Abstract
Pyogenic granuloma (PG) is benign vascular lesions of the skin and mucous membranes that often involve the skin and mucous membranes, which often trouble patients due to its frequent bleeding. The traditional treatment is surgical removal, but its bleeding, pain, and trauma have led doctors to look for more minimally invasive methods. Between June 1, 2022 to March 1, 2024, we retrospectively analyzed 72 children with PG who were seen and treated in our department for long pulsed 1064 nm Nd: YAG laser (Gentle Nd: YAG laser) and sclerotherapy, respectively. The efficacy of the two treatments, pain scores, duration of surgery, and adverse events were assessed. The results showed no significant difference between the two groups in the efficacy of first treatment and the efficacy of secondary treatment. Although the procedure time was shorter in Gentle Nd: YAG laser group than in sclerotherapy group, the pain was more pronounced and the incidence of scarring was higher. No significant recurrence was detected in either group during the 6-month follow-up period. Gentle Nd: YAG laser and sclerotherapy for PG are sensitive, less invasive, and safe treatments. Sclerotherapy may be more acceptable to patients than Gentle Nd: YAG laser therapy because it is less painful and scarring is rare.
Similar content being viewed by others
Introduction
Pyogenic granuloma (PG) is a benign vascular lesion commonly found in the skin and mucous membranes and is an acquired and frequent fibrovascular proliferation1,2. PG can occur at all ages and is more common in children. Although the pathogenesis of PG is unknown, it is thought to be a reactive lesion induced by a variety of stimuli, including trauma, chronic mild stimuli, and hormonal3. Because of its susceptibility to recurrent bleeding, even the smallest trauma often bothers patients and their families.
Some of the common treatments used today are surgical excision, cryosurgery, electric cauterisation, sclerotherapy injections and various lasers4. Surgical excision is difficult for many people to accept due to its trauma and scar5,6. Cryosurgery and electric cauterisation are not used much nowadays due to recurrence rates and scarring7,8,9,10. As the concept of minimally invasive is gaining popularity, doctors are constantly looking for treatments with less trauma and shallower scarring. Some studies suggest that laser and sclerotherapy have advantages over traditional surgery by being less invasive11,12. The Nd: YAG laser uses 1% Nd-doped yttrium aluminum garnet crystals as an active medium, emitting light at 1064 nm, and its affinity for hemoglobin leads to an endothelial thermal effect. It effectively penetrates tissue to a depth of 4–7 mm, making it suitable for vascular mucosal lesions13. Polydocanol is a commonly used sclerosant, generally a tissue irritant, which when injected into or near blood vessels can lead to vascular thrombosis and permanent damage to endothelial vessels, resulting in endofibrosis and vascular occlusion14,15. Although more studies have concluded that Gentle Nd: YAG laser and sclerotherapy for pyogenic granuloma are highly effective12,16,17,18,19,20, none of them have examined the two in direct comparison. We conducted the present study with the aim of evaluating the efficacy and adverse effects of a long pulse width Gentle Nd: YAG laser versus polyphenol sclerosis in the treatment of PGs, in order to help clinical selection of more rational treatment.
Methods
This study was conducted under the auspices of our Department of Plastic and Reconstructive Surgery, in accordance with the principles of the Declaration of Helsinki, and was approved by the Institutional Review Board. Written consent was obtained from the parents of the children for all acts of treatment. All authors declare that the legal guardians of all subjects gave informed consent for the publication of identifying information/images in open access online publications. All authors acknowledge the content of the submitted manuscript and guarantee the accuracy and completeness of the data.
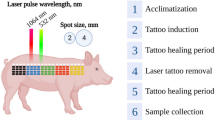
This is a retrospective cohort study. From June 1, 2022 to March 1, 2024 in our plastic surgery clinic, Patients with pyogenic granulomas diagnosed by experienced specialists in our plastic surgery clinic, and divided into two groups based on the specialists’ expertise and clinical experience, who received either Gentle Nd: YAG laser treatment or polydocanol sclerotherapy, respectively. During this period, a total of 81 children with pyogenic granuloma were seen in the outpatient clinic.
We included individuals aged between 0 and 18 years, of both genders, with lesions of any size, who were clinically diagnosed with pyogenic granuloma. Written informed consent was obtained from the parents of the children for all consultations. Children with comorbid coagulopathies, sensitization to sclerosing agents, and previous use of any other treatment modality were excluded. Other exclusion criteria were those with keloid scarring. Ultimately, a total of 72 subjects were enrolled in this study, including 41 in Gentle Nd: YAG laser group and 31 in sclerotherapy group.
A treatment consent form was signed prior to treatment, photographed and saved, and the efficacy was assessed at each follow-up visit. Before treatment, the compound lidocaine cream (Tongfang Pharmaceutical Group Co., Ltd.) was used as local anesthesia. After half an hour, wipe off the lidocaine ointment, disinfect the wound with iodophor, and leave it to dry. Treatment operations are performed by 3 experienced senior attending physicians.
Gentle Nd: YAG laser group was made up of 41 patients treated using Gentle Nd: YAG laser(The Syneron Candela, USA). The pulse duration is adjusted at 30–40 ms, energy density 180–220 J/cm2, and treatment can be performed using a handle with a therapy spot diameter of 3 mm. During the treatment, the operator and the child’s parents wore protective goggles and covered the child’s eyes with an eye mask. The endpoint of the treatment was the atrophy of the lesion in grayish-white or dark purple color, and after the treatment, the patient was given a cold spray to reduce the temperature for 10–15 min to prevent postoperative thermal skin injury.
Sclerotherapy was performed with 1% polydocanol injection (Amplex, Hameln Pharmaceuticals GmbH). Surgical Procedures: Disinfect the working area with iodophor and leave to dry. The original 1% polydocanol injection was drawn with a 1 ml syringe and slowly injected into the tumor at single or multiple points through a 26G injection needle until the tumor turned white or dark purple. Depending on the size of the lesion, the injection dose was 0.1–0.5 ml (average dose: 0.15 ml), and the tumor was compressed with sterile gauze for 2 min after the injection procedure.
Patients in both groups avoided contact with water or scratching for 1 week after the procedure to avoid affecting skin healing. Light radiation such as sunlight was avoided as much as possible to prevent hyperpigmentation from occurring until 4 weeks after the review. On review, treatment was continued if the tumor failed to completely subside until the lesion dried, necrotic, and subsided. Wound healing and the occurrence of adverse events were assessed and recorded at monthly follow-up visits until 6 months after treatment.
The criteria for determining the efficacy of the treatment were as follows: Cure: the tumor eliminates 81–100%, and the skin surface disease returns to normal. Effective: the tumor is eliminated by 21–80%, the volume is significantly reduced, but there is still tumor residue on the skin surface. Ineffective: 0–20% of the tumor is eliminated, and large tumor remains on the skin surface. Overall effective rate = (cured + effective)/total cases.
Children in both groups were given local anesthesia with lidocaine cream for half an hour before treatment. Intraoperative, 5-minute postoperative, 10-minute postoperative, and 15-minute postoperative pain levels were assessed by a surgeon, an assistant surgeon, and a nurse on the basis of the FLACC rating scale (see Appendix).
Other safety indicators include treatment duration, scar, postoperative bleeding, hyperpigmentation, tumor rupture, infection, ocular injury, ectopic embolism, and systemic side effects.
Normality testing was done by Kolmogorov-Smirnov/Shapiro-Wilk test, and Levene’s method was used to verify variance alignment. The independent samples t-test is used for between-group comparisons of normally distributed continuous variables, including age, tumor diameter, treatment duration. Comparisons of nonparametric data such as FLACC scores were made using the Mann-Whitney U test and the Wilcoxon paired signed rank test. Chi-square test or Fisher precision test were used to compare variables with disordered disaggregated data, such as gender, site of lesions, tumor bleeding, combined port wine stains, scar, postoperative bleeding, hyperpigmentation, tumor rupture, infection. The efficacy of the two treatments was compared between variables with sorted information using Chi-square test and Fisher precision test. Statistical analysis was performed using SPSS (version 24.0, IBM INC, Illinois, USA).
Results
Based on the inclusion and exclusion criteria, 71 children were finally included in this study, including 41 in Gentle Nd: YAG laser group and 31 in sclerotherapy group. All participants completed at least two treatments and 6 months of follow-up.
Our study population consisted of 34 males and 38 females. The overall mean (± standard deviation) age was 6.39 ± 0.38 years. The mean (± standard deviation) longest diameter of the lesion was 6.01 ± 0.21 mm. The sites where tumors often accumulated were the face in 31 cases, the head in 10 cases, the neck in 12 cases, the trunk in 8 cases, and the limbs in 11 cases.27 children came to the clinic because of bleeding, and 45 children came to the outpatient clinic because of a red skin mass. One patient in each of the two groups had combined nevus of bright red nevus. The baseline characteristics summarized in Table 1 baseline characteristics were balanced between the two groups.
In terms of efficacy indicators, after one treatment, the cure rate was 53.7% with an effective rate of 95.2% in Gentle Nd: YAG laser group and 61.3% with an effective rate of 93.8% in sclerotherapy group. However, the difference in total effectiveness between the two groups was not statistically significant (p > 0.05). Two groups of patients who were cured after one treatment are listed below, respectively (Figs. 1 and 2).
After two treatments, the cure rate was 78.0% in Gentle Nd: YAG laser group and 83.9% in sclerotherapy group. Meanwhile, the total effective rate of the two groups was 100%, the difference was not statistically significant (P > 0.05). And, no recurrence occurred during the 6-month follow-up period. The efficacy of the two groups is included in Table 2.
In terms of initial treatment pain scores, intraoperative and 10-minute postoperative FLACC scores were higher in Gentle Nd: YAG laser group than in sclerotherapy group. The difference was statistically significant. In contrast, there was no statistically significant difference in FLACC scores between the 20-minute postoperative and 30-minute postoperative periods in Gentle Nd: YAG laser group. FLACC pain scores for both groups of cases are included in Table 3.
We also found that the intraoperative pain was the most intense in both Gentle Nd: YAG laser group and sclerotherapy group, and that the pain tended to decrease gradually with the prolongation of the postoperative period, and the pain basically disappeared by 30 min after the operation. Figure 3 shows the change curve of FLACC scores of children in the two groups.
As for some safety indicators, we found that the treatment duration was shorter in Gentle Nd: YAG laser group than in sclerotherapy group, and the difference was statistically significant (P < 0.001). Gentle Nd: YAG laser group developed more scars than sclerotherapy group and the difference was statistically significant. Adverse reactions during follow-up included hyperpigmentation, infection, bleeding, and tumor rupture, but there was no significant difference between the two groups. We didn’t find ocular injury, ectopic embolism and systemic side effects during the follow-up period. Safety indicators are listed in Table 4.
Discussion
Pyogenic granuloma (PG)—also known as lobular capillar hemangioma or granuloma teleangiectaticum—is a relatively common vascular proliferation of the skin and mucous membranes21. The skin of the head, face, and distal extremities is the most common. Although the exact pathogenic mechanism of PG is not fully understood, it has been associated with pregnancy, trauma, and immunosuppression21,22.
PG, as a common condition, is treated in a variety of ways. Traditional methods include cryotherapy, microwave, radiofrequency, electrocautery, and surgery. Pharmacologic treatments include imiquimod, pharmacotherapy-beta-blockers, sclerotherapy, and glucocorticoids. There are also laser treatments such as CO2, PDL, Nd: YAG, erbium laser, semiconductor laser, KTP laser, etc.23. But the quest of doctors has always been to find treatments that are safe, minimally invasive, and have a quick recovery.
Laser treatment of pyogenic granuloma is based on the principle of selective photothermal action. Hemoglobin reaches peak heat recovery at 2 wavelengths, 595 nm and 1064 nm, which can cause denaturation and coagulation of hemoglobin in the diseased blood vessels and rapid diffusion of heat in the blood vessels, leading to microvascular damage24. Although pulsed dye lasers at a wavelength of 595 nm have previously been shown to be effective in the treatment of pyogenic granulomas25,26, the depth of penetration of the dye laser is limited, and it is not effective in treating larger tumors11. Sud A R also suggests that PGs up to 5 mm in diameter can be used directly with PDL, and PGs over 5 mm in diameter are recommended to be culled at the base of the PDL irradiation first27. The depth of penetration of Gentle Nd: YAG laser used in our study is deep, and its higher absorption in hemoglobin makes this type of laser highly effective in treating deeper pyogenic granulomas11. Our study found that Gentle Nd: YAG laser laser was 95.2% effective with one treatment and 100% effective with two treatments, which is very effective and coincides with the study by Hammes S and Bourguignon R11,28.
Sclerotherapy injections have been used for more than a decade to treat pyogenic granulomas, which involves injecting a chemical into a blood vessel that causes endothelial damage, thrombosis, and vascular fibrosis, leading to lesion destruction29. Commonly used sclerosing agents include bleomycin, glucocorticoids, and polydocanol, as well as monoethanolamine oleate30 and sodium tetradecyl sulfate31,32. Multiple studies conclude that polydocanol injections are effective in the treatment of pyogenic granulomas16,33,34,35. However, none of them directly compared Gentle Nd: YAG laser with polydocanol sclerotherapy. Our current study found that sclerotherapy was effective in all children after two sessions, but did not show a significant difference in efficacy from Gentle Nd: YAG laser.
In terms of pain perception, in our study, there was a statistical difference in FLACC between the operation and 10 min after the operation. However, we also found that the FLACC in 20 min after the operation was very close to 0.05 at the statistical value P. We could not say for sure that there was a difference in pain perception between the two groups at 20 min after the operation, because this study did not carry out random assignment and blind setting. A certain number of children in our study felt pain, even though they were given topical lidocaine cream for half an hour before surgery. Our study population was children, and children undergoing traditional surgical resection generally require general anesthesia, which increases the risk of anesthesia and the financial burden on the child. Laser and sclerotherapy procedures are shorter and can be performed under local anesthesia. We also found that Gentle Nd: YAG laser treatment was more painful than sclerotherapy, even though the procedure duration of the laser was shorter than that of sclerotherapy, probably because of differences in the type of trauma. Laser induces tissue necrosis, leading to the release of pro-inflammatory cytokines such as tumor necrosis factor (TNF)-a, which plays a key role in mediating inflammation36. Some short-wavelength lasers such as diode lasers 810, 940 and 980 nm disperse the epithelium and can penetrate 2–6 mm into tissue. The risk of deeper penetration can cause thermal damage which can lead to pain sensation17. Despite the synchronous cooling device, the pulse is still painful due to the deep penetration of Gentle Nd: YAG laser37. However, polydocanol is supposed to be an anesthetic agent10,38, subcutaneous injection can produce temporary local numbness39. At the same time we can reduce pain by slowing down the rate of injection, polydocanol concentration and volume to reduce pain40. Therefore, polydocanol as a sclerosing agent for the treatment of PG shows more advantages than other sclerosing agents. Our study also found that 10 min after the procedure, pain became minimized in both groups of children, which also made it easier for the children or parents to accept sclerotherapy.
Our study found that no scarring occurred in sclerotherapy group, whereas in Gentle Nd: YAG laser treatment group, scarring occurred in 17.1% of patients. Dong Li et al. conducted experiments on the backs of hamsters, pulsed laser irradiation and applied to hemoglobin, when the temperature exceeds 70℃, instant thermocoagulation is formed41. Heger et al. showed that thrombus formation was triggered after thermocoagulation, and the lesion size reached its peak in 6.25 min after irradiation42. Persistent local heat may cause thermal damage to the dermis leading to scarring. Dong’s reported 21 cases of PG of the digits and toes, applying multifocal Nd: YAG laser treatment, after one to two treatments, all lesions were cleared, and 23.81% of the patients developed minor scarring, but none of them affected the aesthetics and function12. In a case report by Kocaman et al.43, the use of Nd: YAG laser in the treatment of pyogenic granuloma resulted in a shortened operative time, rapid postoperative hemostasis, no scarring and discomfort. Thomas Ples Spradley believes that it has high energy and strong penetrating power, which can effectively seal the blood vessels to achieve the therapeutic purpose, but there is the possibility of post-inflammatory chromatic deposition and scarring, so the clinical treatment should be based on the patient’s individual differences and lesion characteristics of the selection of the appropriate treatment method and to inform the patient of the risk of treatment in advance44. There are many studies of sclerotherapy for vascular lesions, and they all agree that it rarely leads to scarring3,45,46. Ananta Khurana concluded that polydocanol sclerotherapy is an efficient, safe and cost-effective sclerosing agent. However, Hong SK’s study found that when sclerosing agents are used under high pressure, they may damage peripheral nerves or cause skin necrosis, resulting in scarring and aesthetic problems46. It also serves as a wake-up call to the need to be gentle and slow during the operation to minimize the possibility of skin breakdown and scarring.
Bleeding from ruptured tumors after treatment occurred in three children in group Gentle Nd: YAG laser, all of which stopped bleeding after a few minutes of compression, and Hammes S also found that bleeding was rare11. The advantages of the Nd: YAG pulsed laser, such as low thermal damage, good internal homeostasis and antimicrobial effect, and deeper tissue penetration, make it suitable for PG treatment, as it prevents hemorrhage and possible secondary infection47. In our study, the commonly used energy is 200–220 J/cm2, the spot is 3 mm, and the pulse width is 30-40ms. We found that treatments within this energy range can achieve better vascular closure and hemostasis. Bleeding of the tumor after treatment may be caused by the accumulation of pulsed energy over a number of repetitions. Patients in sclerotherapy group exhibited mild or no bleeding, which is consistent with the findings of several studies32,48. Due to the damage to the vascular endothelium caused by sclerosing agents, localized thrombi can form and attach to the vessel wall, ultimately leading to vascular fibrosis and occlusion30,32,48. One study attributed bleeding to the large size of selected lesions49. The largest diameter of the tumor in our study was only 12 mm, which may be related to the importance that parents nowadays attach to their children’s condition.
Limitations
There are also shortcomings in our study. Random allocation and blind method are not carried out, and the grading criteria of efficacy are not mature enough, which is biased. The insufficient number of cases may lead to inconclusive study results and prevent us from obtaining more data on adverse effects. In addition, 6 months of follow-up is not sufficient for us to obtain additional data to evaluate tumor recurrence, pigmentation abnormalities, and scar hyperplasia, and we look forward to a prospective randomized controlled study with more cases and follow-up longer than 2 years.
Conclusions
In this study, Gentle Nd: YAG laser and sclerotherapy were found to be safe and effective in the treatment of PG. While the efficacy is similar, the choice of treatment may vary depending on the patient’s tolerance for pain and scarring risk. From the results of the study, sclerotherapy appears to reflect an advantage and may be a better treatment option. Due to some bias in this study, further prospective studies are needed to validate these conclusions to find the best treatment for suppurative granuloma.
Data availability
The data that support the findings of this study are available from the corresponding author, upon reasonable request.
References
Mahjoub, A. et al. Pyogenic granuloma: clinical, etiological and therapeutic features. A series of five cases. J. Fr. Ophtalmol. 46, e230–e233. https://doi.org/10.1016/j.jfo.2023.01.037 (2023).
Massa, A., Antunes, A. & Varela, P. Pyogenic granuloma in a patient on gefitinib. Acta Med. Port. 29, 569. https://doi.org/10.20344/amp.6343 (2016).
Anwar, S. K., Edward, S. N. & Elsayed, N. M. Diode laser versus sclerotherapy: bloodless approaches in the treatment of oral pyogenic granuloma (randomised controlled clinical trial). Odontology 111, 511–521. https://doi.org/10.1007/s10266-022-00759-9 (2022).
Patra, A. C. et al. Effectiveness and safety of 0.5% timolol solution in the treatment of pyogenic granuloma: a randomized, double-blind and placebo-controlled study. Indian J. Dermatol. Venereol. Leprol. 88, 500–508. https://doi.org/10.25259/ijdvl_565_20 (2022).
Tsunoda, N. et al. Analysis of effects and indications of cryosurgery for oral mucoceles. J. Stomatol. Oral Maxillofac. Surg. 122, 267–272. https://doi.org/10.7537/marsjas120816.01 (2021).
Jafarzadeh, H., Sanatkhani, M. & Mohtasham, N. Oral pyogenic granuloma: a review. J. Oral Sci. 48, 167–175. https://doi.org/10.2334/josnusd.48.167 (2006).
Patrice, S. J., Wiss, K. & Mulliken, J. B. Pyogenic granuloma (lobular capillary hemangioma): a clinicopathologic study of 178 cases. Pediatr. Dermatol. 8, 267–276. https://doi.org/10.1111/j.1525-1470.1991.tb00931.x (1991).
Giblin, A. V., Clover, A. J., Athanassopoulos, A. & Budny, P. G. Pyogenic granuloma—the quest for optimum treatment: audit of treatment of 408 cases. J. Plast. Reconstr. Aesthetic Surg. JPRAS 60, 1030–1035. https://doi.org/10.1016/j.bjps.2006.10.018 (2007).
Daif, E. T. Correlation of age, sex, and location with recurrence of oral giant pyogenic granuloma after surgical excision. J. Craniofac. Surg. 27, e433–e435. https://doi.org/10.1097/scs.0000000000002711 (2016).
Reddy, G. S., Reddy, G. V., Reddy, K. S., Priyadarshini, B. S. & Sree, P. K. Intralesional sclerotherapy—a novel approach for the treatment of intraoral haemangiomas. J. Clin. Diagn. Research: JCDR 10, Zd13–14. https://doi.org/10.7860/jcdr/2016/17568.7137 (2016).
Hammes, S. et al. Pyogenic granuloma: treatment with the 1,064-nm long-pulsed neodymium-doped yttrium aluminum garnet laser in 20 patients. Dermatol. Surg. 38, 918–923. https://doi.org/10.1111/j.1524-4725.2012.02344.x (2012).
Dong, J. et al. Efficacy of Nd-YAG laser for treatment of pyogenic granuloma on the fingers and toes. Lasers Med. Sci. 34, 41–45. https://doi.org/10.1007/s10103-018-2577-7 (2019).
Armogida, N. G. et al. Dye laser to treat an arteriovenous malformation of the tongue: 40-month follow-up. Case Rep. Dentistry 2023, 5583749. https://doi.org/10.1155/2023/5583749 (2023).
Croffie, J. et al. Sclerosing agents for use in GI endoscopy. Gastrointest. Endosc. 66, 1–6. https://doi.org/10.1016/j.gie.2007.02.014 (2007).
Deshpande, A. J. & Dubey, V. C. 3% polidocanol sclerotherapy for pyogenic granuloma: efficacy and safety analysis. J. Cutan. Aesthetic Surg. 15, 284–287. https://doi.org/10.4103/jcas.Jcas_119_21 (2022).
Soni, A. G. Sclerotherapy—a novel modality in the management of oral pyogenic granuloma. J. Indian Soc. Periodontol. 25, 162–165. https://doi.org/10.4103/jisp.jisp_189_20 (2021).
Anwar, S. K., Edward, S. N. & NM, E. L. Diode laser versus sclerotherapy: bloodless approaches in the treatment of oral pyogenic granuloma (randomised controlled clinical trial). Odontology 111, 511–521. https://doi.org/10.1007/s10266-022-00759-9 (2023).
Shivhare, P. et al. Comparative evaluation of efficacy and safety of the Diode laser (980 nm) and sclerotherapy for the treatment of oral pyogenic Granuloma. Int. J. Dent. 2022, 8269221. https://doi.org/10.1155/2022/8269221 (2022).
Sharma, S., Shah, J. S., Asrani, V. K. & Verma, A. The sclerotherapy—an efficacious approach in the management of vascular lesions and pyogenic granuloma: case series with literature review. Indian J. Otolaryngol. Head Neck Surg. 73, 167–173. https://doi.org/10.1007/s12070-020-01960-4 (2021).
Zeng, H., Yang, R. & Ding, Y. Use of a water-cooled nd: YAG pulsed laser in the treatment of giant gingival pyogenic granulomas during pregnancy. J. Stomatol. Oral Maxillofac. Surg. 121, 305–307. https://doi.org/10.1016/j.jormas.2019.05.006 (2020).
Park, S. H., Lee, J. H., Tak, M. S., Lee, H. J. & Choi, H. J. A research of pyogenic granuloma genesis factor with immunohistochemical analysis. J. Craniofac. Surg. 28, 2068–2072. https://doi.org/10.1097/scs.0000000000004148 (2017).
Delbrouck, C., Chamiec, M., Hassid, S. & Ghanooni, R. Lobular capillary haemangioma of the nasal cavity during pregnancy. J. Laryngol. Otol. 125, 973–977. https://doi.org/10.1017/s0022215111001654 (2011).
Plachouri, K. M. & Georgiou, S. Therapeutic approaches to pyogenic granuloma: an updated review. Int. J. Dermatol. 58, 642–648. https://doi.org/10.1111/ijd.14268 (2019).
Srinivas, C. R. & Kumaresan, M. Lasers for vascular lesions: standard guidelines of care. Indian J. Dermatol. Venereol. Leprol. 77, 349–368. https://doi.org/10.4103/0378-6323.79728 (2011).
Wu, J. P. et al. Treatment of pyogenic granuloma in children with a 595 nm pulsed dye laser: a retrospective study of 212 patients. Lasers Surg. Med. 54, 835–840. https://doi.org/10.1002/lsm.23545 (2022).
Kishi, Y. et al. Dye laser treatment for hemorrhagic vascular lesions. Laser Therapy 27, 61–64. https://doi.org/10.5978/islsm.18-CR-01 (2018).
Sud, A. R. & Tan, S. T. Pyogenic granuloma-treatment by shave-excision and/or pulsed-dye laser. J. Plast. Reconstr. Aesthetic Surgery: JPRAS 63, 1364–1368. https://doi.org/10.1016/j.bjps.2009.06.031 (2010).
Bourguignon, R., Paquet, P., Piérard-Franchimont, C. & Piérard, G. E. Treatment of pyogenic granulomas with the Nd-YAG laser. J. Dermatolog. Treat. 17, 247–249. https://doi.org/10.1080/09546630600823344 (2006).
Gurgacz, S., Zamora, L. & Scott, N. A. Percutaneous sclerotherapy for vascular malformations: a systematic review. Ann. Vasc. Surg. 28, 1335–1349. https://doi.org/10.1016/j.avsg.2014.01.008 (2014).
Matsumoto, K. et al. Treatment of pyogenic granuloma with a sclerosing agent. Dermatol. Surg. 27, 521–523. https://doi.org/10.1046/j.1524-4725.2001.01039.x (2001).
Samatha, Y., Reddy, T. H., Jyothirrmai, Ravikiran, A. & Sankar, A. J. Management of oral pyogenic granuloma with sodium tetra decyl sulphate. A case series. N. Y. State Dent. J. 79, 55–57 (2013).
Deore, G. D. et al. Sclerotherapy: a novel bloodless approach to treat recurrent oral pyogenic granuloma associated with port-wine stain. Ann. Vasc. Surg. 28(1), 1514–1569. https://doi.org/10.1016/j.avsg.2014.01.009 (2014).
Khurana, A. & Mathachan, S. R. Polidocanol sclerotherapy in pyogenic granulomas. Dermatol. Surg. 48, 72–75, (2022). https://doi.org/10.1097/dss.0000000000003308
Carvalho, R. A. (ed Neto, V.) Letter: Polidocanol sclerotherapy for the treatment of pyogenic granuloma. Dermatol. Surg. 36 Suppl 2 1068–1070 https://doi.org/10.1111/j.1524-4725.2009.01470.x (2010).
Li, J., Wu, C., Song, D., Wang, L. & Guo, L. Polidocanol sclerotherapy for the treatment of pyogenic granuloma in children. Dermatol. Surg. 47, 802–804. https://doi.org/10.1097/dss.0000000000002967 (2021).
Grellner, W. Time-dependent immunohistochemical detection of proinflammatory cytokines (IL-1beta, IL-6, TNF-alpha) in human skin wounds. Forensic Sci. Int. 130, 90–96. https://doi.org/10.1016/s0379-0738(02)00342-0 (2002).
Spradley, T. P., Johnson, A. B., Wright, H. D., Kincannon, J. M. & Richter, G. T. Modified ND:YAG laser therapy in the treatment of cutaneous venous malformations. Facial Plast. Surg. Aesthetic Med. 23, 289–293. https://doi.org/10.1089/fpsam.2020.0268 (2020).
Lungren, M. P. & Patel, M. N. Endovascular management of head and neck vascular malformations. Curr. Otorhinolaryngol. Rep. 2, 273–284. https://doi.org/10.1007/s40136-014-0053-x (2014).
Hou, F. et al. Percutaneous sclerotherapy with polidocanol under the guidance of ultrasound for venous malformations in children—a retrospective cohort study from a single tertiary medical center. Medicine 99, e18839. https://doi.org/10.1097/md.0000000000018839 (2020).
Da Silva Barros, C. C., Campos, C. M., de Morais Medeiros, H. C. & Queiroz, L. M. G. & Da Silveira É, J. D. evaluation of sclerotherapy of benign oral vascular lesions with monoethanolamine oleate. Clin. Oral Invest. 25, 1767–1774. https://doi.org/10.1007/s00784-020-03479-y (2021).
Li, D. et al. Thermal coagulum formation and hemostasis during repeated multipulse nd:YAG laser treatment of cutaneous vascular lesions: animal experiment study. Lasers Med. Sci. 35, 1589–1597. https://doi.org/10.1007/s10103-020-03007-0 (2020).
Heger, M. et al. Laser-induced primary and secondary hemostasis dynamics and mechanisms in relation to selective photothermolysis of port wine stains. J. Dermatol. Sci. 63, 139–147. https://doi.org/10.1016/j.jdermsci.2011.04.015 (2011).
Kocaman, G. et al. The use of surgical nd:YAG laser in an oral pyogenic granuloma: a case report. J. Cosmet. Laser Therapy 16, 197–200. https://doi.org/10.3109/14764172.2014.910078 (2014).
Spradley, T. P., Johnson, A. B., Wright, H. D., Kincannon, J. M. & Richter, G. T. Gentle ND:YAG Laser Therapy in the treatment of cutaneous venous malformations. Facial Plast. Surg. Aesthet. Med. 23, 289–293. https://doi.org/10.1089/fpsam.2020.0268 (2021).
Fernandes T, D., Elias A, R., Santos-Silva R, A., Vargas A, P. & Lopes A, M. Benign oral vascular lesions treated by sclerotherapy with ethanolamine oleate: a retrospective study of 43 patients. Med. Oral Patol. Oral Cir. Bucal 23, e180–e187. https://doi.org/10.4317/medoral.22253 (2018).
Hong, S. K. et al. Reactive vascular lesions treated using ethanolamine oleate sclerotherapy. Dermatol. Surg. 36, 1148–1152. https://doi.org/10.1111/j.1524-4725.2010.01599.x (2010).
Preeyanont, P. & Nimsakul, N. The nd:YAG laser treatment of hemangioma. J. Clin. Laser Med. Surg. 12, 225–229. https://doi.org/10.1089/clm.1994.12.225 (1994).
Khaitan, T., Sinha, R., Sarkar, S., Ramani, D. & Sharma, M. Conservative approach in the management of oral pyogenic granuloma by sclerotherapy. J. Indian Acad. Oral Med. Radiol. 30, 46. https://doi.org/10.4103/jiaomr.jiaomr_15_18 (2018).
ZaghloolAmer, M., Marzouk, H. A. & Elsharabasy, I. M. J. J. A. Impact of diode laser versus sclerotherapy in treatment of oral pyogenic granuloma. J. Am. Sci. 12, 1–8 (2016).
Acknowledgements
The authors thank all the pyogenic granuloma patients who participated in this study.
Funding
This work was sponsored by Jiangxi Provincial Health Technology Project (Number: 202311001).
Author information
Authors and Affiliations
Contributions
Jun Cheng, Hua Yuan contributed to concept and design, data curation, data analysis, investigation, writing of the original draft, reviewing and editing. Ronghua Fu, Pingliang Jin, Mengyu Huang contributed to data curation, investigation, reviewing and editing.Zhiping Wu, Hanxiang Bai: contributed to acquisition of datas, methodology, software, reviewing and editing. Xiangqun Huang contributed to data curation, investigation, supervision, reviewing and editing. Yun Zou contributed to concept and design, data curation, formal analysis, investigation, supervision, writing of the original draft, reviewing and editing. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was conducted under the auspices of our Department of Plastic and Reconstructive Surgery, in accordance with the principles of the Declaration of Helsinki, and was approved by the Institutional Review Board. Written consent was obtained from the parents of the children for all acts of treatment. All authors acknowledge the content of the submitted manuscript and guarantee the accuracy and completeness of the data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Cheng, J., Yuan, H., Fu, R. et al. Comparison of the efficacy and adverse effects of long pulsed 1064 nm Nd: YAG laser and sclerotherapy in the treatment of pyogenic granuloma in children: a retrospective study. Sci Rep 15, 2843 (2025). https://doi.org/10.1038/s41598-025-85401-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-85401-8