Abstract
OrthoFusion, an intuitive super-resolution algorithm, is presented in this study to enhance the spatial resolution of clinical CT volumes. The efficacy of OrthoFusion is evaluated, relative to high-resolution CT volumes (ground truth), by assessing image volume and derived bone morphological similarity, as well as its performance in specific applications in 2D-3D registration tasks. Results demonstrate that OrthoFusion significantly reduced segmentation time, while improving structural similarity of bone images and relative accuracy of derived bone model geometries. Moreover, it proved beneficial in the context of biplane videoradiography, enhancing the similarity of digitally reconstructed radiographs to radiographic images and improving the accuracy of relative bony kinematics. OrthoFusion’s simplicity, ease of implementation, and generalizability make it a valuable tool for researchers and clinicians seeking high spatial resolution from existing clinical CT data. This study opens new avenues for retrospectively utilizing clinical images for research and advanced clinical purposes, while reducing the need for additional scans, mitigating associated costs and radiation exposure.
Similar content being viewed by others
Introduction
Three-dimensional visualization and creation of bone models are essential for many applications in medical imaging, such as diagnosis of fracture or disease, pre-operative planning, implant design, trainee and patient education, and motion analyses requiring digitally reconstructed radiographs (DRRs). Computed tomography (CT) is a common imaging modality that uses x-rays to produce cross-sectional images of the body, offering detailed volumetric renderings of anatomy and enabling precise examination of internal structures. Although CT is the gold standard for morphologic bone imaging and thus generation of bone models, CT acquisition incurs radiation exposure, cost, and time. Thus, there are concerted efforts across disciplines to reduce radiation exposure to patients to be ‘as low as reasonably achievable’ (ALARA) for the clinical indication. Despite these risks, clinical CT orders are still increasing1.
Clinical CT scans are routinely archived in the patient’s electronic medical records (EMR). Typical clinical scans in EMR are highly anisotropic for a variety of reasons, but primarily driven by methods to reduce both radiation exposure to patients and image file size to account for storage limitations. Imaging protocols export 2 or 3 orthogonal volumes (axial, sagittal, and/or coronal) with high in-plane resolution (e.g., 0.3 × 0.3 mm), but with greater slice thickness and spacing, resulting in a 10-fold courser through-plane resolution (e.g., 3 mm). Unfortunately, high spatial resolution and cortical bone contrast are necessary for visualization of the segmentation process necessary for bone model construction. Therefore, spatial resolution of many CT volumes in EMR is inadequate for multiplanar reconstruction and bone modelling applications.
A method to increase the spatial resolution of clinical CT volumes obtained from EMR would open new opportunities for researchers and clinicians to create multi-planar reconstructions and accurate bone models from the wealth of existing data already stored in EMRs. Super-Resolution is a broad term that refers to a family of techniques to combine multiple low-resolution volumes to produce higher resolution volumes2,3,4. Various super-resolution techniques have been employed to improve medical imaging quality and resolution, including iterative reconstruction2, deconvolution3, deep learning-based approaches5, and registration and fusion6. ‘Registration and fusion’ involves spatially aligning multiple volumes (registration) and combining the information to a single volume that incorporates data from multiple views (fusion). Despite these technological advancements, super-resolution tools in medical imaging are often tailored to a specific research task and are not readily available to researchers or clinicians, requiring advanced programming skills to implement. Additionally, many require large datasets for learning or are not generalizable to other applications.
The objective of this study was to design, implement, and evaluate an intuitive super-resolution algorithm to increase the spatial resolution of low-resolution clinical CT volumes. This effort was motivated by the fact that some participants in our cervical kinematics studies already had recently acquired clinical CT imaging in their EMR. To avoid an additional CT scan and associated radiation exposure, an ethical alternative was desired. Our application requires a subject-specific bone model created from a CT volume to build the DRR for shape-matching via biplane videoradiography. Biplane videoradiography is an advanced imaging technique that captures dynamic radiographs from two views simultaneously so that 3-D bone kinematics can quantified. Our super-resolution solution is generalizable beyond our specific application and will provide an opportunity to other researchers and clinicians to use clinical CTs from EMR to create high-resolution 3-D visualizations and bone models.
Methods
OrthoFusion super-resolution algorithm
The OrthoFusion super-resolution algorithm registers and fuses 2 or 3 orthogonal low-resolution CT volumes to create a single volume with high spatial resolution and is available through the Data Repository for the University of Minnesota (DRUM; link TBD). A graphical representation of the algorithm is provided in Fig. 1, starting from the axial, coronal, and sagittal “Clinical” volumes. First, each low-resolution clinical volume is linearly interpolated to the same high-resolution isotropic grid (0.2 × 0.2 × 0.2 mm) such that an intensity value is assigned to each voxel (registration). Second, the voxel-by-voxel average is computed (fusion). By including multiple orthogonal volumes (axial, coronal, and sagittal), all available information is utilized, capturing features that would otherwise be missed. The generation of a super-resolution volume from the orthogonal volumes takes less than 10 min (including loading DICOMs into MeVisLab, processing, and exporting the SRR volume).
Image acquisition and processing
To evaluate the effectiveness of the OrthoFusion algorithm, we acquired high-resolution CT volumes to serve as the ground truth. CT imaging (B60S; Siemens Biograph PET/CT, Knoxville, USA) of the cervical spine was acquired from 4 participants (3 female/1 male, age 21 to 40 years old) as part of a larger study approved by the University of Minnesota Institutional Review Board. Participants provided informed signed consent and all methods were performed in accordance with all relevant guidelines and regulations. The CT scans were reconstructed into 3 orthogonal high-resolution volumes (axial, sagittal, and coronal), with in-plane resolutions of approximately 0.2 × 0.2 and a through-plane resolution of 0.6 mm.
Image processing
Four CT cases were compared within each participant: (1) high-resolution (HR), (2) clinical (Clin), (3) resliced (RS), and (4) super-resolution (OrthoFusion) volumes. Image processing was performed using custom code in MeVisLab 3.7.2 (MeVisLab Medical Solutions AG). The study design is illustrated in Fig. 2. An axial clinical (Clin) volume with a through-plane resolution of 3 mm was simulated by down-sampling the axial HR volume using Gaussian interpolation. A resampled (RS) volume was created by then up-sampling the axial Clin volume back to 0.6 mm through-plane resolution using Lanczos interpolation, a commonly used technique7. The super-resolution (OrthoFusion) volume was constructed using the OrthoFusion algorithm described above, fusing all 3 orthogonal volumes and resulting in an isotopic resolution of 0.2 mm. The 0.2 mm isotropic resolution was chosen to match the finest in-plane resolution typically achieved by standard CT; however, this value can be adjusted depending on the specific application.
Study design. Four cases were extracted to evaluate the OrthoFusion algorithm – High Resolution (HR), Clinical (Clin), Resliced (RS), and Super Resolution (SR). The axial HR volume was considered the ‘ground truth’. First, HR CT volumes were acquired and reconstructed into 3 orthogonal volumes (axial, coronal, sagittal) with in-plane resolutions of ~ 0.2 × 0.2 mm and a through-plane resolutions of 0.6 mm (top row). Next, Clin volumes were simulated by down-sampling the HR volumes using Gaussian interpolation to a 3 mm through-plane resolution (middle row). The OrthoFusion algorithm (box) was applied, as depicted in Fig. 1. The RS case volume was derived from the axial Clin volume by interpolating back to a 0.6 mm through-plane resolution using Lanczos interpolation.
The biplane videoradiography procedure for measuring intersegmental kinematics and performance measures across the pipeline. To capture the dynamic motion of individual vertebrae, biplane videoradiography is used in conjunction with corresponding bone model(s). This technique uses two synchronized radiographic units to simultaneously capture planar x-ray movies from two perspectives. In parallel, we create subject-specific bone models segmented from a CT scan. The process of shape-matching involves software that simulates a radiographic projection of the bone model – called a digitally reconstructed radiograph or DRR – onto the dynamic radiographic images. An optimization in each frame finds the closest match for the two projections to place and orient the vertebra in 3D space. The OrthoFusion Super Resolution approach was evaluated at each step along this process by quantifying key performance measures.
General Procedure
Bone segmentation
Following image acquisition and processing, subject-specific bone models of the C4 and C5 vertebrae were segmented from each CT case in Mimics (v23, Materialize, Leuven, Belgium) by RA – an experienced segmentation expert. Initial segmentation was performed using a semi-automated CT bone segmentation tool (CT Bone Wizard) that utilizes initial thresholding and a continuity-based algorithm. Additional manual refinement was performed as needed. The segmented CT volumes were then used to create 3-D geometries for morphological comparisons and Digitally Reconstructed Radiographs (DRRs) for kinematic analysis.
Segmentation time
The approximate time and tools (semi-automated vs. manual) required for segmenting each cervical vertebra were recorded for each case.
Image similarity
Image quality assessment was performed comparing each case to the respective HR volume using the structural similarity (SSIM) index and peak signal to noise ratio (PSNR)8. These similarity measures require an identical resolution between comparison images, so the Clin and SR volumes were resampled to the HR volume resolution for these measures. The structural similarity map includes each pixel in the image, based on its relationship to other pixels in a local radius. The measures were calculated on masked CT volumes to isolate the bone, and on the whole CT volumes. The mean and standard deviation of the local SSIM values were compared between cases. The PSNR was computed on the whole volumes.
Morphological similarity
The morphological similarity of the subject specific 3-D bone geometries was assessed using CloudCompare (v2.10). The point-by-point 3-D minimum Euclidean distance between the case geometries and reference HR geometry was computed to determine (1) bias: the mean signed error, (2) precision: the standard deviation of the signed error, and (3) MAE: the mean absolute error. This 3D approach to comparing segmentation results eliminates the need for resolution matching, as required by methods like the DICE and Jaccard indices, and offers an outcome measure directly relevant to our goal of enhancing the spatial resolution of anisotropic volumes.
Application specific procedure
Each of the 4 cases (HR, Clin, RS, and SR) for each of the 4 participants was taken through the following pipeline shown in Fig. 3 for extracting segmental kinematics from biplane videoradiography. Briefly, the process includes simultaneous collection of dynamic radiographs from two views during cervical motion tasks, shape-matching the DRRs to the biplane radiographs, and computing the relative kinematics between the C4 and C5 vertebrae. The error associated with our traditional biplane videoradiography pipeline for the cervical spine kinematics is ≤ 0.49 mm and ≤ 1.80⁰.9 The performance of each case was compared to our traditional high-resolution CT at multiple phases in pipeline.
Biplane Videoradiography
Dynamic radiographs of the cervical spine were acquired using a custom biplane videoradiography system (Imaging Systems & Services, Inc., Painesville, OH, USA) at 30 Hz with approximate imaging parameters of 160 mA, 70 kV, and 0.16 mSv/trial. Each participant performed a 3-second trial of neck flexion-extension, lateral bending, and axial rotation. Post-processing of the radiographic images included undistortion and filtering (DSX Suite, C-Motion Inc., Germantown, MD, USA) and calibration (XMALab, Brown University, RI, USA).
Shape-matching
Shape-matching is the process by which 3-D kinematics are extracted by registering the DRRs (created from the projections of the segmented CT volumes) to the biplane radiographs. The dynamic 3-D positions and orientations of the C4 and C5 vertebrae were resolved using Autoscoper (Brown University, RI, USA), an open-source shape-matching software9,10. Both the DRRs and radiographs are filtered (Gaussian, sobel, etc.) to enhance features and edges. Auto-registration is performed using a particle swarm optimization technique with the inverse of the normalized cross-correlation (NCC) as the cost function. Manual refinement was performed when the optimization algorithm was unable to find an adequate match. The global 3-D kinematics of each bone was exported.
Shape-matching similarity
The match of the DRR to radiographs during the shape-matching process is quantified using the NCC. The NCC is a pixel-by-pixel correlation of the projection of the 3-D DRR to the 2-D radiographs. The inverse of the NCC is used as the optimization criteria for auto-registration by Autoscoper. A lower value for NCC value indicates a better fit. Because the NCC may be affected by radiograph image parameters, the NCC error metric was normalized frame-by-frame by the corresponding HR NCC for each participant and trial.
The mean and standard deviation of the NCC error was computed across all frames of each trial.
Relative kinematics
Relative kinematics between vertebrae were computed using KinematicsToolbox v.4.7.211. Local coordinate systems were created for each vertebra by digitizing anatomic landmarks such that the origin is in the center of the body, x-axis points anterior, and y-axis points left, z-axis points superior12. The rotations and displacements of C4 (relative to C5) were computed for each of the trials, cases, and participants.
Relative kinematics accuracy
The relative kinematics accuracy is represented by two scalar values: the orientation error and position error. The orientation error is the distance between quaternion rotations13 of the case, p, and HR, q, defined as:
The position error was computed as the Euclidean distance between the relative C4-C5 displacements of the case and HR. The mean and variability (standard deviation) of the orientation and position error were computed across each trial.
Statistics
ANOVA was used to determine groupwise differences for each outcome measure, followed by subsequent pairwise comparisons. Normality was assessed and vertebral levels were treated as independent. A one-way repeated measures ANOVA was conducted for measures that are not impacted by trial, i.e., image similarity and bone morphology. A two-way ANOVA was used to examine the effect of both cases and trial for the shape-matching and relative kinematics measures.
Results
The results are reported in Fig. 4, with representative examples in Fig. 5.
Comparisons between the simulated Clinical (Clin), Resliced (RS), and Super Resolution (SR) volumes referenced to the “ground truth” High Resolution (HR) volume in (a) image similarity measures, (b) bone model morphological similarity, (c) shape-matching similarity, and (d) relative kinematics accuracy. Error bars represent standard deviation. Asterisk indicates a significant difference of p < 0.05 between groups. SSIM = Structural Similarity Index Measure, NCC = normalized cross-correlation coefficient.
Image similarity
The SSIM of the masked volumes takes both the internal structure and the segmentation of the bone into account. The mean masked SSIM of the SR volume (0.696 ± 0.024) was statistically greater than the Clin (0.589 ± 0.047; p = 0.001) and RS (0.602 ± 0.037; p = 0.001) volumes. Similarly, the SR volume had significantly less SSIM variability (0.2 ± 0.014) than the Clin (0.313 ± 0.009; p < 0.001) and RS (0.290 ± 0.011; p < 0.001) masked volumes. The RS volume also had less variability than the Clin volume (p = 0.001).
The SSIM of the whole CT volumes represents the structural similarity of the non-segmented CT volumes. The mean SSIM of the whole RS volume (0.766 ± 0.033) was statistically higher than SR (0.747 ± 0.031, p = 0.018) and the Clin volume (0.753 ± 0.031, p < 0.001). The SSIM variability was not statistically different between the cases. The PSNR of the whole volumes were also not statistically different.
Segmentation time
Segmentation of each vertebra was successfully completed with the automated “CT Bone Wizard” tool in Mimics (v23) for the HR and OrthoFusion (SR) volumes with minimal need for manual refinement. This resulted in a segmentation time of approximately 15 min per vertebra. Manual segmentation was required for the Clin and RS vertebrae due to poor distinction between bones (primarily facet joints). This resulted in a segmentation time of approximately 2.5 h per vertebra.
Morphological similarity
Significant differences between cases were found for bias, precision, and MAE distances of the 3-D bone geometry. Bias: The SR bone models (-0.01 ± 0.12 mm) had significantly less bias than the Clin (0.47 ± 0.39 mm; p = 0.017) and RS (-0.24 ± 0.15 mm; p = 0.031) bone models. Precision: The SR (0.38 ± 0.13 mm) bone models were significantly more precise than the RS (0.71 ± 0.19 mm; p = 0.003) or Clin (1.18 ± 0.44 mm; p = 0.005) bone models. MAE: The MAE of the SR bone models (0.29 ± 0.06 mm) were significantly less than the Clin (0.85 ± 0.31 mm; p = 0.002) and RS (0.54 ± 0.12; p = 0.001) bone models.
Shape-matching similarity
The normalized cross-correlation coefficient (NCC) is the measure of pixel-by-pixel similarity of the shape-matched DRR and biplane radiographs. The NCC error is the normalized difference between the case and HR NCC values at each frame of the trial. Within-subjects effects of both trial and case were found to be significant for the normalized NCC error measures. A significant trial effect was observed such that the lateral bending trials had a significantly lower (better matched) mean NCC error than the axial rotation (p = 0.006) and flexion-extension (p = 0.001) trials. A significant case effect was observed such that the mean NCC error for the SR cases (0.106 ± 0.162) were significantly lower than the Clin (0.261 ± 0.119; p = 0.002) and RS (0.194 ± 0.105; p = 0.024) cases. A significant trial effect was observed such that the lateral bending trials had significantly less variability in NCC error than the flexion-extension trials (p = 0.042). A significant case effect was observed such that the NCC error variability for the SR cases (0.060 ± 0.014) was significantly lower than that of the Clin (0.162 ± 0.023; p = 0.002) or RS (0.109 ± 0.010; p = 0.005).
Relative kinematics accuracy
The relative kinematics of the C4 to C5 vertebrae were compared between the HR and cases to determine kinematics accuracy. Significant within-subjects effects of case, but not trial, were found for the kinematics measures. The SR case produced relative kinematics with the least orientation and displacement error. The mean orientation error for the SR case (1.7 ± 1.5 deg) was significantly lower than the Clin (8.0 ± 5.8 deg; p = 0.019) and approaching significance for RS (3.8 ± 2.2 deg; p = 0.053) case. Similarly, the variability of the orientation error for the SR case (1.1 ± 1.2 deg) was significantly lower than the Clin (4.5 ± 2.3 deg; p = 0.004) and approaching significance for RS (3.1 ± 2.4 deg; p = 0.061) case. The mean displacement error for the SR case (0.5 ± 0.2 mm) was significantly lower than that of the Clin (2.5 ± 0.5 mm) and RS (1.2 ± 0.3 mm) cases. The variability of displacement error for the SR case (0.4 ± 0.49 mm) was significantly lower than the Clin (1.4 ± 1.1 mm; p = 0.014) and RS (0.8 ± 0.8 mm; p = 0.026) cases.
Discussion
We designed, implemented, and evaluated OrthoFusion super-resolution technique to increase the spatial resolution of previously acquired low-resolution CT volumes. OrthoFusion significantly improved segmentation time, the structural similarity of the bone images, and the accuracy of bone model geometry. Specific to our biplane videoradiography application, OrthoFusion improved the DRR to radiograph similarity during shape-matching and the accuracy of the relative C4-C5 kinematics. Ultimately, these improvements enable us to use previously acquired clinical CT scans from participant EMR instead of acquiring additional CT imaging as part of our studies, reducing radiation exposure, time, and cost.
Summary Figure. Representative data illustrating the performance measures across the 4 case volumes, with the High Resolution case as the ground truth. Multiplanar Reconstructions emphasize the separation of the facet joints. Segmentation time was substantially less for the High Resolution and Super Resolution cases. Image similarity was improved with the Super Resolution approach, depicted from local SSIM maps where white indicates greater similarity. These improved performances over the Clinical and Resliced volumes yielded a greater morphological similarity and ultimately, for our applications purpose, the Super Resolution Digitally Reconstructed Radiograph (DRR) exhibited better performance for shape-matching similarity and relative kinematics accuracy.
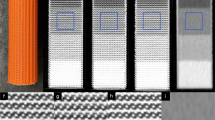
Super-resolution has utility well beyond our specific biplane videoradiography application. OrthoFusion is useful in applications where multiple anisotropic CT volumes are available and high 3-D spatial resolution is important. The abundance of imaging in electronic medical records is an untapped opportunity for retrospective studies that were previously not possible due to poor through-plane resolution. By fusing the CT data in multiple views, applications requiring accurate and high resolution multiplanar reconstruction, segmentation, DRRs, and 3-D geometries become possible. The use of OrthoFusion for other applications, such as improving spatial resolution for bone microarchitecture measures (Fig. 6 – Top Row), will require validation specific to the outcome measures. In cases where hardware or radiation constraints produce a highly anisotropic resolution, OrthoFusion could be a viable solution for prospectively improving spatial resolution (Fig. 6 – Bottom Row). However, its potential to allow for retrospective analysis of previously acquired CT imaging in medical records is the most significant contribution from this work.
Qualitative evaluation of OrthoFusion applications. Top Row: MicroCT images of a mouse tibia. The 3 orthogonal “Clinical” CT volumes had a through-plane resolution of 0.075 mm and in-plane resolution of 0.005 × 0.005 mm. The Clinical images demonstrate representative slices in the plane of lowest spatial resolution, highlighting the loss of architectural detail. The Super Resolution reconstruction recaptures finer structural details, enhancing visualization of the trabecular architecture. Bottom Row: Segmented 3D models of a total knee arthroplasty (TKA) generated using different methods. The Clinical model exhibits significant blocky artifacts, hindering accurate segmentation and anatomical fidelity. The Super Resolution model mitigates these artifacts, producing a smoother and more accurate reconstruction.
To our knowledge, currently available imaging software applications do not provide a tool that increases spatial resolution from multiple low-resolution volumes. Many super-resolution techniques have been reported in the medical imaging literature, often with the goal of exceeding hardware resolution and decreasing noise2 However, these algorithms are complex and challenging to implement for a typical researcher or clinician. Machine learning algorithms offer an alternative approach; however, they require sufficiently large datasets to be effectively trained, which are not always feasible to obtain and often involve manual efforts in imaging preparation or segmentation5,14,15. Morphology morphing algorithms in conjunction with biplane slot scanners offer a low-dose approach to generate bone models, but are limited based on target specific geometries and do not yield a volumetric imaging dataset16. OrthoFusion is an easily implemented technique that is generalizable to any CT imaging target and does not require training. Further development of the OrthoFusion algorithm by integrating filtering and iterative algorithms will provide new possibilities for the use of the large dataset of clinical imaging in EMR.
There are several limitations that should be considered in the interpretation of this study. First, we applied OrthoFusion super-resolution to our specific application with limited scans - the decision to use 4 high-resolution CT scans was based on the exploratory nature of this study, focusing on the initial validation of the OrthoFusion algorithm within the MeVisLab environment. The benefits of improving spatial resolution for bone segmentation are generalizable and have been tested for feasibility in other joints and with two orthogonal volumes, but performance should always be assessed in the context of each specific application. Conducting thorough internal validation ensures the algorithm meets the unique requirements and constraints of new use cases. Second, the processing and analysis involved in our biplane videoradiography pipeline requires significant user interaction and the cases were visibly identifiable, making blinding impossible. Finally, OrthoFusion uses a simple voxel-by-voxel averaging algorithm that creates a blurring effect. The addition of anisotropic filtering17 or a spatial weighted average approach18 are likely to enhance the image quality. These and numerous other enhancements could be implemented in future work, potentially through integration with platforms like 3D Slicer, which would facilitate broader dissemination and accessibility of the software. By incorporating OrthoFusion into such platforms, it could become more widely adopted by the research and clinical communities, allowing for easier application across various use cases.
This study demonstrates the utility of super-resolution to increase the spatial resolution of previously acquired low-resolution CT volumes. The OrthoFusion technique enabled us to use CT imaging from participant EMR for our biplane videoradiography studies, thus reducing exposure to radiation and costs associated with acquiring imaging. This straight-forward technique is easy to implement, generalizable to other applications, and allows researchers and clinicians that require high spatial resolution CT to utilize the abundance of clinical imaging in EMR.
Data availability
The code and datasets analyzed during this study are available in the Data Repository for U of M (https://conservancy.umn.edu/drum: specific link TBD).
References
Smith-Bindman, R. et al. Trends in Use of Medical Imaging in US Health Care systems and in Ontario, Canada, 2000–2016. JAMA 322, 843–856 (2019).
Hakimi, W. E. & Wesarg, S. Accurate super-resolution reconstruction for CT and MR images. in Proceedings of the 26th IEEE International Symposium on Computer-Based Medical Systems 445–448 (2013). https://doi.org/10.1109/CBMS.2013.6627837
Odet, C., Peyrin, F. & Goutte, R. Improved resolution of medical 3-D x-ray computed-tomographic images. in Visual Communications and Image Processing ’90: Fifth in a Series vol. 1360 658–664SPIE, (1990).
Isaac, J. S. & Kulkarni, R. Super resolution techniques for medical image processing. in International Conference on Technologies for Sustainable Development (ICTSD) 1–6 https://doi.org/10.1109/ICTSD.2015.7095900 (2015).
Jiang, C., Zhang, Q., Fan, R. & Hu, Z. Super-resolution CT image Reconstruction based on Dictionary Learning and sparse representation. Sci. Rep. 8, 8799 (2018).
Greenspan, H. Super-resolution in Medical Imaging. Comput. J. 52, 43–63 (2009).
Moraes, T., Amorim, P., Da Silva, J. V. & Pedrini, H. Medical image interpolation based on 3D Lanczos filtering. Comput. Methods Biomech. Biomedical Engineering: Imaging Visualization. 8, 294–300 (2020).
Renieblas, G. P., Nogués, A. T., González, A. M., Gómez-Leon, N. & Del Castillo, E. G. Structural similarity index family for image quality assessment in radiological images. J. Med. Imaging (Bellingham). 4, 035501 (2017).
Miranda, D. L. et al. Static and dynamic error of a Biplanar Videoradiography System using marker-based and Markerless Tracking techniques. J. Biomech. Eng. 133, 121002–121002 (2011).
Akhbari, B., Morton, A. M., Moore, D. C. & Crisco, J. J. Biplanar Videoradiography to study the wrist and distal radioulnar joints. J. Vis. Exp. 10.3791 /62102 (2021).
Rebekah, L. Lawrence. KinematicsToolbox: A Comprehensive Software Program for Analyzing and Visualizing Radiographic Motion Capture Data. (2023). https://doi.org/10.7936/6RXS-103624
Kage, C. C. et al. Validation of an automated shape-matching algorithm for biplane radiographic spine osteokinematics and radiostereometric analysis error quantification. PLOS ONE. 15, e0228594 (2020).
Huynh, D. Q. Metrics for 3D rotations: comparison and analysis. J. Math. Imaging Vis. 35, 155–164 (2009).
Jia, Y., Gholipour, A., He, Z. & Warfield, S. K. A new sparse representation Framework for Reconstruction of an isotropic high spatial resolution MR volume from Orthogonal Anisotropic Resolution scans. IEEE Trans. Med. Imaging. 36, 1182–1193 (2017).
Danker Khoo, J. J., Lim, K. H. & Sien Phang, J. T. A Review on Deep Learning Super Resolution Techniques. in IEEE 8th Conference on Systems, Process and Control (ICSPC) 134–139 (2020). (2020). https://doi.org/10.1109/ICSPC50992.2020.9305806
Dubousset, J. et al. A new 2D and 3D imaging approach to musculoskeletal physiology and pathology with low-dose radiation and the standing position: the EOS system. Bull. Acad. Natl. Med. 189, 287–297 (2005). discussion 297–300.
Kurt, B., Nabiyev, V. V. & Turhan, K. Medical images enhancement by using anisotropic filter and CLAHE. in International Symposium on Innovations in Intelligent Systems and Applications 1–4https://doi.org/10.1109/INISTA.2012.6246971 (2012).
Bätz, M., Eichenseer, A. & Kaup, A. Multi-image super-resolution using a dual weighting scheme based on Voronoi tessellation. in IEEE International Conference on Image Processing (ICIP) 2822–2826 https://doi.org/10.1109/ICIP.2016.7532874 (2016).
Acknowledgements
The authors would like to thank Craig Kage for his assistance with data collection.
Funding
This work was funded by the following NIH grants: R03HD09771, TL1R002493, UL1TR002494, and F32AR082276. Additionally, this work was supported by the Minnesota Partnership for Biotechnology and Medical Genomics (MHP IF #14.02).
Author information
Authors and Affiliations
Contributions
Conceptualization, study design: R.E.A., A.M.E. Methodology: R.E.A., A.N., H.W., R.E.B. Formal analysis: R.E.A., A.N., A.M.E., Writing original draft: R.E.A. Review and editing: all authors. Funding acquisition, project management: A.M.E. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Abbott, R.E., Nishimwe, A., Wiputra, H. et al. A super-resolution algorithm to fuse orthogonal CT volumes using OrthoFusion. Sci Rep 15, 1382 (2025). https://doi.org/10.1038/s41598-025-85516-y
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-85516-y