Abstract
To compare the Model for End-Stage Liver Disease (MELD), MELD-XI, and Child-Turcotte-Pugh (CTP) scores for risk prediction in patients with cirrhosis undergoing heart transplantation. This study enrolled 66 consecutive patients (26 males; median age, 46 [18–68] years) with liver cirrhosis who underwent heart transplantation at our institution from 1994 to 2022. Potential preoperative outcome predictors and the preoperative MELD, MELD-XI, and CTP scores were calculated. The median follow-up duration was 45.2 months. The MELD (p = 0.01) and MELD-XI scores (p < 0.01) were significantly different between survivors and non-survivors. Cox regression analysis showed that high MELD (hazard ratio [HR] 1.07; 95% confidence interval [CI], 1.03–1.11; p < 0.01), MELD-XI (HR, 1.16; 95% CI, 1.06–1.21; p < 0.01), and CTP scores (HR, 1.43; 95% CI, 1.20–1.75; p = 0.01) were associated with the risk of all-cause mortality. Receiver operating characteristic curve analysis revealed that the optimal cut-off values of MELD, MELD-XI, and CTP scores were 12.2, 12.0, and 7.5, respectively (sensitivity: 69.2, 61.5, and 69.2%; specificity: 68.6, 60.0, and 62.9%, respectively) for all-cause mortality (area under the curve: 0.75, 0.69, and 0.73, respectively). Patients with advanced heart failure and liver cirrhosis have high mortality and morbidity rates after heart transplantation. However, these scoring systems can be used as risk stratification tools in patients with liver cirrhosis undergoing heart transplantation.
Research registration unique identifying number: Research Registry (UIN: resarchregistry10791).
Similar content being viewed by others
Introduction
Heart transplantation (HTx) is considered the only curative therapy for patients with end-stage heart failure (HF)1. Organ scarcity has a major adverse impact on the morbidity and mortality of patients awaiting HTx since extended waiting periods are associated with a higher risk of adverse outcomes2,3 Mechanical circulatory support systems have been shown to prevent irreversible end-organ dysfunction and death in patients awaiting HTx4,5,6. However, severe end-organ dysfunction occurrence prior to mechanical circulatory support is an established risk factor for poor outcomes after mechanical circulatory support and HTx7.
Significant liver dysfunction is common in patients with advanced HF. The extent of fibrosis or the presence of cirrhosis may help in post-transplant risk prognostication, especially in patients with restrictive cardiomyopathy and limited hepatic reserve, which is evidenced by persistent hepatic dysfunction despite relief from congestion. The predictive capabilities of hepatic congestion have been mainly considered in pediatric patients, as in the case of candidate patients for the Fontan circulation procedure8,9,10,11. However, organ scarcity continues to have a major adverse effect on morbidity and mortality in adult patients awaiting HTx, and alternative predictive systems might have to be considered. Therefore, this study aimed to compare the efficacy of scoring systems in predicting prognosis after HTx in adult patients with liver cirrhosis.
Methods
A total of 251 consecutive patients underwent HTx between January 1994 and June 2022 at the Severance Cardiovascular Hospital in Seoul, Republic of Korea. We included only patients with liver cirrhosis at the time of HTx in the study. Data on age, sex, diagnosis of heart disease, allograft ischemic time, cardiopulmonary bypass time, renal and liver function tests, liver fibroscan results before and after transplantation, and clinical outcomes were retrieved.
Ethics statements
The study was conducted in accordance with the principles of the Declaration of Helsinki and The International Society for Heart and Lung Transplantation ethics statement. This study was approved by the Ethics Committee/Institutional Review Board (IRB) of the Severance Cardiovascular Hospital, Republic of Korea (IRB number: 4-2018-0426), and the need for informed consent was waived due to the retrospective nature of the study. In addition, this study was registered at Research (UIN: researchregistry10791, www.researchregistry.com).
Diagnosis of liver cirrhosis
The diagnosis of cirrhosis was determined based on a combination of ultrasound sonography, abdominal computed tomography (CT), and fibroscan findings. These diagnostic modalities were used collectively to assess and confirm the presence of cirrhosis in the study population. Ultrasonographic findings of liver cirrhosis are characterized by a coarsened heterogeneous echo pattern, increased parenchymal echogenicity, and liver surface nodularity. The sonographic diagnosis could be made with a combination of these ultrasound criteria; coarse echo pattern, increased echogenicity, and nodularity. Histopathological evaluation of liver tissue biopsy samples has been the standard diagnostic approach, but risks associated with biopsy increase in patients with suspected liver fibrosis, making repeat testing difficult. In fact, the histological examination was not performed due to these practical challenges. To overcome these shortcomings of histologic and blood tests, fibroscan, which uses the elasticity change of liver tissue due to fiber accumulation, is used to further diagnose liver cirrhosis (Metavir classification)12.
Three score calculations
Laboratory results were obtained < 24 h before HTx, and the United Network for Organ Sharing (UNOS)-modified Model for End-Stage Liver Disease (MELD) scores were calculated using the following formula:
[MELD = 9.57 (logecreatinine) + 3.78 (logebilirubin) + 11.21 (logeInternational Normalized Ratio) + 6.43].
The standard MELD score was calculated using the formula described by Kamath et al.13 As per the UNOS modification, the variable lower limit was set at 1.0, and the creatinine upper limit was set at 4.0 mg/dL. Patients who received preoperative renal replacement therapy were assigned a creatinine of 4.0 mg/dL14.
MELD-XI was calculated as follows: [MELD-XI = 11.76 (logecreatinine) + 5.11 (logebilirubin) + 9.44], where total bilirubin and creatinine are considered equal to 1.0 if the raw laboratory values are < 1.0.
The Child–Turcotte–Pugh (CTP) scoring system was designed by Child and Turcotte in 196415 to aid in selecting patients who would benefit from elective surgery for portal decompression. Their original scoring system used five clinical and laboratory criteria to categorize patients: serum bilirubin, serum albumin, ascites, encephalopathy, and prothrombin time. We calculated the total points (range: 5–15) by adding a score for each parameter as a continuous variable; no categorical variables were used (grades A, B, or C) (Supplementary Table S1).
HTx and immunosuppression
All HTx procedures were performed via median sternotomy using previously described cardiopulmonary bypass techniques. Postoperative management in the intensive care unit was the same as that for routine patients undergoing cardiac surgery. All recipients received basiliximab (Simulect®) induction therapy, followed by triple maintenance immunosuppressive therapy [tacrolimus (Prograf®), mycophenolate mofetil (CellCept®), and corticosteroids (Solondo®)]. Patients received basiliximab induction (20 mg intravenous infusion) on postoperative days 0 and 4. Immediately after surgery, 500 mg of methylprednisolone was administered, which was reduced to 125 mg, 8 or 12 hourly for 2 days, along with tacrolimus and mycophenolate mofetil administration. On postoperative day 7, 1 mg/kg/day of prednisolone was administered and tapered to 5 mg/day weekly.
Statistical analyses
Clinical characteristics of the cohort are summarized as means (standard deviation), medians (interquartile range), or numbers (percentage), as appropriate. Baseline characteristics were compared between survivors and non-survivors using two-sample t-tests, Wilcoxon rank-sum tests, or chi-square tests.
For each outcome, patient characteristics and hemodynamic parameters were individually entered into a multivariable Cox proportional hazards regression model, including age, sex, body mass index, preoperative hemodynamic profile, left ventricular ejection fraction, creatinine, prior cardiac surgery, total albumin, total bilirubin, international normalized ratio, liver stiffness measurement score, Metavir classification, New York Heart Association class, extracorporeal membrane oxygenation insertion, ascites, and MELD, MELD-XI, and CTP scores.
The Kaplan–Meier method was used to generate survival curves according to liver cirrhosis. Cause-specific hazards were computed using Cox proportional hazard regression models for survival outcomes. Receiver operating characteristic (ROC) curves were used to assess specific cut-off values for the scoring systems. The Contal and O’quigley method and spline curve were also used to determine the cutoff point for the three predictive scoring systems for survival outcomes.
Statistical analysis was performed using a linear mixed-effects model (LMM) to analyze the overall changes in hematologic parameters. The significance level was set at p < 0.05. The IBM SPSS Statistics (version 25.0, IBM Corp., Armonk, NY, USA) and R packages (version 4.2.2) were used for all statistical analyses.
Results
Patients characteristics
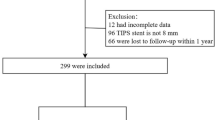
This study evaluated all data on patients who underwent HTx at the Severance Cardiovascular Hospital from January 1994 to June 2022. Among the 251 patients who underwent HTx, 213 (84.9%) were adults. Of the 84 patients (39.4%) with suspected liver cirrhosis who underwent HTx, 18 were excluded because of unconfirmed or incomplete diagnosis of liver cirrhosis (n = 16) or incomplete laboratory data (n = 2). Therefore, 66 patients who fulfilled the inclusion criteria with a confirmed preoperative diagnosis of liver cirrhosis (Metavir classification ≥ F4, Fibroscan score > 14.0 kPa, and ultrasound examination) before HTx were included in this retrospective study (Fig. 1).
Demographics and baseline data
The baseline patient characteristics are shown in Table 1. The mean patient age at surgery was 40.4 ± 14.0 years; 39.4% of the patients were male. The etiology of HF was dilated cardiomyopathy (57.4%), ischemic cardiomyopathy (14.7%), valvular disease (11.5%), and other causes, including congenital, restrictive, and infiltrative cardiomyopathy (16.4%). At the time of admission, 86.9% of the patients presented with New York Heart Association class III or IV, indicative of an advanced state of cardiac disease. Of the patients, 8.1% required preoperative extracorporeal membrane oxygenation for circulatory support. Most patients presented with low left ventricular ejection (28.93 ± 17.88%) and high right ventricular systolic pressure (48.7 ± 12.26 mmHg).
The intraoperative characteristics of the patients are presented in Table 2. All the patients underwent orthotopic heart transplantation using the bicaval technique. The mean time for aortic cross-clamp was 107.48 ± 20.21 min (interquartile range (IQR), 72–165), and the mean time for cardiopulmonary bypass was 181 ± 70.22 min (IQR, 95–250). The intensive care unit length of stay ranged from 3 to 45 days after HTx. There were 20 mortality cases, who were defined as the non-survivor group (sepsis, 10; major bleeding, 4; chronic graft rejection, 3; and sudden collapse events, 3).
Preoperative liver profiles, according to the distinct scoring systems, are shown in Table 1. The MELD, MELD-XI, and CTP scores were significantly higher in the non-survivor group than in the survivor group as precondition status for HTx.
Survival post-heart transplant
The mean and median follow-up periods were 4.78 ± 1.71 years and 4.22 years (1.3 − 10.1 years), respectively. Kaplan–Meier curves demonstrated significant differences in post-transplant survival according to preexisting liver cirrhosis (Fig. 2). In the early period after HTx, the difference between the two groups was statistically significant (p = 0.035). There were two early deaths. Patients with preexisting liver cirrhosis were found to be at risk for major bleeding (one gastrointestinal and one mediastinal) because of severe coagulopathy. The difference between the two groups observed up to one-year post-heart transplantation is sustained beyond one year, with the survival gap between the groups remaining consistent. This suggests that the initial survival disparity has a long-term effect on overall survival outcomes. Five-year survival rates were 79.8% and 72.4% in the non-liver cirrhosis and liver cirrhosis groups, respectively.
Relation between predictive scoring systems and post-transplant mortality
The Cox proportional hazards regression model included preoperative serological and hemodynamic profiles. The MELD, MELD-XI, and CTP scores remained independently and directly related to the incidence of all-cause death during the follow-up period (hazard ratio [HR] for MELD score, 1.07; MELD-XI score, 1.16; CTP score, 1.43). Table 3 shows a detailed risk analysis of patients undergoing HTx with preexisting liver cirrhosis.
Cut-off values of predictive scoring systems for post-transplant mortality
ROC curve analysis
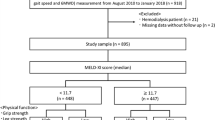
The cut-off values for overall post-transplant were 12.2 in the MELD score (AUC ± SD = 0.75 ± 0.08, p = 0.01, sensitivity: 69.2%, specificity: 68.6%), 12.0 in the MELD-XI score (AUC ± SD = 0.68 ± 0.09, p = 0.04, sensitivity: 61.5%, specificity: 60.0%), and 7.5 in the CTP score (AUC ± SD = 0.73 ± 0.09, p = 0.02, sensitivity: 69.2%, specificity: 62.9%) (Fig. 3A, Supplementary Table S2).
When these cut-off values were applied to patients, the high predictive scoring and overall survival showed a significant correlation in the three scoring systems (MELD score, p = 0.02; Fig. 3B; MELD-XI score, p = 0.02; Fig. 3C; and CTP score, p = 0.04; Fig. 3D).
Contal and O’quigley method analysis
When categorized into two groups based on the MELD score of 18.09, the difference in survival rate between the two groups was the largest (Supplementary Table S3) (p = 0.003). When the MELD-XI score was 17.65, the CTP score was 7, and the difference in survival rate was the largest between the two groups (p = 0.009 and 0.008, respectively).
Spline curve analysis
To assume a non-linear relationship between predictive score systems and mortality risk, the spline method was used for analysis. We presented Akaike Information Criterion (AIC) values and spline curves according to each degree of freedom (adjusting the degree of flexibility of the spline curve). In the case of the MELD, MELD-XI, and CTP scores, it had the smallest AIC value when the degree of freedom was 1 (Fig. 4A, B, and C, respectively). In other words, it seems appropriate to use the general Cox proportional hazards model without considering the spline method.
Spline curve analysis to determine a cut-off point of scoring systems in liver cirrhosis cohorts. (A) MELD score (Akaike information criterion; AIC, 149.19 in degree of freedom; df = 1, 151.10 in df = 2, 152.99 in df 3). (B) MELD-XI score (AIC 147.18 in df = 1, 148.85 in df = 2, 150.39 in df = 3). (C) CTP score (AIC 158.2 in df = 1, 159.51 in df = 2, 159.65 in df = 3).
Change in predictive scoring systems over time after HTx
The individual tree of the distinct scoring system was measured to evaluate time-related changes postoperatively and at follow-up. In all patients with preexisting liver cirrhosis, there were significant decreases in the MELD (R2 = 0.0912) and MELD-XI scores over time (R2 = 0.0637, Fig. 5). However, no significant difference was observed in the CTP scoring system (R2 = 0.1478). In the LMM analysis, we showed a trend of improvement in all three scoring systems after HTx compared with that preoperatively in the patients with liver cirrhosis. Furthermore, the MELD scoring system was reduced with the steepest slope.
The survivor group had significantly lower MELD, MELD-XI, and CTP scores than the non-survivor group, which were related to a lower incidence of perioperative complications. Furthermore, hemodynamic changes were correlated with trends in these scoring systems. Postoperatively, diastolic dysfunction improved in the survivor group, as shown by the reduced left atrial volume index and E/E’ (Supplementary Table S4).
Discussion
In the present study, approximately 30% of all pre-transplant patients with severe HF presented with liver cirrhosis, and it was observed that most patients with cirrhosis had abnormal liver findings on CT and abdominal sonography, which is consistent with previous reports on patients with HTx. Moreover, the present study found that distant scoring systems (MELD, MELD-XI, and CTP scores) can be useful predictors of mortality. Furthermore, the present study found that hemodynamic parameters improved after HTx, and it showed that the scoring systems improved over time.
The prognostic importance of abnormal liver function tests varies among previous studies16,17 However, the unfavorable predictive value of abnormal liver function tests has been described in patients with chronic HF or acute decompensated HF18. In a clinical trial, total bilirubin was among the most significant predictors of mortality in a large cohort of patients with chronic HF19. However, the study did not describe the prognostic value of the three scoring systems, which considers total bilirubin, in pre- and post-HTx patients. The present study was able to derive individual cut-off values for the three scoring systems and found that these systems were meaningful in predicting prognosis. Furthermore, our study investigated the changes in these scores over time and showed that the changes were consistent with the clinical results.
Evidence of significant liver dysfunction is frequently found in patients with advanced HF20. The etiology of liver dysfunction may be directly related to HF, manifesting as congestive hepatopathy, cardiac cirrhosis, or other liver diseases. Patients with liver dysfunction clinically present with jaundice, ascites, elevated bilirubin and transaminase levels, low albumin levels, and abnormal hepatic imaging21,22 Inadequate hepatic synthetic function with abnormal albumin levels, coagulation factors, and acute-phase proteins have been associated with a generally increased risk of bleeding and infection. Our study, as well as some other studies, have demonstrated that abnormalities in liver function correlate with poor outcomes in patients with HF. Furthermore, cardiohepatic dysfunction is associated with increased mortality. In the present study, the CTP score was the most sensitive predictor with the highest HR.
Additionally, patients with mild liver cirrhosis can better tolerate cardiac surgery than those with advanced liver cirrhosis (Child class B and C or Child score ≥ 8), in whom cardiac surgery with cardiopulmonary bypass is completely contraindicated23. Major postoperative complications are reported in > 80% of patients with advanced liver cirrhosis, with a reported in-hospital mortality rate of 50–100%24. However, the clinical outcomes of HTx in patients with liver cirrhosis have not been reported in the literature.
In the current study, the mortality rate was acceptable in these patients. Furthermore, liver cirrhosis had no significant effect on the survival rate 1 year postoperatively. Once HF was surgically corrected, systemic congestion was corrected, right-sided filling pressure decreased, hypoperfusion improved, and finally, the exacerbated liver function also improved (Graphical abstract). Thus, considering the global critical donor shortage, isolated HTx provides an alternative to combined heart and liver transplantation in patients with end-stage HF and liver cirrhosis. In addition, the cut-off values of the scoring systems derived from the present study could be a useful tool in pre-heart transplant evaluation.
Limitations
The cohort included in this retrospective analysis was not representative of the entire HTx population, and the study was limited by the small sample size and lack of preoperative liver biopsies. Direct data on portal venous pressure or hepatic venous pressure gradient (HVPG) values were not available, these variables were excluded from the risk factor analysis. In this study, functional liver abnormalities were reliably identified in high-risk patients using scoring systems. However, these parameters are dynamic and may change during HF therapy and disease progression.
Conclusions
Patients with advanced HF and liver cirrhosis are known to have high mortality and morbidity rates after HTx. However, these scoring systems (MELD, MELD-XI, and CTP scores) can be a useful tool for risk stratification in patients with liver cirrhosis undergoing HTx (Fig. 6).
Data availability
Data availabilityThe source data for all figures included in the manuscript are stored in Mendeley Data, V1, (doi: 10.17632/2z7682cn4m.1). If permissible, the dataset generated and/or analyzed during the current research will be made available upon request from the corresponding author. Limited access to certain clinical data generated in the current study is restricted due to the absence of prior authorization for external sharing of data from research subjects without explicit consent.
Abbreviations
- AIC:
-
Akaike Information Criterion
- CT:
-
Computed tomography
- CTP:
-
Child-Turcotte-Pugh scoring system
- HF:
-
Heart failure
- HR:
-
Hazard ratio
- HTx:
-
Heart transplantation
- IQR:
-
Interquartile range
- IRB:
-
Institutional Review Board
- LMM:
-
Linear mixed-effects model
- MELD:
-
Model for End-Stage Liver Disease
- ROC:
-
Receiver operating characteristic
- UNOS:
-
United Network for Organ Sharing
References
Hosenpud, J. D., Bennett, L. E., Keck, B. M., Boucek, M. M. & Novick, R. J. The Registry of the International Society for Heart and Lung Transplantation: 18th official report 2001. J. Heart Lung Transpl. 20 (8), 805–815 (2001).
Mulvihill Ms, Cox, M. L. et al. Decline of increased risk donor offers on waitlist survival in heart transplantation. J. Am. Coll. Cardiol. 72 (19), 2408–2409. https://doi.org/10.1016/j.jacc.2018.07.097 (2018).
Kobashigawa, J. et al. Report from the American Society of Transplantation Conference on donor heart selection in adult cardiac transplantation in the United States. Am. J. Transpl. 17 (10), 2559–2566 (2017).
Slaughter, M. S. Long-term continuous flow left ventricular assist device support and end-organ function: Prospects for destination therapy. J. Cardiothorac. Surg. 25 (4), 490–494 (2010).
Kamdar, F. et al. Effects of centrifugal, axial and pulsatile left ventricular assist device support on end-organ function in heart failure patients. J. Heart Lung Transpl. 28 (4), 352–359 (2009).
Kamdar, F. et al. Postop-cardiac transplant survival in the current era in patients receiving continuous-flow left ventricular assist devices. J. Thorac. Cardiovasc. Surg. 145 (2), 575–581 (2013).
Choksi, A. et al. Hepatic dysfunction and survival after heart transplantation: Application of the MELD scoring system for outcome prediction. J. Heart Lung Transpl. 31 (6), 591–600 (2012).
Gewilling, M. et al. The Fontan circulation: Who controls cardiac output? Interact. Cardiovasc. Thorac. Surg. 10 (3), 428–433 (2010).
Khairy, P. et al. Long-term survival, modes of death, and predictors of mortality in patients with Fontan surgery. Circulation 117 (1), 85–92 (2008).
Camposilvan, S. et al. Liver and cardiac function in the longterm after Fontan operation. Ann. Thorac. Surg. 86 (1), 177–182 (2008).
Kiesewetter, C. H. et al. Hepatic changes in the failing Fontan circulation. Heart 93 (5), 579–584 (2007).
Castera, L. et al. Prospective comparison of transient elastography, fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology 128 (2), 343–350 (2005).
Kamath, P. S., Kim, W. R. & Advanced Liver Disease Study Group. The model for end-stage liver disease. Hepatology 45 (3), 797–805 (2007).
Heuman, D. M., Mihas, A. A. & Habib, A. MELD-XI: a rational approach to sickest first liver transplantation in cirrhotic patients requiring anticoagulant therapy. Liv Transplant. 200;13(1):30–37.
Child, C. G. & Turcotte, J. G. Surgery and portal hypertension. Major Probl. Clin. Surg. 1, 1–85 (1964).
Batin, P. et al. The importance of abnormalities of liver function tests in predicting mortality in chronic heart failure. Eur. Heart J. 16 (11), 1613–1618 (1995).
Zannad, F. et al. Clinical profile, contemporary management and one-year mortality in patients with severe acute heart failure syndromes: The EFICA study. Eur. J. Heart Fail. 8 (7), 697–705 (2006).
Van Deursen, V. M. et al. Abnormal liver function in relation to hemodynamic profile in heart failure patients. J. Card Fail. 16 (1), 84–90 (2010).
Allen, L. A. et al. Liver function abnormalities and outcome in patients with chronic heart failure: Data from the Candesartan in heart failure: Assessment of reduction in mortality and morbidity (CHARM) program. Eur. J. Heart Fail. 11 (2), 170–177 (2009).
Xanthopoulos, A. et al. Heart failure and liver disease: Cardiohepatic interactions. JACC Heart Fail. 7 (2), 87–97 (2019).
Gelow, J. M. et al. Clinical predictors of hepatic fibrosis in chronic advanced heart failure. Circ. Heart Fail. 3 (1), 59–64 (2010).
Samsky, M. D. et al. Cardiohepatic interactions in heart failure: An overview and clinical implications. J. Am. Coll. Cardiol. 61 (24), 2397–2405 (2013).
Costanzo, M. R. et al. Selection and treatment of candidates for heart transplantation. A statement for health professionals from the committee on heart failure and cardiac transplantation of the council on clinical cardiology, American Heart Association. Circulation 92 (12), 3593–3612 (1995).
Hsu, R. B. et al. Heart transplantation in patients with liver cirrhosis. Eur. J. Cardiothorac. Surg. 34 (2), 307–312 (2008).
Author information
Authors and Affiliations
Contributions
Hyo-Hyun Kim; Conceptualization, Investigation, Writing- original draft, Writing-review & editing. Visualization.Young-Nam Youn; Conceptualization, Project administration, Supervision, Writing-review & editing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, HH., Youn, YN. Predictive scoring systems for mortality in heart transplant patients with liver cirrhosis. Sci Rep 15, 12663 (2025). https://doi.org/10.1038/s41598-025-87675-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87675-4