Abstract
Risk stratification for sudden cardiac death (SCD) in hypertrophic cardiomyopathy (HCM) remains challenging. Enhanced imaging techniques could improve prognostic accuracy. This study investigates myocardial resting perfusion and metabolism using [13N]-NH3 and 2-[18F]FDG PET/CT and their correlation with HCM SCD risk scores. Thirty non-obstructive HCM patients (mean age 54 years, 57% male) with a mean SCD risk score of 3.7 ± 2.5% were evaluated. Myocardial 2-[18F]FDG metabolism and rest [13N]-NH3 perfusion PET/CT were analyzed. Hypermetabolism (2-[18F]FDG uptake with normal perfusion) occurred in 53% of cases (mean extension 11.8 ± 17.2%), while fibrosis (reduced perfusion without 2-[18F]FDG uptake) averaged 10.3 ± 10.2%. Mean rest myocardial blood flow (MBF) was 0.75 ± 0.21 ml/min/g, increasing with hypermetabolism extension (0.83 ± 0.32 ml/min/g for ≥ 20%, p = 0.019) but decreasing with SCD scores ≥ 6% (0.58 ± 0.05 ml/min/g, p = 0.034). Hypermetabolism correlated moderately with SCD risk scores (rho = 0.38, p = 0.036), with hypermetabolism peaking at intermediate risk (23.5 ± 27.1%) before declining. Fibrosis extension consistently increased with SCD risk (rho = 0.38, p = 0.039). In conclusion, our findings identify important correlations between myocardial hypermetabolism and fibrosis and SCD risk in HCM. Hypermetabolism peaks in intermediate-risk patients, reflecting earlier disease stages, while fibrosis increases with higher SCD risk, signaling disease progression and structural damage.
Similar content being viewed by others
Introduction
Hypertrophic cardiomyopathy (HCM) is an inherited cardiac disorder with an annual incidence of cardiovascular death ranging from 1 to 2%, primarily attributed to sudden cardiac death (SCD), heart failure, and thromboembolism1,2. The most prevalent form of HCM is associated with autosomal dominant mutations in sarcomeric genes, showcasing a variable phenotypical expression3. A significant challenge in managing this condition lies in the limited accuracy of the risk stratification score for predicting SCD1. Key clinical features linked to an increased risk of SCD include age, the presence of non-sustained ventricular tachycardias, maximum left ventricular (LV) wall thickness, a family history of SCD at a young age, syncope, left atrial (LA) diameter, and LV outflow tract obstruction2. Late gadolinium enhancement (LGE) observed in cardiac magnetic resonance (CMR) is indicative of intramyocardial fibrosis and exhibits a direct correlation with the incidence and severity of arrhythmias in HCM4,5,6. While the extent of LGE is not currently integrated into the 5-year SCD risk score, its assessment can aid in the decision-making process regarding the placement of implantable cardioverter-defibrillators (ICD)2,7. It’s important to note that not all instances of LGE necessarily denote myocardial fibrosis, as LGE is more frequently detected in the thickest LV segments. Remarkably, extensive LGE can also manifest in asymptomatic elderly HCM patients without resulting in adverse disease consequences7,8. Additionally, there may be patients who, despite not yet displaying evident fibrosis, exhibit underlying abnormal myocardial dysfunction and deformation, thereby posing a heightened risk of SCD1.
Improving imaging techniques is important for accurately identifying abnormal myocardial dysfunction without fibrosis and predicting prognosis more effectively1,4,8,9. Prolonged myocardial T1 assessed through CMR suggests diffuse myocardial fibrosis in HCM, even in the absence of regionally apparent LGE10,11. Despite its promise, the diagnostic and prognostic potential of this technique is not yet firmly established.
In HCM, even without apparent fibrosis, there could be impaired myocardial cell metabolism. While 18-fluorodeoxyglucose (2-[18F]FDG) myocardial positron emission tomography (PET) has been sporadically investigated in HCM, its precise role remains unclear8,12.
13N-ammonia ([13N]-NH3) myocardial perfusion PET/CT offers valuable information on microvascular circulation and flow reserve in HCM13. Microvascular ischemia in HCM could coincide with impaired myocardial blow flow (MBF) and reserve (MFR), inversely correlating with myocardial wall thickness14 and potentially contributing to the development of arrhythmias, cavity dilation, and fibrosis15,16,17.
Radiolabeled tracers targeting fibroblast activation protein inhibitors (FAPI) have been developed to identify activated fibroblasts as a surrogate of early-stage myocardial fibrosis18. FAPI activity has also been correlated with SCD risk score in HCM patients19.
The presence of intense 2-[18F]FDG uptake in HCM hints at a metabolic shift from fatty acids to glucose. Additionally, areas displaying noticeable LGE often show relatively low FDG uptake20. Consequently, heightened 2-[18F]FDG uptake might signify the earlier stages of the disease, though its clinical and prognostic implications are yet to be fully understood.
We postulate that this pattern of 2-[18F]FDG uptake and hypermetabolism could serve as an earlier indicator of disease progression, potentially manifesting even before the onset of abnormal myocardial deformation and fibrosis. Consequently, it might contribute to predicting the SCD risk in certain patients. The aim of our study was to examine myocardial perfusion and metabolism using [13N]-NH3 and 2-[18F]FDG PET/CT in patients with HCM and evaluate its correlation with SCD.
Methods
Study population
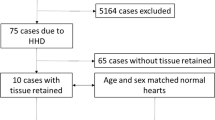
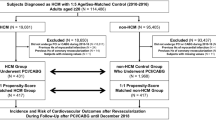
In this cross-sectional observational study, from January 2022 to September 2023, we initially enrolled 35 patients with sarcomeric NOHCM. Exclusion criteria encompassed individuals below 18 or above 70 years of age; false-positive 2-[18F]FDG-uptake; other morphological types of HCM [obstructive HCM (OHCM) and apical HCM]; left ventricular ejection fraction (LVEF) less than 55%; pregnancy; competitive athletes; autoimmune, inflammatory, neoplastic, or infiltrative diseases (including amyloidosis, sarcoidosis, and Fabry’s disease); significant valvular disease; significant coronary artery disease, and significant arterial hypertension (uncontrolled arterial hypertension leading to secondary left ventricular hypertrophy).
Of the initial cohort of 35 patients, 3 exhibited patterns consistent with false-positive uptake, and 2 did not undergo the standardized dietary preparation. All five of these cases were excluded from the final analysis to ensure the accuracy and reliability of our findings. False-positive FDG uptake was identifiable based on its characteristic pattern—typically more homogeneous and diffuse—distinct from the focal or heterogeneous uptake observed in pathological cases. This distinction was especially evident in patients who did not follow the dietary preparation protocol.
Study design and procedures
Baseline clinical data were collected from patients’ hospital medical records, obtained in our Cardiology department. This included demographic information (age and gender), results from genetic testing, history of syncope, presence of atrial and ventricular arrhythmias, family history of SCD, SCD risk score, and ICD status.
We analyzed CMR scans pre-study to gather data on wall thickness, myocardial mass, and LGE.
All patients underwent a baseline echocardiography performed in our center, followed by PET/CT.
All patients underwent assessment of rest myocardial perfusion and myocardial metabolism by PET/CT.
This study was approved by the Ethics Committee of the Coimbra Hospital and University Center and Faculty of Medicine of University of Coimbra Consortium (project reference number: CE-017/2021). Informed consent was obtained from all individual participants included in the study. All methods and research were performed in accordance with the Declaration of Helsinki.
Echocardiography and CMR data
A comprehensive echocardiographic analysis, namely LA dimensions and LVEF, was performed. We utilized a Vivid 7 (GE Healthcare, Horten, Norway) cardiovascular ultrasound device, with a 1.7/3.4-MHz tissue harmonic transducer. Standard echocardiographic views were obtained with frame-rate optimization (60–80 frames per second in 2D imaging). Subsequently, we performed offline analysis of the echocardiographic data using a specific software (EchoPAC 16.0; GE Healthcare).
We analyzed CMR scans pre-study to gather data on wall thickness, myocardial mass, and LGE. Imaging had been conducted on a 1.5-T Siemens Sonata scanner. After gadolinium injection, LGE images were acquired and analysis involved manual delineation of hyperenhancement areas across short-axis slices. Total hyperenhancement volume, as a percentage of myocardium, resulted from summing the areas, as previously described21. Quantification was performed using a 2-standard deviation technique.
PET/CT
We obtained rest [13N]-NH3 perfusion and 2-[18F]FDG metabolism images on the same day utilizing a PET/CT scanner (Biograph Vision 600, Siemens). To mitigate physiologic 2-[18F]FDG cardiac uptake, subjects adhered to a high-fat/low-carbohydrate diet 48 h prior to the scan, coupled with a 12-h fasting period leading up to the scan. Rest perfusion imaging involved injecting 10 mCi of [13N]-NH3 ove2r 10 min, employing dynamic and gated acquisitions. Subsequently, 2-[18F]FDG imaging took place around 60 min after injecting 10 mCi of 2-[18F]FDG, acquired over a 10-min interval. Low-dose CT scans of the heart were performed for attenuation correction (120kv and 10 mA) before both [13N]-NH3 and 2-[18F]FDG imaging. The verification of CT attenuation map registration with PET images was ensured. Evaluation of myocardial metabolism via 2-[18F]FDG and perfusion analysis through [13N]-NH3 PET/CT was conducted using dedicated software (Corridor 4DM INVIA).
Assessment of rest myocardial blood flow
Dynamic perfusion images with [13N]-NH3 were employed to evaluate resting myocardial blood flow, both on a global scale and within specific vascular territories. The nominal transaxial/axial spatial resolutions were 4.4 mm/4.7 mm. To conduct a semi-quantitative analysis of regional myocardial perfusion, a 17-segment visual interpretation was executed using a standard five-point scoring system. Quantification of both global and regional (based on vascular territories) MBF (mL/min/g) was carried out using commercially available software (INVIA Ann Arbor, MI, USA) on the dynamic rest datasets.
Myocardial regions with rest MBF values ≥ 0.7 mL/min/g were considered to have normal [13N]NH3 PET perfusion, while those with MBF values < 0.7 mL/min/g were classified as having reduced perfusion. This threshold is based on prior published literature indicating that resting perfusion below this level may reflect impaired microvascular function or fibrotic replacement in the context of cardiomyopathies14,17,22,23.
Assessment of 2-[18F] FDG uptake pattern
LV surfaces were delineated from [13N]-NH3 images using the standard surface algorithm. Through indirect registration across perfusion images, PET and CT, and metabolism images, the [13N]-NH3 left ventricle surfaces were transferred to the FDG images. Our software identified significant increases in 2-[18F]FDG metabolism when myocardial uptake exceeded the activity of the left ventricle vascular pool (threshold ≥ 1.1).
While this approach differs from standard viability protocols—typically based on glucose loading or insulin-clamp techniques—our objective was not to assess myocardial viability, but rather to evaluate inflammatory/metabolic activity. This strategy is aligned with protocols previously established for detecting myocardial inflammation, such as those used in cardiac sarcoidosis evaluation24,25,26.
Increased metabolic activity/hypermetabolism was characterized by 2-[18F]FDG uptake with normal [13N]-NH3 PET perfusion; fibrotic myocardium was characterized by no 2-[18F]FDG uptake with reduced [13N]-NH3 PET perfusion. Hypermetabolism and fibrosis/scar extension were expressed globally as a percentage of LV involvement and regionally (apex, septum, anterior, inferior, and lateral walls) (Fig. 1). Maximum Target to Background Ratio (TBR) of the LV and of each of its walls was also evaluated by the same software.
Final Software Processing of 2-[18F]FDG Myocardial uptake analysis. Top panel: short-axis, horizontal long-axis and vertical long-axis images from 2-[18F]FDG PET/CT with LV volume of interest (VOI) superimposed as defined in the perfusion PET. A VOI in the LV cavity was drawn to determine blood pool activity. The 2-[18F]FDG threshold was calculated as the blood pool activity (SUV mean) multiplied by a factor of 1.1. Middle panel: Left: Rest [13N]NH3 perfusion polar plots. The first plot shows average perfusion, percentage wise, per region. The blackout areas in the second plot indicate abnormally low perfusion. Right: 2-[18F]FDG uptake (metabolism) polar plots. The third plot indicates the average SUV for each region. The black areas in the fourth plot indicate abnormally high 2-[18F]FDG uptake (SUV exceeds the threshold). Bottom panel: Integration of the rest [13N]NH3 perfusion and 2-[18F]FDG myocardial uptake analysis identifies distinct patterns: Scar (green): Reduced perfusion and no significant 2-[18F]FDG uptake (referred to, in the text, as fibrosis). Inflammatory myocardium (blue): Normal perfusion and increased 2-[18F]FDG uptake (referred to, in the text, as hypermetabolic myocardium). These patterns are expressed as percentages of the total left ventricle and further categorized according to five regions: apex, septum, anterior wall, inferior wall, and lateral wall. In the example provided, the patient exhibited 33% normal myocardium, 46% inflammatory (hypermetabolic) myocardium and 3% scar (fibrosis) extension.
Statistical analysis
Normality of the distribution of continuous variables was assessed by histogram analysis and the Kolmogorov–Smirnov test. Continuous variables were expressed as mean ± standard deviation, and categorical variables were expressed as frequency (percentage). Between-group differences were evaluated using one-way ANOVA analysis. For each variable with non-normal distribution, the homogeneity of variance was assessed using the Levene test. For categorical variables, the chi-square test or the Fisher’s exact test were used, as appropriate.
Continuous variables were categorized for analysis as follows: hypermetabolism extension was grouped into tertiles (0, < 20, and ≥ 20%); fibrosis extension was divided into tertiles (0, < 10, and ≥ 10%); TBR was stratified into three levels based on the 2-[18F]FDG tissue-to-background uptake ratio (< 1, 1–2, and ≥ 2); SCD risk score was classified into three risk categories (< 4, 4–6, and ≥ 6%) in accordance with the 2023 European Society of Cardiology Guidelines for the management of cardiomyopathies2. Spearman correlation analysis was employed to correlate several continuous parameters. Statistical significance was set at p value < 0.05. Data analysis was performed using Stata IC for Windows (version 13; StataCorp, Lakeway Drive, TX, USA).
Results
Study population
Clinical and echocardiographic baseline data are summarized in Table 1. The mean age was 54.4 ± 11.3 years, with 57% of patients being male. Eleven patients (36.7%) had a positive genetic result: 3 carried mutations in the MYBPC3 gene, 4 in MYH7, 3 in TNNT2, and 1 patient harbored coexisting mutations in both MYH7 and TNNT2.The mean maximum wall thickness was 20.3 ± 4.39 mm, with a minimum value of 15 mm and a maximum of 32 mm. In our study population, the maximum wall thickness was consistently observed in the interventricular septum, corresponding to the morphological subtype of asymmetric septal hypertrophy.The mean SCD score was 3.7 ± 2.5% and 30% of patients had a score ≥ 4%.
PET/CT analysis
[13N]-NH3 rest myocardial perfusion and 2-[18F]FDG myocardial metabolism PET/CT analysis
PET/CT data is presented in Table 2 and Supplementary Table A.
Mean resting MBF rates were 0.75 ± 0.21 ml/min/g, varying across myocardial segments. The apical segment had the highest rates (0.78 ± 0.21 ml/min/g), and the septal segment the lowest (0.71 ± 0.21 ml/min/g). Increased 2-[18F]FDG uptake (TBR > 1.1) was observed in 53% of the cohort. Mean TBR was 1.35 ± 0.5, highest in the septal segment and lowest in the apical segment. Mean global hypermetabolism extension was 11.8 ± 17.2%, most in the anterior (13.4 ± 21.7%) and septal (12.8 ± 19.1%) segments, and least in the lateral segment. Global fibrosis extension averaged 10.3 ± 10.2%, highest in the anterior (19.7 ± 25.1%) and lowest in the septal segment (2.5 ± 4.9%).
Table 2 presents the variations in [13N]-NH3 rest myocardial perfusion (MBF) based on 2-[18F]FDG uptake (TBR levels, hypermetabolism extension terciles; fibrosis extension terciles).
For TBR levels, MBF was lower at intermediate values (TBR between 1 and 2) but showed a significant global and regional increase when TBR reached ≥ 2. Regarding hypermetabolism extension, MBF significantly increased across higher terciles of global hypermetabolism extension (p = 0.019), as illustrated in Fig. 2a. This trend was also observed at the segmental level.
For fibrosis extension, MBF exhibited a decreasing trend with increasing extension terciles (second to third terciles, when fibrosis extension exceeds 0%) (Table 2). This pattern was similarly noted at the segmental level.
Resting flow rates did not demonstrate a direct correlation with either increased metabolism or fibrosis (as indicated by non-significant results in Spearman analysis—rho 0.23 and − 0.03, p = 0.21 and 0.87, respectively). However, it is noteworthy that both global and segmental MBF showed significant variations, with an ascending trend observed across global hypermetabolism and a descending trend across fibrosis (Table 2, Fig. 2a).
[13N]-NH3 rest myocardial perfusion PET/CT analysis and SCD risk scores
MBF did not exhibit a direct correlation with the SCD score (rho = − 0.19, p = 0.310). However, it demonstrated a significant decreasing trend across higher levels of SCD risk score (Table 2, Fig. 2b). Segmental analysis also revealed a decreasing MBF trend across SCD risk score levels, with statistical significance observed only in the anterior and apical segments.
2-[18F]FDG myocardial metabolism PET/CT analysis and SCD risk scores
Increased 2-[18F]FDG uptake, expressed as TBR, demonstrated a significant moderate correlation with SCD risk score (rho of 0.38, p = 0.036). This correlation was notably significant in the anterior (rho = 0.44) and inferior (rho = 0.44) myocardial segments (Table 3).
Increased 2-[18F]FDG uptake expressed as hypermetabolism extension, had a significant moderate correlation with SCD risk score when analyzing the inferior myocardial segment (rho = 0.47, p = 0.008) (Table 3, Fig. 3a).
Left panel: Scatter plots illustrating variation of sudden cardiac death (SCD) risk scores with (a) hypermetabolism extension (%) and (b) PET/CT fibrosis extension (%). Right panel: Bar charts displaying mean values (± SD) of (c) hypermetabolism extension (%) and (d) PET/CT fibrosis extension (%), across different SCD risk score categories. SCD: sudden cardiac death.
Global and segmental myocardial hypermetabolism and fibrosis extension did not show statistically significant variations across the SCD score levels (see Supplementary Table B). However, myocardial hypermetabolism displayed an ascending trend from low to intermediate SCD risk levels, peaking in the intermediate level (23.5 ± 27.1%), and subsequently showing a descending trend at the higher risk score level (10.8 ± 15.2%) (Fig. 3c). Meanwhile, myocardial fibrosis exhibited an ascending trend across the SCD risk score levels (Fig. 3b and d).
Fibrosis assessment via CMR (LGE)
Mean LGE extension was 9.8 ± 7.4%, with 53% (n = 16) of patients exhibiting LGE in the CMR.
LGE extension showed no significant correlation with MBF (rho = − 0.02, p = 0.925) or fibrosis extension assessed by PET/CT (rho = 0.06, p = 0.775).
However, a moderate correlation was observed between LGE extension and hypermetabolism extension (rho = 0.45, p = 0.037), particularly in the anterior and septal myocardial segments (Table 4).
Additionally, LGE extension moderately correlated with SCD risk scores (rho = 0.45, p = 0.035), with the strongest association noted in the septal myocardial segment (rho = 0.48, p = 0.023) (Table 3).
Discussion
We present noteworthy findings on a NOHCM population, with a notable prevalence of positive genetic study, significant SCD scores, and prior ICD implantation.
Our analysis of PET/CT in this cohort revealed the following:
-
MBF increased across hypermetabolism terciles and decreased across fibrosis terciles, consistent in global and segmental analyses (Fig. 2a, Table 2). MBF followed a significant downward trend with higher SCD risk levels (Fig. 2b, Table 3).
-
A moderate positive correlation emerged between increased 2-[18F]FDG uptake (TBR) and SCD risk scores, especially in anterior and inferior myocardial segments. Hypermetabolism extension showed an upward trend from low to intermediate SCD risk score categories before declining in high-risk patients (Fig. 3a,c).
-
Fibrosis extension (assessed by PET/CT) also moderately correlated with SCD risk scores, particularly in the septal segment, and consistently increased across SCD risk categories (Fig. 3b,d).
-
Hypermetabolism extension demonstrated a moderate correlation with LGE as assessed by CMR; however, no such correlation was observed with fibrosis extension assessed via PET/CT.
To the best of our knowledge, this study marks the first instance of reporting a correlation between myocardial hypermetabolism and fibrosis (assessed by 2-[18F]FDG PET-CT) and SCD scores. Furthermore, we present novel insights, highlighting significant trends in the variation of resting flow rates with myocardial hypermetabolism and fibrosis, including analyses at myocardial segmental level.
In our study, we adopted a distinct methodological approach for the PET protocol, employing a high-fat, low-carbohydrate diet combined with prolonged fasting prior to 2-[18F]FDG PET imaging. Unlike standard viability protocols, which typically aim to assess myocardial viability through glucose loading, our goal was to evaluate inflammatory and metabolic activity. This preparatory strategy suppresses physiological myocardial glucose uptake and highlights pathological uptake—an essential distinction when investigating hypermetabolic patterns that may reflect early myocardial injury, low-grade inflammation, or altered substrate metabolism in HCM. Our analysis was purposefully structured to assess the spatial extent of hypermetabolism (defined as increased 2-[18F]FDG uptake with preserved perfusion) and fibrosis (characterized by reduced perfusion without corresponding 2-[18F]FDG uptake). This binary classification enabled quantification of myocardial involvement as a percentage of the LV surface. We considered these spatial burden metrics clinically relevant for exploring the relationship between metabolic/perfusion abnormalities and SCD risk scores.
Resting flow rates showed significant fluctuations across SCD risk score levels, with a consistent downward trend. Although no study directly reports this trend, [13N]-NH3 myocardial perfusion PET/CT offers insights into microvascular circulation and flow reserve in HCM13. Severe microvascular dysfunction predisposes to myocardial ischemia, leads replacement fibrosis, and may result in heart failure and arrhythmias over time15,16,17,22.
Initial studies using nuclear magnetic resonance spectroscopy indicate reduced mitochondrial energy reserves in HCM, suggesting metabolic changes may precede coronary microvascular dysfunction27. HCM-related mutations increase the energetic cost of sarcomere contraction, supporting the hypothesis that heightened sarcomere energy consumption causes progressive strain on cardiomyocytes, contributing to its pathophysiology22,28.
Newer research documented abnormal uptake of 2-[18F]FDG in HCM12,29,30,31,32,. The observed increase in uptake in HCM was attributed to heightened glucose utilization and impaired fatty acid metabolism32.
In NOHCM, 2-[18F]FDG uptake was observed to be limited to the hypertrophied segments, where LGE was also found32. In our study, hypermetabolism (FDG uptake) extension showed a moderate correlation with LGE extension, which, in turn, typically demonstrated a moderate correlation with SCD risk scores.
MBF rises in parallel with hypermetabolism (Fig. 2a), while hypermetabolism exhibits a declining trend beyond the intermediate SCD risk score levels (Fig. 2b).
Notably, hypermetabolism extension exhibits an initial upward trend, peaking at the intermediate SCD risk score level. A plausible explanation is that, in the early stages of HCM, there is an increased blood inflow to hypertrophied segments with elevated metabolic demands. This heightened metabolic activity may contribute to microvascular dysfunction and the progression of fibrosis, ultimately advancing the disease to later stages. This hypothesis is further supported by the upward trend in fibrosis extension across higher SCD risk scores (Fig. 3b,d).
In a recent study, PET/CT utilizing fibroblast activation protein tracers (FAPI) as a marker for early-stage fibrosis revealed a significant correlation between FAPI activity and SCD risk scores19. However, the precise timing of hypermetabolism onset during HCM progression remains uncertain. Our findings suggest that hypermetabolism predominantly emerges during intermediate stages of the disease and begins to decline as fibrosis becomes more prominent.
A recent investigation indicated that impaired global longitudinal strain (GLS) served as a predictor of SCD and cardiovascular mortality in patients with HCM33. It suggests intermediate to later stages of the disease, where microvascular dysfunction has already occurred, and a linear relationship between GLS and SCD is established. In our study, we delve into the correlation between hypermetabolism and SCD, revealing a significant association, albeit not a linear one, as higher SCD scores demonstrate a trend toward decreasing myocardial metabolism. We propose that in the intermediate SCD risk category, where hypermetabolism extension decreases, might correspond to later stages, marking the point where the correlation begins to diminish.
Our study has certain limitations. Firstly, the sample size could potentially constrain the statistical power essential for a robust analysis and interpretation of the data. Secondly, the absence of histological confirmation through endomyocardial biopsy. As routine biopsy is not performed in patients with HCM at our center, the diagnosis was based on clinical, imaging, and genetic criteria. While these approaches are widely accepted in clinical practice, they do not allow for direct histopathological confirmation of the disease. Thirdly, prior ICD implantation could introduce a degree of selection bias, particularly by enriching the cohort with individuals perceived to be at higher risk. However, we do not believe this substantially confounds our primary imaging findings. The goal of the study was to explore imaging-based markers of metabolic and perfusion alterations and their correlation with SCD risk scores, rather than arrhythmic outcomes or ICD therapies. Nevertheless, prior ICD implantation is an important contextual factor and is a potential limitation in terms of generalizability.
Finally, we did not conduct myocardial stress during perfusion PET, which restricts our capability to draw conclusions about microvascular ischemia. Even so, the prediction of arrhythmias does not show consistent correlation with MBF16,34. Moreover, the challenge lies in objectively establishing a direct association between microvascular ischemia and fibrosis, particularly given the presence of fibrosis in cases where MFR remains within the normal range35. Significantly, our study concentrated solely on analyzing rest perfusion and rest metabolism. The results indicate anomalous myocardial metabolism occurring at the basal state, regardless of subsequent myocardial stress induction and the eventual manifestation of microvascular dysfunction. Finally, being a cross-sectional study, we lack the capacity to conduct follow-ups on the patients, thereby impeding the acquisition of prognostic data. It is worth noting that the infrequency of events makes short-term follow-up endeavors particularly challenging.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- [13N]-NH3 :
-
Ammonia
- 2-[18F]FDG :
-
Fluorodeoxyglucose
- CMR:
-
Cardiac magnetic resonance
- GLS:
-
Global longitudinal strain
- HCM:
-
Hypertrophic cardiomyopathy
- ICD:
-
Implantable cardioverter-defibrillator
- LA:
-
Left atrium
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- MWT:
-
Maximum wall thickness
- NOHCM:
-
Non-obstructive hypertrophic cardiomyopathy
- OHCM:
-
Obstructive hypertrophic cardiomyopathy
- PET:
-
Positron emission tomography
- SCD:
-
Sudden cardiac death
- SUV:
-
Standard uptake values
References
Todiere, G. et al. Prognostic role of late gadolinium enhancement in patients with hypertrophic cardiomyopathy and low-to-intermediate sudden cardiac death risk score. Am. J. Cardiol. 124(8), 1286–1292 (2019).
Arbelo, E. et al. 2023 ESC Guidelines for the management of cardiomyopathies: Developed by the task force on the management of cardiomyopathies of the European Society of Cardiology (ESC). Eur. Heart J. 44(37), 3503–3626 (2023).
Zen, K. et al. Analysis of circulating apoptosis mediators and proinflammatory cytokines in patients with idiopathic hypertrophic cardiomyopathy: Comparison between nonobstructive and dilated-phase hypertrophic cardiomyopathy. Int. Heart J. 46(2), 231–244 (2005).
Mentias, A. et al. Late gadolinium enhancement in patients with hypertrophic cardiomyopathy and preserved systolic function. J. Am. Coll. Cardiol. 72(8), 857–870 (2018).
Sakuma, H. Late gadolinium enhancement and prognosis of hypertrophic cardiomyopathy. Circ. J. 78(4), 832–834 (2014).
Panovsky, R. et al. The prognostic impact of myocardial late gadolinium enhancement. Cardiol. Rev. 22(3), 128–139 (2014).
Ommen, S. R. et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 76(25), 3022 (2020).
Jung, K. E., Hee, L. S. & Ho, C. I. Myocardial fibrosis in hypertrophic cardiomyopathy demonstrated by integrated cardiac F-18 FDG PET/MR. Nucl. Med. Mol. Imaging. 47(3), 196–200 (2013).
Kramer, C. M. & Neubauer, S. Further refining risk in hypertrophic cardiomyopathy with late gadolinium enhancement by CMR ∗. J. Am. Coll. Cardiol. 72(8), 871–873 (2018).
Xu, J. et al. MRI T1 mapping in hypertrophic cardiomyopathy: Evaluation in patients without late gadolinium enhancement and hemodynamic obstruction. Radiology 294(2), 275–286 (2020).
Huang, L. et al. MRI native T1 and T2 mapping of myocardial segments in hypertrophic cardiomyopathy: Tissue remodeling manifested prior to structure changes. Br. J. Radiol. 92(1104), 20190634 (2019).
Uehara, T. et al. Myocardial glucose metabolism in patients with hypertrophic cardiomyopathy: Assessment by F-18-FDG PET study. Ann. Nucl. Med. 12(2), 95–103 (1998).
Opstal, T., Knol, R., Cornel, J., Wondergem, M. & van der Zant, F. Myocardial blood flow and myocardial flow reserve values in 13N–ammonia myocardial perfusion PET/CT using a time-efficient protocol in patients without coronary artery disease. Eur. J. Hybrid Imaging. 2(1), 11 (2018).
Knaapen, P. et al. Determinants of coronary microvascular dysfunction in symptomatic hypertrophic cardiomyopathy. Am. J. Physiol. Heart Circ. Physiol. 294(2), H986–H993 (2008).
Bravo, P. E. et al. Apparent left ventricular cavity dilatation during PET/CT in hypertrophic cardiomyopathy: Clinical predictors and potential mechanisms. J. Nucl. Cardiol. 23(6), 1304–1314 (2016).
Lu, D.-Y. et al. Stress myocardial blood flow heterogeneity is a positron emission tomography biomarker of ventricular arrhythmias in patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 176(5), 139–148 (2018).
Bravo, P. E. Is there a role for cardiac positron emission tomography in hypertrophic cardiomyopathy?. J. Nucl. Cardiol. 26(4), 1125–1134. https://doi.org/10.1007/s12350-018-1298-4 (2019).
Matthijs Blankesteijn, W. Has the search for a marker of activated fibroblasts finally come to an end?. J. Mol. Cell. Cardiol. 88, 120–123 (2015).
Wang, L. et al. Myocardial activity at 18F-FAPI PET/CT and risk for sudden cardiac death in hypertrophic cardiomyopathy. Radiology 306(2), e221052 (2023).
Takeishi, Y. et al. Cardiac imaging with 18F-fluorodeoxyglucose PET/MRI in hypertrophic cardiomyopathy. J. Nucl. Cardiol. 24(5), 1827–1828 (2017).
Moon, J. C. et al. Toward clinical risk assessment inhypertrophic cardiomyopathy withgadolinium cardiovascular magnetic resonance. J. Amer. College Cardiol. 41(9), 1561–1567. https://doi.org/10.1016/S0735-1097(03)00189-X (2003).
Timmer, S. A. J. & Knaapen, P. Coronary microvascular function, myocardial metabolism, and energetics in hypertrophic cardiomyopathy: Insights from positron emission tomography. Eur. Heart J. Cardiovasc. Imaging. 14(2), 95–101 (2013).
Camici, P. G. & Rimoldi, O. E. The clinical value of myocardial blood flow measurement. J. Nucl. Med. 50(7), 1076–1087 (2009).
Hutt, E., Goldar, G., Jaber, W. A. & Cremer, P. C. Standardized ketogenic dietary preparation for metabolic PET imaging in suspected and known cardiac sarcoidosis. Eur. Hear J. Imaging Methods Pract. 2(1), 1–5. https://doi.org/10.1093/ehjimp/qyae037 (2024).
Miller, R. J. H. et al. Quantitative assessment of cardiac hypermetabolism and perfusion for diagnosis of cardiac sarcoidosis. J. Nucl. Cardiol. 29(1), 86–96 (2022).
Blankstein, R. et al. Cardiac positron emission tomography enhances prognostic assessments of patients with suspected cardiac sarcoidosis. J. Am. Coll Cardiol. 63(4), 329–336 (2014).
Jung, W. I. et al. P NMR spectroscopy detects metabolic abnormalities in asymptomatic patients with hypertrophic cardiomyopathy. Circulation 97(25), 2536–2542 (1998).
Ashrafian, H., Redwood, C., Blair, E. & Watkins, H. Hypertrophic cardiomyopathy:a paradigm for myocardial energy depletion. Trends Genet. 19(5), 263–268 (2003).
Norikane, T. et al. Occasionally increased 18F-FDG uptake in apical hypertrophic cardiomyopathy on serial follow-up PET/CT. J. Nucl. Cardiol. 26(6), 2125–2128. https://doi.org/10.1007/s12350-019-01623-0 (2019).
Katagiri, M. et al. Incidental spade-shaped FDG uptake in the left ventricular apex suggests apical hypertrophic cardiomyopathy. Ann. Nucl. Med. 31(5), 399–406 (2017).
Kagaya, Y. et al. Differences in myocardial fluoro-18 2-deoxyglucose uptake in young versus older patients with hypertrophic cardiomyopathy. Am. J. Cardiol. 69(3), 242–246 (1992).
Aoyama, R. et al. Evaluation of myocardial glucose metabolism in hypertrophic cardiomyopathy using 18F-fluorodeoxyglucose positron emission tomography. PLoS ONE 12(11), 1–16 (2017).
Choi, Y.-J. et al. Left ventricular global longitudinal strain as a prognosticator in hypertrophic cardiomyopathy with a low-normal left ventricular ejection fraction. Eur. Hear J. Cardiovasc. Imaging. 24(10), 1374–1383. https://doi.org/10.1093/ehjci/jead177 (2023).
Lorenzoni, R. et al. Syncope and ventricular arrhythmias in hypertrophic cardiomyopathy are not related to the derangement of coronary microvascular function. Eur. Heart J. 18(12), 1946–1950 (1997).
Bravo, P. E. et al. The relationship of delayed enhancement by magnetic resonance to myocardial perfusion by positron emission tomography in hypertrophic cardiomyopathy paco. Circ. Cardiovasc. Imaging 6(2), 210–217 (2013).
Acknowledgements
To José Paulo de Almeida, MD, for his invaluable assistance in gathering CMR data.
Author information
Authors and Affiliations
Contributions
All authors have made substantial contributions to the conception and design of the work. Acquisition, analysis and interpretation of data were performed by PMA, MJF and RS. PMA has drafted and substantially revised the manuscript. All authors have approved the submitted version of the manuscript. All authors have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Marques-Alves, P., Ferreira, M.J.V., Silva, R. et al. 2-[18F]FDG PET identifies metabolic substrates of sudden cardiac death in hypertrophic cardiomyopathy. Sci Rep 15, 41298 (2025). https://doi.org/10.1038/s41598-025-25140-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-25140-y