Abstract
The increasing use of recreational nitrous oxide (\(\hbox {N}_{2}\)O) in the Netherlands and its link to traffic accidents highlights the need for reliable detection methods for law enforcement. This study focused on ex vivo detection of \(\hbox {N}_{2}\)O in exhaled breath and examining its persistence in the human body. Firstly, a low-cost portable infrared based detector was selected and validated to detect \(\hbox {N}_{2}\)O in air. Then, the influence of interferents and conditions potentially influencing the analysis were evaluated including relative humidity, ethanol, acetaldehyde and \(\hbox {CO}_{2}\). Subsequently, \(\hbox {N}_{2}\)O breathing dynamics were evaluated in vitro and ex vivo. Initially, a lung simulator was used to model respiratory mechanics and \(\hbox {N}_{2}\)O decay, revealing detectable \(\hbox {N}_{2}\)O levels up to 90 min after exposure. In the final part of this study, a controlled single and double dose of \(\hbox {N}_{2}\)O gas was administered to 24 volunteers in an operating theatre. The presence of \(\hbox {N}_{2}\)O in exhaled breath of the volunteers was analysed using infra red spectroscopy every 12-15 min. Our results show that \(\hbox {N}_{2}\)O was detectable in exhaled breath for a minimum of 60 min post-administration and revealed a window of detection to potentially measure \(\hbox {N}_{2}\)O for law enforcement and forensic purposes.
Similar content being viewed by others
Introduction
Nitrous oxide (\(\hbox {N}_{2}\)O) is a gaseous inorganic compound under standard atmospheric pressure which has a sweet taste and smell1. In combination with its bacteriostatic properties \(\hbox {N}_{2}\)O is considered to be an ideal propellant for culinary whipped cream preparations2,3. Consequently, \(\hbox {N}_{2}\)O is easily obtainable in e.g., retail stores. When inhaled in sufficient quantities, \(\hbox {N}_{2}\)O acts as a mild anesthetic and is employed as such during medical procedures4. A common side effect of \(\hbox {N}_{2}\)O inhalation is the induction of feelings of euphoria, which gives the gas its colloquial name laughing gas5,6. Its euphoric potential and widespread availability are the likely reasons for \(\hbox {N}_{2}\)O to be ranked the 10th most common recreational drug of abuse in the 2019 Global Drug Survey7. Unlike its use in medical practice, where the concentration is typically limited to 70 percent \(\hbox {N}_{2}\)O and 30 percent oxygen (\(\hbox {O}_{2}\)), recreational misuse consists of the inhalation of an imprecise dose of almost pure \(\hbox {N}_{2}\)O8,9,10. Notably, the absence of \(\hbox {O}_{2}\) in recreational \(\hbox {N}_{2}\)O use introduces the risk of asphyxiation11and consequently loss of consciousness is often reported6. Other risks of recreational \(\hbox {N}_{2}\)O inhalation include frost bite injuries, as a result of gas decompression when \(\hbox {N}_{2}\)O is released from a pressurized container, accidents due to falling, \(\hbox {N}_{2}\)O addiction, and a potentially severe peripheral myelopathy caused by inactivation of cobalamin, in turn leading to demyelination of spinal tract neurons12,13,14.
A directly related and potentially significant threat to public health is the misuse of \(\hbox {N}_{2}\)O in road traffic15,16. In recent years, national statistics of the Dutch police reported over 900 traffic accidents involving serious injury or a fatal outcome, where \(\hbox {N}_{2}\)O abuse was suspected to have played a role (Fig. 1a). Also outside the Netherlands \(\hbox {N}_{2}\)O abuse is increasingly becoming a problem and in 2019 it was identified as the \(10^{th}\)most prevalent drug of abuse by the global drug survey16. Given the profound state of dissociation, ataxia, and impaired consciousness that is generally described to accompany the recreational inhalation of \(\hbox {N}_{2}\)O, this suspicion seems justified. Furthermore, previous experimental studies on the effects of medical \(\hbox {N}_{2}\)O (i.e. \(\hbox {N}_{2}\)O - \(\hbox {O}_{2}\) mixtures) unequivocally have demonstrated significant psychomotor impairment during \(\hbox {N}_{2}\)O exposure17. For example, one study specifically investigated driving performance and reported performance impairment that lasted up to 30 min after exposure18.
(a) Statistics retrieved from the Dutch National police, showing the prevalence of laughing gas related traffic accidents from 2019–2023. (b) The recreational dosing method and schematic depictions of the in vitro and ex vivo models used in this study. (c) The detection methodology used to detect \(\hbox {N}_{2}\)O in exhaled breath.
In order to address these public health concerns, the Dutch government installed a ban on \(\hbox {N}_{2}\)O effective from January \(1^{st}\), 2023 and referred to its risks regarding road safety in the public announcement of the state secretary of the Ministry of Health19. As a schedule 2 illicit substance under the Dutch Opioid law trafficking, usage, selling and possession of \(\hbox {N}_{2}\)O have been prohibited since then, with the exception of professional, technical, culinary, and medical use; hence a legitimate circuit for \(\hbox {N}_{2}\)O remains. Therefore, when confronted with \(\hbox {N}_{2}\)O paraphernalia, law enforcement need to be able to demonstrate that these are intended or have been used for recreational inhalation of \(\hbox {N}_{2}\)O. Similarly, in case of driving under influence (DUI), the police need to make a plausible case that the driver recently inhaled \(\hbox {N}_{2}\)O. However, in the absence of a validated method for the detection of recreational \(\hbox {N}_{2}\)O use, law enforcement are dependent solely on circumstantial evidence. To make solid arguments in court and dissuade recreational \(\hbox {N}_{2}\)O users from DUI, it is imperative to have suitable and reliable portable detection technologies.
After inhalation \(\hbox {N}_{2}\)O enters the bloodstream as a result of pressure gradients where the rate of exchange largely depends on its blood gas partition coefficient20. Interestingly, studies on the excretion have shown that \(\hbox {N}_{2}\)O is metabolized to a minimal extent, mainly leaving the body in the intact form through the lungs via expiration5,21. Since the main elimination pathway after dosage is through respiration, a plausible detection system for forensic and law enforcement applications would thus focus on analysis of exhaled breath. As a consequence, \(\hbox {N}_{2}\)O’s window of detection is expected to largely depend on the human respiratory mechanics and blood-gas exchange in the lungs. Furthermore, when measuring \(\hbox {N}_{2}\)O in exhaled breath, several other parameters are crucial for accurate on-site detection and reliable dosing estimation. Humidity and the presence of interfering substances are critical factors that can significantly influence the performance and accuracy of detection equipment in an operational environment. Different studies on gas analyzers have shown these unwanted effects of humidity on the detector signal22,23,24. When it comes to selectivity the study of Wilkes (1996) discussed the interference of \(\hbox {CO}_{2}\) and \(\hbox {N}_{2}\)O on IR analysis of volatile anaesthetics due to the overlapping bands in the IR spectrum, where they solved this overlap by background subtraction of the signal25. In an operational environment not all of these factors can be eliminated, highlighting the importance of understanding the detectability of \(\hbox {N}_{2}\)O in exhaled breath after a recreational dose of \(\hbox {N}_{2}\)O.
Consequently, the primary aims of this study were to determine the feasibility of measuring \(\hbox {N}_{2}\)O in exhaled breath after exposure to a recreational dosing method and assessing the influence of potential interferents on the concentration measurements (Fig. 1b). Secondly, this works aims to establish a window of detection, using both in vitro and ex vivo models (Fig. 1c). In the final part of the study a conceptual framework has been provided using a two-compartment re-circulatory model in order to understand the \(\hbox {N}_{2}\)O concentration decay pathway in exhaled breath26,27. We envisage that the knowledge gained in this study will deepen our understanding of \(\hbox {N}_{2}\)O kinetics after a recreational consumption and pave the way for the development of detection capabilities for forensic and law enforcement purposes related to \(\hbox {N}_{2}\)O misuse.
Results
Selectivity and sensitivity of detection
The response of the \(\hbox {N}_{2}\)O analyzer across four generated concentrations (0, 25, 48, and 92 ppm) of \(\hbox {N}_{2}\)O at low (RH = 10%), medium (RH = 50%), and high relative humidity (RH = 95%) are presented in Fig. 2. The measured concentrations were measured with standard deviations at and below (1 ppm) and the accuracy of the analyzer was found to be within 20% of the generated concentrations. Furthermore, no notable difference in measured signal was observed between the three different RH levels.
Then, the extent to which the \(\hbox {N}_{2}\)O analyzer was affected by the presence of significant levels of interferents, \(\hbox {CO}_{2}\) and high humidity was analysed. Ethanol (1000 ppm), nitrogen dioxide \(\hbox {NO}_{2}\) (1000 ppm) and acetaldehyde (1000 ppm) did not show any signal response on the \(\hbox {N}_{2}\)O analyzer. In turn, 100 ppm \(\hbox {N}_{2}\)O in the presence of ethanol (1000 ppm), nitrogen dioxide (1000 ppm) or acetaldehyde (1000 ppm) showed concentrations of 91, 93 and 93 ppm respectively. No signal was observed when the \(\hbox {N}_{2}\)O analyzer was exposed to air mixed with \(\hbox {CO}_{2}\) yielding a gas mixture containing up to percent 8% (v/v) of \(\hbox {CO}_{2}\). A continuous stream of 100 ppm \(\hbox {N}_{2}\)O mixed with 8% (v/v) of \(\hbox {CO}_{2}\) yielded a measured concentration of 93 ppm \(\hbox {N}_{2}\)O as indicated by the analyzer.
Influence of respiratory mechanics on the window of detection
In vitro study
In Fig. 3(a) the measured \(\hbox {N}_2\)O concentration in the lung simulator is shown for four different Air Refresh Ratios (ARR). In the first 15 min the \(\hbox {N}_2\)O concentration exceeded the upper limit of detection of the \(\hbox {N}_{2}\)O analyzer. The initial concentration is approximately between \(10^{5}\) and \(10^6\) ppm. This depends on the total volume of the lung simulator that is replaced with \(\hbox {N}_2\)O. Each experiment was performed in triplo and the average concentration and standard deviation is shown. The solid lines are fits using Eq. 4. The associated half-lifes of the fits are shown in (b) and (c) of Fig. 3. The gas exchange in the lung simulator is very well described by a fast exhalation process (b), typically \(t_{1/2,1} =1-2.5\) min, and slower gas redistribution process in the elastomer bellows (c), typically \(t_{1/2,2} =6-12\) min. Fig. 3 (b) shows that increasing the ARR shortens the half-life of the exhalation process. The gas redistribution process \(t_{1/2,2}\) is largely unaffected by the ARR.
(a) Concentration \(\hbox {N}_2\)O in the exhaled air of the lung simulator versus time for varying air refresh ratios (ARR). The \(\hbox {N}_2\)O concentration with an ARR of 0.10 first shows a steep decline (\(t_{1/2,1} = 2.45 \pm 0.09\) min) between 0–30 min, after 30 min the decline is less steep (\(t_{1/2,2} = 9.39\pm 1.25\) min). The lines are fits using the linear series gas redistribution model. (b/c) The corresponding half-lifes of (a) for different ARR. The \(\hbox {N}_2\)O concentration in the lung simulator is described by a fast gas-exchange process \(t_{1/2,1}=1-2.5\) min (b) and a slower timescale \(t_{1/2,2}=6-12\) min (c).
Ex vivo study
All participants in the ex vivo study successfully completed the entire testing procedure without the need for intervention by the supervising physician. The exhaled air of each participant was collected, analysed and repeated every 12–15 min until approximately 60 min had passed. The exact timing between succeeding measurements varied slightly per participant. Hence, the individual measurements of the first 80 min were binned in blocks of 20 min. After 80 min the data was averaged into a single bin. Fig. 4 shows the mean and the standard deviation of each bin of the ex vivo data, the dashed areas show the boundaries of each bin. No \(\hbox {N}_{2}\)O was observed with the \(\hbox {N}_{2}\)O analyzer by participants that underwent the placebo condition. At t = 20 min the measured \(\hbox {N}_2\)O concentration was below the upper limit of detection of the detector. At = 20 min the single dose \(\hbox {N}_2\)O concentration varied between 597–950 ppm, averaging at 742 \(\pm 138\) ppm and the double dose \(\hbox {N}_2\)O concentration varied between 855–940 ppm, averaging at 885 \(\pm 48\) ppm. The solid lines are fits using Eq. 5 (single dose \(t_{1/2} = 29.0 \pm 0.8\) min, double dose \(t_{1/2}=30.6 \pm 0.6\) min).
\(\hbox {N}_{2}\)O concentrations found in the ex vivo study at different time intervals. The individual measurements of the single-dose and double-dose are binned in time-steps of 20 min. The blue and grey lines are a fits with \(t_{1/2} = 29.0 \pm 0.8\) min (single dose) and \(t_{1/2}=30.6 \pm 0.6\) min (double dose).
Discussion
This study aimed to find a reliable method to measure \(\hbox {N}_{2}\)O in exhaled breath after exposure to a recreational inhalation method in a representative environment. Both in vitro and an ex vivo system were applied to define \(\hbox {N}_{2}\)O’s detection window. and determine the influence of potential interferents on concentration measurements. By applying a two-compartment recirculatory model, our objective was to understand the decay pathway of \(\hbox {N}_{2}\)O concentration in exhaled breath.
Measuring \(\hbox {N}_{2}\)O in a laboratory environment is vastly different than measuring it in exhaled breath. Human exhaled breath \(\hbox {CO}_{2}\)concentrations are generally quantified at 4 – 5% (v/v) and RHs ranging from 65 – 89%28. It is generally known that the strongest IR bands of \(\hbox {N}_{2}\)O (2224 \(\hbox {cm}^{-1}\)) and \(\hbox {CO}_{2}\) (2349 \(\hbox {cm}^{-1}\)) correspond very closely29. However, in the detection of \(\hbox {N}_{2}\)O, it is essential to account for the significantly higher background levels of \(\hbox {CO}_{2}\) compared to the relatively low concentrations of \(\hbox {N}_{2}\)O. The \(\hbox {N}_{2}\)O analyzer used in this study circumvented \(\hbox {CO}_{2}\) interference by fitting the inlet with a soda-lime filter for ex situ \(\hbox {CO}_{2}\) removal. However, when used without the filter the analyzer showed background concentrations of \(\hbox {N}_{2}\)O at elevated (>0.4% v/v) concentrations of \(\hbox {CO}_{2}\). In addition to \(\hbox {CO}_{2}\) interference, water is also an IR absorbent, which has a strong absorption band between 3000 and 3600 \(\hbox {cm}^{-1}\)due to the O-H stretch region30. In the gas phase, spacious water clusters can form with a enormous number of rotational and vibrational combinations, which may also overlap with the absorption bands \(\hbox {N}_{2}\)O31. Nonetheless, an interfering effect of varying RH levels on the signal of the IR analyzer was not observed when the analyzer was subjected to RH levels ranging from 10% to 95%. Both selective and sensitive detection of \(\hbox {N}_{2}\)O was achieved under laboratory and representative conditions, i.e. \(\hbox {CO}_{2}\) concentrations of up to 8% (v/v), a RH of 95% and the presence of a selection of common interfering compounds (acetone, nitrogen dioxide and acetaldehyde) that are likely to be found in a forensic or law enforcement situation. A possible explanation that no interference was observed by these compounds might a combination of the filter and a lack of overlap between the band maximums between these interferents and \(\hbox {N}_{2}\)O in the IR spectrum. In a similar fashion, the \(\hbox {N}_{2}\)O analyzer was able to determine concentrations in exhaled breath against a background of tobacco smoke. The exact composition of this background was unknown, but tobacco smoke has been reported to contain a complex chemical composition consisting of oxygen, nitrogen and sulfur-containing hydrocarbons in varying fractions depending on the source32. Additionally, no false positives were in these samples. The aforementioned interferents do not encompass all possible substances that could be encountered in exhaled breath in an operational context. This study did not consider the effects of substances originating from e-cigarettes, mouthwashes, medical conditions, or food residues. Temperature effects were also not systematically considered in this study.
The detection window of \(\hbox {N}_{2}\)O was shown both in vitro and ex vivo, and was found to be at least 60 min. The breathing simulator highlighted the extent to which the respiratory mechanics impact the longevity of \(\hbox {N}_{2}\)O in a human body. These parameters were effectively controlled in the in vitro model. Fleming et al used a similar approach using a breath emulator when evaluating a IR \(\hbox {CO}_{2}\)gas sensor in a non-clinical setting before using it in a medical environment33. Their work showed a sound agreement between measured, modeled and emulated \(\hbox {CO}_{2}\) concentrations. The breathing simulator used in our study showed that at least two time-scales are important in the detection of \(\hbox {N}_2\)O, namely a fast gas-exhalation process \(t_{1/2,1}=1-2.5\) min and a slower gas-redistribution process \(t_{1/2,2}=7-12\) min. After 20 min the initial concentration in the upper respiratory system of the lung simulator has already dropped by at least a factor of 300, depending on the ARR. However, the slower-gas distribution process allows a much longer window of detection of \(\hbox {N}_2\)O, vital for reliable detection by law enforcement. Also, the slower gas distribution process is to a large extent unaffected by the ARR. Still, the exact process of the gas-redistribution in the lung simulator remain unknown, only the associated timescales are resolved by the two compartment model.
In contrast to the breathing simulator results, in the ex vivo data, only a single much slower timescale \(t_{1/2}=29.0-30.6\) min was resolved. Even though in previous studies on pharmacokinetics of anesthetic gases two or three-compartment kinetics have been described, in the ex vivodata of our study these two processes could not be discerned34,35. This is most likely accounted to the fact that there was too much variability in the ex vivo data, resulting from the ad libitum component of the dosing and the lack of control over respiratory parameters due to working with conscious test subjects. In the clinical study, managing the three parameters of interest (\(V_t\), FRC and breathing time) proved to be complex due to ethical and practical concerns and this is reflected in the considerable degree of variance observed in the measurement outcomes. Since this variance was observed in both the single and double dosages, it is impossible to discern a difference between a single dose and a double dose from a solitary measurement taken at a single point in time. In realistic scenarios, a multitude of initial dosages are possible. Hence, this study demonstrates that a method to retrospectively calculate concentrations in the case of \(\hbox {N}_{2}\)O is practically unfeasible. In this study the high concentrations (>1,000 ppm) of \(\hbox {N}_{2}\)O at the first 20 min post-administration could not be measured. Altogether this study has shown that it is possible to detect and measure \(\hbox {N}_{2}\)O in exhaled breath of humans subjected to a representative recreational dose of \(\hbox {N}_{2}\)O using a balloon. \(\hbox {N}_{2}\)O remained detectable in exhaled breath for at least 60 min after inhalation at levels beyond 100 ppm. The detection limits (0 to 1,000 ppm) of the \(\hbox {N}_{2}\)O analyzer were therefore found to be suitable for law enforcement considering a police arrival time of approximately 15 min in 90% of the cases36. However, in order to study the ex vivo decay mechanics of \(\hbox {N}_{2}\)O we recommend extending the measurements well beyond one hour. Our findings suggest suggest that in order to fully map the \(\hbox {N}_{2}\)O concentration in an ex vivo setting, that during the first 20 min post-administration a detector with an upper limit of detection of at least 100,000 ppm is required. In this interval we recommend measuring the concentration at shorter time intervals \(< 1\) min. The knowledge gained from this research may help in providing the tools for \(\hbox {N}_{2}\)O detection in exhaled breath for forensic and law enforcement applications.
The following limitations should be taken into account for future research. The participants in this study were exclusively from a mid-twenties age cohort, which aligns with the typical demographic of occasional \(\hbox {N}_{2}\)O users37. However, this restricts the generalizability of the findings to a wider population. Additionally, the potential contamination of breath samples by both endogenously produced and exogenously introduced sources of \(\hbox {N}_{2}\)O remains a concern in real-world scenarios. While relevant interferents were included in this study, a considerable number of additional potential interferents were not examined. This limitation is particularly pertinent to alcohol in the ex vivo component of the study. Consequently, further research conducted under operationally representative conditions is recommended to enhance the robustness and applicability of these findings to real-world contexts and to statistically evaluate the false positive rate of a \(\hbox {N}_{2}\)O detector..
Materials and methods
Study design
The current study consisted of three parts. In the first part, the potential of ethanol, acetaldehyde, acetone, nitrogen dioxide, and exhaled tobacco smoke to interfere with \(\hbox {N}_{2}\)O measurements was investigated in synthetic air. In the second part a lung simulator was employed to simulate controlled respiratory conditions and validate nitrous oxide detection under reproducible and more representative settings. A lung simulator allows measuring the influence of tidal volume (\(V_t\)), functional residual capacity (FRC), and respiratory rate (RR) on \(\hbox {N}_{2}\)O depletion. The third part of the study consisted of a randomized, balanced, placebo-controlled, single-blind, three-period, crossover trial including 24 healthy, occasional \(\hbox {N}_{2}\)O users who produced breath samples before and up to 60 min after inhaling placebo, a single recreational dose of \(\hbox {N}_{2}\)O, or two subsequent recreational doses.
Method of detection of \(\hbox {N}_{2}\)O
A portable infrared (IR) based \(\hbox {N}_{2}\)O analyzer (Geotech G200, Coventry, UK) designed for \(\hbox {N}_{2}\)O detection in laboratory and hospital environments was acquired to measure \(\hbox {N}_{2}\)O concentrations in (exhaled) air (detection range 0 - 1000 ppm) and used in leak detection mode according to the manufacturers instructions. The detector was purchased pre-calibrated and certified and calibrated yearly during the experimental period. For the evaluating the performance of the detector against operational and the forensic relevant interferents \(\hbox {CO}_{2}\), acetaldehyde, acetone, \(\hbox {NO}_{2}\) and cigarette smoke. \(\hbox {N}_{2}\)O (1000 ppm in \(\hbox {N}_{2}\)) from a cylinder (Linde Gas Benelux, Schiedam, The Netherlands) was diluted in (humidified) air and mixed with these interferents.
First the accuracy and precision of the detector were verified by preparing and measuring known concentrations of \(\hbox {N}_{2}\)O 10, 25, 48 and 92 ppm against a background of ambient air using an in-house developed gas generation set-up. In this setup RH and concentrations of \(\hbox {N}_{2}\)O and \(\hbox {CO}_{2}\) can be controlled with EL-FLOW®mass flow controllers (MFC) (Bronkhorst, Veenendaal, The Netherlands). Secondly, the influence of interferents was investigated by measuring known concentrations of \(\hbox {N}_{2}\)O against more complex backgrounds. The interferents ethanol, acetaldehyde were acquired from Sigma-Aldrich and brought into vapour using a headspace calibrator vial. Nitrogen dioxide 99% (Linde Gas Benelux, Schiedam, The Netherlands) was diluted through a balloon using a gas tight syringe (Model 1025 TLL, Hamilton, Darmstadt, Germany).
The \(\hbox {N}_{2}\)O analyzer was challenged against the aformentioned interferent mixtures directly after preparation and mixing them for 30 s. These interferents were used as received without additional purification. Ethanol and acetaldehyde were injected in separate 1 L Tedlar airtight sample bags (Merck, Darmstadt, Germany) using a graduated 25.0 mL gas tight syringe until an equilibrium headspace concentration was reached. This was further diluted to a concentration of approximately 1000 ppm, and verified by measurement of the Tedlar bag by a MiniRae 3000 photo ionisation detector (Rae Benelux, Hoogstraten, Belgium) according to the manufacturer’s instruction. In the same fashion a Tedlar bag with a concentration of 1000 ppm nitrogen dioxide was prepared and measured with a MultiRae Lite gas detector (Rae Benelux, Hoogstraten, Belgium) equipped with a volatile organic compound sensor according to the manufacturer’s instructions. To these bags, either 100 ppm \(\hbox {N}_{2}\)O or 100 ppm pressurized air was added with the gas tight syringe. The volume of the Tedlar bag was consequently filled to the maximum volume of 1 L with ambient air and the prepared bags were measured in triplicate with the \(\hbox {N}_{2}\)O analyzer.. The effects of acetone on the detector were evaluated by forming a headspace by stirring a bottle of acetone and measuring the fumes directly afterwards.
An interferent mixture for tobacco smoke was prepared by collecting exhales of a cigarette smoker. The smoke (Marlboro mix, Philip Morris, Neuchâtel, Switzerland) was collected from the first exhale, directly after inhalation of the cigarette and stored in a 1 L Tedlar bag. The aforementioned procedure was repeated four times on different occasions. From the 1 L cigarette smoke filled Tedlar bag, 100 mL was removed using the gas tight syringe and 100 mL \(\hbox {N}_{2}\)O of a concentration of 1000 ppm was added to it yielding a mixture containing 100 ppm \(\hbox {N}_{2}\)O in 1 L partially diluted cigarette smoke. The same procedure was followed using 100 mL of pressurized air as a control. These experiments have been performed in duplicate. The accuracy and precision of the \(\hbox {N}_{2}\)O analyzer were further evaluated in the in-house developed gas generation set-up. The MFCs were used to dilute the concentration from the 1000 ppm \(\hbox {N}_{2}\)O cylinder in two stages to a minimum concentration of 10 ppm by mixing air of controlled humidity to the mixture. To assess the impact of humidity on the IR detector, generated concentrations were measured at levels of RH = 10% to RH = 95%. A schematic representation of the gas generation set-up is provided in the supplementary information (Figure S1).
In vitro \(\hbox {N}_{2}\)O detection using a breathing simulator
A breathing simulator consisting of a Dual Adult TTL mechanical test lung (Michigan Instruments, Grand Rapids, USA), a BSM - P00463 breath simulation module (Michigan Instruments, Grand Rapids, USA) and a AHSM test head (Michigan Instruments, Grand Rapids, USA) were used for in vitro breath simulations, as shown in Fig. 5.
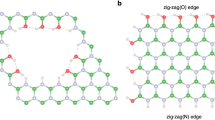
(a) Schematic setup of the Michigan Instruments Dual Adult Lung Simulator. The interior of the lung simulator consists of elastomer bellows. The lifting movement of the frame of the elastomer bellows generates a negative pressure in the lung, this allows a controlled mechanical ventilation with \(V_t\) =100–1800 mL at \(2-30\) breaths per minute. (b) The linear series two-compartment gas redistribution model. \(V_1\) represents the lumping of homogeneous alveoli, and \(V_2\) is the volume present in the trachea up to the upper respiratory tract. The initial \(\hbox {N}_2\)O concentration is assumed to be homogeneously distributed in \(V_1\) and \(V_2\) with concentration \(C_1(0)=C_2(0)=C_0\). After inhalation, the concentration of \(\hbox {N}_2\)O redistributes: the exhalation is controlled by a linear exhalation parameter \(\lambda _2\), the gas-exchange between the alveoli and the upper respiratory tract is modeled using \(\lambda _1\). The ambient concentration is assumed to be zero \(C_3=0\).
In vitroinhalation was achieved by an electric actuator that opens and closes a valve to let in pressurized air that mechanically lifts the lung thereby forcing in ambient air. The exhalation process of the breathing simulator was driven by the mechanical action of springs positioned bilaterally. To mimic the human respiratory system, we focused on three critical respiratory variables38,39,40, The respiratory rate was fixed at 15 breaths per minute in all experiments, equivalent to the average respiration rate of a human. Two tidal volumes (\(V_t\)) of 0.10 L and 0.20 L were fixed in the experiments. The functional residual capacity (FRC), the volume remaining in the lungs after passive exhalation, was varied between 0.4, 0.56, 0.60 and 0.9 L. Using the \(V_t\) and FRC we calculated the Air Refresh Ratio (ARR) by 1:
Based on human average \(V_t\) and FRC values, the ARR of an average human ranges between 0.11 and 0.14. However, in order to assess the longevity of \(\hbox {N}_2\)O in different representative settings, the \(\hbox {N}_2\)O longevity was tested at elevated ARR using the breathing simulator set-up. The different experimental conditions resulted in ARR’s of 0.10 (FRC = 0.90 L, \(V_t\) = 0.1 L), 0.15 (FRC = 0.56, \(V_t\) = 0.10), 0.20 (FRC = 0.40, \(V_t\) = 0.1) and 0.25 (FRC = 0.60, \(V_t\) = 0.20).
The \(\hbox {N}_2\)O was measured by in vitro coupling of the \(\hbox {N}_2\)O analyzer into the breathing simulator. A non-rebreather mask (Hudson RCI®, Morrisville, USA) was fitted with the inlet nozzle of the \(\hbox {N}_{2}\)O analyzer and connected directly in the mouth of the breathing simulator test head. The in vitro dosage was set via a balloon filled with the contents of a whipped cream charger (Cream whipper cartridge ± 8 g \(\hbox {N}_2\)O, 100%, Hendi Food service equipment, de Klomp, The Netherlands) as the \(\hbox {N}_2\)O source. The lung simulator was manually ventilated eight times after the connection to the \(\hbox {N}_{2}\)O filled balloon. The \(\hbox {N}_2\)O analyzer measured and recorded the concentration at intervals of 70 s.
To quantify the longevity of \(\hbox {N}_2\)O gas we employed a series two-compartment model of the respiratory system41,42,43. The two-compartment series model of the respiratory system assumes an uneven distribution of the \(\hbox {N}_2\)O gas in the lungs. The series gas redistribution model is made of two compartments, \(V_1\) and \(V_2\), connected in series, finally is it coupled to the ambient air. In Fig. 3 (b), a schematic representation is shown. The distal volume \(V_1\) represents the lumping of homogeneous alveoli, and \(V_2\)represents the volume present in the trachea up to the upper respiratory tract43. The distal volume is connected to the proximal volume by a gas exchange rate \(\lambda _1\). The proximal volume is coupled to the ambient air, this is controlled by the exhalation gas-exchange rate \(\lambda _2\). We assumed that in each compartment i the total mass of \(\hbox {N}_2\)O is conserved. Next, we applied the law of conservation of mass in compartment i; hence
where we used \(m_i = V_i C_i\) with volume \(V_i\) and \(\hbox {N}_2\)O mass concentration \(C_i\). \(\dot{m}_{i,in}\) is the inlet mass and \(\dot{m}_{i,out}\) is the outlet mass. The over-dot denotes the time derivative. Furthermore, we assumed that during a full breathing cycle the total volume of each compartment is unchanged. During each breathing cycle, a fixed volume \(\Delta V_i\) is exchanged between each compartment. This gas exchange process results in a mass exchange \(\Delta m_i = \Delta V_iC_{ij}\), with \(\Delta C_{ij}=(C_i-C_j)\) the concentration difference between compartments i and j. Hence, the mass balance reads
\(\lambda _{12} = \lambda _1\Delta V_1/V_1\), \(\lambda _{21} = \lambda _1\Delta V_1/V_2\) and \(\lambda _{23} = \lambda _{2}\Delta V_2/V_2\) are the gas-exchange rates corrected by the volumetric gas-exchange fraction in each compartment. At \(t=0\) we have \(C_1(0)=C_2(0) = C_0\) and \(C_3(t)=0\), i.e. the initial mass concentration \(\hbox {N}_2\)O in the alveoli and trachea is \(C_0\) and the ambient air \(\hbox {N}_2\)O concentration is zero. Equations 3a and 3b describe the change in concentration in the respiratory system after inhalation of \(\hbox {N}_2\)O gas. \(C_2(t)\) is the concentration in the exhaled air. The solution of the concentration of \(\hbox {N}_2\)O in the exhaled air is given by
A an B are the initial concentrations, \(\tilde{\lambda }_{1}\) and \(\tilde{\lambda }_{2}\) are the associated rate constants of the \(\hbox {N}_2\)O transport mechanism. Both rate constants are related to their half-life by \(t_{1/2,i}=\ln (2)/\tilde{\lambda _i}\). A similar solution can be found for \(C_1(t)\), however, this cannot experimentally be verified and is therefore not given. Each additional compartment is associated with an additional timescale; depending on the complexity of the lung simulator and respiratory system, the series gas redistribution model can be extended to n-compartments. Also, depending on the relative size of each timescale it is experimentally possible that only a single timescale is resolved. E.g., one starts a measurement at a time instant \(\tau\) that is in between the associated timescales of the experiment i.e. \(t^1_{1/2,2}\approx \tau \gg t^2_{1/2,1}\). In this case, the model is described by a single compartment and Equation 4 simplifies to
Note that A, B, \(\tilde{\lambda }_1\) and \(\tilde{\lambda }_2\) can be calculated by first principles, however, the exact exchange rates and the volume of each compartment are not measured. Hence, the exact values cannot be calculated beforehand.
Ex vivo detection of \(\hbox {N}_{2}\)O in exhaled breath
A randomized, placebo-controlled, single-blind, crossover trial was conducted in the operating theatres of the Leiden University Medical Center from September of 2021 to November 2023. Medical-ethical approval was obtained from the medical ethics committee of the academic hospital Maastricht, (Registration date: 28-01-2022, Trial Number: EudraCT 2021–003242-20) and the study protocol and procedures were executed in accordance with the declaration of Helsinki (1964) and its most recent amendments (2013). Informed consent was obtained from all participants, including additional consent from legal guardians where required, in accordance with the ethical standards of the Declaration of Helsinki. Twenty-four, healthy and occasional users of \(\hbox {N}_{2}\)O were passively recruited through poster and flyer advertisements spread throughout Leiden University and Maastricht University medical and social sciences campuses, as well as via social media. Participants were only allowed to take part in the study if (1) they were aged between 18 - 64 years, (2) indicated to have used \(\hbox {N}_{2}\)O recreationally before in a similar fashion as the administration method specified in the study protocol, (3) did not experience any negative effects associated with this previous use, and (4) were physically and psychologically in good health (as determined through a medical questionnaire and a clinical screening at the start of each study visit). The questions of the medical questionnaire are shown in the supplementary information, at section “medical questionnaire”. Candidates were excluded if they used \(\hbox {N}_{2}\)O recreationally on>10 separate occasions during the previous year or used >10 recreational doses of \(\hbox {N}_{2}\)O on a single occasion during the previous year. Furthermore, candidates were excluded when they consumed >21 alcoholic beverages weekly, regularly or recently used any other recreational of medicinal drug that might pose a health risk in combination with \(\hbox {N}_{2}\)O. This was controlled at the operating theatre with a \(\hbox {Surestep}^{tm}\) (Urine Test Drug Screen Cassette, Underdale, Australia) urine drug screening cassette at each study visit). A more detailed description of the inclusion and exclusion criteria is made available in the supplementary information section. A concise overview of the included participants’ characteristics is presented in table 1.
Participants took part in three experimental conditions and completed each these once: [placebo] two subsequent latex party balloons containing 4 L of Medical grade compressed air (ATC: V03AN05, Airapy, Linde Gas Benelux), [Single] one latex party balloon of air followed by one latex party balloon containing 4 L, 100% of medical grade \(\hbox {N}_{2}\)O (ATC: N01AX13, Niontix, Linde Gas Benelux), and [Double] two consecutive dosages of \(\hbox {N}_{2}\)O. Participants were randomly assigned to one of the six possible sequences in which the experimental conditions could be administered. Subsequent study visits were separated by at least one day. All conditions were performed in the operating theatre against a clear background i.e. 0 ppm \(\hbox {N}_{2}\)O and continuous ventilation.
Both the single and the double dosage conditions were based on an online survey conducted by Vinckenbosch et al. on recreational \(\hbox {N}_{2}\)O dosing and administration and its use in traffic16. All three dosage conditions consisted of inhalation of the content of two balloons with a 15-min rest interval in between the two subsequent balloons. The participants were seated in a chair with arm rests and instructed to inhale the content of the balloon, then exhale back into the balloon, and subsequently inhale from the balloon again, continuing this cycle. Upon completing five cycles of inhalation and exhalation, participants were asked to perform three deep inhalations and exhalations with the balloon removed from the mouth. Subsequently, participants were permitted to complete the next set of five inhalation and exhalation cycles from the balloon. This procedure continued until one of the following conditions was met: (1) 15 cycles of inhalation and exhalation were completed, (2) the participant was no longer able to inflate or hold the balloon, (3) the supervising physician decided to terminate the administration or testing to ensure the participant’s safety, or (4) the participant expressed a desire to discontinue inhalation. At the onset of inhalation, it was explicitly communicated to the participants that they could cease inhalation at any point, indicating that completion of the 15 cycles was not obligatory. Hence, the administration was conducted on an ad libitum basis, with no explicit instruction on depth or rate of inhalation.
A baseline value was determined by collecting the exhale of a participant in a 1 L Tedlar bag prior to the administration of the balloons containing either placebo or \(\hbox {N}_{2}\)O. Directly after the final dosage participants were asked to exhale in a 1 L Tedlar bag for analysis with the \(\hbox {N}_{2}\)O analyzer. This was repeated every 12 to 15 min until 60 min post inhalation, marking the end of the study visit. Initially, \(\hbox {N}_{2}\)O concentrations were measured after inhalation with the \(\hbox {N}_{2}\)O analyzer.
Data Availability
The data supporting the findings of this study are available from TNO and the Dutch National Police. Due to licensing restrictions, the data used in this study are not publicly accessible. For data requests, please contact the corresponding author. Access to the data will be granted upon reasonable request, pending approval from both TNO and the Dutch National Police.
References
Kaufman, E., Galili, D., Furer, R. & Steiner, J. Sensory experience induced by nitrous oxide analgesia. Anesthesia Progress 37, 282 (1990).
Sanders, R., Weimann, J., Maze, M., Warner, D. & Warner, M. Biologic Effects of Nitrous Oxide: A Mechanistic and Toxicologic Review. Anesthesiology 109, 707–722, https://doi.org/10.1097/ALN.0b013e3181870a17 (2008). https://pubs.asahq.org/anesthesiology/article-pdf/109/4/707/245231/0000542-200810000-00020.pdf.
Hopkins, P. M. Nitrous oxide: a unique drug of continuing importance for anaesthesia. Best Practice and Research Clinical Anaesthesiology 19, 381–389, https://doi.org/10.1016/j.bpa.2005.03.002 (2005). Renaissance of Inhalational Anaesthesia.
Savage, S. & Ma, D. The neurotoxicity of nitrous oxide: The facts and “putative’’ mechanisms. Brain Sciences 4, 73–90. https://doi.org/10.3390/brainsci4010073 (2014).
van Amsterdam, J., Nabben, T. & van den Brink, W. Recreational nitrous oxide use: Prevalence and risks. Regulatory Toxicology and Pharmacology 73, 790–796. https://doi.org/10.1016/j.yrtph.2015.10.017 (2015).
Randhawa, G. & Bodenham, A. The increasing recreational use of nitrous oxide: history revisited. British Journal of Anaesthesia 116, 321–324. https://doi.org/10.1093/bja/aev297 (2016).
Winstock, A. R. et al. Global drug survey 2019: Key findings report. (2020).
Donaldson, M., Donaldson, D. & Quarnstrom, F. C. Nitrous oxide-oxygen administration: When safety features no longer are safe. The Journal of the American Dental Association 143, 134–143 (2012).
Myles, P. S. et al. Avoidance of nitrous oxide for patients undergoing major surgery: a randomized controlled trial. The Journal of the American Society of Anesthesiologists 107, 221–231 (2007).
Xiang, Y. et al. Recreational nitrous oxide abuse: prevalence, neurotoxicity, and treatment. Neurotoxicity Research 39, 975–985 (2021).
Wagner, S. A., Clark, M. A., Wesche, D. L., Doedens, D. J. & Lloyd, A. Asphyxial deaths from the recreational use of nitrous oxide. Journal of forensic sciences 37, 1008–1015 (1992).
Back, S., Kroon, E., Colyer-Patel, K. & Cousijn, J. Does nitrous oxide addiction exist? an evaluation of the evidence for the presence and prevalence of substance use disorder symptoms in recreational nitrous oxide users. Addiction 119, 609–618. https://doi.org/10.1111/add.16380 (2024).
Campdesuner, V., Teklie, Y., Alkayali, T., Pierce, D. & George, J. Nitrous oxide-induced vitamin b12 deficiency resulting in myelopathy. Cureus 12 (2020).
Kaar, S. J. et al. Up: The rise of nitrous oxide abuse. an international survey of contemporary nitrous oxide use. Journal of psychopharmacology 30, 395–401 (2016).
Srichawla, B. & Kaur, K. Nitrous oxide/’whippets’ induced thoracic spinal cord myelopathy and cognitive decline with normal serum vitamin b12 (p7-12.002) (2022).
Vinckenbosch, F., Theunissen, E., Stelling, A., Goldenbeld, C. & Ramaekers, J. G. Recreational nitrous oxide dosing and administration and its use in traffic: An online survey. Journal of Drug Issues 00220426241233193 (2024).
Vinckenbosch, F. R. J. et al. The prevalence, risks, and detection of driving under the influence of nitrous oxide. WIREs Forensic Science n/a, e1508, https://doi.org/10.1002/wfs2.1508 (2023).
Moyes, . C.-J. P. L. J., D. Evaluation of driving skills after brief exposure to nitrous oxide. South African Medical Journal 56, 1000–1002 (1979).
Schleim, S. Substance use. In Mental Health and Enhancement: Substance Use and Its Social Implications, 93–125 (Springer, 2023).
Becker, D. E. & Rosenberg, M. Nitrous oxide and the inhalation anesthetics. Anesthesia progress 55, 124–131 (2008).
Potocka-Banas, B., Majdanik, S., Dutkiewicz, G., Borowiak, K. & Janus, T. Death caused by addictive inhalation of nitrous oxide. Human & experimental toxicology 30, 1875–1877 (2011).
Li, H.-Y., Lee, C.-S., Kim, D. H. & Lee, J.-H. Flexible room-temperature nh3 sensor for ultrasensitive, selective, and humidity-independent gas detection. ACS applied materials & interfaces 10, 27858–27867 (2018).
Yu, J., Wang, D., Tipparaju, V. V., Tsow, F. & Xian, X. Mitigation of humidity interference in colorimetric sensing of gases. ACS sensors 6, 303–320 (2020).
Qi, Q. et al. Electrical response of sm2o3-doped sno2 to c2h2 and effect of humidity interference. Sensors and Actuators B: Chemical 134, 36–42. https://doi.org/10.1016/j.snb.2008.04.011 (2008).
Wilkes, A. & Mapleson, W. Interference of volatile anaesthetics with infrared analysis of carbon dioxide and nitrous oxide tested in the dräger cicero em using sevoflurane. British journal of anaesthesia 76, 737–739 (1996).
Upton, R. The two-compartment recirculatory pharmacokinetic model-an introduction to recirculatory pharmacokinetic concepts. British Journal of Anaesthesia 92, 475–484 (2004).
Copot, D., Chevalier, A., Ionescu, C. M. & De Keyser, R. A two-compartment fractional derivative model for propofol diffusion in anesthesia. In 2013 IEEE International Conference on Control Applications (CCA), 264–269, https://doi.org/10.1109/CCA.2013.6662769 (2013).
Pleil, J. D. & Lindstrom, A. B. Measurement of volatile organic compounds in exhaled breath as collected in evacuated electropolished canisters. Journal of Chromatography B: Biomedical Sciences and Applications 665, 271–279. https://doi.org/10.1016/0378-4347(94)00545-G (1995).
London, J. W. & Bell, A. T. Infrared spectra of carbon monoxide, carbon dioxide, nitric oxide, nitrogen dioxide, nitrous oxide, and nitrogen adsorbed on copper oxide. journal of catalysis 31, 32–40 (1973).
Nasu, T., Ozaki, Y. & Sato, H. Study of changes in water structure and interactions among water, ch2, and coo? groups during water absorption in acrylic acid-based super absorbent polymers using raman spectroscopy. Spectrochimica Acta Part A: Molecular and Biomolecular Spectroscopy 250, 119305. https://doi.org/10.1016/j.saa.2020.119305 (2021).
Yablonskaya, O., Voeikov, V., Buravleva, E., Trofimov, A. & Novikov, K. Physicochemical effects of humid air treated with infrared radiation on aqueous solutions. Water 13, 1370 (2021).
Perfetti, T. & Rodgman, A. The complexity of tobacco and tobacco smoke. Beitrage zur Tabakforschung International/ Contributions to Tobacco Research 24, 215–232. https://doi.org/10.2478/cttr-2013-0902 (2011).
Fleming, L. et al. Breath emulator for simulation and modelling of expired tidal breath carbon dioxide characteristics. Computer Methods and Programs in Biomedicine 200, 105826. https://doi.org/10.1016/j.cmpb.2020.105826 (2021).
Ghoneim, M. & HAMME, M. V. Pharmacokinetics of thiopentone: effects of enflurane and nitrous oxide anaesthesia and surgery. BJA: British Journal of Anaesthesia 50, 1237–1242 (1978).
Copot, D., Chevalier, A., Ionescu, C. M. & De Keyser, R. A two-compartment fractional derivative model for propofol diffusion in anesthesia. In 2013 IEEE International Conference on Control Applications (CCA), 264–269 (IEEE, 2013).
Scholtens, A. & Helsloot, I. Een betere politie vraagt om andere sturing door burgemeesters. (2023).
van Laar, M. et al. Nationale drug monitor-kerncijfers en ontwikkelingen 2021 en 2022. (2023).
Neder, J. A., Andreoni, S., Castelo-Filho, A. & Nery, L. E. Reference values for lung function tests: I. static volumes. Brazilian journal of medical and biological research 32, 703–717 (1999).
Hallett, S., Toro, F. & Ashurst, J. Physiology, tidal volume. statpearls. treasure island (fl) (2024).
Chourpiliadis, C. & Bhardwaj, A. Physiology, Respiratory Rate (StatPearls Publishing, Treasure Island, FL, 2023).
Crooke, P., Head, J. & Marini, J. A general two-compartment model for mechanical ventilation. Mathematical and Computer Modelling 24, 1–18. https://doi.org/10.1016/0895-7177(96)00122-7 (1996).
Similowski, T. & Bates, J. Two-compartment modelling of respiratory system mechanics at low frequencies: gas redistribution or tissue rheology?. European Respiratory Journal 4, 353–358 (1991).
Tsoukias, N. M. & George, S. C. A two-compartment model of pulmonary nitric oxide exchange dynamics. Journal of Applied Physiology 85, 653–666 (1998).
Acknowledgements
This work was funded by the Dutch National Police under the KOP programme and financially supported by a research grant from Health Holland. We would like to extent our special thanks to the technical staff members Tomas van Groningen and Paola Donata of TNO for their assistance with the laboratory work. We are also grateful to the participants of the clinical part of our study who willingly took part, making this research possible. Finally, we highly acknowledge the contributions of Roxy van de Langkruis and Mette Rurup from the Dutch National Police who provided critical insights and discussions that greatly enhanced the quality of this work.
Author information
Authors and Affiliations
Contributions
D.D.J and F.V conceived the experiment(s), D.D.J, J.Z, D.T and F.V. conducted the experiment(s), D.D.J, M.S and J.B. analysed the results. D.D.J. and J.B. made the Figures. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interest:
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jiménez, D.D., Vinckenbosch, F., Busink, J. et al. Ex vivo detection of recreationally consumed nitrous oxide in exhaled breath. Sci Rep 15, 2901 (2025). https://doi.org/10.1038/s41598-025-86666-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-86666-9