Abstract
Although the link between inflammation and chronic obstructive pulmonary disease (COPD) is increasingly recognized, the correlation between systemic immune response index (SIRI), a novel marker of inflammation, and COPD is unknown. This cross-sectional study used data from patients with complete lung function in NHANES 2007–2012 to explore the relationship between SIRI and COPD. We performed a series of statistical analyses on a total of 5056 participants, including multiple linear regression, smoothed curve fitting, ROC curve analysis, and subgroup analysis. In the fully corrected model, the logistic multiple regression showed that SIRI was associated with a high risk of COPD (OR1.350, 95% CI:1.220,1.493). The ROC curve showed that SIRI (AUC = 0.596) was significantly more efficient than other inflammatory factors in predicting COPD. Smoothed curve fit effect and threshold effect analyses showed a linear correlation between SIRI COPD prevalence, and subgroup analyses showed that the effect of SIRI on COPD was more pronounced in still smokers (OR 1.58, 95% CI: 1.34, 1.86) versus men (OR 1.62, 95% CI: 1.44, 1.83). The results of the interaction test provide evidence supporting SIRI as an independent risk factor for COPD.
Similar content being viewed by others
Introduction
Chronic obstructive pulmonary disease (COPD) is a common respiratory disease characterized by progressive and irreversible airflow limitation1. Currently, COPD remains one of the major contributors to morbidity and mortality in the world’s population, substantially impacting patients’ well-being and increasing their medical expenses2. According to projections, COPD will rank as the third most common cause of mortality globally by 2030. The disorder is more common among men, yet the occurrence in women is rising, leading to a diminishing gender disparity. Additionally, COPD is more common in low-income countries, possibly because these areas are more exposed to more severe air pollutants3. The pathogenesis of COPD consists of many factors and the process is complex and varied4, and although important advances have been made in the understanding of COPD, there is still a need for further research into the underlying mechanisms of COPD and the implementation of effective interventions to improve patient prognosis.
SIRI includes absolute numbers of neutrophils, monocytes, and lymphocytes5. According to recent research, SIRI is linked to the onset of CVD6; there is a positive correlation with psoriasis7, high levels of SIRI are associated with a high mortality rate in sepsis8, and SIRI can be used to predict the survival of patients with pancreatic cancer who are receiving chemotherapy9, however, there are few data on the connection between SIRI and the prevalence of COPD.
COPD is characterized by persistent airway inflammation and immune dysfunction10. Research has demonstrated a correlation between inflammation and immunology in the onset and progression of COPD. Higher levels of oxidative stress and pro-inflammatory cytokines in the airways of patients with COPD suggest that inflammation persists11,12. Given how simple it is to get clinical data straight from SIRI, investigating its relationship to COPD is crucial for both diagnosing and treating the disease.
Therefore, the purpose of the research was to investigate the connection between SIRI and COPD, utilizing cross-sectional information obtained from the NHANES.
Method
Study data and population
We analyzed data from the 2007–2012 NHANES in this cross-sectional investigation. For a thorough explanation of the NHANES and information on how data are collected, observe the National Center for Health Statistics. In summary, NHANES is a series of cross-sectional, complex, multistage surveys conducted by the Centers for Disease Control and Prevention (CDC) of a nationally representative U.S. noninstitutionalized population that provides data on the health and nutritional status of the populations surveyed.
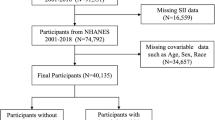
We analyzed NHANES data collected during the period 2007–2012, totaling N = 30,442 subjects, and included a total of 5,056 (2,517 males and 2,539 females) subjects after excluding data on lack of demographics, smoking, alcohol consumption, whole blood counts, lipids, lung function, and comorbidities. Inclusion exclusion criteria are shown in Fig. 1.
NHANES has received ethical approval from the National Center for Health Statistics Research Ethics Review Board (National Center for Health Statistics Research Ethics Review). National Center for Health Statistics Research Ethics Review Board approval (National Center for Health Statistics, 2012).
Criteria for COPD
In this study, the COPD diagnostic standards were (1) FEV 1/FVC < 70% after inhalation of bronchodilators, (2) a history of chronic bronchitis or smoking and current need for COPD treatment, and (3) self-reported presence of emphysema13.
Calculation of different systemic inflammation indices
Patients were collected from eligible subjects at the NHANES mobile screening center. SIRI was defined as (N × M)/L, where N, M, and L represent peripheral neutrophil, monocyte, and lymphocyte counts, respectively. The calculation of other inflammatory factors is detailed in the accompanying table.
Covariates
Relevant or potential confounders were determined based on existing research literature and clinical knowledge. For this article, the following covariate information was collected. Participant demographic data and sociodemographic data: including age (continuous), sex (male/female), race (non-Hispanic white, non-Hispanic black, Mexican American, other Hispanic, and other races), education level (< high school, high school, and > high school), and poverty-to-income ratio. Lifestyle and body measurements such as smoking situation (never, former, current), alcohol consumption, and body mass index (BMI) were also included. Criteria for categorizing smoking and alcohol use were consistent with previous reports. Information on concurrent cardiovascular diseases, including hypertension, diabetes, coronary heart disease, angina, stroke, and heart attack was also added as covariates through the questionnaire.
Statistical analysis
Since the NHANES survey employs a sophisticated, multi-phase, stratified probability sampling method, suitable weights, sampling units, and strata were utilized for the statistical analysis. Comparisons were done based on the normality and distribution of the data for continuous variables, which were displayed as the median with the first and third quartiles or the mean with its standard deviation (SD), utilizing either the Student’s t-test or the Mann-Whitney U test. Meanwhile, categorical variables were reported as counts and percentages, and they were analyzed using either the chi-squared test or the Fisher’s exact test. Multifactorial logistic regression analysis was used to analyze the relationship between different inflammatory indicators and COPD. Covariates were not taken into account in Model 1. Age, gender, race, and education were taken into account in model 2, and all of the aforementioned covariates were taken into account in model 3. 95% CI (confidence intervals) and odds ratios (OR) were used to express the results. The diagnostic value of novel inflammatory biomarkers screened by multivariate regression analysis was evaluated using subject work characteristics (ROC) curves. To determine whether there was a nonlinear association between COPD and SIRIs, smoothed curve fitting, threshold effect, and saturation effect studies were employed. Heterogeneity between subgroups is assessed by interactions. R (version 4.2.2) and EmpowerStats software were used for all analyses, and a p-value of less than 0.05 was deemed statistically significant.
Result
Baseline characteristics of the participant population
A total of 5056 participants were recruited for the study, and the sample included 4350 non-COPD participants as well as 706 COPD patients. The baseline characteristics of the participants are shown in Table 1. Patients with COPD were older than normal, and the difference was statistically significant (P < 0.001). The COPD group had higher age, gender, race, education, BMI, history of hypertension, diabetes, coronary heart disease, heart attack, history of stroke, smoking status, drinking status, FEV1 values, leukocyte count, lymphocyte count, neutrophil count, and indices such as SIRI, SII, NLR, and LMR, and the differences were statistically significant (P < 0.001).
Relationship between inflammatory markers and CODP
Table 2 displays the results of the multivariable logistic regression study investigating the connection between inflammatory indicators and COPD. An increase in SIRI, SII, NLR, and LLR was positively correlated with the overall occurrence of COPD, whereas a decrease in LMR was negatively related to COPD. When these inflammatory markers were analyzed as categorical variables in quartiles, in the fully adjusted model, SIRI was in quartile 3 (OR 1.344 95%CI 1.042,1.732) and quartile 4 (OR 1.836 95%CI 1.438,2.343), SII was in quartile 3 (OR 1.288 95%CI 1.010, 1.642 ) and quartile 4 (OR1.486 95%CI 1.173, 1.883), NLR in quartile 2 (OR1.313 95%1.016, 1.698), quartile 3 (OR1.611 95%CI 1.256, 2.067) and quartile 4 (OR1.745 95%CI 1.370, 2.222), and LLR in quartile 4 (OR1.342 95%CI1.060, 1.699) both showed significant.
Smooth curve fitting
Smoothed curve fitting showed in Fig. 2 that there was a linear relationship between the SIRI index and the incidence of COPD after adjusting for all covariate models. the risk of COPD incidence for each unit increase in the SIRI was a 16% increase from the previous level (OR = 1.166 95% CI (1.040,1.307)).
ROC curve analysis
ROC curve analysis was shown in Fig. 3 which used to evaluate the validity of inflammatory indicators. The results were shown in Fig. 3, and the AUCs of SIRI, LMR, NLR, SII, and LLR were 0.596, 0.583, 0.574, 0.555, and 0.521 indicating that SIRI was better than the other inflammatory indicators in predicting COPD.
Subgroup analysis and interactions
The results of subgroup analyses and interactions are shown in Fig. 4 which illustrates that there was no significant moderating effect of SIRI on the COPD association across age, race, and the presence or absence of diabetes, hypertension, coronary heart disease, heart attack, angina pectoris, stroke, and whether or not alcohol was consumed. In contrast, significant moderating effects were demonstrated in gender and whether or not they smoked, with the association of SIRI with COPD being stronger in men than in women, and the effect of SIRI on COPD being stronger in smokers, especially those who still smoked, whereas the association was not significant in never-smokers. Interestingly, although racial differences were not significant in the effect of SIRI on COPD, the effect of SIRI on COPD was strongest among Mexican Americans.
Discussion
This is the first article to examine the relationship between SIRI and COPD. We discovered that elevated levels of SIRI exhibited a linear correlation with a higher incidence of COPD. Meanwhile, the ROC curve showed that SIRI was superior to SII and other inflammatory indicators in distinguishing COPD from non-COPD. Subgroup analyses showed that the effect of SIRI on COPD was more pronounced in men as well as in those who still smoked. The present study suggests that the SIRI index can be used as a potential COPD biomarker for further studies.
The underlying mechanisms of COPD have not yet been fully characterized. Studies have shown that activated neutrophils in COPD patients can secrete serine proteases, which generate oxidative stress and increase alveolar destruction, thereby exacerbating hypoxia in COPD patients11,12,14. A variety of cytokines and proteases secreted by neutrophils have been associated with lung injury and lung remodeling in COPD.IL-1 and CXCL 8, neutrophil elastase (NE), matrix metalloproteinase (MMP), and high-mobility-group protein 1 (HMGB 1) were shown to be associated with COPD severity and frequency15,16,17. T cells activated by chemokines are also able to promote the process of alveolar cell apoptosis11. Lymphocytes play an important role in COPD airway remodeling by mediating acquired immunity as inflammatory mediators regulatory or protective functions. Current research focuses on the infiltration of T and B lymphocytes and the reduction of regulatory T cells in the airway18,19,20,21. It has also been shown that platelets can be involved in the development and progression of COPD through a variety of mechanisms, including the secretion of platelet factor 4 that disrupts pulmonary elasticity and induces a prethrombotic state and pulmonary vascular remodeling22,23. These cells and their derived ratios have been further investigated as potential inflammatory markers capable of guiding COPD prediction and prevention.
In previous literature, it has been shown that SII, NLR, LLR, PLR, etc. can be used as new inflammatory markers in COPD.NLR may be associated with COPD combined with pulmonary hypertension and mortality in COPD24,25. It may serve as an indicator of unfavorable outcomes and fatality during acute flare-ups of COPD17,26,27. According to one study, people with COPD who do not have sarcopenia have a greater chance of dying if their SII levels are raised28. It has also been shown that COPD patients at higher risk of malnutrition have elevated NLR and PLR and reduced LMR compared to COPD patients whose risk of malnutrition is accordingly lower29. LLR is an independent factor influencing severity in COPD patients30。 This is further confirmed by our experiments.
The strengths of this study are the design based on a large prospective population, which fills a gap in the relationship between SIRI and COPD prevalence, as well as revealing the quantitative and qualitative relationship between the SIRI index and COPD. Second, NHANES used a stratified multistage sampling design to obtain a sample representative of the institutionalized civilian population in the United States, which allows for broad applicability and generalizability of the study. Third, it controlled for many potential factors and used ROC curves to compare the efficiency of the effects of each indicator on COPD. In addition, the study had the following limitations; first, although we controlled for potential confounding factors, we were unable to eliminate some unknown other uncontrollable factors. Second, due to the nature of cross-sectional studies, it is difficult to infer causal relationships. Third, some of the survey data from the questionnaire may have been biased due to the effects of recall. Fourth, the study only looked at people in the United States; it needs to be verified in other countries. To further improve the utility of this marker, it is necessary to confirm the predictive value of SIRI for COPD in future studies with some longitudinal studies and RCTs.
Conclusion
Overall, this study showed that SIRI was positively associated with the prevalence of COPD, and for every 1-unit increase in SIRI, the prevalence of COPD increased by 16.6% compared with the previous one, meanwhile, the ROC curve showed that the SIRI index predicted COPD significantly better than the other indexes, which may play an important role for us in the routine clinical practice of diagnosing COPD.
Data availability
The data used in this study were derived from the National Health and Nutrition Examination Survey (NHANES) 2007-2012 datasets, which are publicly available and can be accessed through the NHANES website at https://www.cdc.gov/nchs/nhanes/index.htm.
References
Soriano, J. B. et al. Global, regional, and National deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: a systematic analysis for the global burden of disease study 2015. Lancet Respiratory Med. 5, 691–706 (2017).
Lareau, S. C., Fahy, B., Meek, P. & Wang, A. Chronic Obstructive Pulmonary Disease (COPD).
Christenson, S. A., Smith, B. M. & Bafadhel, M. Putcha, N. Chronic obstructive pulmonary disease. Lancet 399, 2227–2242 (2022).
Kaur, M., Chandel, J., Malik, J. & Naura, A. S. Particulate matter in COPD pathogenesis: an overview. Inflamm. Res. 71, 797–815 (2022).
Gu, L. et al. Systemic inflammatory response index (SIRI) is associated with all-cause mortality and cardiovascular mortality in population with chronic kidney disease: evidence from NHANES (2001–2018). Front. Immunol. 15, 1338025 (2024).
Jin, Z. et al. The Associations of Two Novel Inflammation Indexes, SII and SIRI with the Risks for Cardiovascular Diseases and All-Cause Mortality: A Ten-Year Follow-Up Study in 85,154 Individuals. JIR Volume 14, 131–140 (2021).
Ma, R. et al. Association between systemic immune inflammation index, systemic inflammation response index and adult psoriasis: evidence from NHANES. Front. Immunol. 15, 1323174 (2024).
Zhang, Y., Xing, Z., Zhou, K. & Jiang, S. The predictive role of systemic inflammation response index (SIRI) in the prognosis of stroke patients. CIA Volume. 16, 1997–2007 (2021).
Qi, Q. et al. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer 122, 2158–2167 (2016).
Brightling, C. & Greening, N. Airway inflammation in COPD: progress to precision medicine. Eur. Respir J. 54, 1900651 (2019).
Barnes, P. J. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J. Allergy Clin. Immunol. 138, 16–27 (2016).
Barnes, P. J. Inflammatory endotypes in COPD. Allergy 74, 1249–1256 (2019).
Ye, C., Yuan, L., Wu, K., Shen, B. & Zhu, C. Association between systemic immune-inflammation index and chronic obstructive pulmonary disease: a population-based study. BMC Pulm Med. 23, 295 (2023).
Lodge, K. M. et al. Hypoxia increases the potential for Neutrophil-mediated endothelial damage in chronic obstructive pulmonary disease. Am. J. Respir Crit. Care Med. 205, 903–916 (2022).
Gangemi, S. et al. Association between HMGB1 and COPD: A Systematic Review. Mediators of Inflammation 164913 (2015). (2015).
Al Nakouzi, N. et al. Cabazitaxel remains active in patients progressing after docetaxel followed by novel androgen receptor pathway targeted therapies. Eur. Urol. 68, 228–235 (2015).
Sakurai, K. et al. Clinical utility of blood neutrophil-lymphocyte ratio in Japanese COPD patients. BMC Pulm Med. 18, 65 (2018).
Hogg, J. C., Buzatu, L. & Coxson, H. O. The nature of Small-Airway obstruction in chronic obstructive pulmonary disease. N Engl. J. Med. (2004).
Duncan, S. Role of T-lymphocytes and pro-inflammatory mediators in the pathogenesis of chronic obstructive pulmonary disease. COPD Volume. 3, 531–541 (2008).
Brusselle, G. G., Joos, G. F. & Bracke, K. R. New insights into the immunology of chronic obstructive pulmonary disease. Lancet 378, 1015–1026 (2011).
Duan, M. C. et al. Infiltration of IL-17-Producing T cells and Treg cells in a mouse model of Smoke-Induced emphysema. Inflammation 39, 1334–1344 (2016).
Chebbo, M., Duez, C., Alessi, M. C., Chanez, P. & Gras, D. Platelets: a potential role in chronic respiratory diseases? Eur. Respir Rev. 30, 210062 (2021).
Mallah, H., Ball, S., Sekhon, J., Parmar, K. & Nugent, K. Platelets in chronic obstructive pulmonary disease: an update on pathophysiology and implications for antiplatelet therapy. Respir. Med. 171, 106098 (2020).
Jiang, T. et al. Value of the neutrophil-to-lymphocyte ratio in chronic obstructive pulmonary disease complicated with pulmonary hypertension. J. Int. Med. Res. 51, 03000605231200266 (2023).
Hu, H. S., Wang, Z., Jian, L. Y., Zhao, L. M. & Liu, X. D. Optimizing inhaled corticosteroid use in patients with chronic obstructive pulmonary disease: assessing blood eosinophils, neutrophil–to–lymphocyte ratio, and mortality outcomes in US adults. Front. Immunol. 14, 1230766 (2023).
Neutrophil-to-Lymphocyte. Ratio Predicts Clinical Outcome of Severe Acute Exacerbation of COPD in Frequent Exacerbators. COPD.
Pascual-González, Y., López-Sánchez, M., Dorca, J. & Santos, S. Defining the role of neutrophil-to-lymphocyte ratio in COPD: a systematic literature review. COPD Volume. 13, 3651–3662 (2018).
Benz, E. et al. Sarcopenia, systemic immune-inflammation index and all-cause mortality in middle-aged and older people with COPD and asthma: a population-based study. ERJ Open. Res. 8, 00628–02021 (2022).
Baldemir, R. & Cirik, M. Ö. Practical parameters that can be used for nutritional assessment in patients hospitalized in the intensive care unit with the diagnosis of chronic obstructive pulmonary disease: prognostic nutritional index, neutrophil-to-lymphocyte, platelet-to-lymphocyte, and lymphocyte-to-monocyte ratio. Medicine 101, e29433 (2022).
Huang, Y. et al. The relationship of Low-Density-Lipoprotein to lymphocyte ratio with chronic obstructive pulmonary disease. COPD Volume. 17, 2175–2185 (2022).
Acknowledgements
The authors thank the participants of the NHANES databases.
Author information
Authors and Affiliations
Contributions
Conceptualization: S.J.; Methodology: S.J.; Writing—original draft preparation: S.J. and W.H.; Writing—review and editing: S.J. and Q.C. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The protocols of NHANES were approved by the institutional review board of the National Center for Health Statistics, CDC. NHANES has obtained written informed consent from all participants.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jia, S., Chen, Q., Huang, W. et al. Relationship between systemic immune response index (SIRI) and COPD: a cross-sectional study based on NHANES 2007–2012. Sci Rep 15, 7887 (2025). https://doi.org/10.1038/s41598-025-90947-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-90947-8
Keywords
This article is cited by
-
Visceral adiposity index, premature mortality, and life expectancy in US adults
Lipids in Health and Disease (2025)
-
Joint association of inflammatory markers and sedentary time with mortality in metabolic dysfunction-associated steatotic liver disease population and the mediating role of inflammation
European Journal of Medical Research (2025)