Abstract
The Textbook Outcome (TO) is a composite outcome measure that integrates commonly utilized independent outcome measures to comprehensively reflect the optimal post-surgical treatment result. It is used to assess the quality of surgeries and has been widely employed in hepatobiliary and pancreatic surgeries. However, its utility in splenic surgery remains unknown. Patients with cirrhosis and portal hypertension are often managed with splenectomy. The objective of this study was to investigate the perioperative textbook outcomes of splenectomy and identify the risk factors associated with achieving textbook outcomes after undergoing splenectomy. The clinical data of 263 patients with portal hypertension and hypersplenism who underwent splenectomy at our hospital were retrospectively analyzed. Perioperative clinical data were statistically analyzed using t-test, Wilcoxon test, χ2 test, or Fisher exact test. The 10-year survival and the incidence of postoperative hepatocellular carcinoma (HCC) were assessed using the Kaplan-Meier method and compared using the Log-Rank test. Among the 263 enrolled patients, 139 (52.85%) achieved textbook outcomes. Multivariate analysis revealed that preoperative prothrombin time and splenic vein diameter were independent risk factors for attaining textbook outcomes in patients undergoing splenectomy. The success rate of minimally invasive surgery was comparable to that of open surgery. Patients with high prognostic nutritional index and low Child-Pugh scores exhibited higher success rates. At 10-years of follow-up, there was no significant differences observed in terms of overall survival or hepatocellular carcinoma (HCC) incidence. However, patients who achieved TO demonstrated a higher long-term survival rate and a lower HCC incidence. Textbook outcomes serve as a comprehensive tool for assessing the quality of splenectomy. This study offers valuable insights guiding surgical treatment decisions for splenic diseases.
Similar content being viewed by others
Introduction
Portal hypertension, a syndrome characterized by elevated pressure in the portal venous system1, is attributed to increased intrahepatic vascular resistance and a hyperdynamic circulatory state. The progression of portal hypertension has been associated with complications such as hypersplenism, gastroesophageal varices, ascites, spontaneous bacterial peritonitis (SBP), hepatorenal syndrome (HRS), and even hepatocellular carcinoma (HCC)2. Among these complications, hypersplenism and upper gastrointestinal bleeding pose significant hazards for patients with portal hypertension. Splenectomy is the primary surgical approach for treating hypersplenism3; however, it carries a high incidence of postoperative complications including local hemorrhage and infection, portal vein thrombosis, and hepatic encephalopathy4. In the past, clinicians often relied on parameters such as postoperative complication rates, length of hospital stay, and mortality to assess the short-term prognosis after splenectomy5. Nevertheless, modern surgical practice demands the consistent delivery of quality health care throughout the entire patient care process6.
The Textbook Outcome (TO) is a comprehensive evaluation system that has been proposed in recent years to assess the quality of surgical treatment7. Since its introduction in 2013, it has gained widespread utilization in the assessment of hepatobiliary and pancreatic surgeries, such as radical resection of hepatocellular carcinoma8, pancreaticoduodenectomy9, and radical resection of gallbladder cancer10. However, there is a paucity of data and literature regarding textbook outcomes for splenectomy in patients with portal hypertension11.
In this study, we present the first definition of textbook outcomes following splenectomy based on a comprehensive review of existing literature and clinical expertise. We retrospectively collected clinical data from hospitalized patients who underwent splenectomy for portal hypertension at our center over the past decade to investigate the factors influencing the attainment of textbook outcomes after splenectomy for portal hypertension. Furthermore, subgroup analyses were conducted based on the choice of laparoscopic surgery and variations in preoperative nutritional and liver function status to ascertain whether these factors influenced textbook outcomes.
Materials and methods
Study setting and patients
This retrospective study analyzed clinical data from 512 patients diagnosed with liver cirrhosis and portal hypertension who underwent splenectomy at Shaanxi Provincial People’s Hospital between 2010 and 2022. Data was collected between August 2022 and April 2023, and the analysis was conducted in August 2023. Patients with viral hepatitis included in this group mainly consisted of those with hepatitis B and C infections. Portal hypertension was defined as a portal pressure gradient ≥ 25mmH2O or based on clinical assessment. Surgical treatment of portal hypertension is mainly suitable for patients who have had or are currently gastrointestinal bleeding, or have obvious varicose veins and have a high risk of bleeding accompanied by “red syndrome”, and are generally acceptable, have good liver function (Child A, B), and can tolerate surgery. Patients with liver function Child C generally do not advocate surgery, and try to use non-surgical treatment. Patient details were obtained from the hospital’s electronic medical record system. Patients meeting any of the following conditions were excluded: (1) patients with malignant tumors other than HCC; (2) patients with severe cardiovascular and cerebrovascular diseases; (3) previous history of hepatectomy; (4) complicated by autoimmune diseases or other serious illnesses that could affect surgical outcomes; (5) patients with incomplete medical records or follow-up data. Finally, a total of 263 patients were included in this study. The study protocol received approval from the Ethics Committee of Shaanxi Provincial People’s Hospital (approval number: SPPH-LLBG-17-3.2), adhering strictly to the principles required by the Helsinki Treaty. Due to the retrospective nature of this study, written informed consent could not be obtained, and private patient information was anonymized prior to analysis.
Date collection
The clinical data of patients upon admission were collected and analyzed. These data encompassed various factors, including age, gender, comorbidities (such as smoking, drinking, hypertension, diabetes, and esophagogastric varices), laboratory results (Leucocytes, platelet count, hemoglobin, liver and kidney function indicators, coagulation profile parameters, alpha-fetoprotein, and hepatitis virus replication levels), intraoperative details (spleen volume, splenic vein diameter, portal vein diameter, and intraoperative bleeding), postoperative anticoagulant management. Intraoperative adverse events were classified according to the ClassIntra system. Postoperative complications were graded using the Clavien-Dindo scores. The presence of postoperative portal vein thrombosis was determined through abdominal vascular ultrasound. Based on previous literature and clinical practice, the definition of TO after splenectomy included: (1) absence of serious intraoperative adverse events (ClassIntra ≥ III); (2) no severe complications within 90 days after surgery (Clavien-Dindo ≥ III); (3) no occurrence of portal vein thrombosis (PVT) within 7 days following splenectomy; (4) postoperative hospital stay less than 14 days; (5) no re-hospitalization due to the operation within 30 days after surgery; and (6) no surgery-related deaths during postoperative hospital stay. Prognostic nutritional index (PNI) was calculated: serum albumin (g/L) +5 ×lymphocyte count (×10− 9/L). Model for end-stage liver disease (MELD) score was calculated: 10 × [0.957 × ln(Creatinine)] + 0.378 × ln[total bilirubin + 1.12 × ln(INR)] + 6.43.
Follow-up
The follow-up was conducted through outpatient examinations or telephone interviews. The follow-up period for all patients ended in April 2023. Patients were retrospectively followed from the date of splenectomy until the occurrence of death, loss to follow-up and the end of the study. The follow-up process encompassed assessing postoperative living status, disease progression, and mortality. To mitigate bias, two investigators independently carried out the follow-up procedure.
Statistical analysis
Continuous variables were reported as means ± standard deviations or medians (min-max), while categorical variables were presented as frequencies and percentages. The t-test or Wilcoxon test was employed for measurement data, and the chi-square test or Fisher exact probability test was used for count data analysis. Survival curves were generated using the Kaplan-Meier method, and statistical analysis was performed using the Log-Rank test. Risk factors with a P value less than 0.10 in univariate analysis were further assessed through multivariate analysis. Statistical analyses were conducted using IBM Corporation’s Statistical Products and Services Solutions 23.0 software, while GraphPad Prism 8.0 software from GraphPad Software Inc., La Jolla, USA was utilized to enhance visual presentation of survival curves. A significance level of P < 0.05 was considered statistically significant.
Results
Perioperative characteristics and textbook outcome of splenectomy
263 patients with portal hypertension underwent splenectomy. In Table 1, the average duration of postoperative hospitalization was 14.42±6.20 days, and 92 patients (34.98%) were hospitalized for more than 14 days. Intraoperatively, serious adverse events were observed in 15 patients, including intraoperative massive hemorrhage in 10 cases, splenic pedicle tear in 2 cases, pancreatic tail injury in 2 cases, and cauterisation of the intestinal wall in 1 case. Postoperatively, massive ascites occurred in 123 cases (46.77%). Portal vein thrombosis occurred in 47 patients (17.87%), out of which 18 patients (6.84%) developed portal vein thrombosis (PVT) within 7 days after surgery. Postoperative abdominal hemorrhage occurred in 4 patients. There were 2 cases of intra-abdominal infection, 3 cases of surgical site infection, 5 cases of pulmonary infection, and 4 cases of urinary tract infection. 1 patient experienced delayed gastric emptying, while 2 developed hepatic encephalopathy. Follow-up results revealed that 2 patients required transfer to the ICU for further treatment. 3 patients died during their hospital stay, and 1 patient underwent emergency surgery again due to postoperative massive hemorrhage. Among these in-hospital deaths, 1 case was attributed to postoperative liver failure complicated with hepatic encephalopathy, and the remaining 2 cases resulted from postoperative hemorrhage. 6 patients (2.28%) died within 90 days after discharge. Among them, 3 cases were caused by postoperative hemorrhage, 2 cases by liver failure combined with hepatic encephalopathy and infection, and 1 case by pre-existing cardiopulmonary comorbidities. According to our definition of textbook outcomes following splenectomy, a total of 139 (52.85%) patients ultimately achieved textbook outcomes (Table 2). The predominant factor contributing to TO non-achievement was an extended postoperative hospital stay (35.0%), followed by the occurrence of Clavien-Dindo Grade ≥ III complications (5.7%), early PVT within 7 days post-surgery (6.8%), and intraoperative ClassIntra Grade ≥ III adverse events (3.8%). Notably, no 30-day readmissions were observed, and 3 patients (1.1%) died during hospitalization.
Risk factors associated with achieving TO after splenectomy
In Table 3, patients were categorized based on the achievement of textbook outcomes following splenectomy. The findings revealed no significant disparities between the two groups in terms of age, gender, coexisting condition, leucocytes, liver and kidney function, hepatitis B virus replication, preoperative prognostic nutritional index (PNI), spleen volume, portal vein diameter, surgical approach, early postoperative anticoagulant drug usage, postoperative overall survival and occurrence of postoperative HCC. However, patients who did not achieve textbook outcome after splenectomy exhibited inferior PT, INR, and Child-Pugh score (P < 0.05). Interestingly, there was a higher prevalence of patients with splenic vein diameters exceeding 9 mm among those who achieved textbook outcome compared to those who did not achieve (P = 0.043). Compared to non-textbook outcome group, although the levels of AFP, MELD score, and preoperative regular use of antiviral drugs were comparatively lower in patients who achieved textbook outcome, there was no statistically significant difference (P > 0.05).
To further investigate the factors influencing textbook outcomes following splenectomy, we conducted a multivariate analysis. The findings in Table 4 show that splenic vein diameter exceeding 9 mm and preoperative regular antiviral therapy are independent factors for achieving textbook outcomes after splenectomy in patients with portal hypertension (P < 0.05).
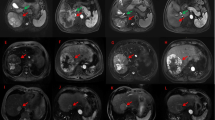
Effects of surgical approach, preoperative nutritional status and liver function on achieving TO after splenectomy
The perioperative outcomes of splenectomy with different surgical approaches (open vs. laparoscopic) are examined in Fig. 1. Compared with open surgery, laparoscopic surgery had a significantly lower rate of no-PVT within 7 days after splenectomy (80.56% vs. 95.15%, P = 0.001). However, the proportion of patients with postoperative hospital stay ≤ 14 days was significantly higher in laparoscopic splenectomy group than in open surgery group (50.66% vs. 22.22%, P = 0.001), which resulted in no significant difference in the success rate of achieving the textbook outcome between the two groups (55.56% vs. 52.42%, P>0.05). In Fig. 2, the patients were categorized and analyzed based on their preoperative nutritional status. The prognostic nutritional index (PNI) was utilized as an indicator to assess the nutritional status of patients prior to splenectomy, with lower PNI values indicating poorer nutritional status. We employed the mean PNI value to divide them into two groups: the high PNI group (≥ 37.72, n = 134) and the low PNI group (< 37.72, n = 129). Interestingly, the incidence of no-PVT within 7 days post-surgery was found to be significantly lower in the low PNI group compared to the high PNI group (3.10% vs. 10.45%, P = 0.026). However, although the low PNI group exhibited a slightly lower success rate in achieving the textbook outcome, this difference did not reach statistical significance (49.88% vs. 57.31%, P > 0.05). In Fig. 3, the group analysis was performed according to the preoperative liver function. Compared with patients in Child-Pugh A, the incidence of postoperative severe complications (Clavien-Dindo ≥III) was higher in patients with Child-Pugh B/C, but the difference was not statistically significant (7.73% vs. 2.44%, P>0.05). Interestingly, the rate of postoperative hospital stay within 14 days was significantly lower in patients with Child-Pugh B/C (46.96% vs. 67.07%, P = 0.002). This resulted in a lower success rate of achieving the textbook outcome in Child-Pugh B/C patients (48.62% vs. 62.20%, P = 0.041).
Textbook outcome of splenectomy categorized by surgical approaches (open laparotomy vs. laparoscopic surgery). Notes: “Proportion” = compliance rate of each group with individual TO criteria; “Accumulation” = cumulative compliance of each group with all TO criteria. Y-axis = compliance rate (%). PVT: Portal vein thrombosis.
Overall survival and HCC occurrence for TO patients
Although the 10-year overall survival rate of the group that did not achieve TO was lower than that of the group that achieved, there was no statistically significant difference between the two groups (Log-Rank test, P > 0.05). Interestingly, the incidence of HCC in the non-TO group was also higher than that in TO group, but this was not statistically significant (Log-Rank test, P > 0.05).
Discussion
Definition of TO after splenectomy
The purpose of this study was to investigate the prevalence of textbook outcomes (TO) of splenectomy and to identify the factors influencing its attainment. TO is a composite outcome measure integrating various optimal surgical outcomes12, and is argued to provide a better evaluation of the entire surgical treatment process from the surgery to the perioperative standard of care than any single outcome measure alone11. TO was first defined in the context of colorectal surgery by Kolfschoten13, and since then has been widely adopted in various surgical fields including hepatobiliary surgery. While most studies define TO with factors such as intraoperative adverse events, post-operative complications and length of stay, differences in the definition of TO exist between different surgical procedures due to surgery specific differences; There is even variability amongst different authors in the choice of individual parameters defining TO for the same surgical procedure14. While no universal definition of TO exists, parameters included in the definition of TO should be included based on whether they adequately reflect the quality of perioperative care, and whether they have a clear impact on welfare of patients or future outcomes.
In the context of this study, extensive literature review has found that there is no pre-existing definition of TO in the context of splenectomy patients with portal hypertension. Hence, outcomes included in the definition of TO was based on previously established definitions of TO in other hepatobiliary surgeries14and clinical understanding of the common adverse outcomes observed post-splenectomy. In particular, absence of PVT was included in our definition of TO because it is a known fact that PVT one frequent complication of splenectomy15,16, which can cause severe adverse consequences for the patient such as worsening portal hypertension causing gastrointestinal bleeds, intractable ascites, liver failure and hepatic encephalopathy15,16,17. Other outcomes like length-of-stay and post-operative complications are also included because these are factors that reflect and/or affect surgical quality and patient recovery. According to relevant literature and clinical experience, patients who do not have complications after portal hypersplenectomy generally have a hospital stay of less than 14 days, and if complications such as portal venous thrombosis, bleeding, infection, and ascites occur after surgery, the hospitalization time will be extended to varying degrees with the change of condition. Interestingly, even though the results were not statistically significant, patients who attained TO had better 10-year survival and lower HCC rates on follow-up. While more studies would be required to evaluate this relationship, it could be argued that our definition of TO may go beyond short-term implications on patient well-being to have a predictive effect on long term patient outcomes.
Rates of TO in patients with portal hypertension undergoing splenectomy
In this study, 263 patients with portal hypertension were treated by splenectomy, but only 139 patients (52.85%) achieved TO, suggesting that the adverse events associated with this procedure should not be ignored. Of patients who did not achieve TO, length of hospital stay and development of PVT were the strongest contributing factors for the failure to achieve TO. The prolonged hospital stay after portal hypertension splenectomy is mainly due to the fact that the immune function of patients with cirrhosis may be reduced, and the body’s immune ability is further weakened after splenectomy, coupled with surgical trauma, which is more prone to infection. And most patients with cirrhosis with portal hypertension have a certain degree of ascites, which may lead to hypoproteinemia and malnutrition, so wound healing and ability recovery will be slower; In addition, patients with heavy intraoperative bleeding and large blood transfusion will recover more slowly after surgery. This is unsurprising given the known complications of PVT occurring around 5%-55% of splenectomy patients15, possibly as a result of hemodynamic changes produced by the splenic vein stump, local endothelial injury, increases in platelet count after splenectomy, and decrease in portal blood flow due to interrupted splenic vein blood flow15,18. The thrombotic risk is further compounded by derangements in the production of procoagulant and anticoagulant factors as well as slower portal venous flow due to portal vein hypertension in cirrhotic patients15,19. Given the limited attainment of TO, surgeons have to carefully consider whether the benefits outweigh the harms before offering splenectomy to patients. On the other hand, our finding also highlights the importance of continued effort to strive towards better surgical outcomes, which this study seeks to achieve by exploring the influencing factors of surgical TO.
Significant risk factors affecting TO after splenectomy
In the univariate analysis, a better Child-Pugh status, PT and INR, as well as splenic vein diameter > 9 mm was significantly associated with attainment of textbook outcomes. Univariate analysis found an association between attainment of textbook outcomes and better Child-Pugh status. This was confirmed by group analysis which showed a lower success rate of achieving the textbook outcome in Child-Pugh B/C patients compared to Child-Pugh A patients (48.62% vs. 62.20%, P = 0.041). The Child-Pugh Score for cirrhosis was validated as a prognostic indicator in patients with chronic liver disease and cirrhosis20, as well as a predictor for intra-operative complications like massive intraoperative bleeding21, which would provide an adequate explanation for our findings.
Univariate analysis also found that a reduction in pre-operative PT was beneficial for TO, with patients who achieved TO having a pre-operative average PT of 15.84 ± 2.06 compared to 16.88 ± 2.32 in those who did not. A similar pattern was seen in INR: patients who achieved textbook outcomes had a lower INR on average (1.29 ± 0.17 compared to 1.38 ± 0.35. This relationship can be explained by the fact that poorer pre-operative coagulation profile may indicate an increased risk of coagulation dysfunction, which increases the peri-operative complications22. It is important to note that it may not solely be an increased risk of bleeding that contributes to higher rates of peri-operative complications, but rather that the abnormal coagulation profile could suggest a more advanced state of liver dysfunction, affecting production of both pro-coagulant and anti-coagulant factors and thus the balance between bleeding and clot formation23. Nonetheless, results from this study suggest that coagulation abnormalities should be recognized and adequately managed pre-operatively to improve outcomes for patients.
Interestingly, this study also revealed a positive association between intraoperative splenic vein diameter > 9 mm and attainment of TO, which was further found to be an independent predictor of TO in multivariate analysis. This finding contradicts pre-existing studies and meta-analyses that link increased pre-operative splenic vein diameter to an increased portal vein thrombosis risk post-splenectomy15,18. Significantly, the same finding was not observed for splenic vein diameters > 13 mm in our study, which could suggest that the link between larger splenic diameters (> 9 mm) and achievement of TO was a spurious one, given that only a small proportion of patients studied had pre-operative splenic diameters < 9 mm. Nonetheless, more studies need to be done to elucidate this association.
Lastly, multivariate analysis highlighted pre-operative anti-viral treatment as a significant factor influencing the attainment of textbook outcomes, with an odds ratio of 2.3. Perioperative antiviral therapy has been recommended as treatment to improve outcomes in patients with hepatitis B related HCC undergoing hepatectomy as it prevents exacerbations or reactivations of chronic hepatitis B and the associated post-operative complications brought about by hepatic insufficiency24,25. While our population of interest in this study is splenectomy (instead of hepatectomy) patients, our study should draw attention to the importance of proactive management of hepatitis B with perioperative anti-viral therapy especially given the large proportion of patient with cirrhosis due to hepatitis.
Effect of surgical modality and prognostic nutritional index (PNI) on TO
In this study, an attempt was also made to investigate the effect of surgical approach and prognostic nutritional index on attainment of TO. Laparoscopic surgery is often the preferred choice for splenectomy due to its minimally invasive nature, permitting a shorter post-operative length of stay, fewer post-operative complications, lower levels of pain, lower intra-operative blood loss21,26,27, even though it is associated with a longer operating time. Yet, portal hypertension in cirrhosis leading to massive splenomegaly is sometimes seen as a contraindication to laparoscopic splenectomy. Uncontrolled hemorrhage may require conversion to open splenectomy21. Additionally, the increased technical difficulty of laparoscopic splenectomy in patients with massive splenomegaly owing to impaired tactile feedback, poor identification of the splenic hilum, lack of operating space and difficulty in handling a massively enlarged spleen, may result in a lower utilization of laparoscopic approach for splenectomy28. This explains the lower rates of laparoscopic splenectomy of only 13.69% in this study. Despite the technical challenges, benefits of laparoscopic splenectomy should not be ignored, and meta-analysis of evidence have recommended that laparoscopic splenectomy in most cirrhotics with portal hypertension is a safe and feasible option that offers better outcomes21,27,28. This is supported by data from our study showing a drastically higher achievement of length of stay < 14 days. In the present study, the incidence of PVT within 7 days was relatively higher in the laparoscopic group. We hypothesize that this phenomenon may be associated with the pneumoperitoneum required for laparoscopic procedures, which is likely to compress the portal venous system and thereby induce blood stasis. Secondly, patients with portal hypertension typically exhibit dilated splenic veins, and following laparoscopic splenectomy, blood stasis at the splenic vein stump becomes more pronounced. Notably, laparoscopic splenectomy has been increasingly adopted in the management of patients with portal hypertension; however, data comparing its impact on textbook outcomes (TO) with that of open surgery remain scarce. Our findings therefore offer preliminary insights to inform surgical decision-making for this specific patient cohort. Additionally, the achievement of no-PVT within 7 days of the date of operation was much lower in laparoscopic surgeries possibly due to the minimal trauma and stress response associated with laparoscopic procedures, as well as the limited sample size of this study. This resulted in no statistically significant difference between rates of attainment of TO between the two surgical approaches.
Prognostic nutrition index (PNI) is a nutritional indicator and has been shown to effectively predict surgical prognosis or outcomes29. In our study, although not statistically significant, patients with a higher PNI achieved higher rates of TO. One possible mechanism is that, malnutrition related hypoalbuminemia, as well as lymphopenia due to cirrhosis (alone or in combination), may underlie this process. Thus, adequate preoperative nutritional therapy or immunonutrition can improve prognosis by strengthening the immune system and increasing resistance to complications.
Limitations
This study has limitations due to the retrospective, single-center nature and limited sample size. This could have contributed to biases in identification of the risk factors for TO. The single-center nature of this study means that different surgical approaches and peri-operative care guidelines were not reflected which may lead to poorer generalizability of results. Parameters included in the definition of TO may require revision, particularly in terms of length of stay to more accurately reflect longer hospital stays arising from complications or poor healing and rehabilitation, instead of a prescribed cut off of 14 days. Additionally, while laparoscopic splenectomy, high PNI, low Child-Pugh score, and shortened prothrombin time correlated with specific TO-related indicators in descriptive subgroup and univariate analyses (e.g., lower 7-day postoperative PVT in laparoscopy, higher postoperative hospital stay compliance in high-PNI patients), they were not validated as independent factors for overall TO achievement via multivariate analysis. Due to the single-center retrospective design limitations—including small sample size and potential inter-variable confounding—their actual predictive value for TO remains unclear. Future large-sample, multicenter prospective studies are needed to verify these associations and clarify their clinical reference significance.
Currently, the major factor preventing the attainment of TO was due to the post-operative length of stay requirement, which may not reflect poor surgical care per se but rather the expected hospitalization requirements for patients with such extensive comorbidities or hospital guidelines. In the same vein, only severe post-operative (Clavien-Dindo ≥ III) and intra-operative complications (ClassIntra ≥ III) were considered, resulting in minimal contributions of these factors to the failure to attain TOs, which may have skewed the significant risk factors towards those that affect length of stay. More importantly, despite absence of severe outcomes, less severe but unexpected outcomes may still have an impact on the patient and reflect surgical quality, which may explain why some authors considered all complications in the assessment of TO14. Thus, a revised definition of textbook outcomes may better reflect quality of surgery and surgical care, as well as help to uncover more significant risk factors affecting outcomes of splenectomy patients.
Although this study has the aforementioned limitations, it still provides preliminary evidence for the TO assessment of portal hypertension splenectomy. To further enhance the universality of the TO definition, subsequent external validation studies will be conducted: jointly collecting independent case cohorts from multicenters, using the TO standard proposed in this study to assess the compliance rate, and verifying the cross-center consistency of factors affecting preoperative PT and splenic vein diameter; and based on the distribution of postoperative hospitalization time and differences in complication management among different centers, optimizing the indicator thresholds in the TO definition, ultimately forming a surgical quality evaluation standard that can be widely applied, providing more reliable references for clinical practice.
Conclusions
Splenic vein diameter (> 9 mm) and preoperative regular antiviral therapy are independent risk factors for achieving textbook outcomes (TO) after splenectomy in patients with portal hypertension. Laparoscopic splenectomy, high prognostic nutritional index (PNI), low Child-Pugh score, and shortened prothrombin time correlate with better performance in specific TO-related indicators, including lower 7-day postoperative portal vein thrombosis (PVT) incidence and higher proportion of postoperative hospital stay ≤ 14 days. This study offers valuable insights to guide surgical diagnosis and treatment decisions for patients with portal hypertension.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- TO:
-
Textbook outcomes
- PVT:
-
Portal venous thrombosis
- ICU:
-
Intensive care unit
- HBV:
-
Hepatitis B virus
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- PT:
-
Prothrombin time
- APTT:
-
Activated partial thromboplatin time
- INR:
-
International normalized ratio
- AFP:
-
Alpha-fetoprotein
- MELD:
-
Model for end-stage liver disease
- HCC:
-
Hepatocellular carcinoma
- PNI:
-
Prognostic nutritional index
- SBP:
-
Spontaneous bacterial peritonitis
- HRS:
-
Hepatorenal syndrome
References
Boike, J. R. et al. North American practice-based recommendations for transjugular intrahepatic portosystemic shunts in portal hypertension. Clin. Gastroenterol. Hepatol. 20 (8), 1636–1662. https://doi.org/10.1016/j.cgh.2021.07.018 (2022).
Gunarathne, L. S. et al. Cirrhotic portal hypertension: from pathophysiology to novel therapeutics. World J. Gastroenterol. 26 (40), 6111–6140. https://doi.org/10.3748/wjg.v26.i40.6111 (2020).
Li, Y. et al. Early prevention and risk factors analysis of portal vein system thrombosis after laparoscopic splenectomy and pericardial devascularization. Surg. Endosc. 36 (12), 8918–8926. https://doi.org/10.1007/s00464-022-09340-5 (2022).
Tsilimigras, D. I., Pawlik, T. M. & Moris, D. Textbook outcomes in hepatobiliary and pancreatic surgery. World J. Gastroenterol. 27 (15), 1524–1530. https://doi.org/10.3748/wjg.v27.i15.1524 (2021).
Remiker, A. & Neunert, C. Splenectomy for immune thrombocytopenia: the evolution and preservation of treatment. Haematologica 105 (11), 2507–2509. https://doi.org/10.3324/haematol.2020.261099 (2020).
Arroyo, N. A. et al. What promotes surgeon practice change? A scoping review of innovation adoption in surgical practice. Ann. Surg. 273 (3), 474–482. https://doi.org/10.1097/sla.0000000000004355 (2021). http://doi.otg/
Wu, Y. et al. Textbook outcome as a composite outcome measure in laparoscopic pancreaticoduodenectomy: a multicenter retrospective cohort study. Int. J. Surg. 109 (3), 374–382. https://doi.org/10.1097/js9.0000000000000303 (2023).
Tsilimigras, D. I. et al. Hospital variation in textbook outcomes following curative-intent resection of hepatocellular carcinoma: an international multi-institutional analysis. HPB (Oxford). 22 (9), 1305–1313. https://doi.org/10.1016/j.hpb.2019.12.005 (2020).
Kulshrestha, S. et al. Textbook oncologic outcome in pancreaticoduodenectomy: do regionalization efforts make sense? J. Surg. Oncol. 125 (3), 414–424. https://doi.org/10.1002/jso.26712 (2022).
Li, Q. et al. Textbook outcome in gallbladder carcinoma after curative-intent resection: a 10-year retrospective single-center study. Chin. Med. J. (Engl). 136 (14), 1680–1689. https://doi.org/10.1097/cm9.0000000000002695 (2023).
Pretzsch, E. et al. Textbook outcome in hepato-pancreato-biliary surgery: systematic review. BJS Open. 6, 6. https://doi.org/10.1093/bjsopen/zrac149 (2022).
Görgec, B. et al. Assessment of textbook outcome in laparoscopic and open liver surgery. JAMA Surg. 156 (8), e212064. https://doi.org/10.1001/jamasurg.2021.2064 (2021).
Kolfschoten, N. E. et al. Focusing on desired outcomes of care after colon cancer resections; hospital variations in ‘textbook outcome’. Eur. J. Surg. Oncol. 39 (2), 156–163. https://doi.org/10.1016/j.ejso.2012.10.007 (2013). http://doi.otg/
Kryzauskas, M. et al. Achieving textbook outcomes in colorectal cancer surgery is associated with improved Long-Term survival: results of the multicenter prospective cohort study. J. Clin. Med. 13, 5. https://doi.org/10.3390/jcm13051304 (2024).
Péré, G. et al. Splenic volume and Splenic vein diameter are independent pre-operative risk factors of portal vein thrombosis after splenectomy: a retrospective cohort study. BMC Surg. 21 (1), 366. https://doi.org/10.1186/s12893-021-01364-3 (2021).
He, S. & He, F. Predictive model of portal venous system thrombosis in cirrhotic portal hypertensive patients after splenectomy. Int. J. Clin. Exp. Med. 8 (3), 4236–4242 (2015).
Kinjo, N. et al. Risk factors for portal venous thrombosis after splenectomy in patients with cirrhosis and portal hypertension. Br. J. Surg. 97 (6), 910–916. https://doi.org/10.1002/bjs.7002 (2010).
Lin, Y. K. et al. Risk factors of portal vein system thrombosis after splenectomy: a meta-analysis. ANZ J. Surg. 93 (12), 2806–2819. https://doi.org/10.1111/ans.18633 (2023).
Prakash, S. et al. Portal vein thrombosis in cirrhosis: a literature review. Front. Med. (Lausanne). 10, 1134801. https://doi.org/10.3389/fmed.2023.1134801 (2023).
Palmieri, C. & Macpherson, I. R. A review of the evidence base for utilizing Child-Pugh criteria for guiding dosing of anticancer drugs in patients with cancer and liver impairment. ESMO Open. 6 (3), 100162. https://doi.org/10.1016/j.esmoop.2021.100162 (2021).
Cai, Y., Liu, Z. & Liu, X. Laparoscopic versus open splenectomy for portal hypertension: a systematic review of comparative studies. Surg. Innov. 21 (4), 442–447. https://doi.org/10.1177/1553350613520513 (2014).
Lv, Y. et al. Coagulation dysfunction in patients with liver cirrhosis and splenomegaly and its countermeasures: a retrospective study of 1522 patients. Dis. Markers 2023, 5560560. https://doi.org/10.1155/2023/5560560 (2023).
Crăciun, R. et al. The bleeding edge: managing coagulation and bleeding risk in patients with cirrhosis undergoing interventional procedures. Diagn. (Basel) 14, 22. https://doi.org/10.3390/diagnostics14222602 (2024).
Zhang, B. et al. Perioperative antiviral therapy improves safety in patients with hepatitis B related HCC following hepatectomy. Int. J. Surg. 15, 1–5. https://doi.org/10.1016/j.ijsu.2014.12.030 (2015).
Liu, J. et al. Antiviral therapy inhibited HBV-reactivation and improved long-term outcomes in patients who underwent radiofrequency ablation for HBV-related hepatocellular carcinoma. World J. Surg. Oncol. 21 (1), 42. https://doi.org/10.1186/s12957-023-02921-1 (2023).
Huang, J. et al. Laparoscopic splenectomy and azygoportal disconnection to treat liver cirrhosis with hypersplenism and esophagogastric variceal bleeding: a video vignette. Asian J. Surg. 46 (8), 3122–3123. https://doi.org/10.1016/j.asjsur.2023.02.079 (2023).
Konishi, T. et al. Laparoscopic versus open distal pancreatectomy with or without splenectomy: a propensity score analysis in Japan. Int. J. Surg. 104, 106765. https://doi.org/10.1016/j.ijsu.2022.106765 (2022).
Deng, Z. C. et al. Laparoscopic VS. open splenectomy and oesophagogastric devascularisation for liver cirrhosis and portal hypertension: a retrospective cohort study. Int. J. Surg. 80, 79–83. https://doi.org/10.1016/j.ijsu.2020.06.026 (2020).
Liu, M. et al. Prognostic nutritional index (PNI) as a potential predictor and intervention target for perioperative ischemic stroke: a retrospective cohort study. BMC Anesthesiol. 23 (1), 268. https://doi.org/10.1186/s12871-023-02216-8 (2023).
Funding
Supported by National Natural Science Foundation of China (No. 82200686).
Author information
Authors and Affiliations
Contributions
Conceptualization: ZD, YZ; Data curation: ZD, CL, ZL, DL; Formal analysis: ZD; Validation: RW, YZ; Funding acquisition: ZD; Investigation: ZD, YZ, YW, WL; Methodology: ZD; Project administration: ZD, RW; Resources: YZ, RW; Supervision: RW, ZD; Visualization: ZD, RW; Writing – original draft: LC, ZL; Writing – review & editing: ZD.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Informed consent
This study was reviewed and approved by the Ethics Committee of the Shaanxi Provincial People’s Hospital (Permit Number: SPPH-LLBG-17-3.2). Due to the retrospective nature of the study, the review board of Shaanxi Provincial People’s hospital waived the need of obtaining informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, L., Lin, Z., Li, D. et al. Textbook outcomes after splenectomy in patients with portal hypertension. Sci Rep 16, 2451 (2026). https://doi.org/10.1038/s41598-025-32375-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-32375-2