Abstract
Hypothermia during robot-assisted radical prostatectomy (RARP) has been proposed to enhance functional recovery. This study aimed to assess the efficacy of BELLOCOOL-induced hypothermic RARP for improving urinary continence and erectile function. A total of 200 patients with cT1-T3aN0M0 prostate cancer, eligible for bilateral nerve-sparing surgery, were enrolled across three tertiary centers and randomized 1:1. Stratification was based on International Index of Erectile Function (IIEF-5) scores (≥ 12). The primary endpoint was continence status at 6 months, defined by the use of < 1 pad versus ≥ 1 pads daily. Secondary endpoints included continence and erectile function recovery and safety assessment using the Clavien system. The primary outcome showed no significant difference between groups. However, among patients with IIEF-5 ≥ 12, those in the hypothermic group exhibited significantly better erectile function recovery than normothermic group at 12 months, with higher IIEF-5 score (9.29 ± 7.25 vs. 6.33 ± 5.16, p = 0.02). In a hypothesis-generating post hoc analysis, non-diabetic patients with baseline IIEF-5 ≥ 12 had a significantly higher erectile function recovery (81% vs. 70%, p = 0.04) and continence recovery rates (89% vs. 67%, p = 0.02) in the hypothermic group, findings that warrant cautious interpretation.
Similar content being viewed by others
Introduction
Prostate cancer (PCa) is the most common cancer in men;1 approximately 75% of patients diagnosed are with localized disease, making them candidates for surgical treatment2,3. The widespread adoption of robot-assisted radical prostatectomy (RARP) has improved postoperative functional outcomes, notably in mitigating urinary incontinence and erectile dysfunction4,5. However, a significant percentage of patients (10–46%) experience compromised postoperative functional outcomes, which underscores the necessity for further optimization of surgical techniques6.
Among the most prevalent approaches is the nerve-sparing technique, which aims to minimize damage to the delicate neurovascular bundles7. Another one involves real-time nerve monitoring during surgery, which helps surgeons identify and preserve nerves critical for erectile function8,9. Furthermore, efforts have been directed towards implementing intraoperative imaging techniques to aid in nerve identification, preservation, and minimizing adjacent tissue damage10,11. Finally, hypothermic techniques, inducing local hypothermia, have emerged as an approach to mitigate acute inflammatory damage arising from surgical incisions and thermal injuries12.
We had previously introduced an innovative endorectal cooling balloon device named BELLOCOOL (CEBIKA, Uiwang, South Korea), meticulously designed to induce and sustain lower pelvic temperatures13. The safety and effectiveness of this device were validated in a previous single-center study14. Therefore, in this study, we undertook a multicenter, randomized, single-blinded, controlled trial to evaluate whether regional hypothermia induced by the BELLOCOOL device can yield enhanced functional outcomes in patients who undergo RARP.
Materials and methods
Trial design and participants
This multicenter, prospective, single-blinded randomized controlled trial (RCT) was conducted across three major tertiary centers in the Republic of Korea. Patients aged 19–79 years, who met the following criteria were eligible: (i) pathologically confirmed prostate cancer (PCa), (ii) being considered for RARP, (iii) clinical stage T1-T3aN0M0, (iv) Eastern Cooperative Oncology Group performance status of 0 or 1, and (v) ability to comprehend and provide the informed consent form. The exclusion criteria were prior PCa treatment, pelvic radiation therapy or surgery, history of urinary incontinence, neurogenic bladder, neurological disorders, and refusal to participate. Patient randomization was required within 12 weeks of diagnosis. The patient-reported measures were collected using paper-based surveys, including the EuroQol-5 Dimensions 5-Level (EQ-5D-5 L), the 5-item International Index of Erectile Function (IIEF-5), and the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP).
The trial protocol was approved by the Institutional Review Board of Seoul National University Hospital (2101-062-1188). Written informed consent was obtained from all patients. The study adhered to the principles of the Declaration of Helsinki and the results are presented following the CONSORT guidelines. This trial was registered in the Clinical Research Information Service (CRiS) of the Republic of Korea (CRIS ID: KCT0006926) on 14/01/2022.
Randomization
Central randomization was performed by the Medical Research Collaborating Center team at Seoul National University Hospital using a web-based system. Stratification was based on pre-trial International Index of Erectile Function (IIEF-5) scores, categorized as < 12 and ≥ 12 points. Equal-sized strata were formed, and within each stratum, the subjects were randomly assigned in a 1:1 ratio to either the hypothermic (treatment) or normothermic (control) groups. The random sequence was generated using uniform random numbers from SAS RANUNI function with a specified seed value. A randomly permuted block design with block sizes of 4 and 6 was employed to develop a random allocation list for each stratum, with separate lists for each participating institution. Randomization was implemented by an independent person using a web-based system when a subject was enrolled. The research participants and their guardians were blinded to the random allocation. This blinding was rigorously maintained throughout the study by restricting access to allocation data and managing patient interactions carefully to prevent inadvertent disclosure. Additionally, both groups received identical postoperative care protocols, minimizing the risk of unintentional unblinding through treatment differences. These measures were implemented to preserve the integrity of the blinding throughout the 12-month follow-up, thereby reducing potential bias and enhancing the validity of our findings.
Intervention
All enrolled patients underwent RARP within 12 weeks of randomization. Pelvic hypothermia was induced using the BELLOCOOL system (CEBIKA, Uiwang, South Korea), which is approved by the Korean Ministry of Food and Drug Safety. A lubricated rectal balloon was introduced into the anus before robot docking and subsequently expanded using cold saline (4 °C). The saline temperature was dynamically adjusted in real time based on intra-rectal pressure measurements. Following prostate resection, the balloon was deflated and removed before the anastomosis procedure (Supplementary Fig. 1). All patients underwent conventional six-port transperitoneal RARP using an anterograde approach. Nerve-sparing was preoperatively planned based on multiparametric MRI findings, biopsy Gleason grade, and the predicted risk of extracapsular extension (ECE). The surgical plan was individualized according to each patient’s oncologic risk and anatomical characteristics. Nerve-sparing was preoperatively planned according to clinical circumstances, Dissection was generally performed at the intrafascial or interfascial level, while extrafascial dissection was permitted when oncologic concerns existed. Hemostasis around the NVB was primarily achieved using clips or Hem-o-Lok to minimize thermal energy application. To minimize differences between institutions and researchers, the following surgical techniques were standardized: (1) Bladder neck sparing technique, (2) posterior reconstruction, (3) anterior reconstruction, and (4) maximization of urethral length. Furthermore, postoperative PDE5 inhibitor prescription was standardized with Tadalafil 5 mg daily therapy.
Primary and secondary study endpoints
The primary outcome was continence status at 6 months after surgery, defined by the use of < 1 pad versus ≥ 1 pads daily. Secondary outcomes included continence status (patients using 0 pad versus any pad per day), potency status (patients with IIEF ≥ 12) at 3, 6, 9, and 12 months post-surgery, and results of the EuroQol-5 dimensions (EQ-5D-5 L), IIEF-5, and Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP) at 6, and 12 months postoperatively. In the context of IIEF-5 scores, a treatment response was defined as a 2-point increase in the total IIEF-5 score, consistent with the threshold adopted in previous randomized studies evaluating postoperative erectile function recovery15. Safety assessment was performed using the Clavien-Dindo classification system.
Statistical analyses
The sample size was calculated with the assumption that the treatment (hypothermic group) and control groups will have a continence rate of 73% and 53%, respectively, at 6 months (based on our feasibility trial)14. With a statistical power of 80% and a two-sided significance level of 5%, to detect a difference between the group proportions of 20%, each group (treatment and control) required 90 patients (a total of 180 patients) with an assumed dropout rate of 10%, resulting in a final sample size of 200 patients (100 per group). The study used PASS 2020 v20.0.2 to calculate the required number of participants.
Descriptive statistics of the baseline characteristics of the patients according to surgical groups (hypothermic vs. normothermic) are presented and compared using the chi-squared test or student’s t-test. These included age, hypertension (HTN), diabetes (DM), pre-operative PSA, prostate volume, period between prostate biopsy and operation, MRI T stage, ISUP GG, total IIEF score, EPIC-CP score EQ-5D-5 L VAS and utility score. To compare the primary outcome between the surgical groups with respect to the post-operative period, we used chi-squared test. Furthermore, student’s t-test was utilized to assess differences in the secondary outcome between the surgical groups with respect to the post-operative period.
Additionally, subgroup analyses were performed in a post hoc (a posteriori) manner, which were not predefined in the original study protocol. In exploratory post-hoc analyses, patients were stratified by the presence or absence of diabetes mellitus (DM), given that diabetes is associated with microvascular dysfunction and peripheral neuropathy, which may alter the neuroprotective impact of pelvic hypothermia on nerve recovery. These exploratory analyses were conducted to identify potentially meaningful findings that may warrant further investigation. We determined all P-values using a two-sided approach, with a type I error rate set below 0.05, which we considered to indicate statistical significance. All statistical analysis was performed using SPSS version 26 software.
Results
Patients characteristics
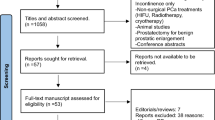
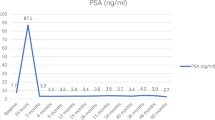
200 eligible patients were enrolled across three tertiary centers. During the trial period, seven patients dropped out for various reasons: four patients underwent non-nerve-saving RARP due to suspicion of advanced disease, two were lost to follow-up, and one patient encountered combined urethral stricture. The final analysis included 193 patients altogether (Fig. 1). The clinical characteristics were well balanced between the treatment and control groups (Table 1). The positive surgical margin (PSM) rate was higher in the treatment group than in the control group (Supplementary Table 1). However, no statistically significant differences were observed in other surgery-related factors between the two groups. Furthermore, both groups had similar tumor staging (pathological stage) and degrees of nerve-sparing during surgery.
Endpoints
Functional outcome
Entire cohort
The primary outcome of the study was the proportion of patients using < 1 pad per day at the 6-month follow-up; 71% (69/98) of the patients in the control group and 78% (74/95) in the treatment group met this criterion (Table 2). However, there were no statistically significant differences between the two groups. Erectile function recovery was analyzed at four timepoints: 3, 6, 9, and 12 months. At the 12-month follow-up, erectile function recovery was observed in 48% (47/98) of patients in the control group and 60% (57/95) in the treatment group; however, this difference was not statistically significant.
Sub-cohort (IIEF ≥ 12)
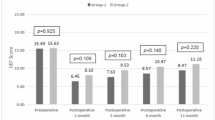
Among these 193 patients, 97 exhibited an IIEF score ≥ 12; among them, the proportion of patients using < 1 pad per day at the 6-month follow-up was 71% (32/49 patients) and 77% (37/48 patients) in the control and treatment groups, respectively (Table 3). However, this difference was not significant, nor were significant differences observed at other timepoints.
Concerning erectile function recovery, 47% (23/49) and 65% (31/48) of patients in the control and treatment groups, respectively, had recovered erectile function (p = 0.08) at the 6-month follow-up. At the 12-month follow-up, 59% (29 /49) and 77% (37/48) of patients in the control and treatment groups, respectively, had recovered erectile function (p = 0.06) (Table 3).
Sub-cohort (IIEF ≥ 12 without DM) –post hoc analysis
We performed additional functional outcome analysis on the subgroup of patients with an IIEF score ≥ 12 and without diabetes as a post hoc analysis. At the 12-month follow-up, the treatment group had a significantly higher erectile function recovery rate with a difference of approximately 21% compared to that exhibited by the control group (60% (25/42 patients) vs. 81% (30/37 patients), p = 0.04) (Table 4). Regarding urinary incontinence, the treatment group had a higher continence recovery rate at 9-months (67% vs. 89%, p = 0.02).
Patient-reported quality of life
Entire cohort
We compared IIEF-5 scores at 6 and 12 months, and the treatment group demonstrated significantly better erectile function than the control group. At 6 months, the mean IIEF-5 scores were 4.46 ± 4.14 in the control group and 6.16 ± 5.72 in the treatment group (p = 0.02). At 12 months, the respective scores were 4.95 ± 4.79 and 6.92 ± 6.17 (p = 0.01). However, no significant differences were observed in patient-reported quality of life scores, including the EuroQol-5 Dimensions 5-Level (EQ-5D-5 L) and the Expanded Prostate Cancer Index Composite for Clinical Practice (EPIC-CP). (Supplementary Table 2).
Sub-cohort (IIEF ≥ 12)
We performed additional functional outcome analysis for the group of patients with an IIEF score ≥ 12. We compared the scores at two timepoints, 6 and 12 months; the treatment group showed significantly superior erectile function results compared to those of the control group. At 6 months, the mean IIEF-5 scores were 5.43 ± 4.55 in the control group and 8.10 ± 6.88 in the treatment group (p = 0.03). At 12 months, the control and treatment groups had average IIEF-5 scores of 9.29 ± 7.25 and 6.33 ± 5.16, respectively (p = 0.02) (Supplementary Table 3). We compared the EQ-5D-5 L VAS, EQ-5D-5 L utility, EPIC-CP total, and EPIC-CP sexual subscale scores between the treatment and control groups at 6 and 12 months. However, the two groups did not differ significantly in terms of any outcome measure (Supplementary Table 3).
Adverse event
Four participants in the control group experienced Grade III or higher adverse events, while two in the treatment group experienced adverse events. No device-related adverse events were observed (Supplementary Table 4).
Discussion
In this multicenter randomized trial, regional hypothermia using the BELLOCOOL device did not improve the primary endpoint of urinary continence recovery at 6 months. Several clinical and procedural factors likely contributed to this negative outcome.
First, the enrolled population was heterogeneous, with variable preoperative erectile function, diabetes status, and age—all known predictors of postoperative functional recovery independent of surgical technique. These confounding factors may have mitigated the impact of hypothermia. Second, inter-surgeon variability across centers, including differences in experience with the device and the amount and duration of energy use in nerve-sparing, may have reduced the potential benefit of hypothermia. Third, continence recovery often continues beyond 6 months; therefore, the predefined endpoint may have been too early to capture delayed functional benefits. These factors together suggest that the lack of superiority reflects biological and procedural limitations rather than device failure.
When compared with previous multicenter studies using the UroCool device developed by Ahlering et al.,16,17 similar limitations were encountered. The UroCool trial also failed to demonstrate a functional benefit from hypothermia, underscoring the challenge of translating experimental neuroprotection into consistent clinical improvement. The BELLOCOOL system was developed to address some of these technical constraints by optimizing the rectal balloon design for improved anatomical contact and incorporating automated coolant flow and pressure control to maintain a stable target temperature of 26 °C.14 Nonetheless, differences in study populations may have further influenced outcomes. In our cohort, patients were older (mean 64.7 years vs. 62.5 years), had lower preoperative IIEF-5 scores (11.6 vs. 19.4), and included a higher prevalence of DM (18% vs. 7%) compared with the prior UroCool trial. In addition, Asian men have been reported to experience slower and less complete potency recovery after RARP, which may also contribute to the modest functional effects observed in the present study18. These contextual and demographic differences highlight the complexity of achieving measurable benefits from intraoperative hypothermia, even with technical refinements in device design.
Although exploratory subgroup analyses indicated trends favoring the hypothermic group in non-diabetic patients with baseline IIEF-5 ≥ 12, these findings were post hoc, based on small samples, and not adjusted for multiple comparisons. They should therefore be interpreted cautiously and regarded only as hypothesis-generating observations. From a physiological standpoint, diabetes19 and preoperative erectile20 function are closely related to neurovascular health; impaired microcirculation and neuropathy in diabetic patients may attenuate any neuroprotective effects of hypothermia. Nevertheless, these exploratory signals require prospective validation in more homogeneous populations.
Importantly, while the BELLOCOOL device demonstrated an acceptable safety profile, this study has several limitations that should be acknowledged. First, inter-surgeon learning curves and procedural variability may have influenced the results. Two of the five surgeons had no prior experience with the BELLOCOOL device, and intraoperative findings such as tissue edema, condensation, or changes in visibility of the dissection plane were not systematically documented, precluding further procedural correlation analyses. Second, the absence of double blinding could have introduced potential bias among surgeons, potentially affecting the degree of meticulousness during nerve-sparing. This is reflected in the variability of PSM rates between the two groups, although no statistically significant difference was observed (control vs. hypothermic group: 5% vs. 11%, p = 0.3). Within the primary sub-cohort (IIEF ≥ 12 and without diabetes mellitus), the hypothermic group achieved better functional outcomes without an increase in PSM rates. Analysis by individual surgeons also revealed mixed results—two surgeons had higher PSM rates in the control group, while three had higher rates in the treatment group—suggesting that surgeon variability rather than device-related limitations likely contributed to these discrepancies. Third, the assessment of continence and sexual function relied on patient-reported measures rather than objective tests. Continence was evaluated by pad use instead of a 24-hour pad-weight test, which may introduce subjectivity. Similarly, although IIEF-5 scores improved modestly in the hypothermic group, the mean difference (approximately 2–3 points) was below the minimal clinically important difference for the IIEF as established by Rosen et al.21, suggesting limited clinical relevance. Fourth, quality-of-life improvements were not observed on EPIC-CP and EQ-5D-5 L scales. Cultural factors22, as well as the relatively short follow-up duration of 12 months, may have limited the detection of meaningful QoL recovery, which often becomes evident only after one-year post-surgery23,24. Fifth, the randomization process was permitted up to 12 weeks prior to surgery, which may have increased the risk of compromising patient blinding. Although most of the randomizations were conducted after the patients were under anesthesia, the multicenter nature of the study may have led to randomization occurring at varying time points within the protocol, potentially affecting the integrity of blinding. Finally, this study did not assess long-term functional or oncologic outcomes beyond one year. Future trials with standardized surgical protocols, objective endpoint definitions, and extended follow-up are warranted to confirm these preliminary findings.
Despite these limitations, the present study demonstrates the feasibility and safety of applying regional hypothermia during RARP. Future research should include more standardized operative protocols, objective intraoperative temperature mapping, and longer follow-up to assess delayed recovery. Trials focusing on non-diabetic patients with preserved neurovascular function may better clarify whether pelvic hypothermia provides tangible functional benefits.
Conclusions
In this multicenter RCT, hypothermic RARP using the BELLOCOOL device did not improve urinary continence recovery, the pre-specified primary endpoint. While the device was safe and feasible, its efficacy in enhancing postoperative functional recovery remains unproven. Exploratory subgroup findings suggesting potential benefits in selected non-diabetic patients require prospective validation through future, adequately powered studies.
Data availability
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Siegel, R. L., Miller, K. D., Fuchs, H. E. & Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 72, 7–33. https://doi.org/10.3322/caac.21708 (2022).
Gray, P. J., Lin, C. C., Cooperberg, M. R., Jemal, A. & Efstathiou, J. A. Temporal trends and the impact of Race, Insurance, and socioeconomic status in the management of localized prostate cancer. Eur. Urol. 71, 729–737. https://doi.org/10.1016/j.eururo.2016.08.047 (2017).
Siegel, D. A., O’Neil, M. E., Richards, T. B., Dowling, N. F. & Weir, H. K. Prostate cancer incidence and Survival, by stage and Race/Ethnicity - United States, 2001–2017. MMWR Morb Mortal. Wkly. Rep. 69, 1473–1480. https://doi.org/10.15585/mmwr.mm6941a1 (2020).
d’Altilia, N. et al. A Matched-Pair analysis after robotic and retropubic radical prostatectomy: A new definition of continence and the impact of different surgical techniques. Cancers (Basel). 14. https://doi.org/10.3390/cancers14184350 (2022).
Haglind, E. et al. Urinary incontinence and erectile dysfunction after robotic versus open radical prostatectomy: A prospective, controlled, nonrandomised trial. Eur. Urol. 68, 216–225. https://doi.org/10.1016/j.eururo.2015.02.029 (2015).
Lima, T. F. N., Bitran, J., Frech, F. S. & Ramasamy, R. Prevalence of post-prostatectomy erectile dysfunction and a review of the recommended therapeutic modalities. Int. J. Impot. Res. 33, 401–409. https://doi.org/10.1038/s41443-020-00374-8 (2021).
Menon, M. et al. Potency following robotic radical prostatectomy: a questionnaire based analysis of outcomes after conventional nerve sparing and prostatic fascia sparing techniques. J. Urol. 174, 2291–2296. https://doi.org/10.1097/01.ju.0000181825.54480.eb (2005). discussion 2296.
Mandhani, A. et al. Real time monitoring of temperature changes in neurovascular bundles during robotic radical prostatectomy: thermal map for nerve-sparing radical prostatectomy. J. Endourol. 22, 2313–2317. https://doi.org/10.1089/end.2008.9712 (2008).
Song, W. H. et al. Establishment of novel intraoperative monitoring and mapping method for the cavernous nerve during Robot-assisted radical prostatectomy: results of the phase I/II, First-in-human, feasibility study. Eur. Urol. 78, 221–228. https://doi.org/10.1016/j.eururo.2019.04.042 (2020).
Rais-Bahrami, S. et al. Optical coherence tomography of cavernous nerves: a step toward real-time intraoperative imaging during nerve-sparing radical prostatectomy. Urology 72, 198–204. https://doi.org/10.1016/j.urology.2007.11.084 (2008).
Schiavina, R. et al. Real-time augmented reality Three-dimensional guided robotic radical prostatectomy: preliminary experience and evaluation of the impact on surgical planning. Eur. Urol. Focus. 7, 1260–1267. https://doi.org/10.1016/j.euf.2020.08.004 (2021).
Ahlering, T. E. & Skarecky, D. W. Preserving sexual function after robotic radical prostatectomy: avoiding thermal energy near nerves. BJU Int. 114, 131–132. https://doi.org/10.1111/bju.12663 (2014).
Song, W. H. et al. Feasibility study of a novel rectal cooling system for hypothermic radical prostatectomy in a swine model. Investig Clin. Urol. 63, 475–481. https://doi.org/10.4111/icu.20220092 (2022).
Han, J. H. et al. Feasibility, Safety, and functional outcomes of pelvic hypothermia induced using a rectal cooling device during Robot-Assisted radical prostatectomy: A phase I/II trial. J. Endourol. 37, 407–413. https://doi.org/10.1089/end.2022.0560 (2023).
Cui, W. et al. Efficacy and safety of novel low-intensity pulsed ultrasound (LIPUS) in treating mild to moderate erectile dysfunction: a multicenter, randomized, double-blind, sham-controlled clinical study. Transl Androl. Urol. 8, 307–319. https://doi.org/10.21037/tau.2019.07.03 (2019).
Finley, D. S., Osann, K., Skarecky, D. & Ahlering, T. E. Hypothermic nerve-sparing radical prostatectomy: rationale, feasibility, and effect on early continence. Urology 73, 691–696. https://doi.org/10.1016/j.urology.2008.09.085 (2009).
Huynh, L. M. et al. A randomized control trial of Anti-Inflammatory regional hypothermia on urinary continence during Robot-Assisted radical prostatectomy. Sci. Rep. 8, 16352. https://doi.org/10.1038/s41598-018-34657-4 (2018).
Namiki, S. et al. Sexual function following radical prostatectomy: a prospective longitudinal study of cultural differences between Japanese and American men. Prostate Cancer Prostatic Dis. 11, 298–302. https://doi.org/10.1038/sj.pcan.4501013 (2008).
Philippi, A. et al. Diabetes mellitus lowers the chance of short-term urinary continence recovery in prostate cancer patients undergoing radical prostatectomy. Cent. Eur. J. Urol. 75, 162–168. https://doi.org/10.5173/ceju.2022.0279.R1 (2022).
Wille, S., Heidenreich, A., Hofmann, R. & Engelmann, U. Preoperative erectile function is one predictor for post prostatectomy incontinence. Neurourol. Urodyn. 26, 140–143. https://doi.org/10.1002/nau.20314 (2007). discussion 144.
Rosen, R. C., Allen, K. R., Ni, X. & Araujo, A. B. Minimal clinically important differences in the erectile function domain of the international index of erectile function scale. Eur. Urol. 60, 1010–1016. https://doi.org/10.1016/j.eururo.2011.07.053 (2011).
Pak, S., Kim, M. & Ahn, H. Changes in health-related quality of life after radical prostatectomy for prostate cancer: A longitudinal cohort study in Korea. Investig Clin. Urol. 59, 313–320. https://doi.org/10.4111/icu.2018.59.5.313 (2018).
Lane, J. A. et al. Functional and quality of life outcomes of localised prostate cancer treatments (Prostate testing for cancer and treatment [ProtecT] study). BJU Int. 130, 370–380. https://doi.org/10.1111/bju.15739 (2022).
Huynh, L. M., Osann, K., Skarecky, D. & Ahlering, T. E. Predictive modelling of 2-year potency outcomes using a novel 90-day erection fullness scale after robot-assisted radical prostatectomy. BJU Int. 122, 249–254. https://doi.org/10.1111/bju.14190 (2018).
Acknowledgements
We thank Prof. So Yeoun Kim, stastical specialist at Seoul National University Hospital, for the statistical review.
Funding
This study was supported by a sponsored contract with CEBIKA Inc. This work was supported by a Korea Medical Device Development Fund grant funded by the Korean government (Ministry of Science and ICT; Ministry of Trade, Industry, and Energy; Ministry of Health & Welfare, Republic of Korea; and Ministry of Food and Drug Safety) (Project Number:202015 × 30).C.W. Jeong (co-inventor) receives royalties from the company.
Author information
Authors and Affiliations
Contributions
C.Kwak, S.S. Jeon and C.W. Jeong had full access to all data in the study and take responsibility for the integrity of the data and accuracy of the data analysis. Concept and design: Jeon and Jeong, Acquisition of data, Analysis and Interpretation of data: All authors, Initial drafting of the manuscript: Han, Critical revision of the manuscript for important intellectual content: All authors, Statistical analysis: Han, Jeong, Obtained funding: Jeon and Jeong, Administrative, technical, and material support: All authors, Supervision: All authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Han, J.H., Jeong, C.W., Chung, J.H. et al. Functional outcomes of hypothermic robot assisted radical prostatectomy using BELLOCOOL in a randomized controlled trial. Sci Rep 15, 45366 (2025). https://doi.org/10.1038/s41598-025-29165-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-29165-1