Abstract
To analyze and compare the efficiency of three phaco-emulsifying machines by evaluating parameters related to fluidics and ultrasound time (UST). Pilot, prospective, observational, comparative study conducted at the “Mediterranea” Clinic Ophthalmology Operative Unit, Naples, Italy. A total of 145 consecutive cases of phacoemulsification were included in the study. Patients were randomized into 4 arms and operated using three phaco-emulsifying machines in 4 configurations equipped with three different infusion systems. The phaco machines were: (1) Centurion®, with and without the Active Sentry® handpiece (Alcon), (2) Stellaris Elite™ (Bauch & Lomb), and (3) Whitestar Signature® Pro (Johnson & Johnson). The primary outcomes were UST and fluid aspiration volume. Centurion, with and without Active Sentry, required less UST compared to other phaco machines (P < 0.001). Furthermore, Centurion required lower values of intraocular pressure (IOP) to complete the procedure and aspirated less fluid compared to the Stellaris Elite. No statistical differences in UST, aspirated fluid, and IOP have been found between Centurion and Centurion with Active Sentry. Centurion, with and without Active Sentry required lower UST and IOP for cataract removal compared to Stellaris Elite and Whitestar Signature Pro. Less fluid is necessary to complete the procedure compared to the Stellaris Elite.
Similar content being viewed by others
Introduction
Modern cataract surgery makes use of a wide range of devices optimized for safety and efficiency, aiming at restoring visual function as early as possible. With the introduction of new technologies into the market, it is now possible to achieve favorable postoperative results employing diverse surgical strategies. In recent years, phaco-emulsifying machines have undergone continuous improvements. Despite an increase in complexity, the principle of function is based on the use of a transducer to turn electrical signals into mechanical, ultrasonic, acoustical, and cavitational energy1,2,3,4. To minimize complications, it is desirable to apply the minimal amount of phaco power/energy needed for effective nucleus emulsification. Unnecessary energy output can generate heat, resulting in wound trauma, corneal endothelial cell loss, trabecular meshwork and iris damage, with disruption of the blood-aqueous barrier5,6,7,8.
The safety and efficiency of phacoemulsification depends on the proportion of applied ultrasound (US) energy and fluid exchange in the anterior chamber (AC) during the removal of nuclear material. The reduction in US energy and quantity of fluid used during phacoemulsification has been shown to improve surgical outcomes, while decreasing endothelial cell loss9,10,11,12,13. To optimize results, it is necessary to combine effective and efficient fluidic and US systems.
The purpose of this study is to analyze and compare the efficiency of three phaco-emulsifying machines equipped with three different infusion systems, by evaluating parameters related to fluidics and US time (UST).
Materials and methods
Study design
This is a pilot, single center, prospective, observational, comparative study. Surgery was performed between September 2021 and March 2022. The study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board (Comitato Etico Campania Centro, Italy, Prot. CE 755/40–2021). All eligible patients provided written informed consent.
To minimize variability in the hardness of the cataract nucleus, only patients with grade 3 cataracts according to the Lens Opacities Classification System (LOCS) III were included in the study14. Patients were excluded if they presented with any of the following conditions: pupil that could not dilate to at least 5.0 mm or required mechanical intervention to achieve adequate dilation; pseudo-exfoliative syndrome; floppy iris syndrome; zonular instability; posterior polar cataracts; glaucoma; diabetes; age-related macular degeneration; previous ocular surgeries; other preoperative pathological conditions deemed relevant by the investigators. Patients were also excluded in case of intraoperative complications such as posterior capsular tear, dislocation of cataractous material into the vitreous cavity that required anterior vitrectomy, intraoperative floppy iris, and expulsive hemorrhage.
Before surgery, all patients underwent complete ophthalmologic examination including best-corrected visual acuity (BCVA), slit-lamp biomicroscopy, applanation tonometry, fundoscopy, and specular microscopy.
Phaco machines
The phaco machines used in this study were the Centurion® Vision System using the Active Fluidics™ technology, with and without the Active Sentry® (AS) hand-piece (Alcon Laboratories, Inc.; Fort Worth, TX, USA); the Stellaris Elite™ (Bausch + Lomb, Bridgewater, NJ, USA); the Whitestar Signature™ Pro (Johnson & Johnson Surgical Vision, Santa Ana, CA, USA). Detailed technical characteristics of all the phaco machines are reported in Table 1. The Centurion systems employed a balanced phaco tip with pure torsional ultrasound in burst mode, supplemented by Intelligent Phaco (IP) at a 90% threshold that activated longitudinal ultrasound only to clear tip occlusions. The other phaco machines operated in longitudinal mode. The phaco settings were optimized individually for each phaco machine, focusing on maintaining a stable AC and on minimizing delivered energy. The surgeon decided to set the lowest IOP to avoid AC shallowing and to mitigate the post-occlusion surge effect (Table 1).
Patients were allocated to undergo phacoemulsification with one of the four phacoemulsification systems using simple randomization with a computer-generated random number sequence. Randomization was implemented by P.N. The randomization sequence was inaccessible to the surgeon and the clinical staff involved in patient recruitment. Allocation concealment was maintained until immediately before surgery, when equipment preparation revealed the patient’s assigned group to the surgeon.
Surgical technique
Surgery was performed by the same experienced surgeon (D.B.). All patients underwent a standardized cataract surgery protocol. Briefly, a 2.4-mm near-clear corneal tunnel was created, followed by the injection of intracameral anesthesia (lidocaine 1%) and dispersive viscoelastic agent (DisCoVisc®; 1.6% hyaluronic acid, 4.0% chondroitin sulfate; Alcon Laboratories, Inc., Fort Worth, TX, USA) into the AC. Then, circular curvilinear capsulorhexis, hydrodissection, and phacoemulsification with phaco-chop technique were performed. After removing the remaining cortical with a coaxial irrigation/aspiration hand-piece, a cohesive viscoelastic device was injected and an acrylic intraocular lens (IOL) was implanted. The procedure ended with intracameral injection of 0.1 mg/ml of cefuroxime as antibiotic prophylaxis.
Main outcomes
The main outcomes of the study were: (1) UST, defined as the sum of the time intervals in which the surgeon activated the phacoemulsifier’s ultrasonic tip to emulsify the cataract, and (2) fluid aspiration volume expressed in cubic centimeters (cc).
Statistical analysis
All data were entered into an electronic database via Microsoft Office Excel 365 (Microsoft Corp., Redmond, WA, USA) and analyzed with GraphPad Prism (version 10.3.1; GraphPad Software Inc., San Diego, CA). Preoperative BCVA was assessed with a Snellen chart and converted to the logarithm of the minimum angle of resolution (LogMAR) for the purpose of statistical analysis. The Shapiro-Wilk test was used to assess the normality of data. The Kruskal-Wallis test has been performed to compare independent non-parametric variables across the four study groups. Values for continuous variables are expressed as mean ± standard deviation (95% confidence interval [CI]). A P value < 0.05 was considered significant.
Results
The study included 145 eyes of 145 consecutive patients (68 males, 77 females; age 74.9 ± 6.2 years, range 62–91 years). Patients were divided in 4 groups, according to the phacoemulsifier employed for surgery: (1) Centurion without AS (n = 36), (2) Centurion with AS (n = 37), (3) Stellaris Elite (n = 36), and (4) Whitestar Signature Pro (n = 36). Overall, preoperative BCVA was 0.45 ± 0.15 LogMAR (95% CI, 0.42–0.47). Preoperative IOP was 14.73 ± 2.52 mmHg (95% CI, 14.32–15.14). Detailed baseline characteristics for individual study groups are shown in Table 2.
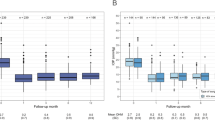
Surgery was completed uneventfully in all cases. The only comparable variable across the four phaco machines was UST. Significantly different USTs were reported across study groups (Centurion = 30.61 ± 9.21 s [95% CI, 27.49–33.73], Centurion with AS = 29.47 ± 9.61 s [95% CI, 26.37–32.57], Stellaris Elite = 42.85 ± 18.3 s [95% CI, 36.87–48.83], Whitestar Signature Pro = 59.15 ± 24.45 s [95% CI, 51.16–67.14]; P < 0.001). Overall, Centurion, both with and without AS, required significantly less UST compared to both Stellaris Elite and Whitestar Signature Pro phacoemulsification systems (always adjusted P < 0.001). Furthermore, the Stellaris Elite required less UST compared to the Whitestar Signature Pro (adjusted P = 0.03). There was no significant difference in UST between Centurion with and without AS. Table 3 shows the mean difference and significancy values for multiple comparisons of the 4 groups, while Fig. 1 shows the findings using box plots.
Concerning fluidics, Stellaris Elite aspirated more fluid compared to both the Centurion and Centurion with AS groups (respectively, 75.31 ± 19.46 cc [95% CI, 68.95–81.66] vs. 51.81 ± 9.531 cc [95% CI, 49.25–54.36] and 49.68 ± 11.85 cc [95% CI, 45.86–53.49]; always P < 0.001) (Table 4; Fig. 2). Fluid aspiration is not detected by the Whitestar Signature™ Pro phacoemulsificator and was not included in the analysis.
In the two Centurion groups, additional intraoperative variables were evaluated and reported in Table 5. There was no significant difference in any parameter between the two configurations.
Discussion
Fluidics and US strategies both play a critical role in the cataract aspiration process. The variability of these two features differentiates the phacoemulsification systems available on market. During phacoemulsification, energy is delivered to the eye in three forms: mechanical, US, and fluid dynamics15. Each company employs various technologies to manage the US system while designing the fluidic components to ensure safety and effectiveness.
The most important aspect of fluidics is the system that each phaco machine uses to deliver BSS into the eye. In our study, we compared three different infusion profiles: the gravity infusion system (Whitestar Signature Pro), the mixed gravity and pressurized infusion system (Stellaris Elite), and the compression of a soft fluid filled bag between metal plates (Centurion). The gravity infusion system enables the infusion by using a glass bottle filled with BSS at a certain height. The bottle’s height over the patient’s head determines the pressure of the BSS in the infusion line16. This approach may be considered suboptimal, because it cannot dynamically adjust the infusion pressure during the surgical procedure.
Instead, the mixed gravity and pressurized system (“Adaptive Fluidic”) combines bottle height with controlled air injection into an incompressible bottle. This setup enables a range of infusion pressures that can be directly correlated with the vacuum level. In the Stellaris Elite, stepping on the foot pedal simultaneously increases both the vacuum and the infusion pressure inside the eye, effectively compensating for the increasing aspiration and flow rates17,18. A significant consequence of the Venturi pump is its requirement for high infusion pressure to balance the intense vacuum levels. This can create turbulence in the AC, leading to endothelial trauma, zonular stress, iris movement and chattering, as well as pain resulting from the zonular tension19,20.
Finally, the “Active Fluidic” system generates the infusion by the compression of a soft fluid-filled bag by two metal plates21. The Active Fluidic can benefit from the AS handpiece, with a pressure sensor positioned on the handpiece on the infusion line and close to the AC. The sensor provides continuous data about the pressure in the eye, can identify IOP fluctuations, and communicates with the control unit of the phaco machine to compensate for the fluctuations of the AC pressure by increasing the pressure into the eye, opening the quick valve device in the cassette in case of a post-occlusion surge, reducing the negative pressure in the aspiration line, and avoiding the shallowing of the AC22.
Energy delivery represents another key factor in phacoemulsification systems. The energy delivered inside the eye depends on the frequency of US, the elongation of the tip, and the type of activation profile of the US themselves. Furthermore, the energy and efficiency of the emulsification process indirectly depends on the shape of the tip, which varies from one brand to another23. The phaco tip represents an integral component of each phacoemulsification system, working synergistically with its specific US modality (longitudinal, torsional, or combined). A tip design optimized for one specific ultrasound modality may not demonstrate the same efficiency when used with a different US system. Since manufacturers’ proprietary technologies prevent tip interchangeability between different systems, and each tip is specifically engineered for its corresponding ultrasound frequency and stroke parameters, we evaluated each phaco machine as a complete integrated system rather than attempting to isolate individual component contributions. A different study design using a single phaco machine with interchangeable tips would be required to specifically assess the impact of tip design on surgical efficiency.
In addition, the real value of energy delivered inside the eye is calculated differently by each phaco machine manufacturer and cannot be directly compared across platforms. Therefore, UST serves as a standardized metric for indirectly evaluating the efficiency of different phaco-emulsifying machines. In our paper, a significant reduction in UST was found for the Centurion and the Centurion with the Active Sentry handpiece compared to the other two phaco machines. The Stellaris Elite showed a notable advantage over the Whitestar Signature Pro, which stands out as the machine requiring the longest UST.
An important feature that expresses the stability and balance of the fluidic system is the working IOP required to complete the cataract aspiration and to obtain a safe and stable AC.
The Centurion system can complete the procedure using very low IOP compared to the Whitestar Signature Pro and the Stellaris Elite. The Centurion with Active Sentry, thanks to the pressure control valve, allows the lowest infusion pressure with respect to the safety and efficiency of the procedure. However, the Centurion without Active Sentry can also work with very low infusion pressure (26 mmHg), while maintaining high standards of safety and efficiency. The Stellaris Elite, leveraging its Adaptive Fluidics technology, effectively compensates for flow and vacuum, ensuring a strong safety profile while dynamically adjusting infusion to accommodate the varying gradients generated by the Venturi pump. Finally, the Whitestar Signature Pro employs the oldest technology, relying on gravity-based infusion determined by bottle height. Since this cannot be adjusted during surgery, the infusion pressure must be set at the highest value to compensate for flow variations and maintain adequate safety and efficiency. Consequently, the volume of fluid used to complete the procedure is lower in the Centurion and Centurion with Active Sentry groups compared to the Stellaris Elite. This comparison could not be performed with the Whitestar Signature Pro because the system does not allow to record the volume of fluid aspirated. Interestingly, the volume of BSS required to complete the procedure depends not only on the IOP but also on the duration of the procedure performed by the surgeon. In our study, the volume of BSS was lower in the group operating at reduced working pressure. This highlights the efficiency of performing the procedure with lower pressure and reduced BSS usage.
The Venturi pump system provides high AC stability together with great efficiency of nucleus aspiration, but it requires a high volume of BSS at higher pressure to balance and stabilize the Venturi effect. The greater attention paid to IOP and volume of BSS is justified by the potential risks associated with high pressure during cataract surgery. High pressure compresses the optic nerve, leading to vessel ischemia, which is particularly threatening for glaucoma patients. It also affects the corneal endothelium, increasing the risk of postoperative edema, and causing greater discomfort in myopic patients with weak zonules19,24.
High working pressure is not only unnecessary but also potentially harmful in case of zonular instability and floppy iris syndrome. It can increase the risk of iris displacement and engagement in the wound, resulting in pain and fraying of the iris.
The Centurion with Active Sentry, through continuous pressure monitoring, operates at the lowest IOP among all tested phaco machines while maintaining safety and efficiency comparable to the standard configuration, with no statistically significant differences in energy delivery or fluid usage. Concerning AC stability and incidence of posterior capsular tear, all the phaco-emulsifying machines demonstrated equal safety.
Although the Sentry group demonstrated lower cumulated dissipated energy and total UST compared to the Centurion group, along with reduced energy and fluid requirements at a lower IOP, these differences were not statistically significant. Centurion and Centurion with Active Sentry required less UST and allow lower IOP levels during cataract surgery in respect to Stellaris Elite and Whitestar Signature Pro systems. Less fluid is necessary to complete the procedure as compared to Stellaris Elite.
To our knowledge, this study presents the first in-vivo comparative analysis between different phaco machines focusing on UST values and on fluidics. However, some limitations deserve mentioning. The absence of a standardized energy model prevented us from comparing the actual energy delivered inside the eye. The necessity of using UST as a practical, measurable proxy is a consequence of the different proprietary algorithms used by different manufacturers to measure the energy delivered by the phaco tip, which depends on many factors, including the elongation of the tip, the frequency of oscillation of the piezoelectric US generator, and finally, the shape and the efficiency of the tip itself. Furthermore, the Whitestar Signature Pro system lacks the capability to measure aspirated fluid volume, preventing comparative analysis of BSS consumption across all tested devices. Finally, while we evaluated the Whitestar Signature Pro, it should be noted that the manufacturer J&J has since released the Veritas™ Vision System as their latest phacoemulsifier model.
In conclusion, our results suggest that both the Centurion and Centurion with Active Sentry outperform the Stellaris Elite and Whitestar Signature Pro in terms of UST and aspirated fluid. This translates to both energy savings and reduced tissue stress. Further research is necessary to confirm these findings and investigate postoperative outcomes.
Data availability
Data are available upon reasonable request by contacting d.boccuzzi78@gmail.com.
References
Hoffman, R. S., Fine, I. H. & Packer, M. New phacoemulsification technology. Curr. Opin. Ophthalmol. 16, 38–43 (2005).
Devgan, U. Phaco fluidics and Phaco ultrasound power modulations. Ophthalmol. Clin. North. Am. 19, 457–468 (2006).
Fishkind, W. J. The Phaco machine: analysing new technology. Curr. Opin. Ophthalmol. 24, 41–46 (2013).
Helvacioglu, F. et al. Comparison of two different ultrasound methods of phacoemulsification. Am. J. Ophthalmol. 158, 221–226e1 (2014).
Fishkind WJ. Evolution of Ultrasound Pumps and Fluidics and Ultrasound Power: From Standard Coaxial Towards the Minimal Incision Possible in Cataract Surgery. In: Alió JL, Fine IH (eds) Minimizing Incisions and Maximizing Outcomes in Cataract Surgery. Berlin, Heidelberg: Springer, pp. 37–49 (2010)
Davison JA. Comparison of ultrasonic energy expenditures and corneal endothelial cell density reductions during modulated and non-modulated phacoemulsification. Ophthalmic Surg Lasers Imaging 38, 209–218 (2007).
Baykara, M., Ercan, I. & Ozcetin, H. Microincisional cataract surgery (MICS) with pulse and burst modes. Eur. J. Ophthalmol. 16, 804–808 (2006).
Badoza, D., Fernández Mendy, J. & Ganly, M. Phacoemulsification using the burst mode. J. Cataract Refract. Surg. 29, 1101–1105 (2003).
Pirazzoli G, D’Eliseo D, Ziosi M, et al. Effects of phacoemulsification time on the corneal endothelium using phacofracture and phaco chop techniques. J Cataract Refract Surg 22, 967–969 (1996).
Kreisler, K. R., Mortenson, S. W. & Mamalis, N. Endothelial cell loss following ‘modern’ phacoemulsification by a senior resident. Ophthalmic Surg. 23, 158–160 (1992).
Colvard DM, Kratz RP, Mazzocco TR, et al. Endothelial cell loss following phacoemulsification in the pupillary plane. J Am Intraocul Implant Soc 7, 334–336 (1981).
Hayashi, K. et al. Risk factors for corneal endothelial injury during phacoemulsification. J. Cataract Refract. Surg. 22, 1079–1084 (1996).
Hoffman RS, Fine IH, Packer M. New phacoemulsification technology. Curr Opin Ophthalmol 16, 38–43 (2005).
Chylack, L. T. et al. The lens opacities classification system III. The longitudinal study of cataract study group. Arch. Ophthalmol. 111, 831–836 (1993).
Liu, Y. et al. Torsional mode versus conventional ultrasound mode phacoemulsification: randomized comparative clinical study. J. Cataract Refract. Surg. 33, 287–292 (2007).
Nicoli, C. M., Dimalanta, R. & Miller, K. M. Experimental anterior chamber maintenance in active versus passive phacoemulsification fluidics systems. J. Cataract Refract. Surg. 42, 157–162 (2016).
Georgescu, D. et al. A fluidics comparison of Alcon Infiniti, Bausch & Lomb Stellaris, and advanced medical optics signature phacoemulsification machines. Am. J. Ophthalmol. 145, 1014–1017 (2008).
Luo, Y. et al. Active-fluidics versus gravity-fluidics system in phacoemulsification for age-related cataract (AGSPC): study protocol for a prospective, randomised, double-blind, controlled clinical trial. BMJ Open. 12, e059062 (2022).
Beres H, de Ortueta D, Buehner B, et al. Does low infusion pressure microincision cataract surgery (LIPMICS) reduce frequency of post-occlusion breaks? Rom J Ophthalmol 66, 135–139 (2022).
Kawasaki, S. et al. Influence of elevated intraocular pressure on the posterior chamber-anterior hyaloid membrane barrier during cataract operations. Arch. Ophthalmol. 129, 751–757 (2011).
Yu L, Guangcan X, Hongyu L, et al. Application of the Active-Fluidics System in Phacoemulsification: A Review. Journal of clinical medicine 12. Epub ahead of print 1 December 2023. DOI: 10.3390/jcm12020611.
Cyril, D. et al. Comparison of two phacoemulsification system handpieces: prospective randomized comparative study. J. Cataract Refract. Surg. 48, 328–333 (2022).
Malik, P. K. et al. Effect of IOP based infusion system with and without balanced Phaco tip on cumulative dissipated energy and estimated fluid usage in comparison to gravity fed infusion in torsional Phacoemulsification. Eye Vis. (Lond). 4, 22 (2017).
Zhao, Z. et al. Elevated intraocular pressure causes cellular and molecular retinal injuries, advocating a more moderate intraocular pressure setting during phacoemulsification surgery. Int. Ophthalmol. 40, 3323–3336 (2020).
Funding
This study was supported by an investigator-initiated study grant from Alcon, Fort Worth, TX (IIT#57527863).
Author information
Authors and Affiliations
Contributions
Conceptualization, D.B, P.N. and G.G; Methodology, D.B., A.T., and G.G.; Validation, D.B., P.N., A.T., and G.G; Formal Analysis, P.N. and A.T.; Investigation, D.B., P.N., and A.T.; Data Curation, D.B. and P.N.; Writing—Original Draft Preparation, D.B., P.N., and A.T; Writing—Review and Editing, A.T. and G.G.; Visualization, D.B., P.N., A.T., and G.G.; Supervision, D.B. and G.G.; Project Administration, D.B. and G.G. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Boccuzzi, D., Napolitano, P., Giannaccare, G. et al. Comparative analysis of fluidics and efficiency among different phaco-emulsifying machines employed for cataract surgery. Sci Rep 15, 45699 (2025). https://doi.org/10.1038/s41598-025-27683-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-27683-6