Abstract
With the increasing popularity of minimally invasive techniques in thyroid surgery, the transoral endoscopic thyroidectomy vestibular approach (TOETVA) has garnered significant attention. This study aimed to compare the impact of different distances between the observation and operation ports in TOETVA on clinical treatment outcomes. Ninety patients with papillary thyroid carcinoma were retrospectively analyzed. Based on the distance between the observation and operation ports, they were divided into three groups: Group A (2.3–2.7 cm), Group B (less than 2.3 cm), and Group C (more than 2.7 cm). All three groups underwent TOETVA performed by the same surgical team. Operation time, blood loss, postoperative hospital stay, drainage volume, retrieved and metastatic central lymph nodes, postoperative complications, and tumor recurrence were compared among the groups. There were no demographic differences among the three groups. Compared to Groups B and C, patients in Group A had significantly shorter operation times, lower postoperative drainage volumes, and shorter postoperative hospital stays (p < 0.05). There were no significant differences in bleeding amount, retrieved and metastatic central lymph nodes, or incidence of complications among the groups. No postoperative recurrences were observed in any patient. In TOETVA, the best surgical outcomes were achieved when the distance between the observation and operation ports was approximately 2.5 cm (2.3–2.7 cm). This configuration ensures smooth surgical operations and facilitates postoperative rehabilitation, making it worthy of further clinical promotion.
Similar content being viewed by others
Introduction
With the increasing popularity of health screenings and advancements in ultrasound diagnostic technology, the global detection rate of thyroid cancer has been steadily rising, with approximately 90% of cases being papillary thyroid carcinoma (PTC)1. Surgical treatment remains the primary approach for managing thyroid cancer. However, since PTC predominantly affects females, particularly young women, there is a growing demand among patients for aesthetically pleasing surgical outcomes2. Endoscopic thyroidectomy involves operating through several discreet puncture ports to place the surgical instruments, thereby avoiding the scarring issues associated with traditional anterior neck incisions3. This makes it increasingly favored by younger patients.
Endoscopic thyroidectomy is classified into different surgical approaches based on the location of the puncture ports, including the transoral endoscopic thyroidectomy vestibular approach (TOETVA), the transaxillary approach, the trans-chest/breast approach, the retroauricular approach and so on4. Among these procedures, TOETVA has quickly become a focal point in clinical practice and research due to its scarless nature, relatively short dissection path, ability to simultaneously address bilateral lesions, and thorough clearance of lower central lymph nodes5.
In TOETVA, the observation port is located anterior to the frenulum of the lower lip, more than 5 mm away from the gingival margin, while the bilateral operation ports are situated near the roots of the first premolars on both sides6. The distance between the operation ports and the midpoint (observation port) is approximately 2.5 cm, a distance deemed optimal based on the collective experience of various medical institutions. However, despite the widespread adoption of this viewpoint in clinical practice, it lacks definitive clinical data support. Therefore, this study aims to compare the effects of different operation port positions on surgical.
Methods
Study cohort
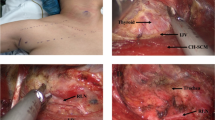
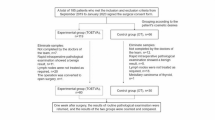
This study conducted a retrospective analysis of 90 patients with PTC who underwent TOETVA at the Breast and thyroid cancer diagnosis and treatment center of the First People’s Hospital of Chenzhou from March 2021 to August 2021. The extent of surgery included unilateral thyroidectomy and unilateral central lymph node dissection. All surgeries were performed by the same surgical team. The distance between the observation and operation ports was measured with a tape ruler post-surgery, after trocar removal. Measurements were taken from the midpoint of the inner edge of each incision near the mandibular surface, which is relatively fixed and unaffected by lip traction. The average of the right-to-middle and left-to-middle distances was calculated to represent the port distance for each patient (Fig. 1). The patients were divided into three groups based on these distances: Group A (2.3–2.7 cm), Group B (less than 2.3 cm), and Group C (more than 2.7 cm). This study was approved by the Ethics Committee of the First People’s Hospital of Chenzhou and all participants provided informed consent. The study was conducted in accordance with the World Medical Association Declaration of Helsinki 2013 and was compliant with the STROBE guidelines7.
Schematic representation of port placement and measurement of distances in TOETVA. The central observation port is positioned at the midpoint of the oral vestibule, while the operation ports are located laterally. The distances between the observation port and the operation ports (bilateral) are shown, measured from the midpoints of the inner edge of each incision near the mandibular surface.
Inclusion and exclusion criteria
Inclusion criteria
-
(1)
Age ≥ 18 years.
-
(2)
Preoperative fine needle aspiration confirming PTC.
-
(3)
The tumor was unilateral with a maximum diameter of less than 2 cm.
-
(4)
Absence of lateral lymph node metastasis.
-
(5)
Patients understood the content of the study and signed informed consent.
Exclusion criteria
-
(1)
History of neck or mandibular surgery or radiotherapy.
-
(2)
Presence of thyroiditis, hyperthyroidism, or hypothyroidism.
-
(3)
Tumor located in the upper pole region of the thyroid gland.
-
(4)
Patients unfit for TOETVA, including those with oral or mandibular deformities.
-
(5)
Lateral cervical lymph node or distant metastasis.
-
(6)
Loss to follow-up or refusal to participate in the study.
Surgical procedure
All surgeries were performed using the Karl Storz TC200EN laparoscopic surgical system. All patients underwent unilateral thyroidectomy and central lymph node dissection. Prophylactic antibiotics (cefoperazone, 2.0 g) were administered intravenously 30 min before surgery.
After general anesthesia, the patient was placed in a supine position with arms adducted and fixed in position. The neck was maintained in a slightly overstretched position. The oral vestibule was exposed, and a single transverse incision (1–2 cm) was made at the midpoint of the oral vestibule, avoiding the lower lip frenulum. This incision was extended bilaterally to the level of the first premolars to allow complete exposure of the mental nerves8. The first space was established by blunt separation after injection of 5 ml of expansion solution (1:500,000 epinephrine in normal saline). A 10 mm trocar was placed through the observation port, CO2 was insufflated, maintaining a pressure of 6 mmHg, and the flow rate was set to medium. Two puncture points were placed approximately 2–3 cm from the central incision, adjusted either medial or lateral to the mental nerves to minimize injury and accommodate anatomical variation. Two 5 mm Trocars were placed at a 45-degree angle, avoiding the mental nerve. These trocars passed over the surface of the mandible and converged with the 10 mm trocar through the subcutaneous surgical channel at the level of the thyroid cartilage. A laparoscope and surgical instruments were inserted, and the dissection proceeded deep to the strap muscles, freeing the space between the strap muscle and the sternocleidomastoid muscle, descending to the suprasternal notch bilaterally to the sternoclavicular muscle.
The linea alba cervicalis was severed by an electrotome and the strap muscles suspended with sutures, A lymphatic tracer (0.1 ml Carbon Nanoparticles Suspension Injection) was injected. The pyramids of thyroid and the prelaryngeal lymph nodes were dissected, the thyroid isthmus was transected with a harmonic scalpel. The upper pole of the thyroid gland on the affected side was severed with an ultrasonic scalpel, the RLN was completely dissected after exposure, the upper and lower paraglands were identified and preserved. The thyroid gland was resected from top to bottom under the guidance of the recurrent laryngeal nerve and the central lymph nodes of the affected side were dissected. The specimen was removed from the observation port in a dedicated specimen bag.
The operation area was rinsed with sterile distilled water, and drainage tubes were placed in the thyroid surgical bed9. A negative pressure ball was attached externally. The linea alba cervicalis was sutured with inverted stitches, the trocars were removed, the incision was disinfected with iodophor, and the oral mucosa was closed with absorbable sutures.
Postoperative management
Prophylactic antibiotics were administered for 24 h postoperatively to prevent infection. Patients rinsed their mouths with a recovery solution daily and maintained a semi-liquid diet for the first 3 days postoperatively. On the second postoperative day, blood routine, electrolytes, thyroid function, and parathyroid hormone levels were checked. Calcium carbonate was administered symptomatically if there was evidence of hypocalcemia. Drainage tubes were removed if the drainage volume was less than 10 mL per day. Follow-up visits were scheduled for 1 month postoperatively and then every 3 months thereafter.
Observation indexes and evaluation criteria
The operation time and bleeding amount were recorded for the three groups. Postoperative hospital stay, postoperative drainage volume, and the number of retrieved and metastatic central lymph nodes were also documented. Postoperative complications, such as hypoparathyroidism, subcutaneous fluid accumulation, recurrent laryngeal nerve (RLN) injury, mental nerve injury, and infection, were recorded for all three groups.
Permanent hypoparathyroidism was defined as subnormal intact parathyroid hormone serum concentrations persisting more than six months after the operation. Permanent RLN palsy was defined as failure to recover vocal cord function within six months10. Postoperative re-examination included measurements of thyroglobulin (Tg), anti-thyroglobulin antibodies and thyroid-stimulating hormone, as well as ultrasonography/CT of the neck operation field. A significant rise in Tg levels and the presence of a significant mass or enlarged lymph nodes on ultrasonography/CT were used as indicators of recurrence11.
Statistical analysis
All data were statistically analyzed using SPSS 26.0 software. Quantitative data are expressed as mean ± SD, classification data are expressed as n (%). One-way ANOVA or chi-square test was used for comparison between multiple groups, and t test or Fisher’s exact test was used for comparison between two groups. Statistical significance was accepted at a P value < 0.05.
Results
Demographics and clinical characteristics
During the study period, 90 patients underwent TOETVA and none of the patient required conversion to open thyroidectomy. There were 8 male patients and 82 female patients, with a mean age of 32.7 ± 6.1 years (range, 21–44 years). There were no significant differences among the three groups in terms of sex, age, BMI and tumor site (Table 1).
Surgical data
Among the three groups, the operation time of group A was the shortest (A = 98.3 ± 17.3 vs. B = 109.3 ± 22.5 vs. C = 114.3 ± 20.7, mins, p = 0.0102). There was no significant difference in intraoperative blood loss among the three groups (Table 2).
Postoperative data
Among the three groups, patients in group A had the least postoperative drainage volume (A = 70.4 ± 17.8 vs. B = 83.1 ± 18.9 vs. C = 89.3 ± 20.3, ml, p = 0.0102), and the shortest postoperative hospital stay (A = 3.4 ± 0.8 vs. B = 4.1 ± 1.1 vs. C = 4.3 ± 1.0, days, p = 0.0102). There was no significant difference in the total number of dissected central lymph nodes and the number of metastatic central lymph nodes among the three groups (Table 3).
Complications and recurrence
There was no significant difference in postoperative temporary RLN palsy and hypoparathyroidism among the three groups. There was one case of subcutaneous effusion in group B and C, respectively, which recovered after drainage with a syringe. At 6-month postoperative follow-up, all patients were not seen permanent RLN palsy, hypoparathyroidism, lower lip and chin skin numbness and other complications. No recurrence was found in all patients (Table 4).
Discussion
TOETVA is highly favored for its excellent cosmetic results and minimal scarring. In 2018, the Thyroid Surgery Committee of the Chinese Medical Doctor Association’s Division of Surgeons formulated the “Expert Consensus on Transoral Endoscopic Thyroidectomy Vestibular Approach” to further standardize the practice of TOETVA in China12. TOETVA utilizes three trocars, all located in the oral vestibule, the central trocar serves as the observation port, while the lateral trocars are the operation ports13. Compared to other approaches in endoscopic thyroid surgery, the shorter distance between the observation and operation ports in TOETVA can lead to the “chopstick effect”, which increases the technical complexity of the surgery14.
The so-called “chopstick effect” refers to the difficulty of maneuvering instruments within a confined space when the instruments (such as surgical tools) are positioned too close to each other15. This effect is akin to using chopsticks to pick up an item when the tips of the chopsticks are too close together, thereby limiting the flexibility and precision of the movement. This effect is particularly pronounced in TOETVA and can lead to several issues, including limited operating space, where the short distance between the observation port and the operation ports restricts the space available for maneuvering the surgical instruments, thereby increasing the difficulty and precision required for the operation. Additionally, the interference between surgical instruments can obstruct the surgical view, impacting the accuracy and safety of the procedure16. Furthermore, the proximity of the instruments increases the likelihood of collisions during the operation, which not only affects the smoothness of the procedure but can also cause damage to the instruments.
Due to the flexibility of the oral cavity, the positioning of the operation ports in TOETVA can vary, resulting in a variable distance between the operation ports and the observation port. The greater the distance between these ports, the less pronounced the chopstick effect, and the less interference occurs between the surgical instruments and the camera. However, the expansion of the oral cavity has its limitations. When the operation ports are placed too far apart, the repeated stretching of the corners of the mouth during surgery can lead to postoperative discomfort, such as peri-oral swelling. Conversely, if the distance between the operation ports and the observation port is too short, the chopstick effect becomes more pronounced, making the surgical procedure more difficult and potentially increasing surgical trauma.
Current experience suggests that positioning the operation ports near the first premolars is optimal, with this location being approximately 2.5 cm from the midline. However, there is a lack of sufficient clinical data to confirm this viewpoint. Therefore, this study aims to compare the effects of different distances between the operation ports on surgical outcomes, in order to determine the optimal positioning of the operation ports in TOETVA.
The study results showed no significant differences in intraoperative blood loss and the number of lymph nodes dissected among the different groups. Additionally, none of the patients experienced severe complications or tumor recurrence and metastasis postoperatively, indicating that different positions of the operation ports can ensure the safety and thoroughness of the surgery. However, it is noteworthy that when the distance between the lateral Trocars and the midline was approximately 2.5 cm (2.3–2.7 cm), the surgery time was shortest, and surgical efficiency was highest. This may be because when the operation ports and the observation port are closer together (Group B), the chopstick effect becomes more pronounced, increasing the interference between the surgical instruments and the camera, thus prolonging the operation time.
Although more lateral placement of the incisions, as suggested in previous study17, can minimize mental nerve injury and reduce instrument collision, our study found that when the distance between the operation ports and the observation port was greater (Group C), the surgery time was actually longer, despite the theoretical reduction of the “chopstick effect” with increasing distance. Upon further analysis of the surgical procedure, we speculated two potential contributing factors to this phenomenon:
Firstly, as the distance between the operation ports and the observation port increases, the Trocars move closer to the corners of the mouth, making it easier for the operation to be constrained by the perioral region, thus affecting the surgical procedure. A more laterally placed incision increases the tension and stretching exerted on the tissues around the corner of the mouth during instrument manipulation. This heightened tension not only raises the risk of postoperative oral discomfort but also makes the perioral region more susceptible to soft tissue trauma, bruising, or delayed healing. Secondly, a greater distance between the operation ports and the observation port leads to increased interference from the trachea during the operation. During TOETVA, the operator stands on the head side to perform top-down operations, with symmetrical distribution of instruments on both sides. Therefore, regardless of which side of the thyroid surgery is being performed, one side of the instruments needs to cross over the trachea to operate on the opposite side (Fig. 2). Due to the triangular anatomical features of the mandible and the anatomical relationship between the trachea and the thyroid (with the thyroid lobes located on either side of the trachea), it can be observed from the coronal plane that when the operation ports on both sides are further away from the midline, the positions of the instruments on both sides gradually move outward and downward, descending below the level of the trachea (Fig. 3). A more lateral incision places the trocar path further posterior along the mandibular contour, and in a supine position, this trajectory positions the instruments beneath the tracheal level. This increases the likelihood of instrument-tissue collision, raising the risk of iatrogenic tracheal injury. Furthermore, this positioning complicates central lymph node dissection across the trachea, increasing the difficulty of the procedure, potentially prolonging the surgical time, and heightening the overall complexity of the operation.
Schematic diagram of port placement for TOETVA. The schematic diagram illustrates the port placement in TOETVA. The observation port is positioned centrally in the oral vestibule, while the operation ports are placed symmetrically on either side. The mandible and trachea are labeled to show the anatomical relationships.
With the increasing penetration of Enhanced Recovery After Surgery (ERAS) concepts, there is a growing focus on postoperative recovery, and the length of hospital stay (LOS) after surgery is often considered a key indicator of surgical recovery and patient rehabilitation18. A more efficient surgical process is typically associated with shorter hospital stays because it helps reduce tissue damage, postoperative pain, and the occurrence of complications19. In this study, we observed that patients in Group A had significantly lower postoperative drainage and shorter hospital stays compared to the other two groups. This is consistent with the emphasis of ERAS on the efficiency of surgical procedures and minimally invasive principles.
The observed reduction in postoperative drainage volume with the optimal port distance (2.3–2.7 cm) can be attributed to several factors. First, precise port placement ensures smoother surgical manipulation and minimizes trauma to adjacent tissues, thereby reducing vascular and lymphatic injury. This advantage is further supported by the stable intraoperative working space provided by this configuration, which helps prevent accidental damage to non-target areas. Conversely, suboptimal port placement may result in awkward instrument angles, increasing surgical difficulty and the risk of unintended dissection. By optimizing ergonomics, the ideal port distance not only minimizes tissue trauma but also enhances surgical safety and efficiency.
Notably, in the Chinese healthcare context, patients are generally discharged after extubation, with drainage volume serving as the primary criterion for tube removal20. An optimal port distance facilitates reduced surgical trauma, leading to lower postoperative drainage volumes. This allows for earlier tube removal, thereby accelerating patient discharge. Standardized treatment protocols not only expedite recovery but also alleviate the financial burden on patients. Furthermore, reducing postoperative hospital stays enhances the overall recovery experience while demonstrating greater healthcare service efficiency21. Defining the optimal port distance in TOETVA procedures can thus improve surgical outcomes, increase patient satisfaction, and optimize resource utilization, ultimately benefiting the entire healthcare system.
It is important to note that while the variation in distance between the operation and observation ports resulted in changes in surgical time, postoperative drainage volume, and length of hospital stay among the three groups, there were no significant differences observed in intraoperative blood loss and postoperative complications. This could be attributed to the fact that although different distances may impact the surgical procedure, the lead surgeons in our study were proficient in TOETVA techniques and possessed extensive surgical experience. They were able to perform the surgeries proficiently under varying circumstances. Despite potential differences in surgical difficulty, the surgeries were successfully completed owing to the expanded field of view and precise anatomical visualization provided by the endoscopic system. However, for beginners in TOETVA, we recommend placing the operation ports approximately 2.5 cm (range 2.3–2.7 cm) from the midline on both sides, as this helps improve surgical maneuverability and facilitates smooth completion of the procedure.
There are several limitations to this study. Firstly, as it was a single-center retrospective study with a relatively small sample size, the generalizability of the research findings may be limited. Conducting larger-scale studies with multi-center participation could enhance the persuasiveness of the results. Secondly, although postoperative follow-up did not indicate tumor recurrence or metastasis, long-term follow-up data were not included, necessitating further observation for the long-term prognosis of the surgical outcomes. Additionally, this study did not classify patients based on their mandibular shape. While previous research suggests that patients with different mandibular contours can achieve safe and effective surgical outcomes with TOETVA, whether mandibular shape influences surgical procedures warrants further investigation. Lastly, it should be noted that variations in oral structure and neck length among different patients may influence surgical outcomes, highlighting the need for further research attention to this factor in future studies.
Conclusion
This study has provided valuable insights into optimizing TOETVA surgery by delineating the optimal positions of the operating ports, thereby enhancing the standardization and controllability of the procedure. This offers a novel approach for refining the techniques of endoscopic thyroidectomy and lays the groundwork for the standardization and refinement of TOETVA. Future endeavors will involve multicenter studies with larger sample sizes to further validate these findings, thereby promoting the standardized application of TOETVA in thyroid surgery.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- TOETVA:
-
Transoral endoscopic thyroidectomy vestibular approach
- PTC :
-
Papillary thyroid carcinoma
- RLN :
-
Recurrent laryngeal nerve
- Tg :
-
Thyroglobulin
- ERAS :
-
Enhanced recovery after surgery
- LOS :
-
length of hospital stay
References
Global Burden of Disease Cancer C et al. Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the global burden of disease study 2019. JAMA Oncol.8(3), 420–444 (2022).
Yu, X. et al. Comparison of different mandibular jawlines classifications on transoral endoscopic thyroidectomy for papillary thyroid carcinoma: Experiences of 690 cases. Front. Endocrinol. (Lausanne)13, 842148 (2022).
Anuwong, A. et al. Safety and outcomes of the transoral endoscopic thyroidectomy vestibular approach. JAMA Surg.153(1), 21–27 (2018).
Li, X., Ding, W. & Zhang, H. Surgical outcomes of endoscopic thyroidectomy approaches for thyroid cancer: A systematic review and network meta-analysis. Front. Endocrinol. (Lausanne)14, 1256209 (2023).
Lee, S. H., Moorthy, R. & Nagala, S. Evolution of transoral endoscopic thyroidectomy vestibular approach according to the IDEAL framework. Br. J. Surg.109(6), 497–502 (2022).
Zheng, G. et al. Safety and surgical outcomes of transoral endoscopic thyroidectomy vestibular approach for papillary thyroid cancer: A two-centre study. Eur. J. Surg. Oncol.47(6), 1346–1351 (2021).
Cuschieri, S. The STROBE guidelines. Saudi J. Anaesth.13(Suppl 1), S31–S34 (2019).
Peng, X. et al. The clinical application of mental nerve dissection in transoral endoscopic thyroidectomy via an oral vestibular approach. Surg. Endosc.34(1), 153–158 (2020).
Liu, Z. et al. Postoperative drain after transoral endoscopic thyroidectomy vestibular approach (TOETVA) with single incision. Surg. Endosc.35(1), 358–366 (2021).
Sun, H. et al. Comparison between transoral endoscopic thyroidectomy vestibular approach (TOETVA) and conventional open thyroidectomy for patients undergoing total thyroidectomy and central neck dissection: A propensity score-matching analysis. Front. Oncol.12, 856021 (2022).
Peiris, A. N., Medlock, D. & Gavin, M. Thyroglobulin for monitoring for thyroid cancer recurrence. JAMA321(12), 1228 (2019).
Wang, P. et al. Expert consensus on transoral endoscopic thyroidectomy vestibular approach (2018). Chin. J. Pract. Surg.38(10), 1104–1107 (2018).
Moreno Llorente, P. et al. Transoral endoscopic thyroidectomy vestibular approach (TOETVA). Cir. Esp. (Engl. Ed.)100, 234 (2021).
Li, X. L. et al. Preliminary application of transoral robotic thyroidectomy: Experience from an initial 30 cases. Zhonghua Wai Ke Za Zhi59(12), 994–998 (2021).
Liu, Y. & Zhang, Z. T. Problems and strategies of laparoendoscopic single site surgery in gastrointestinal surgery. Zhonghua Wei Chang Wai Ke Za Zhi16(10), 915–918 (2013).
Lin-Juan, H., Xue-Lin, D. & Jun-Ying, T. Trinity and the chopsticks effect in laparoendoscopic single-site surgery. Med. Philos. (B)39(09), 76–77+86 (2018).
Zhang, D. et al. Indications, benefits and risks of transoral thyroidectomy. Best Pract. Res. Clin. Endocrinol. Metab.33(4), 101280 (2019).
Chorath, K. et al. ERAS protocols for thyroid and parathyroid surgery: A systematic review and meta-analysis. Otolaryngol. Head Neck Surg.166(3), 425–433 (2022).
Ding, Y. et al. Assessment of ESGO quality indicators in cervical cancer surgery: A real-world study in a high-volume Chinese hospital. Front. Oncol.12, 802433 (2022).
Yu, H. W. et al. Robotic-assisted modified radical neck dissection using a bilateral axillo-breast approach (robotic BABA MRND) for papillary thyroid carcinoma with lateral lymph node metastasis. Surg. Endosc.32(5), 2322–2327 (2018).
McMullan, R. et al. Resource utilisation, length of hospital stay, and pattern of investigation during acute medical hospital admission. Postgrad. Med. J.80(939), 23–26 (2004).
Contributions to the literature
Identifies the optimal distance between observation and operation ports in TOETVA (2.3–2.7 cm), enhancing surgical efficiency and reducing surgical trauma. Provides a standardized guideline for trocar placement in TOETVA, improving consistency and safety. Contributes to the broader adoption and refinement of TOETVA, leading to better clinical outcomes and patient satisfaction.
This study provides valuable insights into the optimization and standardization of port placement in TOETVA procedures. By systematically analyzing the impact of different distances between the observation and operation ports on surgical outcomes, this research identifies an optimal port configuration that enhances both operational efficiency and patient recovery. The findings contribute to the growing body of evidence supporting minimally invasive thyroid surgery, offering a data-driven recommendation for port placement that can be adopted in clinical practice. Moreover, by promoting a standardized approach to TOETVA, this study helps reduce operative time, decrease postoperative drainage, and shorten hospital stays, aligning with the principles of Enhanced Recovery After Surgery and ensuring more consistent and effective patient outcomes.
Funding
This research was funded by Hunan Provincial Natural Science Foundation of China (Grant No. 2023JJ60331), Hunan Cancer Hospital Climb Plan (Grant No. ZX2020002) and Hunan Provincial Health High-Level Talent Scientific Research Project (Grant No. R2023115).
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
The study was approved by the Medical Ethics Committee of the First People’s Hospital of Chenzhou and the subjects gave their informed consent for participation.
Consent for publication
Written informed consent was obtained from all individual patients included in this study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Deng, Z., Hu, X., Zeng, F. et al. Determining the optimal port placement for transoral endoscopic thyroidectomy vestibular approach in a retrospective study. Sci Rep 15, 6948 (2025). https://doi.org/10.1038/s41598-025-91392-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91392-3