Abstract
Despite transmitted drug resistance (TDR) surveillance is the critical role in HIV-1 prevention strategies, epidemiological data remain scarce for newly infected men who have sex with men (MSM) in Hebei Province, China. To address this data gap, we conducted a cross-sectional study involving 173 MSM recently infected with HIV-1. Plasma samples were subjected to HIV-1 RNA extraction, followed by amplification and sequencing of the pol gene region (PR-RT: 1.3 kb; IN: 0.8 kb). In this study, 173 sequences were successfully sequenced, and the sequencing success rate was 92.5% (173/187). Subtyping analysis revealed a predominance of CRF07_BC (36.4%, 63/173) and CRF01_AE (32.3%, 56/173), with a notable proportion of unique recombinant form (URF, 20.2%, 35/173). The overall TDR prevalence was 7.51% (13/173), categorized by drug class as follows: protease inhibitors (PIs, 2.31%, 4/173), nucleoside reverse transcriptase inhibitors (NRTIs, 1.16%, 2/173), non-nucleoside reverse transcriptase inhibitors (NNRTIs, 2.31%, 4/173), and integrase strand transfer inhibitors (INSTIs, 2.89%, 5/173). Notably, one participant exhibited concurrent resistance to NRTIs, NNRTIs, and INSTIs. While these findings suggest moderate TDR control in Hebei’s MSM population, we emphasize the necessity for sustained surveillance to dynamically assess treatment program efficacy, optimize second-line therapy regime, and guide public health interventions. This study provides the first comprehensive TDR profile for recently infected individuals in Hebei, offering critical insights for regional HIV-1 management.
Similar content being viewed by others
Introduction
Globally, the number of recent HIV infections amounted to 1.3 million in 2023. Although this was a 39% decrease from the 2010 figure of 2.1 million, there is still a long way to go to reach the goal of reducing the number of recent infections to 370,000 by 20251. The number of recent HIV infections among MSM (men who have sex with men) increased by 11% per year between 2010 and 2022. It is estimated that 210,000 recent HIV infections occurred in 2022 alone2.
Compared with previous studies on the prevalence of recently diagnosed HIV infections, the caculation of the prevalence rate using recently HIV-infected individuals (defined as those who contracted HIV within the past 130 days) as the study population avoids potential time lag effects, reflects the current epidemic status, and enhances the accuracy of forecasting HIV epidemic trend.
Since the National Free Antiretroviral Treatment Program (NFATP) was fully implemented in China in 20043, the treated people have progressively expanded. In 2016, China aligned with World Health Organization (WHO)’s “Treat All” strategy4, extending antiretroviral therapy (ART) coverage to all diagnosed HIV individuals. Although expanded ART has reduced HIV-related morbidity and mortality, prolonged treatment durations have given rise to the increase of drug resistance rates. HIV drug resistance elevates treatment costs and complexity, substantially increases ART failure risks5, accelerates the transmission of resistant strains, and critically challenges AIDS containment efforts.
WHO classifies HIV drug resistance into three categories: transmitted drug resistance (TDR), pretreatment drug resistance (PDR), and acquired drug resistance (ADR)6. TDR refers to resistance detected in ART - naïve individuals infected with drug - resistant strains. In China, the national HIV control framework mandates that all of recently diagnosed cases are registered in the Comprehensive AIDS Control Data Information Management System (CACDIMS). The initiation of ART is required within 10 working days after diagnosis, with all treatment records systematically archived in the national AIDS database. Given that recently diagnosed HIV individuals have no prior exposure to ART drugs, this surveillance mechanism ensures that the detected resistance in this population is presumptively categorized as TDR, providing a critical foundation for monitoring primary transmission dynamics of resistant variants.
In resource - limited situation, the systematic monitoring of HIV TDR, including baseline surveillance and resistance testing, in China remains inadequately implement compared to standardized protocols in the U.S. and Europe7. MSM are disproportionately affected by drug resistance due to complex behavioral and biological factors8, whcih can severely constrain the efficacy of first - line drugs. To evaluate subtype distribution and TDR prevalence among recently HIV infected MSM in Hebei Province, China, we performed a population - based analysis using 2023 surveillance data from the provincial AIDS registry. This study aims to inform targeted prevention strategies and optimize ART guidelines for high - risk groups in resource - limited regions.
Results
Demographic characteristics
A total of 187 recently infected HIV-1 MSM were included in this study. The age distribution showed a predominance of 25–49 years (48.66%, 91/187), followed by ≤ 24 years (33.69%, 63/187) and ≥ 50 years (17.65%, 33/187). Educational attainment exhibited a bimodal distribution: 36.36% (68/187) had an educational level of junior high school or lower, and 41.18% (77/187) had a college degree or higher. Demographic characteristics revealed that the majority was Han Chinese (93.58%, 175/187), 53.48% (100/187) were unmarried, and 35.29% (66/187) were classified as workers/farmers. 22.99% (43/187) had CD4 + T - cell counts ≥ 500 cells/mm³ without obvious immunodeficiency, while 69.52% (130/187) demonstrated viral loads > 10,000 copies/mL (Table 1).
Genotyping
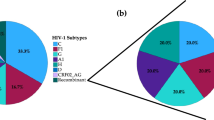
In this study, the gene coding regions of protease/reverse transcriptase (1.3 kb) and integrase (0.8 kb) in the pol region from 173 recently infected individuals were successfully amplified. The sequencing success rate was 92.5% (173/187). Figure 1 indicated that 12 kinds of subtypes were found in this study in total. Of them, the predominant subtypes identified were CRF07_BC (36.4%, 63/173) and CRF01_AE (32.3%, 56/173). URFs accounted for 20.2% (35/173), representing a significant proportion. Additionally, the following subtypes were also detected among recently infected MSM in Hebei Province: CRF55_01B (2.3%, 4/173), B (1.7%, 3/173), CRF59_01B (1.7%, 3/173), CRF65_cpx (1.7%, 3/173), CRF68_01B (1.1%, 2/173), CRF53_01B (0.5%, 1/173), CRF54_01B (0.5%, 1/173), CRF79_0107 (0.5%, 1/173), and CRF120_0107 (0.5%, 1/173) (Fig. 2).
Phylogenetic tree analysis based on HIV-1 pol gene sequences obtained from this study. The neighboring-joining tree was constructed using MEGA 6.0 with 1000 bootstrap replicates. The reference sequences (A–D, F–H, J, K, O, CRF01_AE) were obtained from the HIV database (http://www.hiv.lanl.gov/content/index).
The chi-square test showed that there were significant differences in the distribution of HIV-1 subtypes among MSM with different characteristics: the distribution of CRF01_AE showed obvious difference in different occupational populations; subtype B differed among different CD4 + T-cell count strata; and the distribution of URFs exhibited significant differences in different marital status groups (Table 2).
The chi-square trend test was conducted again. It was found that the distribution of CRF01_AE in different occupational groups showed significant difference (χ² = 17.84, P < 0.001). The distribution of URFs in different marital statuses indecated obvious different (χ² = 6.37, P = 0.040). And,, the distribution of subtype B in different CD4 counts groups was different (χ² = 4.76, P = 0.039), and participants with 350–499 cells/mm³ had the highest proportion of subtype B.
TDR analysis
The overall resistance rate was 7.51% (13/173), which was at a medium prevalence level. There were 4 cases with protease inhibitors (PIs) resistance, with a resistance rate of 2.31%; 1.16% (2/173) had nucleoside reverse transcriptase inhibitors (NRTIs) resistance; 2.31% (4/173) had non-nucleoside reverse transcriptase inhibitors (NNRTIs) resistance; and there were 5 cases with integrase strand transfer inhibitors (INSTIs) resistance, with a resistance rate of 2.89%. Notably, one case exhibited simultaneous resistance to NRTIs, NNRTIs, and INSTIs (Table 3).
Among the 25 ART drugs (8 PIs, 7 NRTIs, 5 NNRTIs, 5 INSTIs) listed in the Stanford HIV Drug Resistance Database, 23 drugs showed low to high level resistance except Darunavir (DRV) and emtricitabine (ETR). The highest resistance rate among PIs was found for Nelfinavir (NFV) (4/173, 2.31%), and 50% of them were high-level resistant. This was followed by Atazanavir (ATV) (2/173, 1.16%), Indinavir (IDV) (2/173, 1.16%), and Saquinavir (SQV) (2/173, 1.16%). Among NRTIs, the drugs with the highest resistance rate were Abacavir (ABC) (2/173, 1.16%), Stavudine (D4T) (2/173, 1.16%), Didanosine (DDI) (2/173, 1.16%), and Tenofovir (TDF) (2/173, 1.16%). Among NNRTIs, the drugs with the highest resistance rate were Efavirenz (EFV) (3/173, 1.73%) and Nevirapine (NVP) (3/173, 1.73%). The resistance rates to EFV and NVP were 66.7% (2/3) and 100% (3/3), respectively. Among INSTIs, the drug with the highest resistance rate was Elvitegravir (EVG) (5/173, 2.89%). The most common mutation sites were G163R (2/173, 1.16%) and R263RK (2/173, 1.16%). It is worth noting that the rate of resistance to INSTIs is slightly higher than other three classes of drugs Table 4.
Distribution of resistant cases in different subtype populations
Among 12 HIV subtypes, CRF55_01B exhibited the highest drug resistance rate (25.0%). Regarding specific drug classes, CRF01_AE showed the highest resistance rates to PIs (3.6%) and NRTIs (1.8%), while CRF55_01B demonstrated the highest resistance rates to NNRTIs (25.0%). For INSTIs, the resistance rate of CRF01_AE was the highest, 7.1%. However, chi-square test results indicated that these differences in resistance rates across subtypes lacked statistical significance (P > 0.05).
Regional distribution of drug-resistant mutations.
Among 173 recently infected individuals from 11 cities of Hebei Province, Baoding had the highest proportion of HIV-1 strains with drug-resistant mutations (45.00%, 9/20), followed by Hengshui (41.67%, 5/12), Xingtai (38.46%, 5/13), Cangzhou (35.00%, 7/20), Handan (33.33%, 2/6), etc. Shijiazhuang (10.00%, 3/30) and Chengde (10.00%, 1/10) had the lowest proportion of such mutations. The chi-square test indicated that the regional distribution of these resistance mutations in the cities show no statistically significant difference (χ² = 14.17, P = 0.163). Consistent with this, the geographical distribution of the 13 TDR patients also showed no statistical significance (P = 0.642). These results suggest that the occurrence of HIV-1 drug resistance mutations and the distribution of TDR are random across the studied cities (Table 5).
Molecular transmission networks
Molecular transmission networks (Fig. 3) indicated that 44 of 173 were circulating in the networks. And, the recently infected individuals with age 18–29 (45.45%, 20/44), CRF07_BC (88.%, 36/44) and unmarried (50.00%, 22/44) were included in networks. And, the CRF07_BC cluster was the largest cluster, containing 34 nodes and 119 lines. In the CRF07_BC cluster, two recently infected individuals contained two mutations (E138G and G163R), resistant to RPV and EVG/RAL, respectively.
Discussion
A comparison with the subtype prevalence among newly diagnosed HIV-1 infections in Hebei Province between 2020–20229,10 revealed that the number and types of HIV-1 subtypes prevalent in the MSM population in Hebei Province in 2023 were almost the same. But, the proportion of different subtypes was not consistent: in our reports in 2018–2022, CRF01_AE (51.9%), CRF07_BC (30.4%) and B (6.2%) were the most predominant subtypes among MSM, however CRF07_BC (36.4%) in this study has been the predominant subtype, exceeding CRF01_AE (32.3%) in 2018–2022, sharing similarities with that in China11. Particularly, URFs accounted for 20.2% has been the third dominant subtype in this study, significantly higher than that (5.8%) in 2018–2022. The epidemic characteristics of different subtypes among recently infected MSM in this study suggests that HIV-1 subtypes will present significant change in the future.
The most recent TDR survey on recently infected HIV-1 MSM in Hebei Province was conducted a decade ago12. This study added recent data on TDR prevalence by conducting drug - resistance studies on recently infected MSM. Compared with that before ten years ago, the TDR prevalence significantly among MSM increased from 2.08% in 2015 to 7.51% in 2023 in Hebei, obviously lower than those in USA (18.9%)13 and Germany (17.8%)14. The individual-class resistance rate of PIs (2.31%), NRTIs (1.16%), and NNRTIs (2.31%) was lower than those (PIs,4.2%; NRTIs ,6.9%; NNRTIs, 12.0%) in USA13. However, the prevalence of INSTI-TDR (2.89%) was higher than those of USA (0.8%), Beijing (0.62%)15, Jiangsu (1.7%)16, lower than higher partial HIV prevalence province such as Yunnan (5.7%)17 and Guangxi (3.1%)18. This suggests that the circulating of HIV-1 TDR strains among recently infected MSM will become the main obstacle in the fight against AIDS. Compared with our previous reports (8.3%) among newly diagnosed treatment-naïve HIV-1 individuals in 2018–202219, the drug resistance prevalence was lower among recently infected individuals in 2023.
INSTIs have been recommended as agents of therapeutic regimes in many countries and regions around the world, including China, because of their high efficiency, good tolerability, and fewer drug - drug interactions20,21. However, since it has not yet been listed as a free antiviral treatment drug in China, its utilization rate is much lower than that of free treatment regimens such as NRTIs, NNRTIs, LPV/r and so on provided by China government22. Currently, the level of integrase resistance among recently infected MSM in Hebei Province is low. Thus, it can be recommended to eligible individuals, but continuous resistance monitoring is still necessary. The fact that INSTIs resistance has been quietly prevalent requires us to consistently test for resistance to the integrase region in the future.
Furthermore, molecular transmission networks identified that youthful individuals aged 18–29, accounting for 45.45%, were circulating in networks. The most of them were unmarried MSM, mainly circulating in the largest CRF07_BC cluster. This reveals that the largest CRF07_BC cluster was very active. And, the CRF07_BC strains resistant to INSTI (EVG/RAL) and NNRTI (RPV) have spread into this population. Currently, MSM is the most predominant transmission route and the prevalence of CRF07_BC is increasing in the Hebei province, suggesting that it is very important for us to take measures to control the diffusing of the resistance strains.
In China, with a treatment-seeking population of over one million, if HIV-1 drug-resistant strains become dominant, these dominant drug-resistant strains will be transmittd to general populations, creating a vicious cycle that is difficult to control. Therefore, apart from monitoring drug resistance in patients who have started treatment, detecting drug resistance in newly infected HIV-1 individuals is of great public-health significance. In the future, we should continue to monitor drug resistance among individuals recently infected with HIV-1, including the resistance related to integrase region, and stay informed about its development. This will enable us to evaluate the effectiveness of the current treatment regimen and make appropriate adjustments to second-line therapies and public-health measures.
It is crucial to emphasize that this study is strictly confined to individuals with recently acquired HIV-1 infection. In contrast, most published data from China were derived from newly reported cases, which were predominantly composed of chronic infections. This fundamental difference in case definitions precludes meaningful direct comparisons and underscores a major methodological gap in current surveillance. In the absence of a nationally representative cohort of recently infected persons, we relied on longitudinal local data to chart temporal trends. The resulting dataset provides a critical benchmark for future standardized national surveillance of recently acquired HIV-1 infections and their resistance profiles.
This study provides a preliminary description of drug-resistance characteristics among recently HIV-1-infected MSM in Hebei Province, establishing a data foundation for subsequent research. Continuous surveillance of drug resistance, including integrase inhibitor resistance, will also be maintained. Together, these efforts will allow us to evaluate the efficacy of current treatment strategies and thus inform targeted refinements to second-line therapies and broader public-health intervention.
Limitations: Subtyping results were classified as low confidence if inconsistencies between coding regions or detectable recombination within a single region were observed. Perhaps because of the small sample numbers, the chi-square test revealed no statistically significant difference in the regional distribution of these resistance mutations.
Materials and methods
Study population and data Sources
This cross-sectional study analyzed all recently infected HIV-1 MSM in Hebei Province, China, who were recorded in the 2023 surveillance database of the CACDIMS. Written informed consent has been obtained from the participants to publish this paper.
Inclusion Criteria:
(1) Participants who have not received ART.
(2) No history of pre-exposure prophylaxis (PrEP) or post-exposure prophylaxis (PEP).
(3) Current residence address is in Hebei Province.
(4) The route of transmission is “MSM”.
(5) Test of limiting antigen avidity enzyme immunoassay (LAg-Avidity EIA) is positive.
(6)Viral Load ≧ 1000 copies/mL.
(7) CD4 cell counts > 200 cells/mm³.
Exclusion Criteria:
(1) Incomplete personal information.
(2) Do not meet any of the inclusion criteria.
HIV-1 RNA extraction, amplification and sequencing
Plasma RNA was extracted using the Nucleic Acid Extraction Kit (Cat. No. 2402007) from Zybio Inc. After reverse transcription, the protease, reverse transcriptase (1.3 kb), and integrase (0.8 kb) gene coding regions within HIV-1 pol were amplified using an in-house method. Subsequently, the amplified products were purified and then sequenced using the Sanger method.
Subtype and drug resistance analysis
The successfully sequenced sequences were edited, spliced, and corrected, and then submitted to the Stanford HIV Resistance Database (https://hivdb.stanford.edu/) for HIV − 1 drug resistance and subtyping. This process enabled the identification of resistance mutation sites and the degree of resistance. The systematic scale categorizes the degree of resistance as S (susceptible), P (potential low - level drug resistance), L (low - level drug resistance), I (intermediate drug resistance), and H (high - level drug resistance). Scores of L ( ≧ 15) and above are recognized as indicating drug resistance. HIV-1 different subtypes were judged via constructing phylogenetic tree and HIV blast (https://www.hiv.lanl.gov/content/sequence/BASIC_BLAST/basic_blast.html), and suspected subtypes were further analyzed using recombination identification tools (jpHMM, RIP 3.0, and SimPlot 3.5.1) to confirm unique recombinant forms (URFs).
Construction of transmission networks
Molecular transmission networks were constructed based on the study pol sequences. Pairwise genetic distances were calculated using HYPHY 2.2.4 with a Tamura-Nei 93 (TN93) model. We selected a genetic distance threshold of 0.015 substitutions/site to construct networks because this threshold is consistent with recent and rapid transmission. Molecular transmission networks were visualized using HIV-Trace-1.5.0.
Data collation and statistical analysis
Data collation and statistical analysis were performed using Microsoft Excel 2021. SPSS 23.0 (IBM SPSS Statistics, USA) was used to conduct the chi - square test, with statistical significance defined as a P - value less than 0.05.
Conclusions
This study provides the first comprehensive TDR profile for recently infected population in Hebei, offering critical insights for regional HIV-1 management.
Data availability
The datasets used and analyzed during the current study are available in the GenBank with the accession numbers PV874282-PV874300, PV929852-PV929871, PV916236-PV916239, PV921469-PV921483, PV921576-PV921588, PV927316-PV927333, PV927348-PV927372, PV929852-PV929871.
References
2024 GLOBAL AIDS update Thematic briefing note: HIV and gay men and other men who have sex with men [EB/OL]. (2023-08-31) [2024-11-12]. https://www.unaids.org/sites/default/files/media_asset/2024-unaids-global-aids-update-gay-men_en.pdf
Stover, J. et al. Updates to the Spectrum/AIM model for the UNAIDS 2020 HIV estimates. J. Int. AIDS Soc. 24 (S5), 10–17 (2021).
Wu, X. Y. & Shen, Y. Z. New advances in antiretroviral therapy for AIDS. Infect. Dis. Info. 32 (1), 81–87 (2019).
Mokgalaboni, K. et al. A systematic review and Meta-Analysis on the impact of Statin treatment in HIV patients on antiretroviral therapy. Int. J. Environ. Res. Public. Health. 20 (9), 5668 (2023).
Wang, X. et al. Short communication: emerging transmitted HIV type 1 drug resistance mutations among patients prior to start of first-line antiretroviral therapy in middle and low prevalence sites in China. AIDS Res. Hum. Retroviruses. 28 (12), 1637–1639 (2012).
Xiong, X. Association between immune activation and disease progression across HIV subtypes. PhD dissertation. China Medical University. (2021).
Su, Y. Y. et al. Distribution and epidemic trends of HIV-1 genetic subtypes in China. Chin. J. Epidemiol. 35 (10), 1164–1168 (2014).
He, X. et al. A comprehensive mapping of HIV-1 genotypes in various risk groups and regions across China based on a nationwide molecular epidemiologic survey. PLoS One. 7(10), e47289. (2012).
Xing, Y. Epidemiological characteristics of novel recombinant strains among newly diagnosed HIV-1 infections in Hebei Province. PhD dissertation. Hebei Medical University. (2022).
Lu, X. et al. Epidemic trend, genetic characteristics, and transmission networks of HIV-1 among treatment-naive men who have sex with men in Hebei province, China. Front. Microbiol. 15, 1405565. (2024).
Ye, J. et al. CRF07_BC is associated with slow HIV disease progression in Chinese patients. Sci. Rep. 12 (1), 3773. https://doi.org/10.1038/s41598-022-07518-4 (2022).
Lu, X. et al. HIV-1 genetic diversity and transmitted drug resistance among recently infected individuals at men who have sex with men Sentinel surveillance points in Hebei Province, China. AIDS Res. Hum. Retroviruses. 31 (10), 1038–1045 (2015).
McClung, R. P. et al. Transmitted drug resistance among human immunodeficiency virus (HIV)-1 diagnoses in the united States, 2014–2018. Clin. Infect. Dis. 74 (6), 1055–1062 (2022).
Melanie, S. et al. Drug resistance spread in 6 metropolitan Regions, Germany, 2001–2018. Emerg. Infect. Dis. 26 (10), 2439–2443. https://doi.org/10.3201/eid2610.191506 (2020).
Song, C. et al. A survey on integrase inhibitor related resistance in HIV-infected persons before antiretroviral treatment in China in 2018 [J]. Chin. J. AIDS STD. 27 (4), 348–351 (2021).
Yu, F. et al. Drug resistance to HIV-1 integrase inhibitors among treatment-naive patients in Beijing, China [J]. Pharmgenomics Pers. Med. 15, 195–203 (2022).
World Health Organization. HIV drug resistance report 2021: November 2021 [EB/OL]. (2021-11-24) [2023-07-03]. https://www.who.int/publications/i/item/9789240038608.
Chang, S. Y. et al. Prevalence of integrase strand transfer inhibitors (INSTI) resistance mutations in Taiwan[J]. Sci. Rep. 6, 35779 (2016).
Lu, X. et al. Drug resistance mutations to integrase inhibitors, proteinase, and reverse transcriptase inhibitors in newly diagnosed HIV-1 infections in Hebei province, China, 2018–2022. Front. Cell. Infect. Microbiol. 15, 1510916 (2025).
Casadellà, M. & Paredes, R. Deep sequencing for HIV-1 clinical management. Virus Res. 239, 69–81 (2017).
Kyeyune, F. et al. Low-Frequency drug resistance in HIV-Infected Ugandans on antiretroviral treatment is associated with regimen failure. Antimicrob. Agents Chemother. 60 (6), 3380–3397 (2016).
Chimukangara, B. et al. Impact of pretreatment low-abundance HIV-1 drug-resistant variants on virological failure among HIV-1/TB-co-infected individuals. J. Antimicrob. Chemother. 75 (11), 3319–3326 (2020).
Funding
This study was supported by the Key Project of Medical Science Research in Hebei Province (Grant No. 20240010).
Author information
Authors and Affiliations
Contributions
X.L. and Q.L. conceived the study project. S.D., Y.W., M.L. and X.X. completed molecular experiment and recent infection test. Y.L. and N.A. completed the test of viral load and CD4 counts. G. B.and L.M. carried out epidemiological investigations. S.D. and X.L. analyzed experimental data and drafted the manuscript. Experimental conditions were provided by Q.L. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical issues
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Local Ethics Committee of Hebei Provincial Center for Disease Control and Prevention. [No. IRB(S)2020-031].
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lu, X., Dong, S., Ma, L. et al. Characterization of transmitted drug resistance among recently infected HIV-1 men who have sex with men in Hebei Province, China. Sci Rep 15, 39382 (2025). https://doi.org/10.1038/s41598-025-26028-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-26028-7