Abstract
Tuberculosis (TB) remains a global health concern, and healthcare workers (HCWs) face a relatively high risk of TB infection because of their frequent exposure. This study evaluated the effectiveness of a TB infection control education program implemented in Jiangsu Province, China, by assessing changes in HCWs’ knowledge, attitudes, and practices (KAP). This study, carried out from December 2019 to October 2023, included pre- and post-intervention surveys administered to HCWs in selected drug-resistant hospitals. The Wilcoxon rank-sum test was used to assess the changes in KAP scores before and after the implementation. Additionally, multivariate regression and Spearman correlation tests were conducted to explore potential relationships between KAP scores and factors such as gender, age, duration of employment, department, and program participation. The mean score for knowledge and attitudes increased after the implementation (7.40 vs. 9.96, p = 2.769e−15; 35.29 vs. 36.05, p = 0.008652). In contrast, the practice score slightly decreased (39.22 vs. 37.14, p = 0.003767), which may be due to many “not applicable” answers. Moreover, a positive, weak but significant relationship was observed between attitudes and practices. This study revealed significant improvements in knowledge and attitude and a slight decrease in the practice scores, indicating that education led to enhanced knowledge and attitude, but greater efficacy in translating knowledge into practice is needed. The correlation between attitude and practice indicates further efforts to improve HCWs’ attitudes to potentially enhance their practice, thereby diminishing the risk of TB infection.
Similar content being viewed by others
Introduction
Tuberculosis (TB) claimed the lives of 1.25 million individuals in 2023, making it replace COVID-19 and return to the leading infectious cause of death globally1. The World Health Organization (WHO) estimates that 10.8 million people worldwide are infected with TB1. According to the WHO, China ranks among the top five countries most burdened by TB, accounting for approximately 6.8% of the total global cases1. Tuberculosis is prevalent across countries and age groups, yet it is both curable and preventable2.
While the majority of TB cases occur in low- and middle-income countries, this disease is a global concern, especially for healthcare systems worldwide. Healthcare workers (HCWs) are a particularly vulnerable group due to occupational exposure, with the transmission of the disease in healthcare settings posing threats not only to HCWs but also to patients and visitors3. Healthcare workers (HCWs) of inpatient settings in China reported a higher prevalence of tuberculosis infection (TBI). One study revealed that HCWs working in inpatient TB wards faced nearly three times higher TBI compared to those in general medical departments4. The recognized risk comes from close contact with infectious TB patients, particularly during procedures inducing cough, such as bronchoscopy and sputum induction5. Tuberculosis transmission occurs through the air and is capable of traveling long distances. The persistence of multidrug-resistant tuberculosis (MDR-TB) remains a significant public health crisis, with only 2 in 5 individuals with drug-resistant TB accessing treatment in 20226. Multidrug-resistant tuberculosis (MDR-TB) complicates treatment, as it is resistant to at least isoniazid and rifampicin, and extensively drug-resistant TB (XDR-TB) poses an even greater challenge, resistant to the best first- and second-line medications7.
The WHO emphasizes administrative, environmental, and personal protection measures as core components of TB infection prevention and control (IPC), particularly in healthcare settings8. WHO guidelines call for early detection, proper triage, isolation of TB suspects, and protection of healthcare workers through training and personal protective equipment8. China has adopted and adapted these guidelines through its National TB Control Program, which integrates TB IPC into standard healthcare facility protocols. The intervention in this study follows the same protocol used in a collaborative infection control project conducted by the China Centers for Disease Control and Prevention (CDC) and the US CDC9.
While TB infection control programs have been widely implemented across China, their effectiveness at the provincial level has not been thoroughly evaluated. This study helps fill a geographical gap by assessing changes in healthcare workers’ knowledge, attitudes, and practices (KAP) before and after program implementation in six representative hospitals in Jiangsu Province.
This study aims to assess the effectiveness of a TB infection control program among HCWs in China’s Jiangsu Province. Specifically, it evaluates whether an infection control program can lead to improvements in HCWs’ KAP.
Methods
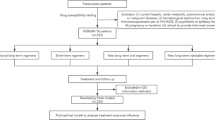
Study design
This study employed a quasi-experimental pre-post design to evaluate the effectiveness of a TB IPC education program among HCWs. This design allows for a practical assessment of changes in KAP before and after the intervention.
Knowledge, Attitudes, and Practices (KAP) surveys play important roles in public health, offering a straightforward way to design, conduct, and interpret valuable information10. They are widely used in the public health field and aid in identifying baseline knowledge, attitudes, beliefs, and behaviors related to specific health topics. They facilitate understanding, analysis, and communication of health-related issues and assist in resource allocation, planning, and implementing public health programs. Knowledge, Attitudes, and Practices (KAP) surveys can also evaluate the effectiveness of intervention programs by measuring changes in knowledge, attitudes, behaviors, and practices post-intervention10. This study was conducted by Jiangsu CDC following the same protocol in a collaborative infection control project by China CDC and US CDC9. All methods were performed in accordance with the relevant guidelines and regulations.
Participants
The study population included HCWs from six designated drug-resistant hospitals in this province. These hospitals were Suzhou Fifth People’s Hospital, Wuxi Fifth People’s Hospital, Changzhou Third People’s Hospital, Yangzhou Third People’s Hospital, Zhenjiang Third People’s Hospital, and Nantong Sixth People’s Hospital. All six hospitals are designated drug-resistant hospitals and have demonstrated good cooperation in previous infection control and surveillance programs. These hospitals are also referral and teaching hospitals and serve as regional centers for diagnosis, treatment, and management of complex TB cases. The selection also ensured geographical diversity across Jiangsu Province, capturing a representative distribution of healthcare settings and TB burden from different cities of Jiangsu Province.
Participants were selected using purposive sampling to ensure representation of various roles. Within each hospital, participation was voluntary, and surveys were distributed to all eligible HCWs who met the inclusion criteria. Inclusion criteria were: (1) currently employed at a designated drug-resistant TB hospital in Jiangsu, (2) willingness to participate in the study. Exclusion criteria included: (1) Interns, temporary workers, or trainees with less than 6 months of clinical experience at the facility, and (2) HCWs who were on extended leave or not available during the intervention period.
The same hospitals, inclusion/exclusion criteria, and survey instruments were used for both the pre- and post-education assessments. Although participants were not individually matched, efforts were made to recruit a similar mix of departments and professional categories during both surveys. This approach helped maintain comparability between groups while allowing for independent participation at each time. Given the non-randomized design, minor variations between pre- and post-survey participants were expected.
Education program
The educational intervention covered three key areas and aligned with WHO and national guidelines: administrative controls, environmental engineering measures, and personal protective practices8.
The TB IC education program commenced in September 2020 and was implemented over 18 months. The faculty members of this program are Chinese program managers for the China–US Infection Control Collaborative Program. The initial phase involved training institutional directors of the infection control department, who were then responsible for carrying on the training to their respective healthcare staff. We collaborated closely with these directors to develop and implement targeted infection control initiatives within their institutions. Following the training, frontline healthcare workers completed KAP surveys to assess the program’s impact.
Questionnaire and quality control
The content of this survey includes basic information such as age, gender, department, years of service, and TB-related knowledge training. It also covers questions related to knowledge, attitude, and practice on TB. The knowledge section includes basic information on the transmission and protection of pulmonary tuberculosis. The attitude items explored key areas such as perceived institutional support, personal responsibility, communication regarding TB symptoms, adherence to protective practices, and willingness to engage in TB health education. The practice section assessed the practical behaviors and clinical routines of HCWs related to TB infection control.
This questionnaire was designed based on the Tuberculosis Building and Strengthening Infection Control Strategies (TB BASICS) by the China CDC9. Content validity was confirmed by an expert panel consisting of specialists in epidemiology, infectious disease, and hospital infection control. Before the main study, the KAP questionnaire was pilot-tested on a small group of healthcare workers not included in the final sample. This allowed for refinement of question wording, item clarity assessment, and average completion time estimation. The reliability and validity of the questionnaire were verified in the pilot survey. The Cronbach’s alpha coefficients were 0.82 for knowledge, 0.85 for attitude, and 0.80 for practice, indicating good internal consistency.
Data collection
Data collection was carried out in two phases: before and after the TB infection control education intervention. Data were collected by the directors of the infection control departments at each institution, all of whom received standardized training prior to the initial data collection. The training covered informed consent procedures, instructions for completing the questionnaire, and protocols for maintaining participant confidentiality.
Data were collected through QuestionStar, an online survey platform, during each phase. The purpose and significance of the study were clearly explained to all participants at the beginning of the questionnaire. Participation was voluntary, and all responses were collected anonymously to protect privacy and encourage honest reporting. To ensure consistency in pre- and post-intervention responses, the same questionnaire format and scoring system were used across both phases.
Sample size calculation
The sample size was determined using item-respondent theory, which recommends a respondent-to-item ratio between 5:1 and 10:111. Given that the questionnaire included 30 KAP items, the estimated sample size ranged from 150 to 300 participants. The final target sample size was adjusted to fall between 180 and 360 participants, considering a 20% drop-out rate. 267 HCWs participated in the pre-intervention survey, and 374 HCWs participated in the post-intervention survey. Both sample sizes fall within the recommended range.
Definitions
The knowledge section includes basic information on the transmission and protection of pulmonary tuberculosis. Five points were given for correct answers to single-choice questions; in the attitude section, four points were given for strongly agreeing with the opinion question, and one point was given for strongly disagreeing with the opinion question; in the practice section, five points were given for completely correct answers to multiple-choice questions; one point was subtracted for correct answers but for choosing one of the other answers (5−X), and deducted until one point; two points were given for incomplete answers; one point was given for incomplete answers and for choosing the other wrong answer at the same time; and for frequency questions, 5 = “always,” 4 = “most of the time,” 3 = “sometimes,” 2 = “rarely,” 1 = “never.”
Data management and statistical analysis
The data were gathered in Excel tables, transformed into scores, and presented as mean ± SD. R 4.2.3 version was employed for proportion calculations. Various statistical analyses were applied to evaluate alterations in KAP scores, including the Wilcoxon rank-sum test, chi-square, Fisher test, and Spearman correlation tests. Additionally, potential associations between KAP scores and variables such as gender, age, employment duration, department, and program attendance were explored via multivariate regression. Statistical significance was determined at a threshold of p < 0.05. Ethical considerations were addressed to ensure the rights and privacy of the study participants. Data confidentiality was maintained throughout the study, and appropriate ethical approvals, if needed, were obtained before data collection.
Results
There were 267 participants included in the pre-program survey. The mean age was 35 years (SD = 10, Table 1), and the average years of service in the current position and organization were 8 years (SD = 9, Table 1) and 11 years (SD = 10, Table 1), respectively. Participants were from a range of hospital departments, with the largest proportion working in internal medicine (51%, Table 1).
Most participants reported prior participation in TB IPC training (88%, Table 1), and 90% (Table 1) had received general infection control training. Regarding institutional infrastructure, 95.5% (Table 1) of participants indicated that their organization had a dedicated infection control department, and a small number were unsure (1.9%, Table 1) or reported the absence of such a department (2.6%, Table 1).
According to Table 2 and 374 HCWs (Table 2) participated in the post-training survey. The mean age of participants was 40 years (SD = 8, Table 2), with an average of 13 years (SD = 9, Table 2) of service in their current position and 14 years (SD = 9, Table 2) within their current organization. Respondents represented various hospital departments, with the largest proportions from internal medicine (23%, Table 2), outpatient departments (18%, Table 2), and the prevention department (12%, Table 2).
Most participants had received prior training related to TB control (87%, Table 2) and infection control (94%, Table 2). Nearly all respondents (98%, Table 2) reported that their organization had a dedicated infection control department. A small proportion either indicated the absence of such a department (1.1%, Table 2) or were unsure (1.3%, Table 2).
The mean age and year of service of the pre-program survey were slightly younger than those of the post-program participants (35 ± 10 vs. 40 ± 8; 8 ± 9 vs. 13 ± 9; 11 ± 10 vs. 14 ± 9; Tables 1 and 2). For the pre-program surveys, the departments with the most representation were internal medicine (51%, Table 1) and tuberculosis outpatient (15%, Table 1), but post-program results featured a more diverse split than pre-training results did, with internal medicine (23%, Table 2), and outpatient department (18%, Table 2) being the most represented fields. Although some variation existed in the distribution of participants across departments, both groups used the same inclusion/exclusion criteria and covered a broad range of clinical areas and staff categories from the same six hospitals, supporting general comparability between the two surveys.
The majority of participants had undergone TB IPC training and/or infection control training within the last 12 months (Tables 1 and 2). The participation rates in TB IPC training remained consistent before and after program implementation, at 88% (Table 1) and 87% (Table 2), respectively. In contrast, the participation rate in infection control training increased from 90% to 94% (Tables 1 and 2). Moreover, the total number of participants, average age, year of service, departmental diversity, and training participation increased in the post-training survey.
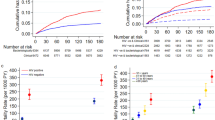
Tables 3 and 4 present the distribution of good and poor KAP scores among HCWs pre-training and post-training, respectively, regarding demographic aspects.
In Table 3, the pre-training data displays significant differences in knowledge scores based on the years of service in position (p-value = 0.012, Table 3) and organization (p-value = 0.041, Table 3). HCWs less experienced in their positions and organizations generally demonstrated poor knowledge. Additionally, it also reveals that participation in TB control training does not significantly impact knowledge, but it does affect substantially attitudes (p-value = 0.020, Table 3) and practices (p-value\(\:<\)0.001, Table 3). Moreover, participation in general infection control training does not significantly influence knowledge (p-value=0.473, Table 3) and attitude (p-value = 0.074, Table 3) but does impact practice (p-value = 0.034, Table 3).
Table 4 suggests that in the post-training survey, only attitude is significantly impacted by participation in both TB control training and infection control training (TB control training: p-value\(\:<\)0.001, Infection control training: p-value = 0.038; Table 4). No significant difference was observed in practice across HCWs who participated in the training and those who did not.
Service time appeared to influence knowledge, and training had a greater impact on attitudes and practices than on knowledge. Moreover, the influence of these demographic factors on knowledge and practice decreased but remained significant for attitude. These results may indicate that a comprehensive approach should be considered when implementing TB control and infection control training, ensuring that knowledge levels are improved along with attitude improvements and practical application.
Tables 5 and 6 show the correlations between knowledge, attitude, and practice (KAP). Notably, the correlation between practice and attitude is weakly positive and statistically significant (rho = 0.122, p-value = 0.045, Table 5; rho = 0.103, p-value = 0.045, Table 6). This program impacted the relationships between knowledge, attitude, and practice variables. Both pre-program and post-program correlations between attitude and practice remained positive and significant. The positive correlation between attitude and practice indicates that the improvement of attitude will have a favorable impact on the good practice of HCWs.
Table 7 compares the mean scores of knowledge, attitudes, and practices before and after the implementation. The mean score for knowledge before the program initiation was 7.40 (SD = 4.81, Table 7). After the program was implemented, the mean knowledge score increased to 9.96 (SD = 3.33, Table 7). There was a slight increase in the mean score of attitude, from 35.29 (SD = 3.40, Table 7) before the program to 36.05 (SD = 3.55, Table 7) after the program. The increase in the mean scores of knowledge and attitudes shows that the program had a positive influence on participants’ knowledge. (Knowledge: p-value < 0.001, Table 7; Attitude: p-value = 0.008652, Table 7). However, the mean score of practice decreased from 39.22 (SD = 13.34, Table 7) to 37.14 (SD = 15.15, Table 7) after the implementation of the program, which may be due to many “not applicable” answers. The distribution of participants across departments differed slightly between the pre- and post-education surveys. These variations may have influenced KAP outcomes to some extent. Still, the overall improvement patterns in knowledge and attitude remained consistent across departments, which may suggest that the intervention’s effect is not confined to a single clinical area.
In addition, we have noticed changes in the frequency of replacement of protective masks. Healthcare workers tend to change masks more frequently after the program implementation. The proportion of masks changed every 4–6 h increased substantially, from 1.50% before the project to 6.15% after the project (Table 8). 15.73% of HCWs reported replacing masks by half a day before the program initiation, which significantly increased to 46.52% after the implementation (Table 8). Moreover, HCWs who changed masks daily decreased from 52.43 to 30.21% (Table 8). However, we noticed that never using masks increased from 6.12 to 12.03% (Table 8).
Discussion
This study aimed to assess the effectiveness of a TB infection control program on HCWs based in Jiangsu Province, China. Our primary focus was to evaluate the effects of our intervention and measure any significant changes in the KAP of HCWs.
Our findings revealed an overall improvement in the knowledge and attitudes of HCWs after the infection control program. Following the implementation of the program, there was a statistically significant improvement in both knowledge and attitude scores among HCWs. The mean knowledge score increased from 7.40 to 9.96 (p < 0.001, Table 7), while the mean attitude score rose from 35.29 to 36.05 (p = 0.009, Table 7). These findings indicate that the intervention was important in enhancing participants’ understanding and perspectives regarding TB infection control. Education works well in boosting knowledge and shaping attitudes. This study aligns with research conducted in Egypt among the general population, which also demonstrated a significant improvement in knowledge about TB12. Similarly, studies in South Africa and China have shown that structured educational programs can lead to substantial increases in TB knowledge and awareness13,14,15. Our intervention not only improved knowledge but also positively influenced the attitudes of HCWs toward TB, which is important to long-term prevention and control efforts. Similar results were shown in a study among health professionals in Ethiopia, where education led to better attitudes toward TB control and prevention16. Improvements in knowledge and attitudes among HCWs are critical to sustaining TB IPC, especially in high-burden settings, as they contribute to more consistent adherence to infection control practices, reduce stigma associated with TB patients, and promote proactive identification and management of potential TB cases.
Contrary to expectations, a decrease in practice scores was observed (39.22 to 37.14, p = 0.046, Table 7). The decrease in practice scores was attributed mainly to an increase in “not applicable” responses, which may suggest a need to bridge the gap between knowledge acquisition and its practical application among HCWs. Although they may have gained knowledge, the challenge lies in translating that knowledge into everyday practice within their specific roles, as they may not have opportunities to apply it. Therefore, more considerations and research may be needed to effectively improve good practice when designing and implementing the infection control (IC) education program.
Our results showed that TB-related training alone does not guarantee adequate IC practices. While possessing proper knowledge is recognized as a predictor of good IC practice, it is important to note that good knowledge does not guarantee adequate IC practices16,17,18. It is critical to evaluate whether training programs lead to meaningful improvements in IC practices. Other studies have similarly reported suboptimal preventive practices despite high awareness and availability of services19,20. Likewise, relatively good TB knowledge among healthcare workers was not consistently reflected in their practices21. To address this, a shift towards skill-based training using adult learning approaches is crucial to modify HCWs’ behavior and improve IC practices in health facilities17.
The implementation of IC measures may also depend on HCWs’ attitudes and motivation. Even with an appropriate attitude toward TB infection control, concerns such as the risk of infecting family members or potential financial consequences can influence daily practices22,23. Our findings showed limited improvement in proper mask use and replacement frequency, possibly due to TB-related stigma. Some HCWs reported avoiding respirators to ensure patient comfort, a practice linked to negative perceptions of TB24. Although HCWs possessed relatively good knowledge about TB, this did not translate into significant improvements in practice or a reduction in stigma associated with the disease.
Furthermore, a weak, positive correlation was found between attitude and practice (rho = 0.122, p = 0.045, Table 5; rho = 0.104, p = 0.045, Table 6), which aligns with another study about Osteoporosis KAP in Malaysia25, where the researchers also found a weak, positive correlation only between attitude and practice. It suggests that improving HCWs’ attitudes may help to enhance their clinical practice, thereby reducing the risk of TB infection.
Finally, the HCWs’ demographic characteristics might have influenced KAP results. In this study, the employment duration also influenced the KAP scores. HCWs with longer service time appeared to have greater knowledge of TB control, but the practice did not increase proportionally. This result also suggests the existence of possible challenges in translating knowledge and positive attitudes into practical action. Our findings also reveal that infection control training, both general training and TB-specific training, has a greater effect on HCWs’ attitudes but does not have consistent effects on practice. The reason may be attributed to the large number of “not applicable” responses in post-training surveys. These findings suggest the need for greater efficacy in translating knowledge into practice. Future interventions could focus on on-the-job training, simulations, or case studies that directly relate to the daily challenges faced by healthcare workers. Identifying and addressing these specific challenges could bridge the gap between knowledge and practical application26.
It should also be noted that the data collection period (2019–2023) overlapped with the COVID-19 pandemic. This global public health emergency may have influenced HCWs’ awareness, attitudes, and behaviors regarding IPC. The heightened emphasis on respiratory protection, personal protective equipment (PPE) use, and infection control practices during COVID-19 likely reinforced HCWs’ general awareness and attitudes toward airborne disease prevention, potentially contributing to the improved knowledge and attitude scores observed post-intervention. This could partly explain the discrepancy between improved knowledge and attitude but decreased practice scores.
Study limitations
This study has several limitations. First, the study employed a pre-post design without a control group, limiting the ability to attribute observed changes to the intervention. Second, different participant groups were involved in the pre- and post-surveys. While both groups were drawn from the same six designated drug-resistant hospitals using the same inclusion and exclusion criteria, differences in demographic characteristics were observed. This may introduce potential selection bias, as the post-intervention group may have had different baseline characteristics that could influence KAP outcomes independently of the intervention. To address potential confounding, we applied multivariate statistical adjustments during the analysis. These included controlling for age, gender, years of service, department, and prior training experience. These steps might help reduce bias, but the lack of a matched or randomized control group remains a limitation and may reduce the strength of causal inference. However, the consistent direction of improvement in knowledge and attitude across diverse healthcare departments suggests that the overall findings remain robust. Future studies using matched or longitudinal designs could better control for such compositional differences. Third, the study recognizes the reliance on self-reported data as a limitation. Although surveys are a common method for collecting information, they may be subject to response bias or social desirability bias. Participants might provide answers they perceive as socially acceptable, potentially influencing the accuracy of the KAP scores. The voluntary nature of participation may have introduced non-response bias; HCWs with stronger opinions or higher engagement in infection control may have been more likely to complete the survey. Finally, we acknowledge the challenge of many “not applicable” answers in the practice survey. This limitation can affect the interpretation of the results. These shortcomings of this research have enabled us to know the direction for future improvement. Therefore, we will keep on following up with HCWs enrolled in the post-training evaluation to enhance the validity and reliability of future research.
Conclusions
This study demonstrated that a structured TB IC education program led to significant improvements in knowledge and attitudes among HCWs in Jiangsu Province, China. While the increased knowledge and positive attitudes are encouraging, the decrease in practice scores post-training indicates that more emphasis must be placed on the applicability of these interventions in everyday healthcare work.
Concerning future research, a deeper exploration of why knowledge does not necessarily translate into good practice could be beneficial. Additionally, other influencing factors such as workplace culture, resources, and system-level policies could be examined more closely.
This study highlights the importance of TB infection control programs for HCWs’ knowledge and attitudes. The decrease in practice scores suggests the need for a more integrated approach that not only equips HCWs with knowledge but also ensures that it directly influences patient care practices. By addressing these gaps, we can enhance the effectiveness of such programs and thereby make significant improvements in TB control.
Data availability
The data analyzed in this study are not publicly available as individual privacy would be compromised. The data that support the findings of this study are available from the author, D. J., upon reasonable request.
Abbreviations
- TB:
-
Tuberculosis
- WHO:
-
World Health Organization
- HCW:
-
Healthcare worker
- TBI:
-
Tuberculosis infection
- MDR-TB:
-
Multidrug-resistant tuberculosis
- XDR-TB:
-
Extensively drug-resistant TB
- IPC:
-
Infection prevention and control
- CDC:
-
Centers for Disease Prevention and Control
- KAP:
-
Knowledge, attitude and practice
- TB BASICS:
-
Tuberculosis building and strengthening infection control strategies
- IC:
-
Infection control
- PPE:
-
Personal protective equipment
References
Global Tuberculosis Report. 1st ed. 1 (World Health Organization, 2024).
Tobin, E. H. & Tristram, D. Tuberculosis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 [cited 2024 Sep 11]. http://www.ncbi.nlm.nih.gov/books/NBK441916/
Paleckyte, A., Dissanayake, O., Mpagama, S., Lipman, M. C. & McHugh, T. D. Reducing the risk of tuberculosis transmission for HCWs in high incidence settings. Antimicrob. Resist. Infect. Control. 10 (1), 106 (2021).
Deng, Y. et al. Isolation measures and protection awareness are significant for latent tuberculosis infection: a cross-sectional study based on T-SPOT. TB among health care workers in China. Epidemiol. Infect. 147, e120 (2019).
The prevalence and risk factors for tuberculosis among healthcare workers in. Yogyakarta, Indonesia—PMC [Internet]. [cited 2024 Sep 11]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10194884/
Tuberculosis (TB). [Internet]. [cited 2023 Dec 25]. https://www.who.int/news-room/fact-sheets/detail/tuberculosis
Seung, K. J., Keshavjee, S. & Rich, M. L. Multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis. Cold Spring Harb. Perspect. Med. 5 (9), a017863 (2015).
WHO Consolidated Guidelines on Tuberculosis. Module 1: Prevention - Infection Prevention and Control 1st edn, 1 (World Health Organization, 2022).
Zhang, C. et al. Indicator-based tuberculosis infection control assessments with knowledge, attitudes, and practices evaluations among health facilities in China, 2017 to 2019. Am. J. Infect. Control. 53 (4), 506–513 (2025).
Andrade, C., Menon, V., Ameen, S. & Kumar Praharaj, S. Designing and conducting knowledge, attitude, and practice surveys in psychiatry: practical guidance. Indian J. Psychol. Med. 42 (5), 478–481 (2020).
Costello, A. B. & Osborne, J. Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 10(1) (2005). https://openpublishing.library.umass.edu/pare/article/id/1650/
El-Gilany, A. H., El-shaer, S., Khashaba, E., El-dakroory, S. A. & Omar, N. Knowledge, attitude, and practice (KAP) of ‘teaching laboratory’ technicians towards laboratory safety and waste management: a pilot interventional study. J. Hosp. Infect. 96 (2), 192–194 (2017).
Zhang, Y., Wu, J., Hui, X., Zhang, P. & Xue, F. Knowledge, attitude, and practice toward tuberculosis prevention and management among household contacts in Suzhou Hospital, Jiangsu province, China. Front. Public Health. https://doi.org/10.3389/fpubh.2024.1249971/full (2024).
Kanjee, Z., Catterick, K., Moll, A. P., Amico, K. R. & Friedland, G. H. Tuberculosis infection control in rural South africa: survey of knowledge, attitude and practice in hospital staff. J. Hosp. Infect. 79 (4), 333–338 (2011).
Hassan, A. O. et al. Knowledge about tuberculosis: A precursor to effective TB Control—Findings from a Follow-Up National KAP study on tuberculosis among Nigerians. Tuberc. Res. Treat. 2017 (1), 6309092 (2017).
Temesgen, C. & Demissie, M. Knowledge and practice of tuberculosis infection control among health professionals in Northwest Ethiopia; 2011. BMC Health Serv. Res. 14(1), 593 (2014).
Shrestha, A., Bhattarai, D., Thapa, B., Basel, P. & Wagle, R. R. Health care workers’ knowledge, attitudes and practices on tuberculosis infection control, Nepal. BMC Infect. Dis. 17 (1), 724 (2017).
Engelbrecht, M., Janse van Rensburg, A., Kigozi, G. & Dingie van Rensburg, H. Factors associated with good TB infection control practices among primary healthcare workers in the free state Province, South Africa. BMC Infect. Dis. 16 (1), 633 (2016).
Bisallah, C. I. et al. Effectiveness of health education intervention in improving knowledge, attitude, and practices regarding tuberculosis among HIV patients in general hospital Minna, Nigeria—A randomized control trial. PLoS One. 13 (2), e0192276 (2018).
Shihora, J. et al. Attitudes, and preventive practices regarding tuberculosis among healthcare workers and patients in India: A mixed-method study. Cureus. 16(3) (2024). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC11022008/
Hashim, D. S., Al Kubaisy, W. & Al Dulayme, A. Knowledge, attitudes and practices survey among health care workers and tuberculosis patients in Iraq. EMHJ East Mediterr. Health J. 94, 718–731 (2003). https://iris.who.int/handle/10665/119325
Woith, W. M., Volchenkov, G. & Larson, J. L. Barriers and facilitators affecting tuberculosis infection control practices of Russian health care workers. Int. J. Tuberc. Lung Dis. Off J. Int. Union Tuberc. Lung Dis. 16 (8), 1092–1096 (2012).
Jelip, J. et al. Risk factors of tuberculosis among health care workers in Sabah, Malaysia. Tuberculosis 84 (1), 19–23 (2004).
Kallon, I. I. et al. Organisational culture and mask-wearing practices for tuberculosis infection prevention and control among health care workers in primary care facilities in the Western Cape, South africa: A qualitative study. Int. J. Environ. Res. Public. Health. 18 (22), 12133 (2021).
Khan, Y. H., Sarriff, A., Khan, A. H. & Mallhi, T. H. Knowledge, attitude and practice (KAP) survey of osteoporosis among students of a tertiary institution in Malaysia. (2014). https://tspace.library.utoronto.ca/handle/1807/61291
Zhao, F. et al. The current status and challenges regarding tuberculosis infection control in health care facilities in China. Biomed. Environ. Sci. 28, 848–854 (2015).
Acknowledgements
We would like to thank the participants from hospitals for their active participation in the training and their cooperation in filling out the questionnaire.
Funding
This work was supported by Jiangsu Provincial Medical Key Discipline (grant number ZDXK202250), Jiangsu Young Medical Talents Project (QNRC2016541) and Jiangsu Province Fifth and Sixth Phase of the “333 High-Level Talent Training Project” Plan.
Author information
Authors and Affiliations
Contributions
Y.L. and L.Z. conceptualized the study and collected and curated the data. H.S. and G.L. were responsible for the organizational work at the project site and the collection of questionnaires. J.X. and D.J. performed the formal analyses and drafted the manuscript with critical revisions by Y.L. All of the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The studies only involve the collection of survey questionnaires from staff and do not involve human or animal samples has been reviewed and approved by the Ethics Review Committee of Jiangsu Provincial Center for Disease Control and Prevention, and all participants provided written informed consent prior to their participation. The Ethics Authorization Number: JSCDCLL(2020) 025.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jia, D., Song, H., Li, G. et al. Evaluation of tuberculosis education effects on healthcare workers’ knowledge attitudes and practices in Jiangsu China 2019 to 2023. Sci Rep 15, 44437 (2025). https://doi.org/10.1038/s41598-025-28031-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-28031-4