Abstract
Using transthoracic echocardiography (TTE) and transesophageal echocardiography (TEE) to investigate the occurrence and related causes of iatrogenic atrial septal defect (iASD) after catheter ablation combined with left atrial appendage closure (LAAC) for atrial fibrillation (AF) and its impact on the right heart system. We retrospectively analyzed 330 patients that underwent combined procedure of catheter ablation for AF and LAAC at General Hospital of Northern Theater Command from January 2018 to March 2022. These patients were divided into iASD group and non-iASD group according to whether there was persistent iASD shown on TEE at 3 months after procedure. There were 96 (29.1%) patients with iASD and 234 patients without in the TEE follow up at 3 months post-operation. Patients with iASD had larger left atrial volumes (76.5 ± 35.2 ml vs. 61.1 ± 21.9 ml, p = 0.036) as well as higher occurrence of mitral regurgitation (MR) (32.3% vs. 12.8%, p = 0.018) and tricuspid regurgitation (TR) (27.1% vs. 7.3%, p = 0.002). Procedural features showed that patients with persistent iASD had longer procedure time (92.1 ± 36.3 vs. 69.1 ± 17.8 min, p = 0.003) and larger sheath sizes (4.1 ± 1.2 mm vs. 3.3 ± 1.2 mm, p = 0.022). The preoperative and postoperative right heart parameters of patients in the persistent iASD group were compared, and there were no significant differences on right atrial/ventricular diameter, right heart systolic/diastolic function and pulmonary artery pressure (P > 0.05). The occurrence of iASD 3 months after combined atrial fibrillation ablation and LAAC was 29.1%. The size of left atrium, the pressure of left atrium, the manipulation time within left atrium, the size of sheath, and the use of ICE during operation was related to the closure of iASD.
Similar content being viewed by others
Introduction
As one of the most common arrhythmias, atrial fibrillation (AF) is prone to cause ventricular rhythm irregularity, impaired heart function and atrial mural thrombosis. The combined operation of catheter ablation and left atrial appendage closure (LAAC) can improve symptoms and prevent thrombosis at the same time to achieve the purpose of “one operation, two curative effects” and to improve the efficiency of treatment. Iatrogenic atrial septal defect (iASD) is initially formed during the process of delivering the sheath from the right heart to the left heart via atrial septal puncture (TSP). At present, there are relatively few researches on iASD and the prognosis of iASD caused by TSP during the combined procedure of AF ablation and LAAC and the influencing factors are still unknown.
Methods
Population
A total of 330 patients who underwent catheter ablation combined with LAAC for AF in General Hospital of Northern Theater Command from January 2018 to March 2022 were included. The patients with previous procedure with TSP, cardiomyopathy, valvular disease, congenital heart disease have been excluded. Demographic information, baseline laboratory information and the previous histories of all patients were collected. The study has been approved by the ethics committee of General Hospital of Northern Theater Command, and all methods were performed in accordance with the relevant guidelines and regulations,, such as Declaration of Helsinki.
TTE and TEE examinations
Philips EPIQ 7 C color Doppler ultrasound and X5-1 transthoracic ultrasound probe were used for transthoracic echocardiography (TTE), and X7-2t multiplane transesophageal ultrasound probe (frequency 5–9 MHz) was used for transesophageal echocardiography (TEE). TTE was used to evaluate the cardiac structure and function and critical parameters were measured, such as the left atrial diameter (LAd), pulmonary artery diameter (PAd), right atrial diameter (RAd), left atrial ejection fraction (LAEF), left ventricular ejection fraction (LVEF), cardiac stroke volume (SV), left ventricular short axis shortening rate (FS), mitral and tricuspid valve regurgitation area and regurgitation velocity. TEE was used to screening for thrombus in left atrial appendage (LAA) and other cardiac chambers and to assess the LAA morphology at angles of 0°, 45°, 90° and 135°, and 3–5 cardiac cycles were taken and saved for off-line analysis.
Catheter ablation and LAAC procedure
Radiofrequency catheter ablation (RFCA) or cryo-balloon catheter ablation (CBCA) was chosen at the operator’s discretion based on individual patients’ situation and was performed under local anesthesia and sedation. All catheters were advanced into the cardiac cavity through femoral veins or right jugular vein. Single transseptal puncture (TSP) in CBCA and dual TSP in RFCA were performed, with a 15 F sheath and two 8.5 F sheaths advanced into the LA, separately. After that, ablation was performed with circumferential pulmonary vein isolation, and additional linear or focal ablation might be done if needed. Ablation point AI criteria: The AI value of the posterior wall of the left atrium is typically 380 to 390, while the AI values for the top and bottom walls are 400, and for the anterior wall, it ranges from 430 to 450. Additional linear ablation or ablation of extra-pulmonary vein trigger sites may be performed when necessary. The endpoint of ablation is complete electrical isolation of both pulmonary veins. If the patient’s rhythm remains atrial fibrillation after ablation, bidirectional 150–200 J synchronous direct current cardioversion is administered to convert to sinus rhythm. After ablation, an electrophysiological examination is conducted. If other types of arrhythmias are induced, radiofrequency ablation is also performed for treatment.
After confirming the complete electrical isolation and un-inducibility of AF, the LAAC was performed under general anesthesia with the TEE and fluoroscopy guidance or under local anesthesia with the ICE and fluoroscopy guidance. The transseptal sheaths for ablation were exchanged for the LAAC sheath (14 F for Watchman and 12 F for LAmbre). The size of LAAC device was selected according to the measurement of LAA on the fluoroscopy with contrast agent infusion and the imaging assessment of ICE or TEE. The LAAC implantation complied with the PASS or COST principle.
Post-procedure management and follow-up
After procedure, patients received NOAC for three months and then aspirin plus clopidogrel for 6 months, after that aspirin alone was administered for lifelong. All patients were scheduled for TEE examination at 3 months and TTE at 3, 6 and 12 months. For patients with poor endothelialization on the surface of LAAC at 3-month follow up, the administration of anticoagulant and antiplatelet was individual-specifically adjusted by physicians (Fig. 1).
Statistical analysis
The categorical variables were expressed as frequencies and percentages and compared with chi square test or Fisher exact test. The continuous variables were expressed as mean ± standard deviation and compared using independent sample t test for those with a normal distribution, or expressed as median (interquartile range) and compared using Mann–Whitney U test for those with a non-normal distribution. Logistic regression correlation analysis was conducted to identify the predictor of iASD closure. P < 0.05 was considered as statistically significant.
Results
Incidence of iASD and the characteristics of patients with iASD
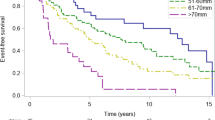
There were 179 males and 151 females, with an average age of 65.81 ± 4.35 years. All patients successfully completed the AF catheter ablation combined with LAAC, without complications such as pericardial tamponade, thromboembolism, left atrial rupture, and left atrial esophageal fistula. In the 3-month follow up with TEE, 96 patients (29.1%) showed defect at the atrial septum and shunt between left and right atrium which demonstrated the existence of iASD, and 234 (70.9%) patients had no iASD. Among these patients in the iASD group, 3 patients were lost to follow-up at 6 months (for the reason of COVID), and in the remaining 93 patients, 42 patients (45.0%) had the spontaneous healing. Comparing the baseline characteristics of patients in iASD group and non-iASD group, there were no significant differences between two groups except for the baseline diameter of left atrium (LA), with the iASD group having larger LA than the non-iASD group [iASD group vs. non-iASD group: 49.0 (31.0, 55.0) vs. 420 (30.0, 48.0), P = 0.036; Table 1]. In the comparison of the clinical information related to the combined procedure, there were no significant differences on the type of LAAC devices between two groups, but the iASD group had larger size of the transseptal sheath and longer manipulation time of catheters and sheathes within LA (92.1 ± 36.3vs 69.1 ± 17.8 min, p = 0.003), and less ICE was used in iASD group (Table 2). In addition, we also observed that the puncture site of iASD group was relatively low, about 1.85 ± 2.23 cm above the ostium of the inferior vena cava.
Comparison on echocardiographic parameters 3 months after operation between the two groups
At 3 months after surgery, the persistent iASD group had higher occurrence of postoperative MR (32.3% vs 12.8%, p = 0.018) and postoperative TR (27.1% vs 7.3%, p = 0.002). No significant differences were found on LVEF, CO, SV, FS and other echocardiographic indexes (P > 0.05; Table 3). Comparing the right heart parameters, there was no significant differences on right heart size, right heart systolic/diastolic function and pulmonary artery pressure between two groups (P > 0.05).
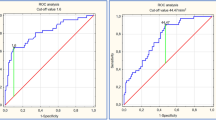
Results of logistic regression analysis
In the univariate analysis, there were significant differences on the pre-operational size of LA, the manipulation time within LA, and the size of sheath between two groups. And when these variables were input into the multivariate analysis, it showed that longer manipulation time within LA and larger size of sheath were the independent risk factors for iASD (Table 4). The risk of non-closure of iASD increased by 20.8% for every 1 mm increase in the size of left atrium before surgery.
Two different operators measure and analyze the ultrasound parameters to compare the repeatability of these parameters among observers. Perform two or more data measurements during analysis and measurement to compare the repeatability of these parameters within the observer. Both inter observer and intra observer repeatability tests are expressed using intra class correlation coefficients (ICC), with ICC values greater than 0.75 (P < 0.05) indicating good repeatability of the diagnostic test.
Discussion
The advantage of the catheter ablation combined with LAAC for AF is symptoms improvement and thrombosis prevention at the same time, and it has been increasingly applied in the clinical treatment of AF. TSP is increasingly applied in transcatheter interventional therapy, so it is important to evaluate the influencing factors of iASD formation and its impact on the right heart system.
Incidence and associated factors of iASD
As a crucial step in many cardiac interventional procedures, TSP can lead to the occurrence of iASD after the operation. However, the incidence of iASD varies with different interventional operations. In the present research, among 330 patients undergoing catheter ablation combined with LAAC for AF, 96 patients developed iASD 3 months after the operation, with the incidence of 29.1%. We found that the incidence of persistent iASD was similar to that after radiofrequency ablation or simple LAAC1, but significantly lower than that after transcatheter edge-to-edge mitral valve repair (TEER)2,3,4.
The results showed that the factors related to the closure of iASD included: the size of left atrium, the pressure of left atrium, the manipulation time within left atrium, and the size of sheath. The increased pressure of the left atrium and the enlargement of the left atrium will lead to the increase of left-to-right shunt in iASD patients, and at the same time, a continuous outward pulling force will be exerted on the defect edge, making the iASD difficult to heal5,6. Therefore, preoperative evaluation of the size and the pressure of the left atrium is crucial to predict the healing of iASD, and different preoperative plans should be made according to these parameters. If the inner diameter of the left atrium is large, it is recommended to use a smaller sheath and to shorten the operation time within the left atrium as far as possible to avoid the occurrence of persistent iASD after operation. Considering that the more severe MR will inevitably lead to further enlargement of the left atrium, which in turn will aggravate the functional MR. We believe that MR is a potential factor for the existence of persistent iASD. Besides, the left-to-right shunt of persistent iASD will lead to the expansion of the right heart system and the left atrium, thus it is possible to further exacerbate functional MR. Previous studies have shown that patients with iASD after cardiac intervention were likely to have more severe MR compared with those with spontaneous closure7.
We compared the patients using 10 F and 14 F sheaths during the operation, and found that the incidence of iASD in the former was significantly lower than that in the latter at 3 months after the operation. The incidence of iASD increased with the increase of sheath size8. Studies have shown that compared with radiofrequency ablation, the incidence of iASD after cryoballoon ablation is often higher. The reason is that radiofrequency ablation often uses a smaller sheath with double puncture, while in cryoballoon ablation, a larger sheath is usually used for single TSP, which will leave a larger aperture on the atrial septum9. In addition, during cryoballoon ablation, a series of sheath manipulations such as rotation and advancement performed by the operator to deliver the catheter to the right inferior pulmonary vein may also lead to the stretching and tearing of the atrial septum10. Larger the size of the sheath and more complicated manipulation of the sheath would cause greater the separation and tearing of the atrial septal tissue. Therefore, it can be inferred that intraoperative sheath manipulation can also be an important factor affecting the occurrence of persistent iASD.32 patients received additional extensive ablation. Extensive ablation, particularly with RF, can exacerbate pulmonary hypertension and increase the likelihood of residual shunting11.
In addition, studies have shown that different sites of TSP can also affect the occurrence of persistent iASD. As the thinnest part of the atrial septum, the oval fossa is the most commonly used site for atrial septal puncture for catheter ablation. However, some studies have shown that the anterior and inferior edge of TSP seems to be a better choice for ablation due to smaller angles between the catheter and pulmonary veins, which would benefit to catheter manipulation12,13. In the present research, the puncture site is usually located near the ostium of inferior vena cava (1.85 ± 2.23 cm above the ostium of inferior vena cava), where the sheath and the left atrial appendage can acquire better coaxiality, which is convenient for the occlusion of the left atrial appendage14. However, more inferior and posterior position of the TSP can impose more tension to the sheath and increase the supporting force between the sheath and the puncture site, which inevitably causes the laceration of the puncture site during the operation. Thus, iASD occurs.
Effects of persistent iASD on the right heart system
After the operation, the restoration of sinus rhythm and improvement on hemodynamics can give rise to the reduction in the size of left and right atrium and relieving TR. However, the occurrence of moderate or severe TR in the persistent iASD group were significantly higher than the spontaneous closure group. We speculated that the occurrence and severity of TR was related to the right heart overload caused by continuous left-to-right atrial shunt, which leads to the enlargement of right heart, thus causing functional TR15,16. On the other hand, after radiofrequency ablation, the flexibility of the left atrium decreases to varying degrees, so the left atrium becomes rigid and the pressure of the left atrium increases17, which further causes pressure of pulmonary vessel increases, ultimately affecting the right heart system.
The hemodynamics of iASD is essentially equivalent to congenital atrial septal defect. Although the clinical consequences caused by persistent right-to-left iASD shunt are often very serious, such as paradoxical embolism18,19, we still cannot ignore the possible harmful consequences caused by left-to-right shunt. For example, the risk and possibility of secondary right heart enlargement, pulmonary hypertension, right heart failure, migraine, and paradoxical embolism. After the comparison of preoperative and postoperative right heart parameters of patients in the persistent iASD group, despite there were no obvious progressive exacerbation of right heart enlargement or pulmonary hypertension, the TTE within 24 h after operation shown that 11 patients with iASD > 7 mm had a trend of increasing right heart systolic pressure, though with no statistically significant. We speculate that once the iASD is large enough, it may have a lasting impact on the right heart system. There is a possibility that the persistent iASD can cause right heart volume overload, but current studies show that it will not affect the right heart function or pulmonary artery systolic blood pressure in the short term.
Effect of persistent iASD on left cardiac system
While LVEF is the main evaluation index of the overall left ventricular systolic function in patients with AF, FS can also reflect the left ventricular contraction and has a certain correlation with LVEF. In this study, M-mode echocardiography was used to measure LVEF, CO, SV and FS to evaluate the potential effects of iASD on left ventricular systolic function. Our results showed that the difference on LVEF between the two groups was not statistically significant, and similar results were also found on FS and SV between the two groups. So, iASD would not cause significant changes in left ventricular systolic function in the short term. This is consistent with findings of Mitrega et al. that atrial septal defect after LAAC did not affect the left cardiac function20 .
The size of left atrium in the persistent iASD group and the spontaneous closure group was compared between pre- and post-operation, and it was found that the size of left atrium of the two groups was reduced to different degrees after operation, and the ratio of reduction on left atrium diameter in the persistent iASD group was higher than that of the spontaneous closure group (15.44% vs 15.12%). We believe that the left-to-right shunting via persistent iASD will increase the pressure of the right atrium and reduce the pressure of the left atrium, which is consistent with the mechanism of percutaneous atrial septostomy, as the treatment of refractory heart failure, to establish a channel between the left and right atrium to effectively reduce the pressure of the side with higher pressure21. Previous studies have shown that AF can lead to left atrium remodeling, and left atrium remodeling will in turn affect the development of AF. Left atrial enlargement and left atrial pressure increase are risk factors for the occurrence of AF. The recovery of left atrial size and pressure can effectively reduce the recurrence rate of AF.
Limitations
There were several limitations in this research. Firstly, patients’ compliance was poor and for the reason of COVID, only 3 patients were lost, the percentage of loss of follow-up was 0.09%, which may cause bias to this research. Secondly, the number of cases involving cryoablation in this study is particularly small. Due to its small proportion, the statistical results have significant deviations and cannot be statistically analyzed, different ablation techniques (radiofrequency catheter ablation [RFCA] and cryo-balloon catheter ablation [CBCA]) might influence the occurrence of iASD. Thirdly, as an invasive examine, TEE only could be done once at three-month follow-up period after the one-stop surgery, the one-stop the follow-up period was relatively short, so the outcomes of long-term follow-up is still unknown. TTE was the only imaging study used in follow-up more than 6 months, so the incidence of iASD may be underestimated. A large number of data are still needed to further verify the results of this study.
Conclusion
The rate of iASD in patients with AF undergoing combined operation of catheter ablation and LAAC was high. And the closure of iASD was related to the size of left atrium, the pressure of left atrium, the manipulation time within left atrium, and the size of sheath.
Data availability
All data generated or analysed during this study are included in this published article.
References
Nagy, Z. et al. Prospective evaluation of iatrogenic atrial septal defect after cryoballoon or radiofrequency catheter ablation of atrial fibrillation-EVITA study. J. Interv. Card. Electrophysiol. 56, 19–27 (2019).
Schueler, R. et al. Persistence of iatrogenic atrial septal defect after interventional mitral valve repair with the MitraClip system: a note of caution. JACC Cardiovasc. Interv. 8, 450–459 (2015).
Kadado, A. J. & Islam, A. Iatrogenic atrial septal defect following the MitraClip procedure: a state-of-the-art review. Catheter. Cardiovasc. Interv. 97, E1043–e1052 (2021).
Paukovitsch, M. et al. Prevalence of iatrogenic atrial septal defects (iASD) after mitral valve (MV) transcatheter edge-to-edge repair (TEER) in the long-term follow-up. Open. Heart 8(2) (2021).
Ikenaga, H. et al. Left atrial pressure is associated with iatrogenic atrial septal defect after mitral valve clip. Heart 105, 864–872 (2019).
Hoffmann, R., Altiok, E., Reith, S., Brehmer, K. & Almalla, M. Functional effect of new atrial septal defect after percutaneous mitral valve repair using the MitraClip device. Am. J. Cardiol. 113, 1228–1233 (2014).
Nelles, D. et al. Incidence, persistence, and clinical relevance of iatrogenic atrial septal defects after percutaneous left atrial appendage occlusion. Echocardiography 39, 65–73 (2022).
Singh, S. M., Douglas, P. S. & Reddy, V. Y. The incidence and long-term clinical outcome of iatrogenic atrial septal defects secondary to transseptal catheterization with a 12F transseptal sheath. Circ. Arrhythm. Electrophysiol. 4, 166–171 (2011).
Linhart, M. et al. High rate of persistent iatrogenic atrial septal defect after single transseptal puncture for cryoballoon pulmonary vein isolation. J. Interv. Card. Electrophysiol. 52, 141–148 (2018).
Sieira, J. et al. One year incidence of iatrogenic atrial septal defect after cryoballoon ablation for atrial fibrillation. J. Cardiovasc. Electrophysiol. 25, 11–15 (2014).
Mohanty, S. et al. Pulsed-field ablation does not worsen baseline pulmonary hypertension following prior radiofrequency ablations. JACC Clin. Electrophysiol. 10 (3), 477–486. https://doi.org/10.1016/j.jacep.2023.11.005 (2024).
Rich, M. E., Tseng, A., Lim, H. W., Wang, P. J. & Su, W. W. Reduction of iatrogenic atrial septal defects with an anterior and inferior transseptal puncture site when operating the cryoballoon ablation catheter. J. Vis. Exp. 15, e52811 (2015).
Velagapudi, P. et al. Intracardiac vs transesophageal echocardiography for percutaneous left atrial appendage occlusion: a meta-analysis. J. Cardiovasc. Electrophysiol. 30, 461–467 (2019).
Della Rocca, D. G. et al. Three-dimensional intracardiac echocardiography for left atrial appendage sizing and percutaneous occlusion guidance. Europace 26 (1), euae010. https://doi.org/10.1093/europace/euae010 (2023).
Akella, K. et al. Evaluating the role of transesophageal echocardiography (TEE) or intracardiac echocardiography (ICE) in left atrial appendage occlusion: a meta-analysis. J. Interv. Card. Electrophysiol. 60, 41–48 (2021).
Ren, J. F. et al. Intracardiac echocardiographic diagnosis of thrombus formation in the left atrial appendage: a complementary role to transesophageal echocardiography. Echocardiography 30 (1), 72–80 (2013).
Puga, L. et al. Iatrogenic atrial septal defect after percutaneous left atrial appendage closure: a single-center study. Int. J. Cardiovasc. Imaging. 37, 2359–2368 (2021).
Morikawa, T. et al. Right-to-left shunt through iatrogenic atrial septal defect after MitraClip procedure. JACC Cardiovasc. Interv. 13, 1544–1553 (2020).
Alkhouli, M. et al. Iatrogenic atrial septal defect following transseptal cardiac interventions. Int. J. Cardiol. 209, 142–148 (2016).
Mitrega, K. et al. The influence of iatrogenic interatrial septum leaks after left atrial appendage closure on cardiac function test results. J. Interv. Cardiol. 31, 679–684 (2018).
Hasenfuß, G. et al. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, open-label, single-arm, phase 1 trial. Lancet 387, 1298–1304 (2016).
Author information
Authors and Affiliations
Contributions
N.N.L.: conceived and designed the experiments, performed the experiments. Y.X.S. and S.N.L.: performed the experiments, analyzed the data, and wrote the manuscript. M.L., Z.L.W., P.Z., Q.Z. and W.W.Z.: analyzed the data and proofed the manuscript. All authors have proofed the article.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the ethics committee of General Hospital of Northern Theater Command, and all methods were performed in accordance with the relevant guidelines and regulations, such as Declaration of Helsinki.
Consent for publication and participation
All the patients have signed the informed consent for participation and publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Su, Y.X., Li, S.N., Liu, N.N. et al. Echocardiography evaluation of iatrogenic atrial septal defect after combined procedure of catheter ablation and left atrial appendage closure for atrial fibrillation. Sci Rep 15, 2466 (2025). https://doi.org/10.1038/s41598-025-86657-w
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86657-w