Abstract
Although various studies have been conducted on food allergy worldwide, large-scale population-based data on food allergen sensitization patterns in South Korea remain limited. In this study, we analyzed age- and sex-specific sensitization patterns to various food allergens by analyzing large-scale multiple allergen simultaneous test (MAST) data. In this study, we analyzed the results of MASTs performed for 344,678 patients with suspected allergies (0.66% of South Korea’s total population) nationwide. The dataset included specific immunoglobulin E (IgE) levels for 56 food allergens, with class 2 (0.70–3.49 IU/mL) or higher indicating sensitization. The age-related pattern of sensitization differed for each allergen category: plant-based, animal-based, and shellfish. All plant-based food allergens exhibited a high sensitization rate between ages 1 and 20 years and reached a second peak between ages 51 and 70 years. The sensitization rate to animal-based food allergens was notably high between ages of 1 and 10 years but rapidly declined thereafter. In the case of the shellfish category, the sensitization rate was high from ages 11–20 years age group and remained consistent until ages 61 to 70 years. Overall, the sensitization rate to all plant-based foods and shellfish was significantly higher in male participants than in female participants. However, there was no sex difference in animal-based food allergens. Food allergens that induce sensitization vary across different age group, and each allergen category exhibits a distinct pattern of sensitization change by age.
Similar content being viewed by others
Introduction
Food allergies differ from respiratory allergies owing to their diverse pathological mechanisms. Generally, food allergy prevalence can be estimated through various approaches, including self-reported questionnaires, oral food challenge (OFC) tests, and specific IgE or skin test results reflecting allergen sensitization1,2. Among these, OFC provides the most accurate confirmation of clinical allergy but is limited by ethical and safety concerns. In contrast, IgE-based testing allows large-scale evaluation of sensitization patterns in the general population, which can serve as an indirect indicator of potential allergy prevalence1,2. Consequently, diagnosis predominantly relies on a detailed medical history, results from skin prick tests or specific IgE assays targeting suspected allergens, and, in some cases, the basophil activation test as a complementary diagnostic tool1,2. However, in the case of non-IgE-mediated food allergy, where skin prick tests or specific IgE assays may yield negative results, specialized tests such as patch tests, human leukocyte antigen typing, or, when necessary, the double-blind placebo-controlled food challenge may be required1,2.
Food allergy prevalence varies widely among countries and regions, influenced by genetic, environmental, and dietary factors. Reported prevalence rates of food allergy, including self-reported symptoms, vary widely across studies ranging from 1.1% to 25% depending on study design and diagnostic criteria3,4,5. The prevalence of food allergy and the common allergens that cause food allergy vary greatly between countries. According to a meta-analysis, overall prevalence of food allergy was 4.3%; 4.2% in Asia, 3.2% in the United States, 4.8% in Europe, 1.6% in Africa, and 7.5% in Oceania6. However, this prevalence also varies greatly depending on the diagnostic method of food allergy. Another meta-analysis shows that the prevalence of food allergy in Europe was 16.6% by specific IgE measurement, 5.7% by skin prick test, and only 0.8% by oral food challenge test7. Common food allergens worldwide include milk, egg, peanut, nuts, shellfish, fish, soya, and wheat. However, the specific foods responsible for allergic sensitization vary greatly between studies and regions6. However, in South Korea, nationwide large-scale studies encompassing diverse age groups are limited, and most available data have been derived from small, hospital-based, or pediatric populations8,9,10. Therefore, a population-level analysis using objective IgE-based testing is needed to better understand the distribution of food allergen sensitization across different age and sex groups.
To address these gaps, we analyzed data from a nationwide multiple allergen simultaneous test (MAST) database comprising 344,678 individuals with suspected allergies, corresponding to approximately 0.66% of South Korea’s total population. The dataset includes information on age, sex, and specific IgE levels for a wide range of food allergens, enabling a comprehensive analysis of sensitization trends by age and sex. Although sensitization alone cannot serve as a diagnostic criterion for food allergy, its presence suggests a high likelihood of food allergy, even in the absence of current symptoms, considering the potential for future manifestations1,2. Furthermore, assessing sensitization rates across different age groups is valuable for understanding the natural course of food allergies.
Materials and methods
Study population
We analyzed the results of the MAST (PROTIA Allergy-Q 96 M panel, ProteomeTech Inc., Seoul, Korea) shared by a local medical diagnostics firm (Seegene, Seoul, Korea). The PROTIA Allergy-Q 96 M (ProteomeTech Inc., Seoul, Korea) is a multiplex fluorescent immunoassay that simultaneously measures specific IgE levels against multiple allergens using a nitrocellulose membrane-based platform. The assay was performed according to the manufacturer’s instructions (ProteomeTech Inc.; https://www.proteometech.com). Between January 2, 2018, and June 30, 2021, a total of 368,156 MASTs were conducted nationwide in 3,735 primary care clinics and secondary/tertiary hospitals. After excluding duplicate tests from the same patient, cases with missing information, and individuals aged 0 or > 90 years due to a heightened risk of input errors, data from 344,678 unique patients were included in the final analysis. The MAST was conducted for patients who presented to clinics or hospitals with suspected allergic diseases, including respiratory, cutaneous, or food-related symptoms, as determined by the attending physician. Unfortunately, access to medical records detailing the symptoms, diagnoses, and physical findings was not feasible. The dataset encompassed information such as sampling date, sex, age, and specific IgE levels for 56 food and 48 inhalant allergens. For analysis, the 56 food allergens were grouped into three categories based on biological origin: (1) plant-based (e.g., peanut, soybean, wheat, fruits, and vegetables), (2) animal-based (e.g., milk, egg, meat, and fish), and (3) shellfish (e.g., shrimp, crab, lobster, and squid). The detailed list of allergens included in each category is presented in Supplementary Table S1.
Depending on the level of IgE, the results are graded into 7 classes as follows: class 0 (0.00–0.34 IU/mL), class 1 (0.35–0.69 IU/mL), class 2 (0.70–3.49 IU/mL), class 3 (3.50–17.49 IU/mL), class 4 (17.50–49.99 IU/mL), class 5 (50.00–99.99 IU/mL), class 6 (≥ 100 IU/mL). Class 2 or higher classes were indicative of sensitization. Sensitization was defined as Class 2 or higher (≥ 0.70 IU/mL) based on the manufacturer’s recommended cut-off and previous Korean population-based studies using the same MAST platform, which reported higher specificity at this threshold compared with the lower 0.35 IU/mL cut-off used in other IgE assays.
Data analysis
The participants were classified into different age groups, divided by 10-year intervals. The sensitization rate for each allergen was calculated for each age group and separately for male and female participants. Statistical inference was not performed.
Results
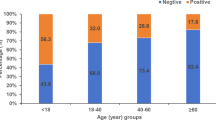
A total of 344,678 MAST results were analyzed. The distribution across each age group was as follows: 1–10 years (91,547), 11–20 years (34,935), 21–30 years (45,989), 31–40 years (46,528) 41–50 years (41,990), 51–60 years (42,061), 61–70 years (28,611), and > 70 years (16,537). The table summarizes the sensitization rates for each food allergen by age group. Notably, 32 food allergens with sensitization rates of 4% or less in all age groups were excluded, and only the remaining 24 were included. A Full lists of the 56 food allergens—including those with sensitization rates below 4%—and the 48 inhalant allergens are provided separately in Supplementary Tables S1 and S2. Food allergens with high sensitization rates differed across different age groups. The common allergens (exceeding 8% prevalence) for participants aged 1–10 years included peanut, egg white, cow’s milk, and beef; for those aged 11–20 years, they included peach, beef, shrimp, and silkworm pupae; for those aged 21–40 years, they included shrimp and silkworm pupae; and for those aged 41–70 years was potato.
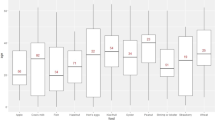
The pattern of change in sensitization according to age was different for each category of allergens (Fig. 1; Table 1); (1) All plant-based food allergens exhibited a high sensitization rate between ages 1 and 20 years, followed by a decrease between ages of 21 and 30 years, and then gradually increase, reaching a second peak between ages 51 and 70 years. These changes according to age group were very noticeable in male participants, and the extent of change was small in female participants. The sensitization rate was higher in male participants in all age groups, and this difference was largest at 51–60 years of age; (2) The sensitization rate to animal-based food allergens (egg white, cow’s milk, and beef) was notably high in participants aged 1–10 years, which rapidly declined thereafter. There was no difference in sensitization rate between male and female participants for this category of allergens; (3) In the case of shellfish (including silkworm pupae), the sensitization rate was higher in participants aged 11–20 years than in those aged 1–10 years, and the rate remained similar until ages 61–70 years. The rate of sensitization to shellfish was significantly higher in male participants than in female participants, and this difference was largest at 21–30 years of age. Sensitization rates by sex are provided in the Supplement.
Discussion
Most studies on the prevalence of food allergies in Korea have been conducted in children. The prevalence rate differed somewhat between studies. Kim et al. compared several surveys targeting elementary school students in Korea and found an increasing trend from 4.6% in 1995 to 6.6% in 201211. Common allergens identified in several studies were egg whites, cow’s milk, and peanuts11. Few studies have been conducted on adults; however, the prevalence of food allergies in patients with other allergic diseases has been reported in previous studies. For instance, 41.7% of patients with pollen allergies had food allergies, 13.1% had chronic urticaria, and 51.1% had atopic dermatitis, indicating that food allergies have a high comorbidity with other allergic diseases12,13,14. The types of common allergens also differed across different studies. In a study including 95 adult patients diagnosed with food allergies, the most common allergens were shellfish such as shrimp and crab (34.8%)15. In another study involving 415 adult patients, the most common allergens were fruit (47.6%), shellfish (26.7%), wheat (15.1%), buckwheat (7.4%), peanuts (7.4%), walnuts (6.0%), meat (1.9%), and silkworm pupae (3.1%)16. These discrepancies may be explained by differences in study populations, geographic regions, diagnostic methods, and dietary habits. In addition, some studies were hospital-based and included patients with pre-existing allergic diseases, which may have influenced the allergen distribution.
Among the allergens with sensitization rates below 4%, many corresponded to foods that are rarely consumed in Korea (e.g., certain exotic fruits and nuts). Limited dietary exposure may explain the very low sensitization rates to these items. Thus, this study reaffirmed that food allergens with high sensitization rates (exceeding 8% prevalence) differed across age groups. Peanuts, egg whites, milk, and beef were common among participants aged 1–10 years, and peaches, beef, shrimp, and silkworm pupae were common among those aged 11–20 years. Among participants aged 21–40 years, shrimp and silkworm pupae were common allergens, whereas potatoes were common allergens among those aged 41–70 years. Another possible explanation for the age-related sensitization patterns is the generational difference in dietary exposure. Older age groups may have been more frequently exposed to certain traditional foods, such as shellfish and silkworm pupae, during their youth, whereas younger generations consume more processed or Westernized foods. These differences in historical dietary patterns may have contributed to the observed sensitization trends in different age groups. It should be noted that patients with atopic dermatitis often exhibit broad IgE sensitization patterns that may not always correspond to clinically relevant allergies. The prevalence of atopic dermatitis in the Korean population may therefore contribute to the wide range of sensitization observed in our study.
However, we found that the pattern of change in sensitization rate based on age group was broadly divided into three types as follows17: (1) for all plant-based food allergens, sensitization rates were high before 10 years of age, subsequently decreasing at 20–30 years and reaching a second peak at 50–70 years. Although the exact mechanism that could explain this bimodal peak has not been identified, it is suspected that pollen-food allergy syndrome is involved12. (2) the sensitization rate to animal-based food allergen (hen’s eggs, cow’s milk, and beef) was observed under 10 years of age and declined rapidly thereafter. This pattern of sensitization changes is reported similarly in most studies, with food allergy to animal-based foods disappearing faster than those to plant foods1,2. (3) In the case of shellfish and silkworm pupae, the sensitization rate was low under 10 years of age but then increased rapidly and remained consistently high thereafter. Silkworm pupae are traditional Korean foods that are usually boiled and consumed; however, their consumption has decreased in recent years. Despite this, the sensitization rate to silkworm pupae remains high, likely due to cross-reactivity with shellfish allergens. Both silkworm pupae and shellfish contain tropomyosin18, a heat-stable muscle protein that also exists in house dust mites, one of the most common aeroallergens in Korea. This cross-reactivity may account for the sustained high sensitization rates to silkworm pupae and shellfish observed in our study19,20.
The difference in food allergy prevalence between men and women is well documented. In general, the prevalence is higher in men in younger age groups; however, in adults, women are more affected by food allergies21. Additionally, the sex-based differences decrease after menopause in women21. However, our results show that the sensitization rates for most food allergens were higher in men than in women and that difference did not decrease but rather increased in adults. Additionally, no sex-based differences in sensitization rates were observed for animal-based food allergens. Further research is needed to determine why this is different from previous results.
Although this study analyzed a large number of MASTs, it has some limitations that must be acknowledged. First, clinical information regarding symptoms were not available. Therefore, we did not know the exact reason why MAST was performed, but it is assumed that most cases are due to inhalant allergy. Second, given the cross-sectional nature of the study, longitudinal changes with age could not be clearly demonstrated. Third, because this study only targeted Koreans, the results may differ slightly from those in other countries. Fourth, although the MAST was conducted over 3 years, there is a possibility for patient duplication. Lastly, even though inhalant allergen data were available in the dataset, the present study focused solely on food allergens to ensure a clear objective and manageable scope. A separate analysis is planned to explore the relationship between inhalant and food allergen sensitization patterns.
Conclusion
Food allergens that induce sensitization vary across different age group, and each allergen category exhibits a distinct pattern of sensitization change by age and sex. There are three characteristic sensitization patterns.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request and are not publicly available.
References
Sicherer, S. H. & Sampson, H. A. Food allergy: A review and update on epidemiology, pathogenesis, diagnosis, prevention, and management. J. Allergy Clin. Immunol. 141(1), 41–58 (2018).
Soares-Weiser, K. et al. The diagnosis of food allergy: a systematic review and meta-analysis. Allergy 69(1), 76–86 (2014).
Loh, W. & Tang, M. L. K. The epidemiology of food allergy in the global context. Int. J. Environ. Res. Public. Health. 15(9), 2043 (2018).
Gupta, R. S. et al. Prevalence and severity of food allergies among US adults. JAMA Netw. Open. 2(1), e185630 (2019).
Rentzos, G., Johanson, L., Goksör Emma, Telemo, E. & Lundbäck Bo, Ekerljung, L. Prevalence of food hypersensitivity in relation to IgE sensitisation to common food allergens among the general adult population in West Sweden. Clin. Transl Allergy. 9, 22 (2019).
Feng, H. et al. Prevalence and influencing factors of food allergy in global context: A Meta-Analysis. Int. Arch. Allergy Immunol. 184(4), 320–352 (2023).
Spolidoro, G. C. I. et al. Frequency of food allergy in europe: an updated systematic review and meta-analysis. Allergy 78(2), 351–368 (2023).
Warren, C. M., Jiang, J. & Gupta, R. S. Epidemiology and burden of food allergy. Curr. Allergy Asthma Rep. 20(2), 6 (2020).
Sampath, V. et al. Food allergy across the Globe. J. Allergy Clin. Immunol. 148(6), 1347–1364 (2021).
Sicherer, S. H., Warren, C. M., Dant, C., Gupta, R. S. & Nadeau, K. C. Food allergy from infancy through adulthood. J. Allergy Clin. Immunol. Pract. 8(6), 1854–1864 (2020).
Kim, Y. H. et al. The change in food allergy prevalence of elementary school children in Seoul since the last 20 years and the risk factor analysis. Allergy Asthma Respir Dis. 4, 276–283 (2016).
Kim, M. A. et al. Pollen-Food allergy syndrome in Korean pollinosis patients: A nationwide survey. Allergy Asthma Immunol. Res. 10(6), 648–661 (2018).
Chung, B. Y., Cho, Y. S., Kim, H. O. & Park, C. W. Food allergy in Korean patients with chronic urticaria. Ann. Dermatol. 28(5), 562–568 (2016).
Noh, G. et al. Eosinophilia as a predictor of food allergy in atopic dermatitis. Allergy Asthma Proc. 31(2), e18–e24 (2010).
Lee, S. H. et al. A retrospective study of Korean adults with food allergy: differences in phenotypes and causes. Allergy Asthma Immunol. Res. 9(6), 534–539 (2017).
Lee, S. C., Kim, S. R., Park, K. H., Lee, J. H. & Park, J. W. Clinical features and culprit food allergens of Korean adult food allergy patients: A Cross-Sectional Single-Institute study. Allergy Asthma Immunol. Res. 11(5), 723–735 (2019).
Choi, J. H., Suh, J. D., Kim, I., Kim, J. K. & Cho, J. H. Changes in sensitization rates for respiratory and food allergens by age. Clin. Exp. Allergy.
Jeong, K. Y. et al. Role of Tropomyosin in silkworm allergy. Mol. Med. Rep. 15(5), 3264–3270 (2017).
Kim, I., Minn, D., Kim, S., Kim, J. K. & Cho, J. H. Aeroallergen sensitization status in South Korea from 2018 to 2021. Clin. Exp. Otorhinolaryngol. 15(3), 254–263 (2022).
Purohit, A. et al. Role of Tropomyosin as a cross-reacting allergen in sensitization to cockroach in patients from Martinique (French Caribbean island) with a respiratory allergy to mite and a food allergy to crab and shrimp. Eur. Ann. Allergy Clin. Immunol. 39(3), 85–88 (2007).
Pali-Schöll, I. & Jensen-Jarolim, E. Gender aspects in food allergy. Curr. Opin. Allergy Clin. Immunol. 19(3), 249–255 (2019).
Author information
Authors and Affiliations
Contributions
JHC and EJE contributed to the conception or design of the study and the acquisition, analysis or interpretation of the data. The manuscript was drafted by EJE; JHC critically reviewed and revised the manuscript. All authors have approved the final version and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests. This research was supported by the Regional Innovation System & Education(RISE) program through the Gangwon RISE Center, funded by the Ministry of Education(MOE) and the Gangwon State(G.S.), Republic of Korea (2025-RISE-10-006).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lee, E.J., Cho, J.H. Three different patterns of food allergen sensitization according to age and sex. Sci Rep 15, 44720 (2025). https://doi.org/10.1038/s41598-025-28491-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-28491-8