Abstract
Early diagnosis of Alzheimer’s disease (AD), particularly during its preclinical and prodromal phases, remains a major challenge. Plasma biomarkers such as phosphorylated tau at threonine 217 (p-tau217), amyloid-β (Aβ) isoforms, neurofilament light chain (NfL), and glial fibrillary acidic protein (GFAP) show promise for early detection; however, their relationships with medial temporal lobe (MTL) subfield atrophy and potential inter-biomarker pathways remain unclear. This study aimed to address this gap by investigating the associations between plasma biomarkers and MTL subfield atrophy, and by assessing potential mediation pathways. We conducted a cross-sectional study using data from 330 participants in the Alzheimer’s Disease Neuroimaging Initiative (ADNI), including cognitively normal (CN) and mild cognitive impairment (MCI) groups. High-resolution coronal T2-weighted MRI quantified MTL subfield volumes using the ASHS protocol. Plasma biomarkers were measured using ultrasensitive immunoassays. The cohort included 209 CN participants (mean age [SD] = 69.3 [6.9] years; 64.2% women; 24.4% APOE ε4 carriers) and 121 MCI participants (mean age [SD] = 71.3 [7.3] years; 48.8% women; 27.9% APOE ε4 carriers). MCI individuals showed significantly higher plasma concentrations of p-tau217, p-tau217/Aβ1–42 ratio, NfL, and GFAP, and greater MTL atrophy. Higher plasma p-tau217 and p-tau217/Aβ1–42 were associated with reduced bilateral hippocampal and CA1 volumes in MCI (β = − 0.37 to − 0.28; FDR p < 0.02). In CN, these biomarkers were positively associated with left hippocampal volume (β ≈ 0.19; FDR p = 0.04), and GFAP correlated with larger sulcal volume (FDR p = 0.03). Mediation analysis demonstrated that in CN individuals, the relationship between p-tau217/Aβ1–42 and left sulcal volume was partially mediated by GFAP (indirect β = 0.11; FDR p = 0.048). This study reveals stage-specific plasma biomarker–MTL relationships across the Alzheimer’s continuum. In MCI, plasma p-tau217 and its ratio to Aβ1–42 closely track hippocampal subfield atrophy, reflecting tau-related neurodegeneration. In CN individuals, higher p-tau217 and p-tau217/Aβ1–42 levels relate positively to hippocampal integrity, partly mediated by GFAP, suggesting early astroglial activity preceding structural loss. These findings underscore dynamic biomarker interactions and support integrating plasma and imaging markers for early AD characterization.
Similar content being viewed by others
Introduction
Dementia affects an estimated 55.2 million individuals globally, with projections indicating a rise to 78 million by 2030 and 139 million by 2050. Among these cases, Alzheimer’s disease (AD) is the most prevalent etiology, accounting for 60–70% of all diagnoses1. Despite increasing awareness and clinical advancements, misdiagnosis rates remain unacceptably high, ranging from 20 to 35% in specialized memory clinics to over 50% in primary care settings lacking biomarker-based support2,3,4. This diagnostic uncertainty underscores the urgent need for sensitive, specific, and scalable biomarkers to facilitate early and accurate detection, particularly in the era of emerging disease-modifying therapies such as lecanemab and donanemab5,6,7.
Blood-based biomarkers have emerged as a transformative solution, offering minimally invasive, cost-effective tools for early AD detection, progression tracking, and treatment monitoring8,9,10,11,12. Technological innovations in ultrasensitive assays now permit the reliable quantification of brain-derived proteins at subfemtomolar concentrations in plasma13,14. Among these, amyloid-β (Aβ) peptides and phosphorylated tau (p-tau) isoforms have shown robust associations with AD pathology15,16,17,18,19,20,21,22. Notably, p-tau217 stands out for its superior diagnostic performance, exhibiting strong correlations with both amyloid and tau positron emission tomography (PET) imaging, and outperforming p-tau181 in predicting cognitive decline and pathophysiological AD across disease stages23,24,25,26,27,28,29,30,31,32,33,34,35. Recent studies have demonstrated the feasibility of measuring p-tau217 and Aβ42/Aβ40 on fully automated platforms, enhancing assay reproducibility and clinical applicability36.
Complementing fluid biomarkers, neuroimaging, particularly high-resolution structural magnetic resonance imaging (MRI), remains indispensable in characterizing early AD-related neurodegeneration. The medial temporal lobe (MTL) is among the earliest affected brain regions in AD and plays a critical role in episodic memory processing37,38. High-resolution T2-weighted imaging provides precise volumetric delineation of hippocampal subfields and adjacent cortical structures, such as the entorhinal and perirhinal cortices39,40. AD progression exhibits region-specific patterns, with early involvement of the entorhinal cortex and CA1, followed by degeneration in other hippocampal subfields and parahippocampal gyrus41,42. Despite substantial progress in blood-based biomarker development, the link between peripheral AD pathology and region-specific neurodegeneration within the MTL remains poorly understood. In particular, it is unknown whether plasma p-tau217 and its ratios with amyloid-β capture the selective vulnerability of hippocampal subfields and other MLT structures across the cognitively normal and mild cognitive impairment (MCI) stages, and whether downstream markers of astroglial activation (GFAP) and axonal injury (NfL) mediate these associations.
To address this knowledge gap, we aimed to (1) characterize the associations between plasma p-tau217, the p-tau217/Aβ1–42 ratio, and other plasma biomarkers (Aβ1–42, Aβ1–40, NfL, GFAP) with high-resolution MRI-derived volumes of MLT subregions in cognitively normal and MCI participants from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) cohort, and (2) explore whether GFAP and NfL mediate the relationships between tau/amyloid plasma markers and MLT subregional atrophy.
Methods
Participants and study design
This cross-sectional study was conducted using data from ADNI database (http://adni.loni.usc.edu/), a longitudinal, multicenter study established in 2003 under the leadership of Dr. Michael W. Weiner. ADNI aims to evaluate whether a combination of serial MRI, PET, fluid biomarkers, and comprehensive clinical and neuropsychological assessments can effectively monitor the progression of MCI and early AD.
Participants aged 55 to 90 years underwent neuroimaging and longitudinal clinical evaluations43. The study’s full inclusion and exclusion criteria have been described previously44. Key exclusion criteria included a Hachinski Ischemic Score > 4, use of non-approved medications, recent changes in allowable treatments, a Geriatric Depression Scale score ≥ 6, and fewer than six years of education or equivalent occupational history.
For the present analysis, cognitively normal (CN) individuals and participants with MCI were selected. MCI classification required at least one of the following: (i) a Mini-Mental State Examination (MMSE) score between 24 and 30, (ii) a Clinical Dementia Rating (CDR) score of 0.5 with a memory box score ≥ 0.5, or (iii) a Logical Memory II subscale score from the Wechsler Memory Scale below the age-specific normative cutoff. All diagnostic criteria adhered to standards established by the National Institute of Neurological and Communicative Disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association.
Participants were eligible for inclusion if they had complete baseline data for T2-weighted MRI measurements, plasma biomarker levels, and cognitive scores. Outliers were identified and excluded using a threshold of ± 2 standard deviations from the mean. After applying these criteria, a total of 338 participants were included in the analysis: 209 CN and 129 MCI individuals. All plasma biomarker measurements, cognitive assessments, and T2 MRI scans included in this study were collected between January 23, 2017 and March 14, 2023 as part of the ADNI-3 phase.
Mini-Mental state examination (MMSE)
The MMSE is a widely validated tool for assessing global cognitive function in older adults. It consists of 11 items evaluating orientation, registration, attention, calculation, recall, and language, with a maximum score of 30. The MMSE is brief and easily administered across clinical and research settings. A total score of 24 or higher is typically considered indicative of normal cognitive performance, whereas scores below 24 suggest cognitive impairment45,46,47.
APOE genotyping
APOE genotyping was performed by the ADNI Biomarker Core using standard polymerase chain reaction (PCR) amplification followed by restriction enzyme digestion to determine ε2, ε3, and ε4 allele status. Genotype calling and quality control procedures were conducted centrally and harmonized across collection sites. Participants were categorized as APOE ε4 carriers (at least one ε4 allele) or non-carriers.
Plasma biomarkers
Plasma samples were collected in EDTA tubes, processed according to the ADNI Procedures Manual, and stored at − 80 °C until analysis. On the day of testing, samples were thawed and analyzed for p-tau217, Aβ42, and Aβ40 using chemiluminescent immunoassays (RUO IVD kits) on the Fujirebio Lumipulse G1200 platform, and for NfL and GFAP using Simoa Neurology 2-Plex B kits on the Quanterix HD-X platform.
The Lumipulse assays were performed in singlicate using analyte-specific reagents, and quality control included dual plasma pools. Analytical precision across multiple runs ranged from 5.1% to 9.9%, and lot-to-lot consistency for p-tau217 was confirmed (R² = 0.989). The Simoa platform employed a bead-based immunoassay in duplicate, with final signal quantification derived from individual fluorescent bead responses. Precision for NfL and GFAP ranged from 6.0% to 10.6% and 6.8% to 9.9%, respectively.
Provisional cut-points, based on an independent UPenn cohort and validated in ADNI, were applied as follows: p-tau217: negative < 0.128 pg/mL, intermediate 0.129–0.299 pg/mL, positive > 0.300 pg/mL; p-tau217/Aβ42: negative < 0.0055, intermediate 0.0056–0.0085, positive > 0.0086. Cut-points for NfL and GFAP have not been established.
Hippocampal subfield segmentation
High-resolution volumetric measurements of hippocampal subfields and select MTL cortical regions were derived using the Automatic Segmentation of Hippocampal Subfields (ASHS) software, version 1.0.0 (https://sites.google.com/site/hipposubfields/). Segmentations were applied to co-registered high-resolution T2-weighted and standard T1-weighted MRI scans acquired during the same session.
MRI acquisition was performed across multiple ADNI sites using 3T scanners from Siemens, GE, or Philips. While scanner models and sequence parameters varied slightly between sites, all were harmonized using standardized ADNI acquisition protocols to minimize inter-scanner variability. Scanner type and site were recorded and included as covariates in downstream analyses when appropriate.
ASHS employs a multi-atlas label fusion approach combined with a learning-based error correction algorithm to produce fully automated segmentations of hippocampal subfields along the anterior–posterior axis of the hippocampal formation, as well as select MTL cortical regions48. Candidate segmentations are first generated by mapping subject images to multiple manually labeled atlases, which are fused into a consensus label map weighted by atlas similarity. Systematic segmentation errors are then corrected using a trained post-processing model.
The regions of interest (ROIs) included in the current study were: hippocampal subfields CA1, CA2, CA3, dentate gyrus (DG), subiculum, and extrahippocampal cortical regions entorhinal cortex (ERC), parahippocampal cortex (PHC), Brodmann area 35 (BA35), and Brodmann area 36 (BA36)49. To reduce hemispheric variability and improve reliability for small subfields, volumes were averaged across the left and right hemispheres for all ROIs and used in the primary analyses49.
To account for individual differences in head size, all volumetric measures were normalized to total intracranial volume (TIV), in line with established approaches to reduce gender- and region-specific bias50. For extrahippocampal cortical regions (ERC, PHC, BA35, BA36), normalized volumes were further adjusted by dividing raw values by the number of slices containing each ROI to correct for partial coverage.
Due to segmentation noise in CA2 and CA3 subfields, analyses focused primarily on CA1 and a composite CA measure (CA1 + CA2 + CA3). All images underwent quality assurance (QA) scoring (range 0–4), and only scans with QA > 1 were included. QA ratings reflect overall image usability, with lower scores typically resulting from motion artifacts or suboptimal slab orientation.
This approach yielded 11 distinct volumetric measures for the primary analyses: CA1, CA (CA1 + CA2 + CA3), DG, subiculum, ERC, PHC, BA35, BA36, and their averaged left-right hemispheric values. These measures were subsequently used in linear regression and ROC analyses to assess associations with plasma AD biomarkers.
Statistical analysis
All statistical analyses were conducted in Python using the following packages: Pandas (v2.1.4), Statsmodels (v0.14.0), Pingouin (v0.5.4), SciPy (v1.12.0), and NumPy (v1.26.4). The Shapiro–Wilk test was employed to assess the normality of continuous variable distributions. Normally distributed variables were summarized as mean ± standard deviation (SD), while non-normally distributed variables were described using appropriate nonparametric statistics. Categorical variables were reported as counts and percentages.
Between-group comparisons were performed using independent-sample t-tests for normally distributed continuous variables and Mann–Whitney U tests for non-normal variables. Group differences in categorical variables were assessed using the chi-square test.
Associations between individual plasma biomarker concentrations and T2-weighted MRI measures were examined using linear regression models. All models were adjusted for relevant covariates, including age, sex, APOE ε4 carrier status, years of education, and ethnicity. Model diagnostics included inspection of quantile–quantile (Q–Q) plots and the Shapiro–Wilk test to assess residual normality, residual-versus-fitted value plots to evaluate homoscedasticity, and variance inflation factor (VIF) analyses to rule out multicollinearity. To account for multiple comparisons, p-values from regression analyses were corrected using the Benjamini–Hochberg false discovery rate (FDR) method.
Causal mediation analysis was conducted to estimate the extent to which the associations between plasma p-tau217 and the p-tau217/Aβ1–42 ratio and T2 MRI-derived volumetric measurements of MLT subregions were mediated through other plasma biomarkers, including GFAP and NfL. Mediation was evaluated within a linear model framework, providing estimates of the total, direct, and indirect effects. Standard errors were computed using nonparametric bootstrapping.
To assess the discriminative ability of MRI-derived regional volumes in classifying amyloid and tau biomarker status, logistic regression analyses were conducted. For this purpose, provisional cut-points from an independent UPenn cohort validated in ADNI were applied to define biomarker positivity (for p-tau217, p-tau217/Aβ₁₋₄₂, and Aβ₁₋₄₂/Aβ₁₋₄₀). Using these categorical outcomes, receiver operating characteristic (ROC) curve analyses were performed to quantify classification performance across diagnostic groups. The area under the curve (AUC), 95% confidence intervals (derived via 1,000 bootstrap resamples), and optimal sensitivity and specificity values were calculated for each brain region and biomarker combination.
Results
Baseline characteristics
Table 1 presents the baseline demographic and clinical characteristics of the CN and MCI groups. Participants with MCI were significantly older than those in the CN group (P = 0.014). Gender distribution also differed significantly between groups (P = 0.008). The frequency of ApoE ε4 carriers did not differ significantly between groups (P = 0.558). The CN group had a significantly higher mean level of education than the MCI group (P = 0.002). The MCI group showed greater cognitive impairment, with significantly higher CDR-SB scores (P < 0.001) and lower MMSE scores (P < 0.001) compared to the CN group.
Plasma biomarker profiles
Participants in the MCI group exhibited significantly elevated levels of plasma p-tau217 (P < 0.001). Similarly, the p-tau217/Aβ1−42 ratio was significantly higher in MCI participants (0.01 ± 0.01 pg/mL) (P = 0.001). Although no significant differences were observed in absolute concentrations of Aβ1−42 (P = 0.37) or Aβ1−40 (P = 0.305), the Aβ1−42/Aβ1−40 ratio was significantly reduced in the MCI group (P = 0.001), indicating a subtle shift in amyloid processing. Additionally, p-NfL, a marker of axonal injury, was significantly elevated in the MCI group (P = 0.001). GFAP levels were also higher in MCI (P = 0.015), suggesting increased astroglial activation in the prodromal phase of cognitive decline (see Table 2).
Medial temporal lobe volumetric differences
Table 3 details the comparison of volumetric measurements derived from high-resolution coronal T2-weighted MRI across subregions of the MTL. Overall, participants with MCI exhibited widespread and statistically significant volume reductions in several hippocampal and parahippocampal subregions, particularly within the CA subfields and dentate gyrus (DG), consistent with early neurodegenerative changes. In the left hemisphere, significant volume loss in the MCI group was observed in the CA1 subfield (P = 0.002), DG (P = 0.001), and subiculum (P = 0.037). Notably, the composite CA volume was also significantly reduced in MCI (P = 0.002), as was the combined hippocampal volume (P < 0.001). Interestingly, the sulcal region volume was markedly greater in MCI (P < 0.001), suggesting compensatory expansion of CSF spaces. In the right hemisphere, similar patterns of atrophy were evident. The MCI group showed significant reductions in CA1 (P = 0.001), CA2 (P = 0.003), DG (P = 0.002), and subiculum (P = 0.043). The right hemisphere CA volume (P = 0.001) and the aggregate hippocampal volume (P < 0.001) were also significantly lower in MCI. Increased sulcal volume was again noted in MCI (P = 0.019).
Associations between plasma biomarkers and MTL volumes
In the total cohort, higher p-tau217/Aβ1–42 levels were associated with reduced right hippocampal (β = − 0.20, FDR p = 0.004), right CA1 (β = − 0.19, FDR p = 0.008), and right CA (β = − 0.19, FDR p = 0.010) volumes. Similarly, higher p-tau217 levels were linked to smaller right hippocampal volume (β = − 0.17, FDR p = 0.014) and right CA1 volume (β = − 0.16, FDR p = 0.022). Conversely, both p-tau217 and p-tau217/Aβ1–42 were positively associated with larger right miscellaneous (MISC) region volume (β range = 0.18–0.21, FDR p ≤ 0.008). Elevated GFAP levels were also associated with greater left sulcal volume (β = 0.18, FDR p = 0.012). In addition, higher Aβ1–42/Aβ1–40 ratios were related to smaller right MISC volume (β = − 0.13, FDR p = 0.049).
Stratified analyses revealed significant associations in the MCI group. Higher p-tau217/Aβ1–42 levels showed robust negative associations with right CA1 (β = − 0.37, FDR p = 0.002), right hippocampus (β = − 0.36, FDR p = 0.003), right CA (β = − 0.36, FDR p = 0.003), right dentate gyrus (β = − 0.31, FDR p = 0.012), left CA (β = − 0.31, FDR p = 0.014), left hippocampus (β = − 0.30, FDR p = 0.019), left CA1 (β = − 0.29, FDR p = 0.026), right entorhinal cortex (β = − 0.27, FDR p = 0.041), and right CA (β = − 0.36, FDR p = 0.003). Higher p-tau217 levels also showed consistent inverse relationships with bilateral hippocampal subregions, including right CA1 (β = − 0.29, FDR p = 0.008), right CA (β = − 0.28, FDR p = 0.013), right hippocampus (β = − 0.28, FDR p = 0.015), right dentate gyrus (β = − 0.24, FDR p = 0.034), left CA (β = − 0.28, FDR p = 0.018), left CA1 (β = − 0.25, FDR p = 0.030), left hippocampus (β = − 0.27, FDR p = 0.022), and right entorhinal cortex (β = − 0.26, FDR p = 0.041). Additionally, higher GFAP levels were associated with reduced right hippocampal volume (β = − 0.26, FDR p = 0.032), whereas greater Aβ1–42/Aβ1–40 ratios were linked to increased right dentate gyrus volume (β = 0.28, FDR p = 0.012).
In the CN group, three significant associations were identified. Higher GFAP levels were associated with increased left sulcal volume (β = 0.21, FDR p = 0.022), and both p-tau217 and p-tau217/Aβ1–42 were positively related to larger left hippocampal volume (β range = 0.18–0.20, FDR p = 0.040) (see Table 4; Fig. 1).
Mediation analyses
We also conducted mediation analyses to determine whether the associations between plasma p-tau217 or the p-tau217/Aβ1–42 ratio and volumetric measurements of MLT subregions derived from high-resolution coronal T2 MRI were mediated by other plasma biomarkers. Significant mediation effects were observed in CN individuals.
Higher p-tau217/Aβ1–42 was strongly associated with increased GFAP concentrations (β = 0.50, SE = 0.08, FDR p < 0.001). Although GFAP was not directly related to left hemispheric sulcal volume (β = 0.19, SE = 0.07, FDR p = 0.061), the indirect pathway linking p-tau217/Aβ1–42 to sulcal volume via GFAP reached significance (indirect β = 0.11, SE = 0.05, FDR p = 0.048).
Similarly, p-tau217 and p-tau217/Aβ1–42 were both strongly associated with NfL (β = 0.48 and 0.41, respectively; both FDR p < 0.001). While NfL was not directly associated with parahippocampal cortex volume (β = −0.11, SE = 0.09, FDR p = 0.494), significant indirect effects were observed. Higher p-tau217 (indirect β = −0.09, SE = 0.05, FDR p = 0.048) and higher p-tau217/Aβ1–42 (indirect β = −0.08, SE = 0.03, FDR p = 0.028) were associated with reduced parahippocampal cortex volume through elevated NfL (Table 5).
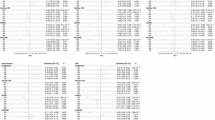
ROC curve analyses
Figures 2 and 3; Table 6 present ROC curves evaluating the ability of MLT subregional volumes, derived from high-resolution coronal T2-weighted MRI, to discriminate p-tau217/Aβ1–42, and p-tau217 positivity in CN and MCI groups, respectively. These findings highlight that structural alterations in MLT subregions are more strongly associated with amyloid and tau burden in individuals with MCI compared to those who are cognitively normal, supporting the utility of volumetric MRI markers in early Alzheimer’s disease detection and staging.
Discussion
Our investigation demonstrates that plasma p-tau217 and its composite ratio with Aβ1–42 track both molecular pathology and mesial-temporal neurodegeneration across the cognitive continuum. Higher circulating p-tau217 predicted smaller volumes in multiple hippocampal subfields—most consistently CA1—and these associations were accentuated once objective impairment emerged, whereas cognitively normal individuals showed weak or inverse relations. These findings integrate fluid biomarkers with ultra-high-resolution volumetry, extending the mechanistic bridge between soluble tau species and focal atrophy.
Plasma p-tau217 has emerged as the most sensitive blood-based indicator of AD pathology, demonstrating stronger associations with amyloid and tau PET, earlier dynamic elevation, and clearer discrimination across disease stages compared with other p-tau epitopes. Longitudinal cohorts have shown that p-tau217 rises earlier and more steeply during preclinical and prodromal phases, closely paralleling cognitive decline and regional neurodegeneration51,52,53. Our findings are consistent with this literature, with p-tau217 showing robust associations with subfield-specific atrophy, particularly within CA1, supporting its role as a superior dynamic marker of early neurodegenerative change.
Beyond absolute concentrations, ratio metrics that normalize tau to Aβ have been proposed to enhance discriminative power and to mitigate inter-individual variance. In keeping with Nature Medicine cohorts showing that Aβ42/40-adjusted plasma tau markers outperform single-analyte assays for predicting PET positivity54, the p-tau217/Aβ1–42 ratio in our study was the strongest biochemical correlate of hippocampal volume in MCI, especially within CA1 (β = − 0.38, P = 0.001). Ratio-based markers therefore appear to capture the integrated burden of upstream amyloidosis and downstream tauopathy more effectively than any single biomarker.
The anatomical selectivity we detected echoes classical neuropathology. CA1 neurons are disproportionately vulnerable to early tangle formation and loss in AD, whereas CA3/dentate gyrus (DG) changes align with encoding deficits55. Mueller et al. used 4-T MRI to show that delayed-recall performance correlates with CA1, while immediate-learning measures map to CA3/DG volumes55. Our observation that plasma tau species predominantly correlate with CA1 atrophy extends the structural-cognitive connections to a peripheral biomarker, reinforcing the idea that soluble p-tau indicates neuronal injury in circuits essential for memory consolidation.
The strong correlation between plasma p-tau and focal atrophy aligns with longitudinal imaging findings, indicating that baseline tau-PET intensity, rather than amyloid burden, forecasts both the extent and distribution of subsequent cortical thinning. La Joie and colleagues further showed that tau-PET explains ~ 40% of the variance in one-year atrophy, independent of baseline thickness56. Our data expand this cascade by indicating that peripheral p-tau217 may serve as an accessible surrogate for the intracerebral tau burden driving neurodegeneration.
An additional finding requiring interpretation is the hemispheric asymmetry in biomarker–atrophy associations. In MCI individuals, p-tau217 and its ratio showed stronger and more consistent relationships with right hippocampal and CA1 volumes, whereas cognitively normal participants exhibited positive or compensatory associations predominantly within the left hippocampus. This pattern is biologically plausible. Prior imaging studies have reported that the right hippocampus may show earlier vulnerability during prodromal AD and MCI progression57,58, particularly in networks supporting spatial and contextual memory processing59,60. In contrast, the left hippocampus, more integrated with language-based and semantic systems, often exhibits greater functional reserve or compensatory hypertrophy during early disease stages61. Intrinsic hemispheric differences in connectivity, metabolic demand, and susceptibility to tau propagation may further modulate these patterns62,63. Collectively, these findings highlight the importance of evaluating lateralized trajectories rather than relying solely on whole-hippocampal averages.
Clinically, these results have several implications. First, plasma p-tau217 (alone or ratio-normalized) could be deployed as a low-cost triage tool to enrich trials with individuals harboring imminent hippocampal degeneration, thereby reducing reliance on expensive PET or lumbar puncture. Second, because CA1 atrophy underlies episodic memory decline, blood-based identification of patients at greatest risk for CA1 loss may allow for earlier cognitive preservation interventions. Third, the biochemical-anatomical linkage suggests the use of combined endpoints—plasma p-tau trajectories and subfield-specific MRI volumetry—to track disease-modifying effects with greater sensitivity.
Strengths of the present work include integration of state-of-the-art single-molecule assays with harmonized high-resolution segmentation, addressing prior concerns about protocol heterogeneity in subfield delineation64. Nonetheless, limitations merit mention. Our cross-sectional biomarker-atrophy analyses cannot resolve temporal ordering; prospective sampling will be necessary to confirm that rising p-tau217 precedes subfield shrinkage. Although we carefully adjusted for age, APOE, and education, residual confounding from cerebrovascular or Lewy body co-pathology cannot be excluded. Indeed, α-synuclein aggregates have independent cognitive effects even in clinically normal individuals65. Finally, the cohort was recruited from a single academic center; validation in population-based samples is required for generalizability.
Subsequent research should investigate if the integration of plasma p-tau217 with indicators of glial reactivity and neurofilament light enhances the prediction of non-hippocampal atrophy and clinical progression. The age-dependency of tau-atrophy coupling seen in PET cohorts56 necessitates investigation in plasma, as younger patients may experience larger advantages from tau-targeted treatments. Applying deep learning to serial plasma data may further elucidate non-linear dynamics and personalised risk.
Conclusion
Our findings highlight plasma p-tau217—and especially the p-tau217/Aβ1–42 ratio—as sensitive indicators of medial temporal lobe degeneration. In the total cohort, higher p-tau217 and p-tau217/Aβ1–42 levels were associated with reduced right hippocampal and CA1 volumes, whereas in MCI individuals, these associations extended bilaterally across hippocampal subregions and the entorhinal cortex, underscoring their value for detecting early neurodegeneration. Notably, in cognitively normal individuals, higher p-tau217 and p-tau217/Aβ1–42 levels correlated with greater left hippocampal volume, and elevated GFAP levels with increased left sulcal volume, suggesting early glial activation or compensatory structural responses preceding atrophy. Mediation analyses further showed that GFAP and NfL partially mediated the links between plasma tau/amyloid ratios and regional volumes, integrating molecular and structural markers of disease. Together, these results bridge peripheral biomarker changes with precise neuroanatomical alterations, supporting the use of plasma biomarkers as minimally invasive tools for early detection, staging, and monitoring of Alzheimer’s disease.
Data availability
The datasets generated and analyzed during this study are not publicly available due to privacy concerns. However, these data can be obtained from the corresponding author upon reasonable request. Additionally, the custom code used for the analysis in this study is available from the corresponding author upon request. For drawing the graphic abstract, we have been using BioRender software under license.
References
2023 Alzheimer’s disease facts and figures. Alzheimer’s Dement 19 (4), 1598–1695 (2023).
Li, W. W. et al. Brain Amyloid-β deposition and blood biomarkers in patients with clinically diagnosed alzheimer’s disease. J. Alzheimers Dis. 69 (1), 169–178 (2019).
Rabinovici, G. D. et al. Association of amyloid positron emission tomography with subsequent change in clinical management among medicare beneficiaries with mild cognitive impairment or dementia. JAMA 321 (13), 1286–1294 (2019).
Liu, Z. et al. Pathophysiology Characterization of Alzheimer’s Disease in South China’s Aging Population: for the Greater-Bay-Area Healthy Aging Brain Study (GHABS) Vol. 16, 84 (Alzheimer’s Research & Therapy, 2024).
van Dyck, C. H. et al. Lecanemab in early Alzheimer’s disease. N. Engl. J. Med. 388 (1), 9–21 (2023).
Sims, J. R. et al. Donanemab in early symptomatic alzheimer disease: The TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA 330 (6), 512–527 (2023).
Consortium, A. B. et al. A framework of biomarkers for brain aging: a consensus statement by the aging biomarker consortium. Life Med. 2 (3) (2023).
Ashton, N. J. et al. Differential roles of Aβ42/40, p-tau231 and p-tau217 for alzheimer’s trial selection and disease monitoring. Nat. Med. 28 (12), 2555–2562 (2022).
Verberk, I. M. W. et al. Plasma amyloid as prescreener for the earliest alzheimer pathological changes. Ann. Neurol. 84 (5), 648–658 (2018).
Pichet Binette, A. et al. Combining Plasma Phospho-tau and Accessible Measures to Evaluate Progression to Alzheimer’s Dementia in Mild Cognitive Impairment Patients Vol. 14, 46 (Alzheimer’s Research & Therapy, 2022).
Palmqvist, S. et al. Prediction of future Alzheimer’s disease dementia using plasma phospho-tau combined with other accessible measures. Nat. Med. 27 (6), 1034–1042 (2021).
Mattsson-Carlgren, N. et al. Prediction of longitudinal cognitive decline in preclinical alzheimer disease using plasma biomarkers. JAMA Neurol. 80 (4), 360–369 (2023).
Teunissen, C. E. et al. Blood-based biomarkers for Alzheimer’s disease: Towards clinical implementation. Lancet Neurol. 21 (1), 66–77 (2022).
Alcolea, D. et al. Blood biomarkers in neurodegenerative diseases: Implications for the clinical neurologist. Neurology 101 (4), 172–180 (2023).
Nakamura, A. et al. High performance plasma amyloid-β biomarkers for Alzheimer’s disease. Nature 554 (7691), 249–254 (2018).
Janelidze, S. et al. Plasma β-amyloid in Alzheimer’s disease and vascular disease. Sci. Rep. 6 (1), 26801 (2016).
Ashton, N. J. et al. Plasma and CSF biomarkers in a memory clinic: Head-to-head comparison of phosphorylated Tau immunoassays. Alzheimers Dement. 19 (5), 1913–1924 (2023).
Schindler, S. E. et al. High-precision plasma β-amyloid 42/40 predicts current and future brain amyloidosis. Neurology 93 (17), e1647–e1659 (2019).
Montoliu-Gaya, L. et al. Blood biomarkers for Alzheimer’s disease in down syndrome. J. Clin. Med., 10 (16) (2021).
Janelidze, S. et al. Head-to-Head comparison of 8 plasma Amyloid-β 42/40 assays in alzheimer disease. JAMA Neurol. 78 (11), 1375–1382 (2021).
Bayoumy, S. et al. Clinical and analytical comparison of six Simoa assays for plasma P-tau isoforms P-tau181, P-tau217, and P-tau231. Alzheimers Res. Ther. 13 (1), 198 (2021).
Illán-Gala, I. et al. Plasma Tau and neurofilament light in frontotemporal Lobar degeneration and alzheimer disease. Neurology 96 (5), e671–e683 (2021).
Teunissen, C. E., Thijssen, E. H. & Verberk, I. M. W. Plasma p-tau217: From ‘new kid’ to most promising candidate for Alzheimer’s disease blood test. Brain 143 (11), 3170–3172 (2020).
Salvadó, G. et al. Specific associations between plasma biomarkers and postmortem amyloid plaque and Tau tangle loads. EMBO Mol. Med. 15 (5), e17123 (2023).
Janelidze, S. et al. Head-to-head comparison of 10 plasma phospho-tau assays in prodromal alzheimer’s disease. Brain 146 (4), 1592–1601 (2023).
Ashton, N. J. et al. Diagnostic accuracy of the plasma ALZpath pTau217 immunoassay to identify Alzheimer’s disease pathology. medRxiv (2023).
Cullen, N. C. et al. Test-retest variability of plasma biomarkers in alzheimer’s disease and its effects on clinical prediction models. Alzheimers Dement. 19 (3), 797–806 (2023).
Milà-Alomà, M. et al. Plasma p-tau231 and p-tau217 as state markers of amyloid-β pathology in preclinical alzheimer’s disease. Nat. Med. 28 (9), 1797–1801 (2022).
Yu, L. et al. Plasma p-tau181 and p-tau217 in discriminating PART, AD and other key neuropathologies in older adults. Acta Neuropathol. 146 (1), 1–11 (2023).
Pais, M. V., Forlenza, O. V. & Diniz, B. S. Plasma biomarkers of alzheimer’s disease: A review of available Assays, recent Developments, and implications for clinical practice. J. Alzheimers Dis. Rep. 7 (1), 355–380 (2023).
Jack, C. R. et al. Predicting amyloid PET and Tau PET stages with plasma biomarkers. Brain 146 (5), 2029–2044 (2023).
Therriault, J. et al. Association of phosphorylated Tau biomarkers with amyloid positron emission tomography vs Tau positron emission tomography. JAMA Neurol. 80 (2), 188–199 (2023).
Therriault, J. et al. Equivalence of Plasma p-tau217 with Cerebrospinal Fluid in the Diagnosis of Alzheimer’s Disease Vol. 19, 4967–4977 (Alzheimer’s & Dementia, 2023).
Groot, C. et al. Diagnostic and prognostic performance to detect alzheimer’s disease and clinical progression of a novel assay for plasma p-tau217. Alzheimers Res. Ther. 14 (1), 67 (2022).
Palmqvist, S. et al. Discriminative accuracy of plasma Phospho-tau217 for alzheimer disease vs other neurodegenerative disorders. JAMA 324 (8), 772–781 (2020).
Hansson, O. et al. The Alzheimer’s association appropriate use recommendations for blood biomarkers in alzheimer’s disease. Alzheimers Dement. 18 (12), 2669–2686 (2022).
Battineni, G. et al. Improved Alzheimer’s disease detection by mri using multimodal machine learning algorithms. Diagnostics (Basel) 11 (11) (2021).
de Flores, R. et al. Contribution of mixed pathology to medial Temporal lobe atrophy in alzheimer’s disease. Alzheimers Dement. 16 (6), 843–852 (2020).
Bussy, A. et al. Hippocampal subfield volumes across the healthy lifespan and the effects of MR sequence on estimates. Neuroimage 233, 117931 (2021).
Lenhart, L. et al. Anatomically standardized detection of MRI atrophy patterns in early-stage Alzheimer’s disease. Brain Sci. 11 (11) (2021).
Stark, S. M., Frithsen, A. & Stark, C. E. L. Age-related alterations in functional connectivity along the longitudinal axis of the hippocampus and its subfields. Hippocampus 31 (1), 11–27 (2021).
Karimani, F. et al. Impairment of entorhinal cortex network activity in alzheimer’s disease. Front. Aging Neurosci. 16, 1402573 (2024).
McKhann, G. et al. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of department of health and human services task force on Alzheimer’s disease. Neurology 34 (7), 939–944 (1984).
Petersen, R. C. et al. Alzheimer’s disease neuroimaging initiative (ADNI): clinical characterization. Neurology 74 (3), 201–209 (2010).
Tombaugh, T. N. & McIntyre, N. J. The mini-mental state examination: A comprehensive review. J. Am. Geriatr. Soc. 40 (9), 922–935 (1992).
Arevalo-Rodriguez, I. et al. Mini-Mental state examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). Cochrane Datab. Syst. Rev. 2015 (3), pCd010783 (2015).
Mitchell, A. J. The mini-mental state examination (MMSE): Update on its diagnostic accuracy and clinical utility for cognitive disorders, in Cognitive Screening Instruments: A Practical Approach (ed Larner, A. J.) 37–48 (Springer, 2017).
Yushkevich, P. A. et al. Automated volumetry and regional thickness analysis of hippocampal subfields and medial Temporal cortical structures in mild cognitive impairment. Hum. Brain Mapp. 36 (1), 258–287 (2015).
Cao, J. et al. The hippocampal subfield volume reduction and plasma biomarker changes in mild cognitive impairment and Alzheimer’s disease. J. Alzheimers Dis. 98 (3), 907–923 (2024).
Voevodskaya, O. et al. The effects of intracranial volume adjustment approaches on multiple regional MRI volumes in healthy aging and Alzheimer’s disease. Front. Aging Neurosci. 6, 264 (2014).
Karikari, T. K. et al. Blood phosphorylated Tau 181 as a biomarker for alzheimer’s disease: a diagnostic performance and prediction modelling study using data from four prospective cohorts. Lancet Neurol. 19 (5), 422–433 (2020).
Janelidze, S. et al. Plasma P-tau181 in Alzheimer’s disease: Relationship to other biomarkers, differential diagnosis, neuropathology and longitudinal progression to Alzheimer’s dementia. Nat. Med. 26 (3), 379–386 (2020).
Mattsson-Carlgren, N. et al. Longitudinal plasma p-tau217 is increased in early stages of alzheimer’s disease. Brain 143 (11), 3234–3241 (2020).
Thijssen, E. H. et al. Diagnostic value of plasma phosphorylated tau181 in Alzheimer’s disease and frontotemporal Lobar degeneration. Nat. Med. 26 (3), 387–397 (2020).
Mueller, S. G. et al. Evidence for functional specialization of hippocampal subfields detected by MR subfield volumetry on high resolution images at 4 T. Neuroimage 56 (3), 851–857 (2011).
La Joie, R. et al. Prospective Longitudinal Atrophy in Alzheimer’s Disease Correlates with the Intensity and Topography of Baseline Tau-PET. Sci. Transl. Med. 12 (524) (2020).
Lombardi, G. et al. Structural magnetic resonance imaging for the early diagnosis of dementia due to alzheimer’s disease in people with mild cognitive impairment. Cochrane Datab. Syst. Rev. 3 (3), pCd009628 (2020).
Shi, F. et al. Hippocampal volume and asymmetry in mild cognitive impairment and alzheimer’s disease: Meta-analyses of MRI studies. Hippocampus 19 (11), 1055–1064 (2009).
Burgess, N., Maguire, E. A. & O’Keefe, J. The human hippocampus and Spatial and episodic memory. Neuron 35 (4), 625–641 (2002).
Iglói, K. et al. Lateralized human hippocampal activity predicts navigation based on sequence or place memory. Proc. Natl. Acad. Sci. U S A. 107 (32), 14466–14471 (2010).
Ezzati, A. et al. Differential association of left and right hippocampal volumes with verbal episodic and Spatial memory in older adults. Neuropsychologia 93 (Pt B), 380–385 (2016).
Vogel, J. W. et al. Spread of pathological Tau proteins through communicating neurons in human Alzheimer’s disease. Nat. Commun. 11 (1), 2612 (2020).
Greicius, M. D. et al. Functional connectivity in the resting brain: A network analysis of the default mode hypothesis. Proc. Natl. Acad. Sci. U S A. 100 (1), 253–258 (2003).
Yushkevich, P. A. et al. Quantitative comparison of 21 protocols for labeling hippocampal subfields and parahippocampal subregions in in vivo MRI: Towards a harmonized segmentation protocol. Neuroimage 111, 526–541 (2015).
Palmqvist, S. et al. Cognitive effects of lewy body pathology in clinically unimpaired individuals. Nat. Med. 29 (8), 1971–1978 (2023).
Acknowledgements
Data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California. Data used in preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in analysis or writing of this report. A complete listing of ADNI investigators can be found at: http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf
Funding
Not applicable.
Author information
Authors and Affiliations
Consortia
Contributions
A.R., A.N., and F.Kh., each contributed to writing the draft. All authors reviewed and approved the final version of the manuscript. H.N. and A.Gh. wrote the Methods and Results sections and analyzed the data. All authors listed have made a substantial, direct, and intellectual contribution to the work, and approved it for publication. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study was conducted following the Declaration of Helsinki. All ADNI data used were de-identified, and the use of these data for research purposes was approved by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) Data Sharing and Publications Committee.
Consent to participate
As this study utilized pre-existing datasets obtained from an online repository using previously conducted research, direct informed consent from participants was not applicable. However, all datasets were originally collected in compliance with ethical standards, including obtaining informed consent from participants at the time of data acquisition. The current analysis adhered strictly to ethical guidelines, ensuring that all data remained anonymized and deidentified, with no potential for re-identification of participants. Relevant approvals for the use of these datasets were obtained where required, and the study was conducted following the principles outlined in the Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Rabiei rad, A., Nadaki, A., Khosravi, F. et al. Plasma p-tau217 and p-tau217/Aβ1–42 ratios associate with medial temporal lobe subfield atrophy in normal aging and mild cognitive impairment. Sci Rep 16, 2692 (2026). https://doi.org/10.1038/s41598-025-32404-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-32404-0