Abstract
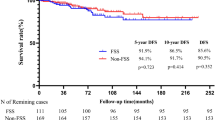
Primary leiomyoma is one of the rarest benign ovarian tumors. Since the first case was identified, less than 100 cases have been reported worldwide. This study aimed to analyze the clinical characteristics and discuss the proper management of this tumor. A review of the patients’ medical records was undertaken from January 2015 to December 2023. A total of 21 cases of primary ovarian leiomyoma and 5 cases of inherent ligament leiomyoma were identified. The mean age was 45.6 years (17–67 years). The tumor size ranged from 1.2 to 7.0 cm (mean, 3.7 cm) by ultrasound. Eighteen (69.2%) patients complained of an asymptomatic pelvic mass. None of them was successfully diagnosed before the surgery. Twelve patients underwent laparoscopic salpingo-oophorectomy or oophorectomy with a mean diameter of 2.9 cm and an average age of 54.2 years. Meanwhile, 12 patients underwent laparoscopic tumorectomy with a mean diameter of 3.0 cm and an average age of 39.3 years. Besides, two patients underwent laparotomic tumorectomy. After a mean follow-up of 35.7 months, patients were alive with no disease recurrence. In conclusion, tumorectomy is preferred for patients with conception requirement or at reproductive age. Laparoscopic surgery is considered as an effective and safe approach.
Similar content being viewed by others
Introduction
Leiomyoma is a kind of benign mesenchymal neoplasms mostly seen in the uterus but rarely in the ovary1,2. Primary ovarian leiomyoma accounts for only 0.5–1% of all benign ovarian tumors1,2. The origin of this tumor remains unresolved. It may arise from smooth muscle cells in the ovarian hilar vessels, ovarian stroma, ovarian ligament, or multipotential cells or undifferentiated germ cells in ovarian stroma, or smooth muscle metaplasia of cortex or endometriotic stroma etc1,3,4,5.
Most of ovarian leiomyomas are asymptomatic, unilateral, small, and occur in middle-aged to postmenopausal women1,2,6. These tumors are usually diagnosed incidentally by routine pelvic examination, ultrasound or postoperative pathological examination6. The differential diagnoses before the operation include broad-ligament fibroid, subserous fibroid in adnexal area, and solid ovarian stromal tumors. The definitive diagnosis is quite difficult prior to surgical removal, as there are no characteristic symptoms or imaging findings7,8.
Since the first case was identified in 1862, less than 100 cases have been reported worldwide, most of which have been described in case reports or small series separately7. Owing to the rarity of this tumor, studies with small sample sizes could not reflect the reality of ovarian leiomyoma. Therefore, in this study, we analyzed the clinical characteristics of patients with the largest number to provide some new information about this tumor, and discussed the proper management strategy to produce a better quality of life after surgery.
Results
During the 9-year study period, a total of 21 cases of primary ovarian leiomyoma and 5 cases of inherent ligament leiomyoma were identified. The mean age was 45.6 years (17–67 years), and 8 (30.8%) patients were postmenopausal. The tumor size ranged from 1.2 to 7.0 cm (mean, 3.7 cm) by ultrasound. Sixteen (61.5%) cases were in the left and 10 (38.5%) in the right. The serum tumor markers were evaluated in 23 (88.5%) patients and a slightly elevated level of cancer antigen 125 (CA125) was observed in one. Basic information of patients with ovarian leiomyoma is shown in Table 1.
Eighteen (69.2%) patients complained of an asymptomatic pelvic mass with a mean duration of 17.2 months (7days–7years), and one (3.8%) presented with irregular menstruation cycle for 3 months. Besides, incidentally intraoperative and postoperative finding of ovarian mass was observed in 4 (15.4%) and 3 (11.5%) cases, respectively.
Ultrasound examination was performed in all patients, reporting 19 (73.1%) cases of solid mass in the adnexal area. Lesions presented as hypoechogenic, well-circumscribed, oval or round in shape, and regular in morphology. No significant blood flow signal was observed in or around the mass in 6 (31.6%) cases, a minimal flow signal was observed in or around the mass in 9 (47.4%) cases, and a slightly rich flow signal was observed in 4 (21.1%) cases.
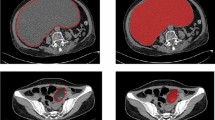
Contrast-enhanced computerized tomography (CT) of the abdominopelvic cavity was performed in 6 (23.1%) patients. Except for 2 cases with incidentally intraoperative and postoperative finding of ovarian mass, CT scan revealed well-circumscribed enhanced lesions in 4 patients, which were initially considered to be subserous uterine fibroid or broad-ligament fibroid.
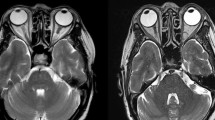
Enhanced pelvic magnetic resonance imaging (MRI) was performed in 4 (15.4%) patients. Lesions presented as well-circumscribed, slightly enhanced mass with low-intensity signals on both T1-weighted and T2-weighted images, which were considered to be fibroma or thecoma.
None of them was successfully diagnosed before the surgery. Twelve (63.2%, 12/19) patients were misdiagnosed as subserous uterine fibroid or broad-ligament fibroid, 6 (31.6%, 6/19) as ovarian sex cord-stromal tumors, and 1 (5.2%, 1/19) as thickened fallopian tube.
Intraoperative frozen section was performed in 10 (43.5%, 10/23) cases. Four (40.0%) patients were diagnosed as ovarian leiomyoma, three (30.0%) were diagnosed as ovarian fibroma, and the other three (30.0%) were diagnosed as ovarian spindle cell tumors. The definitive diagnosis was typical ovarian leiomyoma in all 26 patients. There were no malignant findings, such as significant nuclear atypia, pleomorphism, or necrosis.
Twelve patients underwent laparoscopic salpingo-oophorectomy or oophorectomy with a mean diameter of 2.9 cm (0.5–6.5 cm) and an average age of 54.2 years (39–67 years). Meanwhile, 12 patients underwent laparoscopic excision of ovarian mass with a mean diameter of 3.0 cm (1.0–7.0 cm) and an average age of 39.3 years (28–47 years). Conversions to laparotomy or perioperative complications were not observed. Besides, 2 patients underwent laparotomic tumorectomy, one with total hysterectomy and bilateral salpingectomy because of multiple myomas, the other with contralateral cystectomy because of huge ovarian cyst. All patients had regular menstrual cycle after excision of ovarian mass, except for one who underwent total abdominal hysterectomy and bilateral salpingectomy. Anti-müllerian hormone (AMH) was assayed during spontaneous cycle before and 3 to 6 months after surgery in 3 patients who underwent tumorectomy, and diminished ovarian reserve was not observed. After a mean follow-up of 35.7 months (3–96 months), patients were alive with no disease recurrence. The surgical and histopathological results are shown in Table 2.
In addition, 19 (73.1%) patients underwent surgeries for uterine myomas at the same time, including 15 cases of laparoscopic myomectomy, one case of total abdominal hysterectomy and bilateral salpingectomy, and three cases of laparoscopic total hysterectomy and bilateral salpingectomy or salpingo-oophorectomy.
Discussion
Primary ovarian leiomyoma is an extremely rare form of extrauterine leiomyomas, which is usually asymptomatic, small, and an incidental finding. It has been reported that ovarian leiomyomas are usually less than 3 cm in size9. However, a majority of cases reported had a diameter of more than 5 cm1,7. Liang et al.. shared a case series in 2022, including seven primary ovarian leiomyomas and one inherent ligament leiomyoma with a mean diameter of 7 cm by ultrasound7. In the present study, the mean diameter was 3.7 cm by ultrasound, and only 6 (31.6%) patients had ovarian mass less than 3 cm. Therefore, ovarian leiomyoma may not be as small in size as we previously thought.
Ovarian leiomyoma is usually unilateral with no predilection for the right or left ovary. In a literature review, Liang et al. found that ovarian leiomyoma has a predilection for the right ovary7. However, in current study, 16 (61.5%) lesions were in the left and 10 (38.5%) in the right. Due to the rarity of ovarian leiomyoma, more studies with larger sample sizes are warranted to further evaluate the predilection site.
The symptoms and imaging findings lack specificity; thus, preoperative diagnosis is quite difficult7,8,10,11,12. In our study, all patients had a comprehensive preoperative evaluation, however, none of them was successfully diagnosed before the surgery. About 63.2% of patients were misdiagnosed as subserous uterine fibroid or broad-ligament fibroid.
Frozen section is used to evaluate the nature of tumor and helpful in determining the necessary extent of operation7,8. However, there is no reliable method to intraoperatively differentiate between ovarian leiomyoma and fibroma7,8. Liang et al.. found the accuracy of frozen section for ovarian leiomyoma ranged from 50–62.5%7. In current study, frozen section analysis was performed in 10 (43.5%) cases. However, only 4 (40.0%) were diagnosed properly, three (30.0%) were diagnosed as ovarian fibroma, and the other three (30.0%) as ovarian spindle cell tumors. In general, ovarian leiomyoma and fibroma are mainly composed of spindle-shaped cells. Therefore, rare ovarian leiomyoma is frequently confused with the more common fibroma1. Immunohistochemistry plays an important role in the differential diagnosis of ovarian tumors. The immunohistochemical staining with desmin, inhibin, and α-smooth muscle actin contributes to confirming the histological impression1. In addition, a secondary degeneration, including hyalinization, calcification, edema, and hemorrhage, may increase the diagnostic difficulty1. In our study, degeneration was observed in 2 out of 6 patients without accurate diagnosis by frozen section examination.
Lerwill et al.. reported 22 cases of ovarian leiomyoma in 2004, including 7 typical, 11 cellular, 2 mitotically active, 1 with bizarre nuclei, and 1 myxoid, majority of which were consultation cases1. However, in the studies reported by Liang et al.., Koo et al.., and Doss et al.. with 8, 9, and 15 cases, respectively, there was only one cellular leiomyoma and no malignant findings2,7,8. In our study, except for typical type, other types were not observed. The difference in pathological types might be related with the race and age of patients. In current study, all patients were Ethnicity Han. The mean age was 45.6 years (17–67 years), similar to that reported by Doss et al.., and 8 (30.8%) patients were postmenopausal2. In Lerwill’s study, the patients’ age ranged from 3 to 49 years old, which is much younger than that in this study.
With respect to the solid nature, surgery is advised, even for tumors smaller than 3 cm. Unilateral salpingo-oophorectomy or oophorectomy is a good choice for all ages of women with unilateral ovarian leiomyoma1,2,7,8. However, ovarian-sparing surgery has been reported gradually, and no recurrence has been reported so far7,13,14. Koo et al.. reported among 7 patients under age 40, 2 of them underwent excision of ovarian mass in 2010, while Liang et al.. reported 6 out of 8 patients between 17 and 51 years old had tumorectomy in 20227,8. We presented 14 (53.8%) cases successfully managed with ovarian preservation at an average age of 38.3 years (17-48years), including 12 cases by laparoscopy and 2 cases by laparotomy. After excision of ovarian mass, the ovarian function seemed less affected based on the menstrual cycle and AMH. Therefore, for patients with conception requirement or at reproductive age, conservative surgery should be considered as a first choice to preserve fertility and ovarian function. During the intraoperative period, a high degree of clinical suspicion is helpful to avoid unnecessary oophorectomy and infertility.
The prognosis of ovarian leiomyoma is presumed to be good1,2,7,8,15. After a mean follow-up of 35.7 months, patients were alive with no disease recurrence. In our study, 24 (92.3%) patients underwent laparoscopic surgery. Conversions to laparotomy or perioperative complications were not observed. Similar to ovarian fibromas, ovarian leiomyomas can be treated by laparoscopic surgery effectively and safely13,14,16,17,18,19,20,21,22. Laparoscopy is considered as a minimally invasive and feasible alternative to laparotomy, resulting in reduced postoperative pain, shorter recovery time and a smaller scar.
The patients in study came from one medical center and the number of cases and follow-up were limited. More studies with large sample sizes are needed to better understand primary ovarian leiomyoma.
In conclusion, ovarian leiomyoma is mostly benign and has an excellent prognosis. Tumorectomy is preferred for patients with conception requirement or at reproductive age. Laparoscopic surgery is considered as an effective and safe surgical approach for managing ovarian leiomyomas.
Methods
In the retrospective study, a review was undertaken of the medical records of patients who had primary ovarian leiomyoma after surgery at the Department of Obstetrics and Gynecology of Sir Run Run Shaw Hospital (SRRSH), School of Medicine, Zhejiang University, Hangzhou, China, from January 2015 to December 2023. The hospital ethics committee approved this retrospective study (Approval number: 2024-2298-01). The study was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all patients during a follow-up phone call.
Tumors arising from the broad ligament, or parasitic from the uterus were excluded. Broad ligament myoma is defined as a myoma originating from the broad ligament or lateral uterine wall. Myomectomy and hysterectomy for uterine leiomyoma, especially laparoscopic surgery with unprotected power morcellation, may lead to the dissemination of myoma in the pelvic cavity. Therefore, patients who had aforementioned surgical history were excluded. The definitive diagnosis depends on the histopathology and immunochemical analysis. The immunohistochemical staining with α-smooth muscle actin, desmin, and inhibin were performed to confirm the histological impression. All histopathologic evaluations were performed by experienced pathologists from the Pathology Department of SRRSH. Study data were collected from the patients’ medical files: age, gravidity, parity, menopausal status, complaints, preoperative evaluation, type of surgeries, postoperative histology, and follow-up interval.
Data availability
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
References
Lerwill, M. F., Sung, R., Oliva, E., Prat, J. & Young, R. H. Smooth muscle tumors of the ovary: A clinicopathologic study of 54 cases emphasizing prognostic criteria, histologic variants, and differential diagnosis. Am. J. Surg. Pathol. 28(11), 1436–1451. https://doi.org/10.1097/01.pas.0000141393.99300.d0 (2004).
Doss, B. J. et al. Ovarian leiomyomas: Clinicopathologic features in fifteen cases. Int. J. Gynecol. Pathol. 18(1), 63–68 (1999).
Tsalacopoulos, G. & Tiltman, A. Leiomyoma of the ovary. A report of 3 cases. S Afr. Med. J. 59(16), 574–575 (1981).
Fallahzadeh, H., Dockerty, M. B. & Lee, R. A. Leiomyoma of the ovary: Report of five cases and review of the literature. Am. J. Obstet. Gynecol. 113(3), 394–398. https://doi.org/10.1016/0002-9378(72)90691-6 (1972).
Scully, R. E. Smooth-muscle differentiation in genital tract disorders. Arch. Pathol. Lab. Med. 105(10), 505–507 (1981).
Lim, S. C. & Jeon, H. J. Bilateral primary ovarian leiomyoma in a young woman: Case report and literature review. Gynecol. Oncol. 95(3), 733–735. https://doi.org/10.1016/j.ygyno.2004.07.048 (2004).
Liang, G., Wu, Z., Zhu, L. & Ruan, F. Case Report: Primary ovarian leiomyoma: A clinical analysis of Case Series and Literature Review. Front. Med. (Lausanne). 9, 822339. https://doi.org/10.3389/fmed.2022.822339 (2022).
Koo, Y. J. et al. Ovarian leiomyoma as a potential cause of compromised fertility. Fertil Steril. 95(3),1120.e11-14 (2011). https://doi.org/10.1016/j.fertnstert.2010.09.007
Guney, M., Ozsoy, M., Oral, B., Mungan, T. & Kapucuoglu, N. Unilateral primary ovarian leiomyoma in adolescent: A case report. Arch. Gynecol. Obstet. 275(6), 507–510. https://doi.org/10.1007/s00404-006-0291-3 (2007).
Khaffaf, N., Khaffaf, H. & Weketich, S. Giant ovarian leiomyoma as a rare cause of acute abdomen and hydronephrosis. Obstet. Gynecol. 87(5 Pt 2), 872–873 (1996).
Nicoll, J. J. & Cox, P. J. Leiomyoma of the ovary with ascites and hydrothorax. Am. J. Obstet. Gynecol. 161(1), 177–178. https://doi.org/10.1016/0002-9378(89)90260-3 (1989).
Yumru, A. E. et al. The relation between the presence of a giant primary ovarian leiomyoma and the occurrence of epilepsy as a paraneoplastic syndrome. Arch. Gynecol. Obstet. 281(3), 531–534. https://doi.org/10.1007/s00404-009-1184-z (2010).
Zhao, X., Chen, L., Zeng, W., Jin, B. & Du, W. Laparoscopic tumorectomy for a primary ovarian leiomyoma during pregnancy: A case report. Oncol. Lett. 8(6), 2523–2526. https://doi.org/10.3892/ol.2014.2596 (2014).
Han, L., Shi, G. & Ruan, J. Minimally invasive resection of Ovarian Leiomyoma. J. Minim. Invasive Gynecol. 31(3), 171. https://doi.org/10.1016/j.jmig.2023.11.015 (2024).
Prayson, R. A. & Hart, W. R. Primary smooth-muscle tumors of the ovary. A clinicopathologic study of four leiomyomas and two mitotically active leiomyomas. Arch. Pathol. Lab. Med. 116(10), 1068–1071 (1992).
Cho, Y. J., Lee, H. S., Kim, J. M., Joo, K. Y. & Kim, M. L. Clinical characteristics and surgical management options for ovarian fibroma/fibrothecoma: a study of 97 cases. Gynecol. Obstet. Invest. 76(3), 182–187. https://doi.org/10.1159/000354555 (2013).
Son, C. E. et al. Laparoscopic surgical management and clinical characteristics of ovarian fibromas. JSLS 15(1), 16–20. https://doi.org/10.4293/108680810X12924466009087 (2011).
Pervan, M. et al. Primary ovarian leiomyoma: A rare ovarian tumour. Arch. Gynecol. Obstet. 308(4), 1379–1380. https://doi.org/10.1007/s00404-022-06842-4 (2023).
Kitamura, Y. et al. Primary ovarian Leiomyoma Associated with multiple uterine leiomyomas. Gynecol. Minim. Invasive Ther. 10(1), 50–52. https://doi.org/10.4103/GMIT.GMIT_97_19 (2021).
Lewis, G., Dye, A., Mohamed, A., Siddiqi, A. & Hew, K. Torsion of an ovarian leiomyoma in a patient with Turner Syndrome. J. Minim. Invasive Gynecol. 31(3), 172–173. https://doi.org/10.1016/j.jmig.2023.11.018 (2024).
Kim, M. Laparoscopic management of a twisted ovarian leiomyoma in a woman with 10 weeks’ gestation: case report and literature review. Med. (Baltim). 95(44), e5319. https://doi.org/10.1097/MD.0000000000005319 (2016).
Akizawa, Y. et al. Gorlin syndrome with an ovarian leiomyoma associated with a PTCH1 second hit. Am. J. Med. Genet. A. 170A(4), 1029–1034. https://doi.org/10.1002/ajmg.a.37517 (2016).
Funding
This work was supported by a grant (No. LQ20H040011) from Zhejiang Provincial Natural Science Foundation of China, and a grant (2021KY181) from Zhejiang Province Medical Science and Technology Plan Project.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jiaren Zhang, and Rong Zhu. The first draft of the manuscript was written by Jiaren Zhang and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, J., Zhu, R. & Lin, X. Clinical characteristics and laparoscopic management experience of primary ovarian leiomyoma. Sci Rep 15, 1988 (2025). https://doi.org/10.1038/s41598-025-86280-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86280-9