Abstract
This nationwide register-based cohort study examined the association between castration status and postoperative survival in men who had undergone surgery for spinal metastases from prostate cancer. Bone metastases are common in prostate cancer, with the spine being the most frequent site. Using data from the Swedish Spine Register (Swespine) and Prostate Cancer Database Sweden (PCBaSe), 306 men with prostate cancer who underwent spinal surgery were identified. In total, 81 were categorized as castration-sensitive and 225 as castration-resistant disease at the time of spinal surgery. Postoperative survival was estimated using Kaplan–Meier analysis and compared with the log-rank test. Multivariable Cox regression was used to adjust for potential confounders. Median survival after surgery was significantly longer in men with castration-sensitive prostate cancer (33 months, IQR 15–55) compared to those with castration-resistant disease (8 months, IQR 5–31; p < 0.001). Castration-sensitive status was independently associated with a lower risk of death (hazard ratio 0.29, 95% CI: 0.20–0.41). These findings indicate that castration sensitivity is a strong prognostic factor for survival after surgery for spinal metastases from prostate cancer and should be considered in surgical decision-making.
Similar content being viewed by others
Introduction
Bone metastases are found in approximately 10% of men with prostate cancer at the time of initial diagnosis and are found in more than 80% of patients with advanced metastatic disease 1,2. Metastasis can occur either during the castration-sensitive stage or after the disease progresses to a castration-resistant state 3. The spine is the most common site of bone metastasis 2. Patients with spinal metastases often present with pain, pathological fractures, and/or acute progressive neurological symptoms due to metastatic spinal cord compression (MSCC) 4.
Compared with radiotherapy alone, surgery combined with radiotherapy has been shown to improve outcomes in patients with MSCC 4. However, surgery is associated with high risks of complications, morbidity and mortality 5,6, and is generally only recommended if the life expectancy is expected to exceed 3‒6 months 7. The process for selecting patients with spinal metastases or MSCC who would most likely benefit from treatment is complex, and the estimation of life expectancy is crucial. However, the factors influencing survival following surgical treatment for spinal metastases of prostate cancer remain poorly understood.
In a systematic review, castration-sensitivity and a high Karnofsky performance status were associated with prolonged survival following surgery for spinal metastases 8. Several cohort studies have revealed an association between the castration state at the time of spinal surgery and survival in prostate cancer patients with MSCC. However, the number of patients with castration-sensitive prostate cancer was consistently low across these studies 9,10,11,12,13. Furthermore, the castration-sensitive state was not included as a factor in a later meta-analysis on overall survival in patients with spinal metastases of prostate cancer 14.
The aim of this study was to investigate the association between castration state and survival after surgery for spinal metastases of prostate cancer in a large national multi-register cohort.
Materials and methods
Study design, data sources and setting
This observational study was based on data derived from the Swedish Spine Register (Swespine), the National Prostate Cancer Register (NPCR) of Sweden and the Prostate Cancer Database Sweden (PCBaSe). Swespine has collected data pertaining to spinal surgery since 1993 and data pertaining to surgery for spinal metastases since 2006. Currently, approximately 90% of all spinal surgery units (including all tumor surgery units) in Sweden report to Swespine, and the completeness of patient data is estimated to be approximately 75% 15. The aim of NPCR is to provide a basis for analysis of adherence to national guidelines for prostate cancer with the ultimate aim to improve prostate cancer care for all men in Sweden 16,17. For this purpose, the NPCR registers data on cancer characteristics at the time of diagnosis, diagnostic workup, and primary treatment. In PCBaSe, data in the NPCR have been linked to other nationwide health care registers, including the Prescribed Drug Register, the Patient Register, and the Cause of Death Register 18,19.
Patient selection
We obtained data pertaining to surgeries for spinal metastases classified as either prostate cancer or unknown primary tumors performed between 2011 and 2021 (n = 882) from the Swespine. Only data from the first surgery for each patient was included in the analyses (n = 760). Using the unique personal identity numbers assigned to residents in Sweden, these data were linked to the NPCR to verify the prostate cancer diagnosis and then matched with data pertaining to cancer treatment, classification, and survival in the PCBaSe.
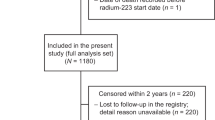
The quality of the data was controlled by removing data pertaining to other primary tumor diagnoses for patients who were registered as having an unknown primary tumor at the time of spinal surgery. We also evaluated duplicate registrations; only the first registration was used. Furthermore, 9 patients were excluded because of an uncertain castration state. The final cohort included 306 patients registered in all three registers (Fig. 1).
Definition of castration-sensitive and castration-resistant prostate cancer
Information on the date of castration resistance was available in PCBaSe for 237 men (Fig. 1). They were classified as castration-sensitive at the time of spinal surgery if surgery occurred before the recorded date of castration resistance, and as castration-resistant if surgery occurred after this date. Symptomatic spinal metastasis that led to spinal surgery was the first manifestation of malignancy in 63 patients, whose prostate cancer diagnosis was established only postoperatively. These patients were therefore classified as castration-sensitive at the time of surgery; among them, 43 had available dates of castration resistance, all occurring after surgery.
In addition, 49 patients had received androgen-deprivation therapy (ADT)—orchidectomy, GnRH agonists, or anti-androgens—prior to spinal surgery but lacked recorded information on castration resistance in the registry. For these patients, ADT type and initiation date were available, and castration resistance was therefore assigned using a clinical definition based on radiographic and/or clinical progression 90 days after ADT (Fig. 1). The presence of spinal metastases causing metastatic spinal cord compression or spinal instability requiring surgical intervention was considered as evidence of such progression 20,21.
To evaluate the validity of this classification, we conducted sensitivity analyses using two other definitions of castration sensitivity at surgery, (i) spinal surgery before start of ADT (n = 63 castration-sensitive; n = 243 castration-resistant) and (ii) spinal surgery within 180 days after start of ADT (n = 96 castration-sensitive; n = 215 castration-resistant).
Variables included
We collected information regarding age at prostate cancer diagnosis, PSA at diagnosis, TNM stage, Gleason score, primary treatment and date of death from the NPCR. Data pertaining to age at surgery, date of surgery, type of surgery, and neurological function prior to surgery according to the Frankel classification were collected from the Swespine. Neurological function was further categorized using the Frankel classification, with patients being classified as nonambulatory (Frankel A, B or C) or ambulatory (Frankel D or E). Using data from the PCBaSe, three different comorbidity indices were calculated: the Charlson Comorbidity Index (CCI), the Drug Comorbidity Index (DCI), and the Multi-Dimensional Comorbidity Index (MDCI) 22,23,24,25,26. For all three indices, we used the date of spinal surgery as the last date of collection of comorbidity data from prior records in The Patient Register and The Prescribed Drug Register.
Statistics
Normally distributed variables are presented as the means with standard deviations (SDs), and nonnormally distributed variables are presented as the medians with interquartile ranges (IQRs). Categorical variables were analyzed with the chi-square test. The start of follow-up was the date of spinal surgery, and the end of follow-up was the date of death or the administrative end of follow-up (31st December 2023), whichever came first. Survival is presented in months.
Crude analysis of survival is displayed in Kaplan–Meier figures. Differences between survival curves were assessed with the log-rank test. Cox proportional hazards with adjusted analyses were performed to evaluate the association between castration state and postoperative survival. The covariates included in the multivariate model were castration state, age at spinal surgery, year of surgery, MDCI, and DCI, all variables were available for all patients. As, 13 patients had missing data for ambulation, a secondary Cox proportional hazard model was also used to evaluate castration state at the time of spinal surgery after adjusting for ambulation, age at surgery and CCI score. The assumption of proportional hazard was tested with Shoenfeld residuals. The associations are presented as hazard ratios (HRs) with 95% confidence intervals (CIs).
A p value < 0.05 was considered to indicate statistical significance. STATA version 17.0 was used for the statistical analysis.
Results
Study patients and descriptive data
The final study cohort comprised 306 men, 81 were classified as having castration-sensitive prostate cancer and 225 classified as having castration-resistant prostate cancer (CRPC) at the time of surgery for spinal metastases (Fig. 1). Among the 81 men with castration-sensitive disease, 63 presented with metastatic spinal cord compression as the initial manifestation of cancer, whereas 18 developed metastases following either curative-intent therapy or during watchful waiting or active surveillance.
The characteristics of the patients at the time of spinal surgery are presented in Table 1 and Table 2, and those at the time of prostate cancer diagnosis are presented in the Supplementary material (Supplementary Table 1). The median age at the time of prostate cancer diagnosis was 67 years (IQR 61–73), and the median age at the time of surgery was 71 years (IQR 67–77). The thoracic spine was the most common location for metastases (n = 191).
Neurological function prior to surgery
Before surgery, 129 of the patients were ambulatory (Frankel grades D and E), 164 patients had lost their ability to walk (Frankel grades A, B, and C), and ambulatory function data were missing for 13 patients (Table 1).
Treatment
Primary treatment at the time of prostate cancer diagnosis
Radical prostatectomy was performed in 36 patients, external curative radiotherapy in 18 patients, brachytherapy in 3 patients, external therapy in combination with brachytherapy in 6 patients, and undefined-type radiotherapy in 2 patients. Noncurative radiotherapy was performed in 212 patients, and active surveillance or watchful waiting was initiated in 17 patients. Three patients had died before the decision was made about primary treatment, and 9 had missing information pertaining to primary treatment. The most common hormone therapy was a combination of GnRH and antiandrogens for flare-up; 267 patients received GnRH, 21 underwent orchidectomy, and 270 patients received antiandrogens either before or after spinal surgery (Supplementary Table 2).
Surgical treatment of the spine
In the total cohort (n = 306), loss of neurological function was the most common indication for surgery, reported in 166 patients. Pain alone was the primary indication in 17 patients, and progressive deformity alone in 3 patients. Combined indications were frequent: 87 patients presented with both neurological impairment and pain, 4 with neurological impairment and progressive deformity, and 6 with pain and progressive deformity. Additionally, 21 patients presented with all three indications, neurological impairment, pain, and progressive deformity. Indication data were missing for 2 patients. Most patients underwent decompression surgery (n = 305). Stabilization was performed in 195 patients and data on stabilization data were unavailable for 9 patients (Table 2). Radiotherapy to the spinal lesion was administered prior to spinal surgery in 10 patients, with a median interval of 15 months (IQR 4–29). Postoperative radiotherapy to the spine was given to 27 patients, with a median interval of 1 month after surgery (IQR 0.5–7).
Survival
The median postoperative survival for the entire cohort was 11 months (IQR 5–31). Survival was significantly longer in the group with castration-sensitive disease, who had a median survival of 33 months (IQR 15–55), compared with 8 months (IQR 4–18) in the CRPC group (p < 0.001) (Fig. 2). In the multivariable model, castration-sensitive disease remained independently associated with longer survival after surgery (HR 0.29, 95% CI: 0.20–0.41) compared with castration-resistant disease (Table 3, Supplementary Table 2). The findings were consistent across the main analysis and both complementary sensitivity analyses, with castration state at the time of surgery persistently showing strong association with survival (Supplementary Table 3). Ambulatory status was not associated with postoperative survival (Supplementary Table 2). Patients who were ambulatory prior to surgery had a median postoperative survival of 11 months (IQR 5–30), whereas non-ambulatory patients had a median postoperative survival of 10 months (IQR 4–30), (p = 0.75).
Discussion
In this nationwide register-based study of spinal metastases from prostate cancer, men with castration-sensitive disease had fourfold longer survival after spinal surgery than men with CRPC.
The presence of spinal metastases typically indicates a poor prognosis, making careful patient selection a critical task. This selection process is based on life expectancy, among other factors. Advances in oncology have significantly improved the prognosis for certain tumors, although these improvements can complicate accurate survival estimation.
Our results are in accordance with previous reports on the impact of castration state on survival in prostate cancer patients with spinal metastases 8,9,10,11,12,13. These studies included few patients with castration-sensitive tumors and a short postoperative follow-up. Huddart et al. 13 reported that among 17 patients, 13 underwent surgical treatment, and 4 received radiotherapy, with a median survival of 627 days after treatment. In a study by Crnalic et al. 10, 8 out of 13 castration-sensitive patients were still alive after surgery, with a median postoperative follow-up of 26 months. Wänman et al. 9 reported a median postoperative survival of 60 months for patients in the castration-sensitive group (n = 26) compared with 5.5 months for patients with CRPC (n = 84) in a local cohort of 110 prostate cancer patients. In a study by Ju et al. 12, all 3 castration-sensitive patients were alive at 37 months, 40 months, and 46 months after surgery. A recent systematic review and meta-analysis assessed prognostic factors for survival in patients with spinal metastases secondary to prostate cancer 14. Factors such as visceral metastases, ambulatory status, extraspinal bone metastases, performance status, time to motor deficit development, and time from primary diagnosis were identified as significantly associated with overall survival 14. However, the castration state was not included in the analysis, likely due to the limited number of patients with castration-sensitive prostate cancer.
In this national cohort, postoperative survival was four times longer in the castration-sensitive group than in the CRPC group. The median survival of 33 months for castration-sensitive prostate cancer patients in our study was comparable to the survival reported for castration-sensitive prostate cancer patients with bone metastases in general 27. This contrasts with the typically reported median survival range of 6–9 months for patients with spinal metastases 28,29, which aligns with the survival observed in the CRPC group in our study.
Our findings highlight the large range in prognosis among men with spinal metastases from prostate cancer. Although survival differences between castration-sensitive and castration-resistant disease are well recognized, our study adds context-specific evidence by demonstrating how castration status at the time of surgery is associated with postoperative survival in patients undergoing spinal procedures. This information can support clinical decision-making by refining expectations regarding outcomes and reinforcing the need for a tailored, multidisciplinary treatment strategy, including awareness of therapeutic options and realistic postoperative survival estimation when considering surgery.
Our classification of castration-sensitive and castration-resistant disease relied on registry data and was supplemented, when necessary, by clinical criteria based on ADT timing and documented progression to spinal metastases. The consistency of results in sensitivity analyses using alternative timeline definitions strengthens the validity of our classification.
We used the CCI, DCI and MDCI to evaluate comorbidities. All three indices were associated with postoperative survival. Similarly, these indices have been validated in previous studies on prostate cancer, confirming their value as tools for assessing comorbidities and their reliability in evaluating survival outcomes in prostate cancer patients 25,26. While a previous study revealed an association between preoperative ambulation ability and improved postoperative survival 28, our findings did not confirm this relationship.
Nater et al. 29 highlighted that the quality of evidence for current predictors of survival following surgery for symptomatic spinal metastases is low. Prostate cancer bone metastases are highly heterogeneous at the genomic, transcriptomic, proteomic, metabolomic and morphological levels, all of which significantly influence survival outcomes 30. A deeper understanding of the complex biology of metastatic prostate cancer, particularly distinguishing castration-sensitive disease as a potentially distinct entity with significant prognostic implications, may enhance the selection of surgical candidates and lead to improved treatment outcomes.
Strengths and limitations
The main strengths of this study include its nationwide design, which provides strong external validity and generalizability, and its large sample size, which ensures high statistical power. Additionally, the depth of information available from high-quality national registries enhances the robustness of the study. The personal identification numbers assigned to all residents of Sweden also facilitate long-term follow-up on survival. The comorbidity indices were adjusted in this study to provide a comparable risk of death, which is in line with the results of randomized control trials 31.
The main limitation is the retrospective register-based design of the study, which has inherent limitations, including miscoding, transferring errors, underreporting, and missing data 15. However, the data in registries were prospectively collected, minimizing the risk of recall bias and we argue that it is unlikely that these limitations affected men with castration sensitive and CRPC differently. Another limitation is that only patients selected for surgery were included, which introduces the potential for selection bias, as these patients are likely to have a more favorable prognosis. A further limitation is the limited information on systemic therapies in the national registers. Although castration status was available, detailed data on specific treatments including second-generation androgen receptor inhibitors, chemotherapy, radiopharmaceuticals, and bone-protecting agents were not captured. Similarly, important clinical parameters such as bone marrow involvement, baseline hemoglobin, platelet count, and LDH were not systematically recorded, limiting our ability to account for cytopenias or bone marrow infiltration, both of which have prognostic relevance in metastatic prostate cancer 32. Additionally, the lack of detailed data on metastatic burden, including metastatic volume, presence of visceral metastases, and the number of affected vertebral levels, were not consistently available in the registers. To partially address patient heterogeneity, our analyses adjusted for comorbidity burden and neurological function at presentation, using MDCI, CCI, and ambulation/Frankel grade.
Conclusion
In this large cohort of men with spinal metastases from prostate cancer, men who underwent spinal metastasis surgery with castration sensitive cancer, had a four-fold longer survival than men with CRPC. Castration state should be considered when selecting prostate cancer patients for spinal surgery.
Data availability
These data cannot be shared publicly because the individual-level data contain potentially identifying and sensitive patient information and cannot be published owing to legislation and ethical review restrictions ( [https://etikprovningsmyndigheten.se](https:/etikprovningsmyndigheten.se) ). The use of data from national health data registers is further restricted by the Swedish Board of Health and Welfare ( [https://www.socialstyrelsen.se/en/](https:/www.socialstyrelsen.se/en) ) and Statistics Sweden ( [https://www.scb.se/en/](https:/www.scb.se/en) ), which are government agencies providing access to linked healthcare registers.
References
Sung, H. et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 71, 209–249 (2021).
Bubendorf, L. et al. Metastatic patterns of prostate cancer: An autopsy study of 1,589 patients. Hum. Pathol. 31(5), 578–583. https://doi.org/10.1053/hp.2000.6698 (2000).
Corres-Mendizabal, J. et al. Metastatic hormone-naive prostate cancer: A distinct biological entity. Trends Cancer 10(9), 825–841. https://doi.org/10.1016/j.trecan.2024.06.005 (2024).
Patchell, R. A. et al. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: A randomised trial. Lancet 366(9486), 643–648 (2005).
Finkelstein, J. A. et al. A population-based study of surgery for spinal metastases. J. Bone Jt. Surg. 85, 1045–1050 (2003).
Williams, D.M., Thirukumaran, C.P., Oses, J. et al. Complications and mortality rates following surgical management of extradural spine tumors in New York State. Spine (Phila Pa 1976) 45, 474–482 (2020)
George, R. et al. Interventions for the treatment of metastatic extradural spinal cord compression in adults. Cochrane Database Syst. Rev. 9, 6716 (2015).
Clarke, M. J. et al. Systematic review of the outcomes of surgical treatment of prostate metastases to the spine. Glob. Spine J. 7(5), 460–468 (2017).
Wänman, J. et al. Predictive value of the spinal instability neoplastic score for survival and ambulatory function after surgery for metastatic spinal cord compression in 110 patients with prostate cancer. Spine 8, 550–558 (2020).
Crnalic, S., Löfvenberg, R., Bergh, A. et al. Predicting survival for surgery of metastatic spinal cord compression in prostate cancer: A new score. Spine (Phila Pa 1976) 37, 2168–2176. https://doi.org/10.1097/BRS.0b013e31826011bc (2012).
Miyoshi, Y. et al. Clinical outcome of surgical management for symptomatic metastatic spinal cord compression from prostate cancer. BMC Urol. 1, 143 (2020).
Ju, D. G. et al. Factors associated with improved outcomes following decompressive surgery for prostate cancer metastatic to the spine. Neurosurgery 73, 657–666. https://doi.org/10.1227/NEU.0000000000000070 (2013).
Huddart, R. A. et al. Spinal cord compression in prostate cancer: Treatment outcome and prognostic factors. Radiother. Oncol. 44(3), 229–236 (1997).
Gao, Z. Y. et al. Prognostic factors for overall survival in patients with spinal metastasis secondary to prostate cancer: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 21, 388 (2020).
Strömqvist, B., Fritzell, P., Hägg, O. et al. Swedish society of spinal surgeons. Swespine: The Swedish spine register: The 2012 report. Eur. Spine J. 22, 953–974 (2013)
Stranne, J. 2023/2024 update of the national prostate cancer guidelines in Sweden. Scand. J. Urol. 59, 210–211 (2024).
Stattin, P. How to improve cancer care by use of guidelines and quality registers. Scand. J. Urol. 12(59), 190–192 (2024).
Van Hemelrijck, M. et al. Cohort profile update: The National Prostate Cancer Register of Sweden and Prostate Cancer Data Base—A refined prostate cancer trajectory. Int. J. Epidemiol. 45, 73–82. https://doi.org/10.1093/ije/dyv305 (2016).
Tomic, K. et al. Capture rate and representativity of The National Prostate Cancer Register of Sweden. Acta Oncol. 54, 158–163. https://doi.org/10.3109/0284186x.2014.939299 (2015).
Morote, J., Aguilar, A., Planas, J. & Trilla, E. Definition of castrate resistant prostate cancer: New insights. Biomedicines. 10(3), 689 (2022).
Candelieri-Surette, D. et al. Development and validation of a tool to identify patients diagnosed with castration-resistant prostate cancer. JCO Clin. Cancer Inform. 7, E2300085 (2023).
Westerberg, M., Ahlberg, M., Orrason, A.W. et al. Assessment of variability in life expectancy in older men by use of a new comorbidity indices. A nationwide population-based study. Scand. J. Urol. 59, 207–209 (2024).
Ludvigsson, J. F. et al. Adaption of the Charlson Comorbidity Index for register-based research in Sweden. Clin. Epidemiol. 13, 21–41 (2021).
Gedeborg, R. et al. An aggregated comorbidity measure based on history of filled drug prescriptions: Development and evaluation in two separate cohorts. Epidemiology 32(4), 607–615 (2021).
Fallara, G. et al. A drug comorbidity index to predict mortality in men with castration resistant prostate cancer. PLoS ONE 16(7), e0255239 (2021).
Westerberg, M. et al. Development and validation of a multi-dimensional diagnosis-based comorbidity index that improves prediction of death in men with prostate cancer: Nationalwide, population-based register study. PLoS ONE 19(1), e0296804 (2024).
Klaff, R. et al. Clinical presentation and predictors of survival related to extent of bone metastasis in 900 prostate cancer patients. Scand. J. Urol. 50(5), 352–359 (2016).
Wan-Yo, L. & Yang, S. Metastatic spinal cord compression (MSCC) treated with palliative decompression: Surgical timing and survival rate. PLoS ONE 12(12), e0190342 (2017).
Nater, A. et al. Predictive factors of survival in a surgical series of metastatic epidural spinal cord compression and complete external validation of 8 multivariate models of survival in a prospective North American multicenter study. Cancer 124, 3536–3550 (2018).
Thysell, E. et al. Gene expression profiles define molecular subtypes of prostate cancer bone metastases with different outcomes and morphology traceable back to the primary tumor. Mol. Oncol. 13(8), 1763–1777 (2019).
Westerberg, M. et al. Target trial emulation using new comorbidity indices provided risk estimates comparable to a randomized trail. J. Clin. Epidemiol. 174, 11504. https://doi.org/10.1016/j.jclinepi.2024.111504 (2024).
Shahait, M., Abu-Hijih, R., Salamat, A. et al. Bone marrow involvement in patients with metastatic castration sensitive prostate cancer. PLoS One 17(7) (2022)
Acknowledgements
We thank all the physicians who made time to enter information into the Swespine register and the National Prostate Cancer Register. This project was made possible by the continuous work of the National Prostate Cancer Register of Sweden (NPCR) steering group: Elin Axén (register holder), Åsa Jellvert (chariman) Johan Styrke (co-chairman), Johan Stranne, Jon Kindblom, Camilla Thellenberg, Andreas Josefsson, Ingrida Verbiené, Hampus Nugin, Stefan Carlsson, Anna Kristiansen, Karin Holmsten, Mats Andén, Thomas Jiborn, Olof Akre, Per Fransson, Eva Johansson, Johan Stranne, Magnus Törnblom, Fredrik Jäderling, Marie Hjälm Eriksson, Lotta Renström Koskela, Jonas Hugosson, Ola Bratt, Erik Thimansson, Elin Trädgårdh, Viktoria Gaspar, Maria Nyberg, Fredrik Sandin, Marie Brus, Gustaf Hedström Anna Hedström, Nina Hageman, Christofer Lagerros, Hans Joelsson, and Gert Malmberg. Methodological support, statistical analysis, and assistance with the conduct of the study were provided by Registry Centre North, Umeå University Hospital, Umeå, Sweden.
Funding
Open access funding provided by Umea University. The study was funded by grants from the Swedish Prostate Cancer Federation, Lion’s Cancer Research Foundation at Umeå University, and through a regional agreement between Umeå University and Region Västerbotten (ALF).
Author information
Authors and Affiliations
Contributions
SC, JW and HN designed the study. CH performed the statistical analysis. JW and MF helped analyze the data. All the authors helped interpret the data. JW and MF drafted the initial manuscript. All authors helped review the manuscript and provided their final approval of the version to be published and agree to be accountable for all aspects of the work. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics
The study was approved by the Swedish Ethical Review Authority (Dnr 2020-03214 and Dnr: 2023-03892-02) and conducted according to the Helsinki declaration. The authors declare that they have no competing interests related to the present study. The study was funded by grants from the Swedish Prostate Cancer Federation, Lion’s Cancer Research Foundation at Umeå University, and through a regional agreement between Umeå University and Region Västerbotten (ALF).
Consent statement
Due to the retrospective nature of the study, the Swedish Ethical Review Authority waived the need of obtaining informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wänman, J., Farhang, M., Nyström, H. et al. Survival after spinal surgery for metastases in men with castration-sensitive vs castration-resistant prostate cancer: a nationwide register-based study. Sci Rep 16, 887 (2026). https://doi.org/10.1038/s41598-025-34335-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-34335-2