Abstract
purpose of this study was to investigate the relationship between AGEs, TSH, metabolic metrics and DN, and to provide evidence for future intervention. Method: This study selected community health service centers which had signed medical alliance agreement with the First Affiliated Hospital of Anhui Medical University and outpatints and inpatients in Anhui province. From March 2018 to July 2022, the multi-stage cluster sampling. method was used to screen residents aged 18–90 years in the above areas. Participants’ blood was collected on an empty stomach to detect TSH, blood lipids, liver and kidney function and blood glucose, in addition, AGEs levels were detected by skin autofluorescence (SAF), and urine was retained to measure the ratio of urinary microalbumin to creatinine concentration by ACR. One-way ANOVA was used to compare the differences between general data, biochemical markers, and urinary ACR, association between variables. Result: A total of 7000 patients who participated in community health examination and inpatients and also had no history of serious mental disorders were selected. After excluding data with missing value of more than 5%, 6921 samples were finally included, and the effective rate was 94.4%. Following health risk factors (HRFs), such as body mass index (BMI), TSH, low-density lipoprotein (LDL), TyG (triglyceride glucose index), systolic blood pressure (SBP), cholesterol (TC), and uric acid (UA) were associated with a higher incidence of urine ACR. In moderation analysis, there is an significant effect among TSH, AGEs and DN, HRFs moderate also these effect. Conclusion: The findings suggest that HRFs such as HDL, TyG and TC should be prioritized when evaluating indicators related to DN to effectively reduce DN in Chinese patients with high health risk levels. Comprehensive indicators may be an effective and practical. method to evaluate the metabolic progression of DN. Optimizing thyroid function management may be a new strategy to prevent and treat DN and may help reduce the risk of AGE-related complications in people with diabetes. This study highlights the important role of AGEs in the relationship between TSH and DN. In addition, future studies should further explore how to improve the management and prevention of DN by regulating TSH.
Among the leading causes of disability and death in patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes (T2DM), chronic kidney disease (CKD) occupies a certain position. Multi-factor intervention targeting advanced glycation end products (AGEs), blood glucose, blood pressure and lipids can reduce the morbidity and mortality of diabetic nephropathy (DN) in T2DM patients through thyroid stimulating hormone (TSH), which plays an important role in the pathological process of metabolic diseases such as DN. AGEs, as a key factor in metabolic regulation, may affect the formation and function of the thyroid gland; However, in DN, the correlation between AGEs and TSH has not been clarified. We hypothesized that AGEs aggravated the negative effect of TSH on DN. The.
Similar content being viewed by others
Introduction
Diabetes, as a common metabolic disease, has always affected people’s health, according to the latest data from the International Diabetes Federation (IDF), 1 in 10 people suffer from diabetes; and what is even more frightening is that by 2045, this would translate to one in eight people developing diabetes, or approximately 783 million people1. So the complications of diabetes, especially diabetic microangiopathy, bring great distress to patients2, but also bring great negative impact on the economy; diabetic nephropathy (DN) posing a significant morbidity and mortality risk3. A meta-analysis of observational studies showed that the overall combined prevalence of DN from January 1980 to October 2019 was 21.8% [95% confidence interval (CI): 18.5–25.4%]4. Another systematic review and meta-analysis reviewed the incidence rate of diabetic kidney disease (DKD) among patients with T2DM ranged from 6.0 to 62.3%5. In view of such a high prevalence rate, it will have an impact on the life and even the life of diabetic patients, so it is very important to understand the influencing factors of the occurrence of DN and observe the interaction between the influencing factors.
There are several factors and mechanisms related to the development and prognosis of DN. DN is also one of the leading causes of end-stage renal disease worldwide, and some common indicators are major risk factors for DN, including hypertension6and hyperlipidemia7. There are various methods to diagnose DN. Microalbuminuria, as an early marker of DN, can be used as routine screening in most hospitals. However, kidney injury can occur even in the absence of microalbuminuria, which exists in many patients with a long course of diabetes3,8. Meanwhile, lipid profile matrics play an important role, there was an indicator that high TyG (triglyceride-glucose index) was significantly associated with DN9,10, cardiovascular disease (CVD)11,12. We found in the evidence of previous studies that elevated blood pressure is an important risk of DN, and reasonable management of blood pressure plays an important role in DN13.
The thyroid gland plays a critical role in regulating metabolism, and its dysfunction can influence the progression of diabetes and its complications14. Among them, diabetes and thyroid dysfunction can co-exist, and thyroid dysfunction can also impair metabolic control in diabetic patients, and the prevalence of thyroid dysfunction in diabetic patients ranges from 2.2 to 17%15. Moreover, relative study has demonstrated that thyroid stimulating hormone (TSH) and FT3 are significant predictors for DN in patients with T2DM, they used thyroid hormone to predict DN by ROC curve, and the result was 0.850 (95% CI: 0.776–0.923)16, although this study have not explored the mechanism, this study also found TSH correlated with DN. Previous studies looking at the association between thyroid function and DN in T2DM subjects with normal thyroid function suggested that FT3 (odds ratio 0.60606 per SD increase [95%CI: Levels of FT4 (per SD increase, or 0.944 [0.894–0.998]) were inversely associated with DN, suggesting that kidney problems in diabetic patients are affected even when thyroid function is normal17. Han et al. reported that TSH and FT3 were correlated with kidney function. According to the results of logistic regression analysis, high TSH and low FT3 were significantly correlated with kidney function, these include estimated glomerular filtration rate (eGFR), urine protein, serum creatinine and serum cystatin C; The quarterback and 8-point analysis showed that the severity of the changes in the above results decreased with increasing FT3 levels; In addition, the researchers also built a synergistic additive model to compare the effects of a single variable, and found that the incidence of overt proteinuria was significantly higher in the additive model than when the other two variables were presented alone, as was the case with massive proteinuria18. As for other factors, TSH is negatively correlated with serum uric acid, and increased TSH is an independent risk factor for hyperuricemia in T2DM patients with early-stage DKD19.
Hyperuricemia was correlated with metabolic syndrome, which further have an impact on DN20. There was also evidence that indicate that thyroid hormones, especially TSH, may be involved in the regulation of uric acid metabolism in early DKD patients, which further proves that there is some correlation between uric acid (UA), TSH, and DN. Temporary hyperglycemia causes the accumulation of advanced glycosylation end products (AGEs), which further deepens the progression of DN21. Previous studies have found that the formation of AGEs further leads to diabetic complications, including DN22. Therefore, it is urgent to develop AGE-related inhibitors21to prevent the progress of DN, and this study verified receptor for AGEs play an important role between glucagon like peptide-1 receptor agonists and inflmmation through kidney protect effect among DN23.
However, there were also studies with negative results, and although there was a difference in TSH between uncomplicated and diabetic nephropathy patients, the difference was not statistically significant15. Previous studies on these health risk factors (HRFs) to a certain extent supported the evidence that promoted the formation and development of DN. Regardless of the effect size, HRFs is also a predictive factor. Negative results also indicated that the establishment of HRFs and HRFs-DN requires a comprehensive evaluation model. The interaction among factors that affect the development of DN will be considered to a greater extent. Considering the large sample size of comprehensive examination in some primary community hospitals, there is still a lack of relevant reports on comprehensive physical examination suitable for DN assessment. To bridge this important knowledge gap, we undertook a large-scale, multicenter, cross-sectional study across diverse communities within Anhui Province. This research aimed to elucidate the relationships between various HRFs and DN, with the ultimate goal of developing a practical and applicable assessment tool for DN that can be utilized in primary healthcare environments. By doing so, we hope to contribute meaningful data and methodologies that can enhance early detection and management strategies for DN in resource-limited settings24. This study aimed to investigate the relationship between AGEs, TSH, and the development of DN and metabolic disorders in patients with T2DM. Specifically, we hypothesized that suboptimal thyroid function would be associated with higher levels of AGEs and a greater prevalence of diabetic nephropathy, and that TSH would moderate the relationship between AGEs and kidney function.
Methods
Study design
This is a retrospective cross-sectional study, based on the theory that HRFs are closely related to prediabetes, diabetes and its complications, such as and DN, and supported by the role of TSH in DN, this study aimed to explore the comprehensive relationship between HRFs (including metabolic metrics) and the epidemiology of DN and its complications. The study was designed and reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist. This study was approved by the ethics committee of the First Affiliated Hospital of Anhui Medical University (Ethics Approval No: PJ2019-09-05).
Settings
Participants were from community health service centers, outpatients, and inpatients in Anhui Province, China. After obtaining informed consent, individuals aged 18–90 with no clear diagnosis of diabetes or no serious disease were included in the study. Trained investigators conduct questionnaires using uniformly designed forms that record demographic information, lifestyle factors, and medical history. Prior to questioning, participants’ blood was drawn to measure measures such as fasting blood glucose (FBG), glycosylated hemoglobin (HbA1c), C-peptide, cholesterol (TC), and triglyceride (TG) levels. In addition, postprandial blood glucose results were obtained after fasting blood was administered and participants were reminded to perform an oral glucose tolerance test (OGTT), measuring postprandial blood glucose and C-peptide levels 2 h after glucose loading24,25.
Exposure and outcomes
There are two types of routine medical examinations, an outpatient examination and an inpatient examination, which are carried out by trained medical personnel using standardized procedures. Identification with ID card to ensure no duplicate data, physical measurement including height, weight, waist circumference (WC), hip circumference, machine examination including AGEs test, fundus examination, blood pressure; Blood and urine samples were taken. These were recorded in participants’ characteristic information such as sex, age, blood pressure, urinary albumin-creatinine ratio (ACR), calculated body mass index (BMI), and waist-to-hip ratio (WHtR).
Evaluation of advanced glycation end products
After other examinations, the patient was instructed to rest for a period of time before AGE examination, and then autologous fluorescence detection was performed on the skin on the voltaic side of the left forearm of the subject with automatic fluorescence analyzer (Hefei Institute of Physics, Chinese Academy of Sciences, National Medical Device Registration Certificate: Anhui Institute 20152210045) to assess the expression level of AGEs in the skin, detailed methods also measured in previous atudy24. During the measurement, obvious blood vessels, scars and malformed skin areas should be avoided, and the selected test location should be wiped with alcohol. The device uses approximately ultraviolet light (center wavelength: 370 nm, half-height width: 15 nm) to irradiate the skin and stimulate the release of AGEs in the skin (wave length range: 420–600 nm). At the same time, the device emits a broadband light source in the frequency (wave length) range of 420–600 nm to illuminate the skin to measure the light absorption and scattering of the tissue. Skin AGEs are ultimately defined as the ratio of fluorescence intensity to diffuse reflected light intensity, and the absorbance range of the fully automatic fluorescence analyzer is 0–150 (in any unit AU). The measurement was carried out by well-trained medical personnel, and the measurement process was carried out in the semi-dark environment at room temperature. After the test, the data were checked to prevent the occurrence of outliers. If there were outliers, the test was repeated.
Criteria for risk factors
(1) The DN was diagnosed according to the recognized diagnostic criteria26.
(2) Inclusion Criteria: Obtain the informed consent of the participants; Be 18 years of age or older and have lived in the survey area for at least 6 months in the 12 months prior to the survey; Complete the investigation independently.
(3) Exclusion Criteria: Participants who quit midway or are not fully tested; No history of serious mental illness or serious complications; Severe impairment of liver and kidney function, infection or stress; Terminally ill people with various diseases; Pregnancy period.
Sample size estimation
Based on previous research indicating a prevalence of DN ranging from 30 to 40%3,27, with a relative precision of 15% (ɛ), α = 0.05, and Z1−α/2= 1.96, the minimum sample size was estimated to be 161. Considering a multi-center design with different ages and communities, a total of 500 people were surveyed to ensure stratified analysis across multiple levels24.
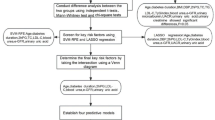
Statistics analysis
All data were analyzed using SPSS 23.0. Descriptive statistics summarized participant demographics and clinical characteristics. Pearson correlations examined relationships between AGEs, thyroid function, and clinical outcomes. Multiple regression analyses identified predictors of diabetic nephropathy and metabolic disorders, examining the moderating role of thyroid function. Moderation analysis was performed using the PROCESS macro in SPSS to test the mediating role of thyroid function. Detailed flow chart is showed in Fig. 1.
Statistical analyses were conducted in three steps:
Descriptive Statistics: Summarized health risk factors by urine ACR group, using chi-squared tests for categorical variables.
Multilevel Logistic Regression: Tested associations between risk factors and urine ACR groups.
Moderation Analysis: Performed using the PROCESS program to test the moderating effect of AGEs on TSH and urine ACR groups. Interaction effects were calculated automatically via SPSS PROCESS, and the proportion of variance explained by the moderating effect of age (R² increase due to interaction) was produced. Adjustments were made for sociodemographic correlates (gender, DBP, hip circumference) in the mediation model. Gender’s moderating effect on the relationship between HRFs (TyG, TC, SBP, HDL) and urine ACR groups was also explored. Moderating effects were considered significant if the 95% confidence interval (CI) did not contain zero28.
In this study, triglyceride glucose (TyG) index was used to comprehensively evaluate the role of blood glucose and lipids, and TyG was calculated using the natural logarithm formula Ln [TG (mg/dL) ×FBG (mg/dL)]/229.
Results
Prevalence characteristics of the urine ACR group
Through initial recruitment, a total of 7000 patients who met the basic requirements were included, and then patients with > 5% missing value were excluded. Finally, 6921 samples were included, with an effective rate of 98.87%.
The prevalence of male was 53.9% (3728/6921). The mean age was (55.46 ± 11.73) years. TSH, UA, TyG was correlated with a positive effect of urine ACR. However, there was no correlation between AGEs and urine ACR; age, gender also not correlated with urine ACR, other results were shown in Table 1.
The correlation between AGEs, TSH, BMI and urine ACR
The study found a significant correlation between HRFs and the urine ACR group, suggesting that HRFs play a crucial role in the development of urine ACR. In Table 2, there was an BMI trend observed in the relationship between HRFs and urine ACR, implying that obesity individuals may be more susceptible to urine ACR due to accumulated HRFs. Furthermore, an interactive correlation was found between AGEs, metabolic metrics, TSH levels, and urine ACR, supported by previous studies demonstrating methods to prevent DN risk by modeling risk factors.
The correlation between AGEs, TSH, age (gender) and urine ACR
Moderation analyses were performed with several variables, the results are presented in Tables 3 and 4. First, AGEs was significantly possible associated with the level of urine ACR, TSH was associated with urine ACR, age also significantly possible associates of the level of urine ACR. Secondly, there were also have significant effect between TSH and AGEs on urine ACR, TSH × age was significant urine ACR, age × AGEs on urine ACR; there are three-way interaction effect between AGEs, TSH and age on urine ACR. similar results was shown in AGEs, TSH and gender on urine ACR.
The correlation between AGEs, TSH, HRFs and urine ACR
Moderation analyses were performed with several variables, the results are presented in Tables 5, 6, 7 and 8. In Table 5, AGEs was significantly possible associated with the level of urine ACR, TSH was associated with urine ACR, SBP also significantly possible associates of the level of urine ACR. Secondly, there were also have significant effect between TSH and AGEs on urine ACR, TSH × SBP was significant urine ACR, SBP × AGEs on urine ACR; there are three-way interaction effect between AGEs, TSH and SBP on urine ACR. Similar results was shown in AGEs, TSH and TG (Table 6), UA (Table 7), TyG (Table 8) on urine ACR.
Discussion
Research significance
This study examined the relationship between HRFs, TSH and DN in a large sample of patients, as well as the relationship between their respective interactions with AGE and DN. This study also provided evidence on the relationship between TSH and AGEs and impaired renal function in T2DM patients, as well as the role of variables related to metabolic disorders. More importantly, in this study, we measured the role of AGEs in the occurrence and development of DN through non-invasive skin detection, thus minimizing the adverse effects caused by invasive lesions.
Previous studies have found that thyroid dysfunction characterized by elevated TSH is associated with a certain degree of AGEs30,31and a higher incidence of DN32. In our study, AGEs were also found to regulate the relationship between TSH and kidney function, with high levels of AGEs exacerbating the positive effects of thyroid underfunction on kidney health. In addition, we found that metabolic metrics based HRFs were correlated with urine ACR, and that there was an AGEs-changing trend between HRFs and urine ACR. That is, there is an interactive relationship between HRFs, AGEs, TSH levels and urinary ACR groups, which is supported by previous studies that demonstrate ways to prevent DN risk by modeling risk factors.
In our study, we concerned age and gender differences may play an important role; Therefore, it is necessary to provide preventive measures for elderly patients with more diabetic complications33. Women are also associated with high urinary ACR levels34; Although in our study, we have not found significant effect among linear regression analysis, while in the moderate analysis, there was a correlation between AGEs, metabolic matrics, and HRFs, with AGEs moderate this correlation between HRFs and urine ACR levels, and AGEs also moderate age (gender) and urine ACR. These results suggest that prevention interventions for diabetes need to focus on gender and age as constant factors, prompting recent assessments of risk scores (including those studied here) to predict DN. In addition, we found correlations between HRFs, AGEs, TSH levels, and urine ACR, suggesting that TSH combined with AGEs may be a comprehensive assessment method to assess the progression of all DN. In our study, we concerned TyG, which can be used as an alternative marker for insulin resistance (IR) and metabolic syndrome, an also correlated with DN9.
Correlations between the TSH, AGEs, HRFs and DN group
AGEs are a class of small molecular compounds formed in the body that bind to proteins, lipids, or nucleic acids through non-enzymatic glycation reactions. AGEs play an important role in the development of a variety of diseases35, especially in diabetes and its complications36, and thyroid related diseases37. In DN, the accumulation of AGEs is considered to be one of the key factors leading to renal function impairment22. It is important to pay close attention to metabolic metrics in managing DN, because they can predict the therapeutic effect of DN, such as obesity38, TyG10, urid acid (UA)39, systolic blood pressure (SBP) [Patel et al., 2020]. Moreover, these risk factors collectively lead to metabolic disorders41, which these could casuse DN.
We have discussed the adverse consequences of individual risk factors before, so the correlation of outcomes caused by the interaction of individual risk factors is also worth exploring. We also explored thyroid-related DN and whether TSH is involved in changes affecting diabetic kidney problems. A hospital-based comparative cross-sectional study have found there were correlation between glucolipid metabolism (such as HbA1c, plasma Cr, albumin-creatinine ratio, HDL-C) as well as objective indicators (such as age, gender) and DN42, a Mendelian randomization study showed there is a causal relationship between HDL-C and TG and DN43. These studies verify abnormal lipid metabolism can lead to progression of kidney disease. Moreover, a prospective observational study verified that although there was a negative correlation between TSH levels and eGFR at baseline, TSH levels did not appear to predict future eGFR declines44; in addition, serum levels of potassium, creatinine and TSH were increased in diabetic nephropathy patients45. There was also study found the correlation between UA and TSH among DN patients46, this study also provide relative basis to verify our hypothesis, the reason why we pay attention to the relationship between UA and TSH is that the two can synergistically enhance the occurrence and development of DN, thyroid hormones, especially TSH, may be involved in regulating uric acid metabolism47, also among patients with early DKD.
Moreover, mouse model also verified the correlation between TSH and DN, in this study, authors concerned that T3 could attenuate albuminuria and improve the renal structural damage in db/db diabetic mice by increasing the activity of phosphatidylinositol 3 kinase and decreasing the expression of transforming growth factor-β148. In addtion, 3,5-diiodothyronine could protect the cells from renal damage in DKD by inhibiting the activation of NF-κβ and JNK; These enzymes and pathways, mentioned above, were involved in the development of DKD49. In vivo and in vitro experiments have shown that exogenous T3 can reverse glucose-induced growth of human podocytes and cardiomyocytes, restore the cellular structure of cardiomyocytes, and reverse pathological changes in kidneys and cardiac organoids. It is through TH receptor α1 activation that glucose-induced transdifferentiation, cell growth and loss of islet beta cells are counterbalanced50; Thyroid stimulating hormone and free triiodothyronine are important indicators for predicting type 2 diabetic nephropathy16. Finally, from genetic content, there was an association between TSH and estimated glomerular filtration rate from creatinine51.
The development mechanism of DN is a complex and multi-factor pathway and mediators involved52, among which the processes AGEs playing an important role include oxidative stress, inflammatory response and extracellular matrix accumulation leading to renal dysfunction. Therefore, controlling blood glucose levels, reducing the formation and accumulation of AGEs, and adopting antioxidant and anti-inflammatory therapeutic strategies are essential for the prevention and treatment of diabetic nephropathy. In addition, regular monitoring of kidney function and urinary protein levels, and adjustment of treatment according to the specific situation is also very necessary.
Implications
These findings highlight the importance of optimizing thyroid function in patients with diabetes to reduce the risk of AGE-related complications, including DN. Regular monitoring of thyroid function and appropriate treatment of thyroid disorders may help improve metabolic control and renal health in this population. If combined with lifestyle interventions, such as a healthy diet, regular exercise to control blood glucose, blood pressure, and lipid management, thyroid function can be more or less improved and AGEs formation reduced.
Strengths and limitations
The obvious advantage of our study is that the sample size is large, and the levels of AGEs are detected by skin fluorescence, which reduces the disadvantages of invasive screening to some extent. Another point is to explore the complex role of AGEs, TSH and metabolic metrics from the perspective of thyroid.
However, there are still some limitations in this study. First, this is only a cross-sectional study without long-term follow-up, so causality cannot be assessed, and the current results are only intended as a reference for future follow-up of these participants. Secondly, the extraction index and physical examination are measured only once, which may lead to classification errors, and should be tested at least 3 times to ensure the deviation of data. Third, due to the limitation of experimental equipment, we did not evaluate the triiodothyronine (T3) of the population. Diabetes may have low triiodothyronine (T3) syndrome, which is prone to hypothyroidism. Therefore, this study may underestimate the relationship between hypothyroidism and some factors, and the level of T3 should be controlled before subsequent analysis. Finally, this study only focused on diabetes patients, and its extensibility is limited. In the future, we should pay attention to the survey results of the general population.
Conclusions
Glucolipid and thyroid function represent modifiable risk factors for prevention and treatment of diabesity and metabolic disease and for promotion of healthy metabolism. In this study, urine ACR used as outcome variables to observe the influencing factors that may lead to DN. In conclusion, this study demonstrates that AGEs plays a significant role in the relationship between TSH and diabetic nephropathy. This study aims to fill a critical gap in the understanding of how HRFs contribute to DN, especially in primary community healthcare settings where resources may be limited. By establishing a comprehensive yet practical evaluation framework, we hope to facilitate better identification and management of DN, ultimately improving patient outcomes in these communities. Optimizing thyroid function may help reduce the risk of AGE-related complications in patients with diabetes. These findings have important implications for the management and prevention of diabetic nephropathy and other metabolic disorders. Early detection of the effects of DN through the hypothalamic-pituitary-thyroid system and urine ACR methods would enable the optimal implementation of effective therapies to prevent diabetes complications.
Data availability
The datasets generated for this study are available on request to the corresponding author.
References
International Diabetes Federation. https://idf.org/.
Madonna, R., Balistreri, C. R., Geng, Y. J. & De Caterina, R. Diabetic microangiopathy: pathogenetic insights and novel therapeutic approaches. Vascul Pharmacol. 90, 1–7. https://doi.org/10.1016/j.vph.2017.01.004 (2017).
Samsu, N. Diabetic Nephropathy: Challenges in Pathogenesis, Diagnosis, and Treatment. Biomed Res Int. ;2021:1497449. doi: 10.1155/2021/1497449. PMID: 34307650; PMCID: PMC8285185. (2021).
Zhang, X. X., Kong, J. & Yun, K. Prevalence of Diabetic Nephropathy among Patients with Type 2 Diabetes Mellitus in China: A Meta-Analysis of Observational Studies. J Diabetes Res. 2020;2020:2315607. Published 2020 Feb 3. https://doi.org/10.1155/2020/2315607
Xu, W., Zhou, Y., Jiang, Q., Fang, Y. & Yang, Q. Risk prediction models for diabetic nephropathy among type 2 diabetes patients in China: a systematic review and meta-analysis. Front Endocrinol (Lausanne). ;15:1407348. Published 2024 Jul 3. (2024). https://doi.org/10.3389/fendo.2024.1407348
Van Buren, P. N. & Toto, R. Hypertension in diabetic nephropathy: epidemiology, mechanisms, and management. Adv. Chronic Kidney Dis. 18 (1), 28–41. https://doi.org/10.1053/j.ackd.2010.10.003 (2011).
Rosario, R. F. & Prabhakar, S. Lipids and diabetic nephropathy. Curr. Diab Rep. 6 (6), 455–462. https://doi.org/10.1007/s11892-006-0079-7 (2006).
Thipsawat, S. Early detection of diabetic nephropathy in patient with type 2 diabetes mellitus: a review of the literature. Diab Vasc Dis. Res. 18 (6), 14791641211058856. https://doi.org/10.1177/14791641211058856 (2021).
Liu, L. et al. Association between the triglyceride-glucose index and diabetic nephropathy in patients with type 2 diabetes: a cross-sectional study. J. Diabetes Investig. 12 (4), 557–565. https://doi.org/10.1111/jdi.13371 (2021).
Yan, H. et al. Associations between cardiometabolic indices and the risk of diabetic kidney disease in patients with type 2 diabetes. Cardiovasc. Diabetol. 23 (1), 142. https://doi.org/10.1186/s12933-024-02228-9 (2024). Published 2024 Apr 25.
Dang, K. et al. The association between triglyceride-glucose index and its combination with obesity indicators and cardiovascular disease: NHANES 2003–2018. Cardiovasc. Diabetol. 23 (1), 8. https://doi.org/10.1186/s12933-023-02115-9 (2024). Published 2024 Jan 6.
Cui, C. et al. Joint association of TyG index and high sensitivity C-reactive protein with cardiovascular disease: a national cohort study. Cardiovasc. Diabetol. 23 (1), 156. https://doi.org/10.1186/s12933-024-02244-9 (2024). Published 2024 May 7.
Hata, S. et al. Impact of continued high blood pressure on the progression of diabetic nephropathy after 10 years: KAMOGAWA-HBP study. Hypertens. Res. https://doi.org/10.1038/s41440-022-01136-3 (2023).
Mantzouratou, P., Lavecchia, A. M., Novelli, R. & Xinaris, C. Thyroid hormone signalling alteration in Diabetic Nephropathy and Cardiomyopathy: a switch to the foetal gene Programme. Curr. Diab Rep. 20 (11), 58. https://doi.org/10.1007/s11892-020-01344-6 (2020). Published 2020 Sep 28.
Rai, S. et al. Thyroid function in type 2 diabetes mellitus and in diabetic nephropathy. J. Clin. Diagn. Res. 7 (8), 1583–1585. https://doi.org/10.7860/JCDR/2013/6216.3299 (2013).
Fei, X. et al. Thyroid stimulating hormone and free triiodothyronine are valuable predictors for diabetic nephropathy in patient with type 2 diabetes mellitus. Ann. Transl Med. 6 (15), 305. https://doi.org/10.21037/atm.2018.07.07 (2018).
Wang, J. et al. Association between thyroid function and diabetic nephropathy in euthyroid subjects with type 2 diabetes mellitus: a cross-sectional study in China. Oncotarget 10 (2), 88–97. https://doi.org/10.18632/oncotarget.26265 (2019). Published 2019 Jan 4.
Han, Q. et al. Thyroid hormones and diabetic nephropathy: an essential relationship to recognize. Nephrol. (Carlton). 24 (2), 160–169. https://doi.org/10.1111/nep.13388 (2019).
Gao, J. & Liu, J. Correlation of serum thyrotropin and thyroid hormone levels with diabetic kidney disease: a cross-sectional study. BMC Endocr. Disord. 24 (1), 170. https://doi.org/10.1186/s12902-024-01699-x (2024). Published 2024 Aug 30.
Maric, C. & Hall, J. E. Obesity, metabolic syndrome and diabetic nephropathy. Contrib. Nephrol. 170, 28–35. https://doi.org/10.1159/000324941 (2011).
Yamazaki, T., Mimura, I., Tanaka, T. & Nangaku, M. Treatment of Diabetic kidney disease: current and future. Diabetes Metab. J. 45 (1), 11–26. https://doi.org/10.4093/dmj.2020.0217 (2021).
Parwani, K. & Mandal, P. Advanced glycation end products and insulin resistance in diabetic nephropathy. Vitam. Horm. 125, 117–148. https://doi.org/10.1016/bs.vh.2024.02.007 (2024).
Sourris, K. C. et al. Glucagon-like peptide-1 receptor signaling modifies the extent of diabetic kidney disease through dampening the receptor for advanced glycation end products-induced inflammation. Kidney Int. 105 (1), 132–149. https://doi.org/10.1016/j.kint.2023.09.029 (2024).
Jiang, T. et al. Advanced glycation end products and diabetes and other metabolic indicators. Diabetol. Metab. Syndr. 14 (1), 104. https://doi.org/10.1186/s13098-022-00873-2 (2022). Published 2022 Jul 25.
Zhang, Y. et al. Effectiveness of early advanced glycation end product Accumulation Testing in the diagnosis of diabetes: a Health risk factor analysis using the body Mass Index as a moderator. Front. Endocrinol. (Lausanne). 12, 766778. https://doi.org/10.3389/fendo.2021.766778 (2022). Published 2022 Mar 11.
American Diabetes Association. Standards of medical care in diabetes–2008. Diabetes Care. 31 (Suppl 1), S12–S54. https://doi.org/10.2337/dc08-S012 (2008).
Alicic, R. Z., Rooney, M. T. & Tuttle, K. R. Diabetic kidney disease: challenges, Progress, and possibilities. Clin. J. Am. Soc. Nephrol. 12 (12), 2032–2045. https://doi.org/10.2215/CJN.11491116 (2017).
Hayes, A. F. & Rockwood, N. J. Regression-based statistical mediation and moderation analysis in clinical research: observations, recommendations, and implementation. Behav. Res. Ther. 98, 39–57. https://doi.org/10.1016/j.brat.2016.11.001 (2017).
Abbasi, F. & Reaven, G. M. Comparison of two methods using plasma triglyceride concentration as a surrogate estimate of insulin action in nondiabetic subjects: triglycerides × glucose versus triglyceride/high-density lipoprotein cholesterol. Metabolism 60 (12), 1673–1676. https://doi.org/10.1016/j.metabol.2011.04.006 (2011).
Chen, X. J. et al. Advanced glycation end-products induce oxidative stress through the Sirt1/Nrf2 axis by interacting with the receptor of AGEs under diabetic conditions [retracted in: J Cell Biochem. ;122 Suppl 1:S97. doi: 10.1002/jcb.30065]. J Cell Biochem. 2019;120(2):2159–2170. (2021). https://doi.org/10.1002/jcb.27524
D’Adamo, E. et al. Thyroid dysfunction in obese pre-pubertal children: oxidative stress as a potential pathogenetic mechanism. Free Radic Res. 46 (3), 303–309. https://doi.org/10.3109/10715762.2011.653967 (2012).
Liu, M. C. et al. Association between thyroid hormones and diabetic kidney disease in Chinese adults. BMC Endocr. Disord. 23 (1), 56. https://doi.org/10.1186/s12902-023-01299-1 (2023). Published 2023 Mar 8.
Thomas, B. The Global Burden of Diabetic kidney disease: Time trends and gender gaps. Curr. Diab Rep. 19 (4), 18. https://doi.org/10.1007/s11892-019-1133-6 (2019). Published 2019 Mar 2.
Shen, Y. et al. Diabetes mellitus as a risk factor for incident chronic kidney disease and end-stage renal disease in women compared with men: a systematic review and meta-analysis. Endocrine 55 (1), 66–76. https://doi.org/10.1007/s12020-016-1014-6 (2017).
Yang, P., Feng, J., Peng, Q., Liu, X. & Fan, Z. Advanced Glycation End products: potential mechanism and therapeutic target in Cardiovascular complications under Diabetes. Oxid. Med. Cell. Longev. 2019, 9570616. https://doi.org/10.1155/2019/9570616 (2019). Published 2019 Dec 6.
Khalid, M., Petroianu, G. & Adem, A. Advanced Glycation End products and Diabetes Mellitus: mechanisms and perspectives. Biomolecules 12 (4), 542. https://doi.org/10.3390/biom12040542 (2022). Published 2022 Apr 4.
Csiha, S. et al. Advanced glycation end products and their soluble receptor (sRAGE) in patients with Hashimoto’s thyroiditis on levothyroxine substitution. Front. Endocrinol. (Lausanne). 14, 1187725. https://doi.org/10.3389/fendo.2023.1187725 (2023). PMID: 37305044; PMCID: PMC10250717.
Lu, J. et al. Body Mass Index and Risk of Diabetic Nephropathy: a mendelian randomization study. J. Clin. Endocrinol. Metab. 107 (6), 1599–1608. https://doi.org/10.1210/clinem/dgac057 (2022).
Bjornstad, P. et al. Fructose and uric acid in diabetic nephropathy. Diabetologia 58 (9), 1993–2002. https://doi.org/10.1007/s00125-015-3650-4 (2015).
PatelDM, Bose, M. & CooperME Glucose and blood pressure-dependent pathways-the Progression of Diabetic kidney disease. Int. J. Mol. Sci. 21 (6), 2218. https://doi.org/10.3390/ijms21062218 (2020). Published 2020 Mar 23.
Mallorquí-Bagué, N. et al. Type 2 diabetes and cognitive impairment in an older population with overweight or obesity and metabolic syndrome: Baseline cross-sectional analysis of the PREDIMED-plus study. Sci. Rep. 8, 16128. https://doi.org/10.1038/s41598-018-33843-8 (2018).
Dejenie, T. A. et al. Dyslipidemia and serum cystatin C levels as biomarker of diabetic nephropathy in patients with type 2 diabetes mellitus. Front. Endocrinol. (Lausanne). 14, 1124367. https://doi.org/10.3389/fendo.2023.1124367 (2023). Published 2023 Apr 4.
Liu, H. et al. The causal relationship between 5 serum lipid parameters and diabetic nephropathy: a Mendelian randomization study. Front Endocrinol (Lausanne). ;15:1358358. Published 2024 May 28. (2024). https://doi.org/10.3389/fendo.2024.1358358
Iwakura, H. et al. Thyroid function, glycemic control, and diabetic nephropathy in patients with type 2 diabetes over 24 months: prospective observational study. BMC Endocr Disord. ;23(1):146. Published 2023 Jul 10. (2023). https://doi.org/10.1186/s12902-023-01393-4
Boruah, P. et al. A study to evaluate the Association between thyroid function and serum potassium level in diagnosed cases of Diabetic Nephropathy. Cureus 13 (10), e18569. https://doi.org/10.7759/cureus.18569 (2021). Published 2021 Oct 7.
Feng, X., Huang, J., Peng, Y. & Xu, Y. Association between decreased thyroid stimulating hormone and hyperuricemia in type 2 diabetic patients with early-stage diabetic kidney disease. BMC Endocr. Disord. 21 (1), 1. https://doi.org/10.1186/s12902-020-00672-8 (2021). Published 2021 Jan 6.
Sun, Y. et al. Impaired sensitivity to thyroid hormones is Associated with Hyperuricemia, obesity, and Cardiovascular Disease risk in subjects with subclinical hypothyroidism. Thyroid 32 (4), 376–384. https://doi.org/10.1089/thy.2021.0500 (2022).
Lin, Y. & Sun, Z. Thyroid hormone ameliorates diabetic nephropathy in a mouse model of type II diabetes. J. Endocrinol. 209, 185–191. https://doi.org/10.1530/JOE-10-0340 (2011).
Shang, G. et al. 3,5-Diiodo-l-thyronine ameliorates diabetic nephropathy in streptozotocin-induced diabetic rats. Biochim. Biophys. Acta. 1832 (5), 674–684. https://doi.org/10.1016/j.bbadis.2013.01.023 (2013).
Lavecchia, A. M. et al. Thyroid hormone treatment counteracts cellular phenotypical remodeling in diabetic organs. iScience 26 (10), 107826. https://doi.org/10.1016/j.isci.2023.107826 (2023). PMID: 37752946; PMCID: PMC10518716.
Ellervik, C., Mora, S., Ridker, P. M. & Chasman, D. I. Hypothyroidism and kidney function: a mendelian randomization study. Thyroid 30 (3), 365–379. https://doi.org/10.1089/thy.2019.0167 (2020).
Pérez-Morales, R. E. et al. Inflammation in Diabetic kidney disease. Nephron 143 (1), 12–16. https://doi.org/10.1159/000493278 (2019).
Acknowledgements
We would like to acknowledge all hospital action teams, the staff and participants from the participating hospitals, and our cooperators, for assistance in data collection.
Funding
This research was funded by the National Natural Science Foundation of China (82370836) and Anhui Province Clinical Medical research transformation Project (202204295107020027).
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Anhui Medical University and in accordance with the Declaration of Helsinki. All focus group participants provided signed informed consent prior to the start of the focus groups.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, Y., Wang, Y., Kang, Q. et al. The role of advanced glycation end products between thyroid function and diabetic nephropathy and metabolic disorders. Sci Rep 15, 7202 (2025). https://doi.org/10.1038/s41598-025-88806-7
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-88806-7