Shaffer, F. Heart rate variability: new perspectives on physiological Mechanisms, assessment of Self-regulatory Capacity, and health risk. Glob Adv. Health Med. 4, 46–61. https://doi.org/10.7453/gahmj.2014.073 (2015).
Shaffer, F. & Ginsberg, J. P. An overview of heart rate variability metrics and norms. Front. Public. Health. 5, 258. https://doi.org/10.3389/fpubh.2017.00258 (2017).
Shlapakova, I. N. et al. Biological pacemakers in canines exhibit positive chronotropic response to emotional arousal. Heart Rhythm. 7, 1835–1840. https://doi.org/10.1016/j.hrthm.2010.08.004 (2010).
Hoshi, R. A., Pastre, C. M., Vanderlei, L. C. & Godoy, M. F. Poincare plot indexes of heart rate variability: relationships with other nonlinear variables. Auton. Neurosci. 177, 271–274. https://doi.org/10.1016/j.autneu.2013.05.004 (2013).
Tulppo, M. P., Makikallio, T. H., Takala, T. E., Seppanen, T. & Huikuri, H. V. Quantitative beat-to-beat analysis of heart rate dynamics during exercise. Am. J. Physiol. 271, H244–252. https://doi.org/10.1152/ajpheart.1996.271.1.H244 (1996).
Buckley, U., Rajendran, P. S. & Shivkumar, K. Ganglionated plexus ablation for atrial fibrillation: just because we can, does that mean we should? Heart Rhythm. 14, 133–134. https://doi.org/10.1016/j.hrthm.2016.09.001 (2017).
Funding
This research was supported by the National Institutes of Health under grants 1R01HL1430651A1, 1R01HL147270-01A1, and 1R01HL157363-01, and by the US Department of Defense under grant W81XWH2010643.
Author information
Authors and Affiliations
Contributions
All authors participated in the design, performance, analysis, drafting, or editing of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Statistical measurements
Statistics were performed utilizing two-sided Mann-Whitney U tests or chi-squared tests with a confidence interval of 0.05 (*), 0.01 (**), and 0.001 (***) when applicable. OriginLab OriginPro software was used to perform these calculations. All animal subjects used in the described experiments were included in the calculations without exclusion.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary Material 1
Supplementary Material 2
Supplementary Material 4
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Weltz, A.N., Fortuno-Miranda, L., Kolandaivelu, A. et al. A highly effective, rodent model of complete heart block by epicardial radiofrequency ablation. Sci Rep 15, 40740 (2025). https://doi.org/10.1038/s41598-025-24479-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-24479-6