Abstract
Studies investigating the relationship between exposure to air pollutants during pregnancy and foetal growth restriction (FGR) in women who conceive by in vitro fertilisation (IVF) are lacking. The objective was to investigate the effect of air pollutant exposure in pregnancy on FGR in pregnant women who conceive by IVF. We included pregnant women who conceived by IVF and delivered healthy singleton babies in Guangzhou from October 2018 to September 2023. We also collected data on air pollutant concentrations in Guangzhou during the same period. We analysed the impact of air pollution exposure during pregnancy on FGR. After adjusting for confounders, our analysis showed that in the first trimester, high concentrations of PM10 and NO2 in the fourth quartile significantly increased the risk of FGR. Specifically, the odds ratios were 6.430 (95% confidence interval [CI]: 1.035–39.96) for PM10 and 10.73 (95% CI: 1.230–93.48) for NO2. In the second trimester, exposure to PM2.5, PM10, and NO2 was associated with an increased risk of FGR. In addition, subgroup analyses showed that exposure to NO2 during pregnancy increased the risk of FGR in women aged 35 years and older. The results of this cross-sectional study suggest that exposure to PM2.5, PM10, and NO2 in pregnant women who conceive by IVF is associated with the occurrence of FGR.
Similar content being viewed by others
Introduction
Foetal growth restriction (FGR) is a relatively common complication of pregnancy. The occurrence of FGR is associated with an increased risk of perinatal complications, increased infant morbidity and mortality1 and respiratory, cardiovascular and neurological problems after birth2,3. A retrospective study by Shankar et al.4 found that 50.8% of unexplained stillbirths were associated with identifiable factors, of which 41.5% were attributable to FGR. Therefore, FGR should be considered highly important by doctors and expectant mothers.
Although many factors can impact FGR risk, including maternal characteristics, lifestyle, and pregnancy complications, the relationship between exposure to air pollutants and FGR risk has not been determined5,6,7. Studies have shown that fine particulate matter (PM2.5) can enter the bloodstream during pregnancy and affect foetal growth8,9, leading to low birth weight, premature birth and reduced head circumference10,11. Fu et al.12 reported that exposure of pregnant women to high levels of nitrogen dioxide (NO2) and PM2.5 during pregnancy may affect infant head circumference and length. A study conducted in southern Sweden revealed that for every 10 µg/m3 increase in the NOx concentration, birth weight decreased by 9 g13. A retrospective cohort study conducted in Australia revealed that NO2 exposure increases the risk of FGR by 31% (95% confidence interval [CI]: 1.07–1.60)14. However, some studies have shown no association between exposure to air pollutants and FGR risk. Bobak M. found no association between intrauterine growth retardation (IUGR) and exposure to air pollutants in an analysis of data from 108,173 singleton births in the Czech Republic6. Dejmek et al.15 also found no correlation between IUGR and exposure to particulate matter, sulphur dioxide (SO2), NOx, or ozone (O3). A study carried out in Norway also showed that NO2, PM10 (particles with an aerodynamic equivalent diameter ≤ 10 μm) and O3 had no significant effect on foetal weight or length16. Therefore, the relationship between air pollution exposure and FGR risk may vary according to geographical location, living standards, etc., and further research on the relationship between exposure to air pollutants and FGR risk in different regions is needed.
In recent years, the use of assisted reproductive technologies, particularly in vitro fertilisation (IVF), has increased, making it essential to understand the specific risks associated with these pregnancies. Despite the growing number of pregnancies achieved through IVF, little is known about the specific effects of exposure to air pollutants on the risk of FGR in this population. Preliminary evidence suggests that air pollution may have a more pronounced effect on pregnancies achieved through assisted reproductive technologies17,18, but the underlying mechanisms of these associations remain unclear.
This study aims to fill the gap by investigating the impact of exposure to air pollutants during pregnancy on the risk of FGR in pregnancies achieved through IVF. It will provide a basis for the development of targeted health policies and interventions by analysing the effects of air pollutants on the risk of FGR in pregnancies achieved through assisted reproductive technologies.
Methods
Participant selection
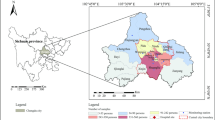
In this study, pregnant women who conceived by IVF and delivered in the hospital from October 2018 to September 2023 were enrolled as recruited participants using the electronic medical record information management system of Guangzhou Huadu District Maternal and Child Health Hospital. By querying the hospital’s electronic medical records, it is possible to obtain relevant information about research participants, such as age, occupation, ethnicity, residential address, implantation time, delivery date, and clinical diagnoses. The diagnosis of diseases in electronic medical records is strictly classified according to ICD-10 codes, this study included pregnant women with a diagnosis of FGR (ICD-O36.5) as the disease group, excluding pregnant women with nonlocal residential addresses and hospitals at which the embryo was transferred, those without specific implantation dates, those with twin pregnancies, gestation less than 27 weeks, and others (Fig. 1). This study was approved by the Ethics Committee of the Maternal and Children Health Care Hospital of Huadu (no. 2024-001), which waived the requirement for informed consent since the study used de-identified information. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Assessment of air pollution concentrations
All those who participated in this study lived in Guangzhou. We obtained real-time concentrations of air pollutants in Guangzhou City from the National Urban Air Quality Real-Time Dissemination Platform of the China National Environmental Monitoring Centre (a pre-processed database is available at https://quotsoft.net/air, which is updated daily). In this study, we used air pollutant concentrations in Guangzhou as a proxy for individual exposure data, the time-varying average concentration method was used to estimate the mean exposure of the participants to air pollutants (PM2.5, PM10, NO2, O3) during different trimesters using real-time air pollutant concentrations in Guangzhou, based on the date of birth and the date of embryo transfer. Based on previous studies19,20, we calculated the average exposure concentration during three different periods: the 1st trimester (weeks 1 to 12 of pregnancy), the 2nd trimester (weeks 13 to 27) and the 3rd trimester (weeks 28 to delivery).
Covariates and outcomes
Covariates were established based on published studies5,13,21,22 and information available in the hospital electronic medical record system. The covariates identified in the present study included age, occupation, ethnicity, pregnancy type, embryo type, eclampsia, anaemia, infant gender, and air pollution.
SO2 concentrations were obtained from the same website as PM2.5, PM10, NO2, and O3. Missing values for all air pollutant concentrations were filled in using monthly averages published by the Guangzhou Municipal Bureau of Ecology and Environment. The number of days of pregnancy varies slightly depending on the type of embryo. When transferring cleavage-stage embryo, the total number of gestation days needs to be reduced by 12 days, and when transferring blastocyst, the total number of gestation days needs to be reduced by 14 days.
FGR was diagnosed based on a clinical diagnosis obtained from the electronic medical records system. Doctors use the diagnostic criteria of the Royal College of Obstetricians and Gynaecologists for FGR23 and diagnose FGR when the estimated foetal weight is less than the 10th percentile for the same gestational age (SGA).
Statistical analysis
The descriptive characteristics of the study participants were analysed using nonparametric tests for continuous variables and χ2 tests for categorical variables. We constructed a binary variable for FGR as the dependent variable, with the control group, air pollutants, age, occupation, pregnancy type, embryo type, eclampsia, anaemia, infant gender and SO2 as independent variables. To reduce the influence of baseline differences in demographic and clinical characteristics on the results, we used propensity score matching (PSM) to match the control group to the disease group in accordance with the suggestion of Lonjon et al.24. A logistic regression model was used to obtain the propensity score representing the likelihood of FGR. Age, occupation, ethnicity, pregnancy type, embryo type, anaemia and infant sex were used as matching factors. We then performed 1:2 greedy nearest neighbour matching with a calliper of 0.2 to match controls with normal foetal growth and development. To further assess the robustness of our findings, we conducted a sensitivity analysis using different matching ratios (1:1, 1:2, 1:3, and 1:4). After matching, conditional logit regression was used to calculate the odds ratio (OR) and 95% CI to analyse the relationship between exposure to air pollutants and FGR risk, adjusting for potential confounders. These confounders included age, occupation, pregnancy type, embryo type, anaemia, infant gender and SO2. In addition, we performed subgroup analyses by age to assess the association between exposure to PM2.5, PM10, NO2 and O3 during the entire gestation period and the risk of FGR in different age groups, in order to identify specific high-risk populations.
In our study, we performed PSM analysis using R version 4.2.2 and the MatchIt package and regression analysis using Stata 16.0 software. p-value < 0.05 was considered to indicate statistical significance.
Results
Characteristics of the baseline
A total of 1,907 pregnant women who underwent IVF were identified from the electronic medical records system. After excluding ineligible participants, 1,433 patients were enrolled in the study, including 30 in the FGR group and 1,429 in the control group. There were significant differences between the control group and the FGR group before PSM matching for eclampsia, gestational diabetes mellitus, hypertension in pregnancy and O3. After performing 1:2 PSM, the p-value of the baseline covariates have increased after matching, indicating that PSM effectively improved the balance of covariates between the control group and the FGR group (Table 1). As shown in Figure S1, it can be observed that the PSM sensitivity analysis using a 1:2 matching ratio demonstrates relatively stable and reasonable effect sizes for different pollutants.
Relationship between exposure to air pollutants and FGR risk
Table 2 shows the relationship between each quartile of air pollution exposure in the first trimester and FGR risk. Using the first quartile as the reference value and adjusting for covariates, we observed that exposure to both PM10 and NO2 concentrations in the fourth quartile significantly increased the risk of FGR compared to the first quartile, with OR of 6.430 (95% CI: 1.035–39.96) for PM10 and 10.73 (95% CI: 1.230–93.48) for NO2, respectively. O3 exposure in the third and fourth quartiles compared to the first quartile was negatively associated with FGR, with OR and 95% CI of 0.071 (0.010–0.485) and 0.165 (0.029–0.943), respectively.
After adjusting for covariates, in the second trimester, our analysis showed a significant escalation in the risk of FGR for pregnant individuals exposed to PM2.5 and NO2 concentrations within the fourth quartile compared to the first quartile. Additionally, exposure to PM10 concentrations in both the second and fourth quartiles compared to the first quartile was associated with an increased risk of FGR, with OR of 5.142 (95% CI: 1.013–26.11) and 21.76 (95% CI: 2.602-182.00), respectively (Table 3). In the third trimester there is no significant association between exposure to PM10, NO2 and O3 and FGR. However, there is a negative association between PM2.5 exposure in the third quartile compared to the first quartile and FGR (Table 4).
Subgroup analysis after PSM
Figure 2. The association between exposure to air pollution during pregnancy and FGR in pregnant women of different ages. Adjusted for age, occupation, pregnancy type, embryo type, anaemia, infant gender and SO2. FGR Foetal growth restriction, OR odds ratio, 95% CI 95% confidence interval, PM2.5 particulate matter with aerodynamic diameter of ≤ 2.5 μm, PM10 particles matter with an aerodynamic equivalent diameter ≤ 10 μm, NO2 nitrogen dioxide, O3 ozone.
Discussion
In this cross-sectional study, we investigated the association between PM2.5, PM10, NO2, O3 exposure and FGR risk in Guangzhou, Guangdong, China. After baseline matching of the study participants at a 1:2 ratio via PSM, we found that exposure to PM10 and NO2 during the first trimester and exposure to PM2.5, PM10 and NO2 during the second trimester were associated with an increased risk of FGR. Specifically, exposure to NO2 during pregnancy was found to increase the risk of FGR in women aged ≥ 35 years. This study indicating a dose‒response relationship between adverse effects of air pollution and FGR.
There has been some controversy about the relationship between the concentration of air pollutants and FGR. PM2.5 exposure in entire pregnancy was strongly associated with smaller gestational age (OR = 1.15, 95%CI: 1.00-1.31) in pregnant women at Rhode Island’s Women and Infants Hospital between 2001 and 2012 25, which is closely linked to FGR26. A Utah-based study of 51,086 mothers found that exposure to PM10 and NO2 in the first, second and third trimester of pregnancy associated with increased risk of FGR27. In addition, a study on the impact of exposure to air pollutants on foetal growth revealed that exposure to PM10 and NO2 during the third trimester was negatively associated with head circumference at birth, and NO2 exposure was negatively associated with birth length in the first, second, and third trimesters28. A previous French study showed that a 10 µg/m3 increase in NO2 exposure during the second trimester, the risk of FGR increased by 55% (95% CI: 1.06–2.27), but exposure to NO2 during early and third trimester does not increase the risk of29. However, a study conducted in Seoul, South Korea, of 824,011 singleton full-term newborns showed that the correlation between PM2.5 and PM10 exposure and FGR was close to zero30. A study in Nigeria revealed that PM2.5 exposure had no effect on foetal growth31. In this study, we found that exposure to PM10 and NO2 during the first trimester was positively correlated with an increased risk of FGR. Furthermore, exposure to PM2.5, PM10, and NO2 in the second trimester was also associated with a heightened risk of FGR. However, no significant differences were observed in the relationship between air pollutant exposure and FGR during the third trimester pregnancy. The difference in results may be due to the different geographical setting and occurrence of air pollution exposure during pregnancy in our study compared with studies in Rhode Island, Utah, Seoul and Nigeria. In addition, our study found significant effects mainly in early and mid-pregnancy, which differs from other studies that reported effects throughout pregnancy. This may be because early and mid-pregnancy are critical periods of foetal development when key organs and systems are being formed, making the foetus more sensitive to environmental factors. In addition, during these early stages, the functions and barriers of the placenta are not fully developed, potentially allowing more pollutants to affect the foetus. Finally, differences in sample size, population characteristics and study design (including measurement methods and data analysis) may also lead to inconsistent results.
Studies have showed that air pollutants can cause histopathological changes in the placenta32, increased oxidative stress33, and placental DNA methylation34, leading to impaired placental function, which in turn allows air pollutants to affect foetal growth and development through the placenta35,36. The results of the Early Autism Risk Longitudinal Investigation from the Infinium HumanMethylation450k platform for 133 placenta platforms showed that prenatal exposure to O3 can cause placental methylation and affect foetal growth and development37. A study conducted in Shanghai from 2015 to 2018 found that exposure to PM2.5 and O3 during pregnancy reduced foetal femur length and head circumference at 36 weeks’ gestation38, this finding suggests that exposure to O3 during pregnancy may have effects on foetal development. However, these previous findings are not entirely consistent with the results of this study. This study found a negative association between O3 exposure in the first trimester and FGR. Additionally, there was a negative association between PM2.5 exposure in the third trimester and FGR. This finding is consistent with a study conducted in Canada from 1985 to 2000, which examined the relationship between air pollutants and intrauterine growth restriction in single live births at term and found that exposure to O3 in first, second and third trimester was negatively correlated with FGR39. In addition, a previous study by Wang et al.20 from 2015 to 2017 in Guangzhou also found a negative association between PM2.5 exposure in the third trimester and SGR, which is now synonymous with intrauterine or FGR40. Inconsistencies in research findings on the relationship between PM2.5 and O3 exposure and FGR may be due to several factors, including differences in the methods used to assess exposure in different studies; differences in the health status, lifestyle and regional characteristics of the study populations; and the influence of regional air pollution levels and other environmental factors, such as climate and lifestyle habits. Since it is logically implausible that PM2.5 and O3 exposure would reduce the risk of FGR, future steps should focus on increasing the sample size to minimise bias and conducting comparative studies in different regions and environmental settings to validate the relationship between PM2.5 and O3 exposure and FGR.
In this study, we also analysed the effect of exposure to air pollution during pregnancy on FGR risk among pregnant women of different ages. The results showed that exposure to NO2 during pregnancy significantly increased the risk of FGR in pregnant women aged ≥ 35 years. This may be related to the gradual decline in the physical functions (such as placental function and the immune system) of pregnant women with age, which increases their vulnerability to external environmental factors. On the other hand, their older age has caused certain changes in their immune system, resulting in increased sensitivity to air pollutants and greater vulnerability to the adverse effects of air pollutants.
Our study has several advantages. First, we used the PSM method to process the data. PSM has unique practicality and simplicity41 and eliminates confounding bias in the cohort when randomization methods cannot be used. Second, we used the implantation date of pregnant women who conceived by IVF as the starting time for evaluating air pollutant exposure, which more accurately reflects the actual start time of pregnancy than the last menstrual period and can more accurately reflect the exposure of pregnant women to air pollutants. This study has several limitations. First, we collected data on potential confounders by reviewing electronic medical records, however, several important factors (such as smoking42 and drinking status43) that may affect the relationship between exposure to air pollutants and FGR risk were not included in the analysis, which may bias the results. Second, we used the address registered in the hospital electronic medical records information system at the time of delivery to assess the pregnant women’s exposure to air pollutants. The lack of potential relocation information for the study participants during the study period may have led to inaccurate assessments of air pollutant exposure. Finally, exposure to air pollutants can cause oxidative stress in pregnant women44, while antioxidants such as tocopherols, ascorbic acid and carotenoids in food are natural antioxidants that can ameliorate oxidative stress in the body45. In this study, we did not collect information on the participants’ diets and were unable to determine the effect of dietary factors on the results. Dietary factors during pregnancy should be considered in future studies to better determine the effects of exposure to air pollution on FGR risk.
Conclusion
The findings confirmed that exposure to PM10 and NO2 during the first trimester and to PM2.5, PM10 and NO2 during the second trimester may increase the risk of FGR in pregnant women undergoing IVF. This risk is particularly pronounced in women aged ≥ 35 years exposed to NO2 during pregnancy. Although this study has several limitations, the research showed that exposure to air pollution in the first and second trimester can increase the risk of FGR, which is not only associated with a higher risk of stillbirth and neonatal mortality46,47, but also increases the risk of metabolic syndrome in adulthood48,49. Considering the health implications of FGR, the actual consequences of air pollution exposure may be more severe than currently documented, making this an important area for further investigation.
Data availability
The data that support the findings of this study are available from correspondence author but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of correspondence author.
References
Kesavan, K. et al. Intrauterine growth restriction: postnatal monitoring and outcomes. Pediatr. Clin. North. Am. 66 (2), 403–423 (2019).
Malhotra, A. et al. Neonatal morbidities of fetal growth restriction: pathophysiology and impact. Front. Endocrinol. (Lausanne). 10, 55 (2019).
Crispi, F. et al. Intrauterine growth restriction and later cardiovascular function. Early Hum. Dev. 126, 23–27 (2018).
Shankar, M. et al. Assessment of stillbirth risk and associated risk factors in a tertiary hospital. J. Obstet. Gynaecol. 22 (1), 34–38 (2003).
Maisonet, M. et al. A review of the literature on the effects of ambient air pollution on fetal growth. Environ. Res. 95 (1), 106–115 (2004).
Bobak, M. Outdoor air pollution, low birth weight, and prematurity. Environ. Health Perspect. 108 (2), 173–176 (2000).
Dejmek, J. et al. The impact of polycyclic aromatic hydrocarbons and fine particles on pregnancy outcome. Environ. Health Perspect. 108 (12), 1159–1164 (2000).
Bove, H. et al. Ambient black carbon particles reach the fetal side of human placenta. Nat. Commun. 10 (1), 3866 (2019).
Liu, N. M. et al. Evidence for the presence of air pollution nanoparticles in placental tissue cells. Sci. Total Environ. 751, 142235 (2021).
Ghazi, T. et al. Prenatal air Pollution exposure and placental DNA methylation changes: implications on fetal development and Future Disease susceptibility. Cells 10(11) (2021).
Bell, M. L. et al. Ambient air pollution and low birth weight in Connecticut and Massachusetts. Environ. Health Perspect. 115 (7), 1118–1124 (2007).
Fu, L. et al. The associations of air pollution exposure during pregnancy with fetal growth and anthropometric measurements at birth: a systematic review and meta-analysis. Environ. Sci. Pollut Res. Int. 26 (20), 20137–20147 (2019).
Malmqvist, E. et al. Fetal growth and air pollution - A study on ultrasound and birth measures. Environ. Res. 152, 73–80 (2017).
Pereira, G. et al. Locally derived traffic-related air pollution and fetal growth restriction: a retrospective cohort study. Occup. Environ. Med. 69 (11), 815–822 (2012).
Dejmek, J. et al. Fetal growth and maternal exposure to particulate matter during pregnancy. Environ. Health Perspect. 107 (6), 475–480 (1999).
Ling, X. The effect of ambient air pollution on birth outcomes in Norway. BMC Public. Health. 23 (1), 2248 (2023).
Liu, J. et al. Associations between ambient air pollution and IVF outcomes in a heavily polluted city in China. Reprod. Biomed. Online. 44 (1), 49–62 (2022).
Wu, S. et al. Interaction of air pollution and meteorological factors on IVF outcomes: a multicenter study in China. Ecotoxicol. Environ. Saf. 259, 115015 (2023).
Wan, Z. et al. Effect of fine particulate matter exposure on gestational diabetes mellitus risk: a retrospective cohort study. Eur. J. Public. Health (2024).
Wang, Q. et al. Seasonal analyses of the association between prenatal ambient air pollution exposure and birth weight for gestational age in Guangzhou, China. Sci. Total Environ. 649, 526–534 (2019).
Jakpor, O. et al. Term birthweight and critical windows of prenatal exposure to average meteorological conditions and meteorological variability. Environ. Int. 142, 105847 (2020).
Shi, W. et al. Association between ambient air pollution and pregnancy outcomes in patients undergoing in vitro fertilization in Shanghai, China: a retrospective cohort study. Environ. Int. 148, 106377 (2021).
Royal College of Obstetricians and Gynaecologists. Green-top guideline 31: the investigation and management othe small-for-gestational-age Fetus. Royal Coll. Obstetricians Gynaecologists (2014).
Lonjon, G. et al. Potential pitfalls of Reporting and Bias in Observational Studies with Propensity score analysis assessing a Surgical Procedure: a methodological systematic review. Ann. Surg. 265 (5), 901–909 (2017).
Kingsley, S. L. et al. Maternal ambient air pollution, preterm birth and markers of fetal growth in Rhode Island: results of a hospital-based linkage study. J. Epidemiol. Commun. Health. 71 (12), 1131–1136 (2017).
Melamed, N. et al. Customized birth-weight centiles and placenta-related fetal growth restriction. Ultrasound Obstet. Gynecology: Official J. Int. Soc. Ultrasound Obstet. Gynecol. 57 (3), 409–416 (2021).
Nobles, C. J. et al. Ambient air pollution and fetal growth restriction: physician diagnosis of fetal growth restriction versus population-based small-for-gestational age. Sci. Total Environ. 650 (Pt 2), 2641–2647 (2019).
Lamichhane, D. K. et al. Air pollution exposure during pregnancy and ultrasound and birth measures of fetal growth: a prospective cohort study in Korea. Sci. Total Environ. 619–620, 834–841 (2018).
Mariet, A. S. et al. Multiple pregnancies and air pollution in moderately polluted cities: is there an association between air pollution and fetal growth? Environ. Int. 121 (Pt 1), 890–897 (2018).
Choe, S. A. et al. Association between ambient particulate matter concentration and fetal growth restriction stratified by maternal employment. BMC Pregnancy Childbirth. 19 (1), 246 (2019).
Dutta, A. et al. Household air pollution, ultrasound measurement, fetal biometric parameters and intrauterine growth restriction. Environ. Health: Global Access. Sci. Source. 20 (1), 74 (2021).
Wylie, B. J. et al. Placental Pathology Associated with Household Air Pollution in a cohort of pregnant women from Dar Es Salaam, Tanzania. Environ. Health Perspect. 125 (1), 134–140 (2017).
Saenen, N. D. et al. Placental nitrosative stress and exposure to Ambient Air Pollution during Gestation: a Population Study. Am. J. Epidemiol. 184 (6), 442–449 (2016).
Zhao, Y. et al. Prenatal fine particulate matter exposure, placental DNA methylation changes, and fetal growth. Environ. Int. 147, 106313 (2021).
Bongaerts, E. et al. Maternal exposure to ambient black carbon particles and their presence in maternal and fetal circulation and organs: an analysis of two independent population-based observational studies. Lancet Planet. Health. 6 (10), e804–e811 (2022).
Saenen, N. D. et al. In Utero Fine Particle Air Pollution and placental expression of genes in the brain-derived neurotrophic factor signaling pathway: an ENVIRONAGE Birth Cohort Study. Environ. Health Perspect. 123 (8), 834–840 (2015).
Ladd-Acosta, C. et al. Epigenetic marks of prenatal air pollution exposure found in multiple tissues relevant for child health. Environ. Int. 126, 363–376 (2019).
Shao, X. et al. Prenatal exposure to ambient air multi-pollutants significantly impairs intrauterine fetal development trajectory. Ecotoxicol. Environ. Saf. 201, 110726 (2020).
Liu, S. et al. Association between maternal exposure to ambient air pollutants during pregnancy and fetal growth restriction. J. Expo. Sci. Environ. Epidemiol. 17 (5), 426–432 (2007).
Iams, J. D. Small for gestational age (SGA) and fetal growth restriction (FGR). Am. J. Obstet. Gynecol. 202 (6), 513 (2010).
Kane, L. T. et al. Propensity score matching: a statistical method. Clin. Spine Surg. 33 (3), 120–122 (2020).
Delcroix-Gomez, C. et al. Fetal growth restriction, low birth weight, and preterm birth: effects of active or passive smoking evaluated by maternal expired CO at delivery, impacts of cessation at different trimesters. Tob. Induc. Dis. 20, 70 (2022).
Carter, R. C. et al. Fetal alcohol growth restriction and cognitive impairment. Pediatrics 138(2) (2016).
Yan, Q. et al. Maternal serum metabolome and traffic-related air pollution exposure in pregnancy. Environ. Int. 130, 104872 (2019).
Ali, S. S. et al. Understanding oxidants and antioxidants: classical team with new players. J. Food Biochem. 44 (3), e13145 (2020).
Pels, A. et al. Early-onset fetal growth restriction: a systematic review on mortality and morbidity. Acta Obstet. Gynecol. Scand. 99 (2), 153–166 (2020).
Lees, C. et al. Perinatal morbidity and mortality in early-onset fetal growth restriction: cohort outcomes of the trial of randomized umbilical and fetal flow in Europe (TRUFFLE). Ultrasound Obstet. Gynecology: Official J. Int. Soc. Ultrasound Obstet. Gynecol. 42 (4), 400–408 (2013).
Crispi, F. et al. Long-term cardiovascular consequences of fetal growth restriction: biology, clinical implications, and opportunities for prevention of adult disease. Am. J. Obstet. Gynecol. 218 (2S), S869–S879 (2018).
Armengaud, J. B. et al. Intrauterine growth restriction: clinical consequences on health and disease at adulthood. Reprod. Toxicol. 99, 168–176 (2021).
Funding
This research was not funded.
Author information
Authors and Affiliations
Contributions
Wq L and Wl L conceived the study. Yq J, Pf L and Mh Z drafted the manuscript. Wq L and Wl L did the statistical analyses. Gy Zh and Wq L conducted an investigation and verification. Cq Q and Ly W supported data collection. All authors participated in the interpretation of the results and approved the version of the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Consent for publication
Applicable.
Ethics statement
This study was approved by the Ethics Committee of Maternal and Children Health Care Hospital (Huzhong Hospital) of Huadu (no. 2024-001), which waived the requirement for informed consent since the study used de-identified information. The study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jiang, Y., Liu, P., Zeng, M. et al. The effect of air pollution exposure on foetal growth restriction in pregnant women who conceived by in vitro fertilisation a cross-sectional study. Sci Rep 15, 3497 (2025). https://doi.org/10.1038/s41598-025-87955-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-87955-z