Abstract
Hand dexterity impairments in patients with stroke reduce activities of daily living (ADL) and quality of life. Visuospatial ability is associated with motor learning, but this has not previously been reported in patients with subacute stroke. We aimed to investigate whether visual terminal feedback (FB) affected motor learning of hand dexterity and the relationship among visuospatial ability. Overall, 17 subacute stroke patients (age: 66.1 ± 13.8 years) with mild upper limb motor impairment were included. The experimental task was the grasping force control task. The visuospatial task was the Rey–Osterrieth Complex Figure Test (ROCFT). The experimental protocol was conducted in 2 consecutive days: day 1 consisted of a pre-test (PRE), practice, and short-term retention test (SRT), and day 2 consisted of a long-term retention test (LRT) and the ROCFT. Grasping errors were significantly decreased in the SRT and LRT than in the PRE. Furthermore, ROCFT scores (copy and recall) and LRT grasping errors were moderately negatively correlated (ρ = -0.51 and − 0.53). In conclusion, visuospatial ability is an important factor associated with motor learning in subacute stroke patients. Future studies should use visual terminal FB, and training programs for visuospatial ability should be considered in stroke rehabilitation.
Similar content being viewed by others
Introduction
The incidence of stroke is increasing worldwide, and stroke adversely affects many patients1. Approximately 85% of stroke survivors experience motor paralysis of the upper extremities, and 50% still have residual motor deficits more than 6 months after onset2. Particularly, patients have difficulty improving movements that require hand dexterity, such as manipulating objects and grasping. Such reduced hand activity results in reduced activities of daily living (ADLs) and quality of life3. Pennati et al.4investigated changes in the sensorimotor function and precision grasping ability of the upper extremities and hands over a 6-month period post-stroke and found that precision grasping remained impaired even in patients with improved sensorimotor function. Patients with stroke have impaired hand coordination of the paralyzed upper extremity when performing actions such as grasping objects and using tools. This can lead them to avoid using the paralyzed upper extremity and to compensate by using the non-paralyzed upper extremity, causing learned non-use of the paralyzed upper extremity5. Therefore, training using coordinated movements of the paralyzed hand is important for improving hand dexterity in patients with stroke.
Task-specific training is a common strategy for improving hand coordination in patients with stroke6. It is used to improve motor skills in tasks based on real-life environmental conditions. In a systematic review of task-oriented training components for upper extremity and hand motor skills in patients with stroke, Timmermans et al.6reported that feedback (FB) on performance has a strong therapeutic effect. FB facilitates motor learning and can be classified into two main categories: intrinsic and extrinsic. Intrinsic FB represents sensory information that individuals obtain from their own movement, whereas extrinsic FB represents information provided externally as instructions about movement results, such as knowledge of results (KR) and knowledge of performance (KP)7. Extrinsic FB includes various FB strategies, such as the timing and frequency of FB provision.
Previous randomized controlled trials have focused on upper-limb and hand motor function in patients with subacute stroke and have compared the improvement of motor function in conditions with and without task-oriented training. However, the details of FB strategies, such as frequency and timing of FB, are unknown8,9,10. In a previous study focusing on the effects of FB on upper-limb motor learning and hand coordination, 37 patients with chronic stroke were classified into three different FB conditions (KR, KR + KP, and no KR), and their performance on a finger-reaching task using the paralyzed upper limb was compared. The KR and KR + KP groups showed greater improvement than the no KR group with respect to movement accuracy and movement time reduction at post-test (after 2 weeks) and retention test (after 1 month)11.
Furthermore, a previous study comparing performance in a finger-reaching task among 28 patients with chronic stroke in two different FB conditions (KR and KR + KP groups) showed that only the KR + KP group had improved motor patterns12. However, negative effects of extrinsic FB in patients with chronic stroke have also been reported. A study of the effects of FB and no-FB conditions on motor learning in an upper-limb tracking task in patients with chronic stroke showed that motor learning was inhibited in the FB condition13,14. In summary, there is no consistent consensus on FB strategies to enhance motor learning of the upper extremities and hand coordination in patients with subacute and chronic stroke.
Visuospatial ability has recently attracted attention as a factor that enhances motor learning15,16,17,18. Visuospatial ability is an important component that includes various cognitive functions that aid the encoding of visual images19and are involved in integrating the location of oneself with objects and tools. The superior and inferior parietal lobes have been shown to be responsible for this function in brain regions20. Visuospatial ability has been assessed using neuropsychological assessment tools such as the Montreal Cognitive Assessment (MoCA), Mental Rotation (MR), and the Rey–Osterrieth Complex Figure Test (ROCFT)21. The ROCFT specializes in the assessment of visuospatial functions, including visuospatial construction and visuospatial memory, compared to other neuropsychological assessments. The measurement time is approximately 5–10 min, so therapists can conveniently use it in clinical settings22. Particularly, the ROCFT result has been found to be an important predictor of motor learning capacity in older individuals15,18. Furthermore, VanGilder et al.16 validated a predictive model of motor learning in patients with chronic stroke and showed that the ROCFT scores were a factor in constructing a well-fitting model.
However, the relationship between visuospatial ability and motor learning in patients with subacute stroke (< 6 months) remains unclear. The patients in the study by VanGilder et al. were in the chronic phase (mean time since onset: 3.8 years) and were younger (mean age: 58.4 years) than the cohort in the present study. The sample size was also small (n = 7). Validating the relationship between visuospatial ability and motor learning can confirm that visuospatial ability is an important component of hand coordination rehabilitation in patients with stroke during the recovery phase. Thus, as a preliminary study, we aimed to clarify FB strategies that enhanced the motor learning of hand coordination and to determine the relationship between visuospatial ability and motor learning in patients with subacute stroke. We hypothesized that the use of visual terminal FB in patients with stroke would improve the ability to adjust the grasping force, even in patients with motor impairments. We also hypothesized that the relationship between visuospatial ability and motor learning in patients with stroke would be positive, with higher visuospatial ability correlating with higher motor learning ability.
Results
Participant characteristics
A total of 19 patients with subacute stroke were included from July 2021 and August 2022. However, one patient was discharged before motor function evaluation, and one patient withdrew during the experiment. Consequently, 17 patients (8 males/9 females) with a mean age of 66.1 ± 13.8 years completed the trial. Figure 1 shows the participant recruitment process. Table 1 presents the participant characteristics. The participants had mild motor deficits in the upper extremities of the paralyzed side. There were six participants with right hemiplegia and 11 participants with left hemiplegia.
Change in ability to adjust grasping force
Figure 2 shows the root mean square error (RMSE) values for the test and practice blocks. According to the Shapiro–Wilk test, the pre-test (PRE, p = 0.022), short-term retention test (SRT, p = 0.002), long-term retention test (LRT, p = 0.045), Block 3 (p = 0.021), Block 4 (p = 0.033), and Block 5 (p = 0.013) data were not normally distributed, whereas data from Blocks 1 (p = 0.271) and 2 (p = 0.338) were normally distributed. The results of the Friedman test showed a significant main effect (F = 23.65, df = 2, p < 0.001). In addition, the post hoc test revealed significant differences between the PRE and SRT (p < 0.001) and between the PRE and LRT (all p < 0.001) (Fig. 2a). Meanwhile, there were no significant differences between the SRT and LRT (p = 0.330). The practice block also showed a significant main effect (F = 26.682, df = 4, p < 0.001) (Fig. 2b). Post hoc tests showed significant differences between Block 1 and all other blocks (Block 1 vs. Block 2: p = 0.003, Block 1 vs. Block 3: p = 0.002, Block 1 vs. Block 4: p = 0.005, Block 1 vs. Block 5: p = 0.003).
Change in ability to adjust grasping force. (a) Results of grasping errors. The center line shows the median value. Whiskers indicate values below 1.5 times the interquartile range (IQR) above the first quartile and up to 1.5 times the IQR above the third quartile; data beyond this are shown as outliers, indicated by black points. Abbreviations: PRE, pre-test; SRT, short-term retention test; LRT, long-term retention test. (b) Results of grasping errors in each practice block. Abbreviations: B1–B5, Block 1–5.
Relationship of test performance with motor function and visuospatial ability
Figure 3 shows the correlations among test performance, motor function (Fugl–Meyer Assessment for the Upper Extremity [FMUE] and Action Research Arm Test [ARAT]), and visuospatial ability (copy score, organization score, and 3-min delayed-recall score). Spearman’s rank correlation coefficients revealed a moderately negative correlation of performance in the LRT with the copy score (p = 0.038, ρ = −0.51) and the 3-min delayed-recall score (p = 0.028, ρ = −0.53). No significant correlations were found between test performance and motor function parameters as well as between pre-test and SRT performance and visuospatial ability.
Correlation of test performance with motor function and visuospatial function. Values in tiles indicate Spearman rank correlation coefficients. Combinations showing significant correlations are color coded, with Spearman’s rank correlation coefficients close to 1 shown in red and those close to −1 shown in blue. Combinations that do not show significant correlations are shown in white. Abbreviations: PRE, pre-test; SRT, short-term retention test; LRT, long-term retention test; FMUE, Fugl–Meyer assessment for upper extremity; ARAT, Action research arm test; Copy, copy score; ORG, organization score; Recall, 3-min delayed-recall score.
Discussion
The relationship between visuospatial ability and motor learning in patients with subacute stroke (< 6 months) remains unclear. This study showed that visual terminal FB enhanced motor learning of the ability to adjust grasping force in patients with subacute stroke. Furthermore, although motor function was not associated with motor learning ability of adjusting the grasping force, visuospatial ability was associated with this ability. There was better improvement in the ability to adjust the grasping force in the SRT and LRT than in the PRE. These results support the appropriateness of an FB strategy.
FB timing can be classified into concurrent FB (FB given during the trial) and terminal FB (FB given after the trial is completed)23. In visual FB, concurrent FB better improved performance during practice than did terminal FB. However, visual concurrent FB has been shown to make learners dependent on extrinsic FB, thus overlooking intrinsic FB (i.e., proprioception) and inhibiting motor learning23. Our result was similar to those of previous studies on older individuals and patients with stroke24,25. In contrast, visual terminal FB has been shown to enhance motor learning in movement tasks with a simple task complexity by facilitating visuomotor transformations, thus improving the preplanning of movements in the next trial26. Furthermore, with respect to FB frequency, previous research has shown that granting FB in all practice trials (i.e., 100% FB) inhibits motor learning27. However, a meta-analysis showed no differences in motor learning according to FB frequency28. The participants in this study were older and had mild upper-extremity motor impairments, based on age and FMUE results29. Rehabilitation in older patients with stroke provides functional improvement; however, this improvement decreases with increasing age30. The current study, which included older patients with subacute stroke and mild motor impairments, suggested that FB strategies are effective in enhancing motor learning.
The results of this study also showed a moderate positive correlation between visuospatial ability and performance in adjusting grasping force, but there was no correlation between motor function and performance in adjusting grasping force. These results suggest that visuospatial ability is a more important factor in motor learning than motor function or pre-test task performance in patients with subacute stroke. Other methods have been used to assess visuospatial ability, such as the MoCA and MR. However, the ROCFT can evaluate visuospatial construction and memory in visuospatial ability21. Visuospatial construction is used to understand the presented visual FB rapidly. Participants need to recognize the grasping error within the short presentation time (10 s) of the FB after the trial ends. This suggests that visuospatial construction contributes to rapid visual FB screen recognition. Visuospatial memory might have contributed to the correct encoding of the presented visual FB, and the retention and recall of important information for motor planning for the next trial. Both visuospatial construction and memory involve the superior and inferior parietal lobe regions, which translate visual information into limb movements31,32. Furthermore, visuospatial training suggests improving visuospatial function by enhancing the activity of the prefrontal cortex and the functional connectivity of the frontoparietal circuit33,34. Therefore, visuospatial training for patients with subacute stroke should be considered for rehabilitation.
However, few studies have focused on the relationship between visuospatial ability and motor learning in patients with stroke, with only one study including a small number of patients with chronic stroke (n= 7)16. Compared with previous studies on motor learning in patients with stroke, this study included a larger number of patients in the recovery phase (n = 17), increasing the reliability of the results.
This study had some limitations. First, no control conditions, such as a control group or concurrent FB group, were included. Furthermore, FB was not used in the test phase to establish an experimental schedule that reflects a rehabilitation setting, and data were collected under a single condition using terminal FB alongside an assessment of motor function and visuospatial function. Future research should examine the disease’s effect on visuospatial function and hand dexterity by using healthy individuals of the same age and sex. Moreover, setting FB conditions other than visual terminal FB would make this study more meaningful. Second, patients with stroke or severe motor impairments and non-subacute stroke were excluded. Based on the inclusion and exclusion criteria, only patients with subacute stroke who could manipulate the grasping device were included. Patients with stroke accompanied by severe motor impairments had difficulty using the grasping device independently. Rehabilitation programs using virtual reality (VR) have introduced new possibilities35. VR training has proven effective in improving motor function, yet has not assessed visuospatial function. VR relies heavily on visuospatial function, so it is important to clearly evaluate this function and understand the training mechanism. In future research, examining the effectiveness of rehabilitation programs addressing visuospatial function in patients with severe stroke is key to fostering better recovery in patients. Therefore, our findings should be cautiously considered for different attributes, such as motor function (severe or moderate) and stage (acute or chronic). Future studies should examine FB strategies that enhance motor learning in patients with stroke in different movement tasks, with assessment of visuospatial ability, and visuospatial ability training methods that enhance motor learning.
Conclusions
Task-specific training using visual FB is effective for patients and indicates that visuospatial ability, rather than motor function, is related to motor learning. Thus, training programs for visuospatial ability should be considered in stroke rehabilitation.
Methods
Ethics
This study was approved by the Ethics Committee of the Ibaraki Prefectural University of Health Sciences (approval number: 995) and was registered in the UMIN clinical trial (UMIN000049991). The experimental design was conducted in accordance with the principles of the Declaration of Helsinki. All participants provided written informed consent after adequate explanation of the conditions of participation in the study.
Participants
This study was conducted at Ibaraki Prefectural University Hospital, which had a convalescent rehabilitation ward36. All patients were diagnosed with stroke by their previous physician and transferred to Ibaraki Prefectural University Hospital for rehabilitation, where physical therapy, occupational therapy, and speech therapy were initiated. Patients admitted to the hospital between July 2021 and August 2022 were consecutively screened. The sample size was based on the study by Riga et al.37, who set up an experimental design similar to this study, as there were no previous studies using the same experimental design. The inclusion and exclusion criteria for the current study were set according to those described by Tabu et al.38. The inclusion criteria were as follows: (1) ability to understand verbal instructions; (2) absence of any disease that interfered with task performance, such as hand pain; (3) mild motor paralysis in the paralyzed upper limb and fingers (Brunnstrom recovery stage 4 or higher); (4) ability to extend the wrist joint on the paralyzed side by 20° or more voluntarily; (5) ability to extend the proximal interphalangeal joints and metacarpophalangeal joints of the first to third fingers voluntarily by at least 10° on the paralyzed side; and (6) ability to sit independently. The exclusion criteria were as follows: (1) previous experience with a similar task, (2) orthopedic or neurological disease of the hand that interfered with daily life on the non-paralyzed side, (3) cognitive impairment (Mini Mental State Examination score < 21), (4) visual impairment (hemianopsia, diplopia, and reduced visual acuity) that prevented them from seeing the monitor, and (5) deemed unsuitable for study participation by the attending investigator.
Equipment
The grasping force was quantitatively measured using a device from iWakka (Nagoya Institute of Technology, Japan). This device consisted of a monitor, grasping device, control box, and Windows PC (Microsoft, Redmond, WA) with the iWakka Viewer application installed. The grasping device had a height of 80 mm, a diameter of 65 mm, and a weight of 0.112 kg. The force of grasping could be visualized by measuring the strain of the plate spring produced when the grasping device was opened and closed with a strain gauge, and a maximum grasping force of 0.5 kg could be measured (Fig. 4a). In previous studies, this device was used to evaluate and practice the ability to adjust the grasping force in healthy young and older adults and patients with stroke39,40,41,42. The sampling frequency was 10 Hz, and the spring constant of the plate spring was 4.82 × 102 N/m. The measurement environment was based on the report of Yamamoto et al.41. Particularly, the participants placed the device on a table with an aluminum plate to reduce the effects of friction and performed the task while seated in a chair. The participants and could check the difference between the target grasping force and the measured grasping force (grasping error) reflected on the monitor as visual FB and were expected to improve their task performance by adjusting their movement for the next trial (Fig. 4b).
Experimental equipment and experimental environments. (a) Grasping device (right) and control box (left). We can quantitatively assess the participant’s grasping force in the range of 0–0.5 kg. (b) Feedback during the experimental task. Participants receive feedback on how accurately they adjusted the measured grasping force (red line) relative to the target grasping force (blue line).
Experimental design
This study was conducted over 2 consecutive days. The participants completed the Edinburgh Handedness Test (EHI), PRE, practice, and SRT on day (1) The LRT and visuospatial ability assessment were completed on day (2) The EHI was used to assess handedness. After EHI, the participants performed a familiarization task in which they grasped the grasping device for 10 s at a force of 0.1 kg, without viewing the monitor, for five trials. The experimental task, including familiarization, was performed using the paralyzed upper limb. The results were not provided to the participants. The experimental task started after the completion of five trials of the familiarization task.
Experimental task
Figure 5 shows the experimental tasks performed in this study. The task trial consisted of adjusting the grasping force for 30 s, 10 s for each waveform, in the order of 0.1, 0.4, and 0.25 kg target grasping force. The participants performed the task without viewing the monitor during the task trials. The trial results were provided to the participants after trial completion. FB was provided by presenting the trial results on the monitor for 10 s. A metronome (6 bpm) was used to signal the change in the target grasping force. This allowed the participants to change their adjusted grasping force in accordance with the timing of the change in the target grasping force. Specifically, the purpose of this task was to learn coordinated hand movements by trying to bring the measured grasping force as close to the target grasping force as possible, based on the tactile and motor sensations that occur when grasping devices.
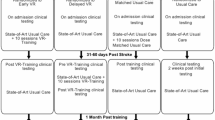
The test phase (PRE, SRT, and LRT) consisted of 3 trials, each without FB, and the practice phase consisted of 15 trials (5 practice blocks × 3 trials per block) with FB. The interval between trials was 10 s. For the practice trials, the next trial started 15 s after the end of the feedback period, and the interval between practice blocks was 1 min. The PRE was conducted to assess the pre-practice conditions. The SRT and LRT were conducted to assess the immediate and long-term effects of practice, respectively. The SRT was conducted 5 min after the completion of the last trial (15th trial) of the fifth practice block, and the LRT was conducted 24 h after the SRT was completed (Fig. 6).
Experimental schedule. The participants perform the pre-test (PRE), practice test, and short-term retention test (SRT) on day 1 and the long-term retention test (LRT) and Rey–Osterrieth Complex Figure Test (ROCFT) on day 2. One block consists of three trials, with one block for each of the three tests (PRE, SRT, and LRT) and five blocks (B1 to B5) for the practice test. SRT is conducted 5 min after completion of the last trial of the practice test, and LRT is conducted 24 h after the SRT.
The ROCFT is a neuropsychological assessment of visuospatial ability (visuospatial construction and memory) that consists of copy and recall trials43. In this study, a copy trial and a 3-min delayed-recall trial were implemented. Previous studies have shown that information is forgotten by 2–3 min after the end of the copy trial44and that performance does not differ between a 3-min and a 30-min delayed-recall trial in various age groups (18–74 years)45. Therefore, a recall trial was performed 3 min after the end of the copy trial. During the copy task, the order of descriptions was recorded using a video camera. To prevent participants from noticing the replay task, a 10-item personality test46 was conducted between the copy and recall trials after completion of the copy trial. This prevented participants from noticing the presence of a recall trial.
Measurement outcome
The FMUE and ARAT were used to evaluate motor function. In a systematic review of the outcome measures of upper extremity function in patients with stroke, the FMUE was the most commonly used upper extremity function assessment tool, while the ARAT was a measure commonly used in combination with FMUE47. Motor function assessment was performed within 1 week prior to the start of the study. The RMSE was calculated from the absolute values of the target grasping force and the measured grasping force per unit time. A smaller RMSE thus indicated a greater ability to adjust the grasping force. We used the central 5-s interval of each target grasping force (e.g., for a 0–10-s interval, the interval from 2.5 to 7.5 s was used) as the analysis interval to exclude any deviation in grasping timing that occurred when the target grasping force switched.
Measurements of visuospatial ability included copy, organization, and 3-min delayed-recall scores on the ROCFT. The copy score indicated whether the participants were able to understand the form and relative position of each unit of the figure and copy it accurately. Meanwhile, the 3-min delayed-recall score indicated whether encoding of the copied figure, retention of the encoding memory, and recall of the retained memory were performed accurately. The scoring method for the copy and 3-min delayed-recall scores was based on the method of Loring et al.48 and used a 36-point scale. The organization score indicated the organizational strategy for how the figure was segmented and described when it was depicted. The scoring method for the organization score was based on the method of Chervinsky et al.49 and used a 36-point scale. Higher scores for each item indicated higher visuospatial ability.
Statistical analysis
First, the Shapiro–Wilk test was conducted to examine the normality of the RMSEs. Then, based on the results of the Shapiro–Wilk test, Friedman tests were conducted with the RMSE as the dependent variable and the tests (PRE, SRT, and LRT) and practice block (blocks 1–5) as factors to clarify the effects of practice and motor learning on the ability to adjust the grasping force. When significant differences were found in the Friedman test, the Wilcoxon signed-rank sum test with Holm’s correction was implemented. Next, Spearman’s rank correlation coefficients were calculated for performance on each test and motor function (FMUE, ARAT) and visuospatial ability (ROCFT) to clarify the relationship of performance on each test with motor function and visuospatial ability (copy score, organization score, and 3-min delayed-recall score). All analyses were performed using R software (version 4.3.1; R Core Team, Vienna, Austria). A p value of < 0.05 was considered statistically significant.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request (j.yabuki@mejiro.ac.jp).
Abbreviations
- ARAT:
-
Action Research Arm Test
- EHI:
-
Edinburgh Handedness Inventory
- FB:
-
feedback
- FMUE:
-
Fugl–Meyer assessment for the upper extremity
- KP:
-
knowledge of performance
- KR:
-
knowledge of results
- MR:
-
mental rotation
- MoCA:
-
Montreal Cognitive Assessment
- RMSE:
-
root mean square error
- ROCFT:
-
Rey–Osterrieth Complex Figure Test
References
Feigin, V. L. et al. World stroke organization (WSO): global stroke fact sheet 2022. Int. J. Stroke. 17, 18–29 (2022).
Birchenall, J. et al. Individual recovery profiles of manual dexterity, and relation to corticospinal lesion load and excitability after stroke –a longitudinal pilot study. Neurophysiol. Clin. 49, 149–164 (2019).
Ekstrand, E., Rylander, L., Lexell, J. & Brogårdh, C. Perceived ability to perform daily hand activities after stroke and associated factors: A cross-sectional study. BMC Neurol. 16, 208 (2016).
Pennati, G. V. et al. Recovery and prediction of dynamic precision grip force control after stroke. Stroke. 51, 944–951 (2020).
Rocha, L. S. O. et al. Constraint induced movement therapy increases functionality and quality of life after stroke. J. Stroke Cerebrovasc. Dis. 30, 105774 (2021).
Timmermans, A. A. A., Spooren, A. I. F., Kingma, H. & Seelen, H. A. M. Influence of task-oriented training content on skilled arm-hand performance in stroke: A systematic review. Neurorehabil Neural Repair. 24, 858–870 (2010).
Schmidt, R. A. & Lee, T. D. Motor Control and Learning: A Behavioral Emphasis 341–373 (Human Kinetics, 2019).
Michaelsen, S. M., Dannenbaum, R. & Levin, M. F. Task-specific training with trunk restraint on arm recovery in stroke: randomized control trial. Stroke. 37, 186–192 (2006).
McDonnell, M. N., Hillier, S. L., Miles, T. S., Thompson, P. D. & Ridding, M. C. Influence of combined afferent stimulation and task-specific training following stroke: A pilot randomized controlled trial. Neurorehabil Neural Repair. 21, 435–443 (2007).
Morris, J. H. et al. A comparison of bilateral and unilateral upper-limb task training in early poststroke rehabilitation: A randomized controlled trial. Arch. Phys. Med. Rehabil. 89, 1237–1245 (2008).
Cirstea, C. M., Ptito, A. & Levin, M. F. Feedback and cognition in arm motor skill reacquisition after stroke. Stroke. 37, 1237–1242 (2006).
Cirstea, M. C. & Levin, M. F. Improvement of arm movement patterns and endpoint control depends on type of feedback during practice in stroke survivors. Neurorehabil Neural Repair. 21, 398–411 (2007).
Boyd, L. A. & Winstein, C. J. Impact of explicit information on implicit motor-sequence learning following middle cerebral artery stroke. Phys. Ther. 83, 976–989 (2003).
Boyd, L. A. & Winstein, C. J. Providing explicit information disrupts implicit motor learning after basal ganglia stroke. Learn. Mem. 11, 388–396 (2004).
Lingo VanGilder, J., Hengge, C. R., Duff, K. & Schaefer, S. Y. Visuospatial function predicts one-week motor skill retention in cognitively intact older adults. Neurosci. Lett. 664, 139–143 (2018).
Lingo VanGilder, J., Lohse, K. R., Duff, K., Wang, P. & Schaefer, S. Y. Evidence for associations between Rey-Osterrieth complex figure test and motor skill learning in older adults. Acta Psychol. 214, 103261 (2021).
Wang, P., Infurna, F. J. & Schaefer, S. Y. Predicting motor skill learning in older adults using visuospatial performance. J. Mot Learn. Dev. 8, 38–51 (2020).
Wang, P., Lingo VanGilder, J., Schweighofer, N. & Schaefer, S. Y. Rey-Osterrieth complex figure recall scores and motor skill learning in older adults: A non-linear mixed effect model-based analysis. Hum. Mov. Sci. 86, 103004 (2022).
Perez, E. & Weisberg, S. M. Individual differences in Spatial navigation in Encyclopedia of the Human Brain (ed. Grafman, J. H.) 277–293 (Elsevier, 2025).
Vingerhoets, G. Contribution of the posterior parietal cortex in reaching, grasping, and using objects and tools. Front. Psychol. 5, 151 (2014).
Cimadevilla, J. M. & Piccardi, L. Spatial skills in Handbook of Clinical Neurology (ed. Lanzenberger, R., Kranz, G. S. & Savic, I.) 65–79 (Elsevier, 2020).
Zucchella, C. et al. Neuropsychological testing. Pract. Neurol. 18, 227–237 (2018).
Sigrist, R., Rauter, G., Riener, R. & Wolf, P. Augmented visual, auditory, haptic, and multimodal feedback in motor learning: A review. Psychon Bull. Rev. 20, 21–53 (2013).
Pellegrino, L., Giannoni, P., Marinelli, L. & Casadio, M. Effects of continuous visual feedback during sitting balance training in chronic stroke survivors. J. Neuroeng. Rehabil. 14, 107 (2017).
Ferris, J., Barone, V. J., Perkins, N. C. & Sienko, K. H. A pilot study comparing the effects of concurrent and terminal visual feedback on standing balance in older adults. Sensors. 22, 2826 (2022).
Rand, M. K. & Rentsch, S. Eye-hand coordination during visuomotor adaptation with different rotation angles: effects of terminal visual feedback. PLOS ONE. 11, e0164602 (2016).
Ong, N. T. & Hodges, N. J. Motor Learning in The Routledge International Encyclopedia of Sport and Exercise Psychology Volume 1: Theoretical and Methodological Concepts (ed. Hackfort, D. & Schinke, R.) 356–374 (Routledge, 2020).
McKay, B. et al. Meta-analysis of the reduced relative feedback frequency effect on motor learning and performance. Psychol. Sport Exer. 61, 102165 (2022).
Woytowicz, E. J. et al. Determining levels of upper extremity movement impairment by applying a cluster analysis to the Fugl-Meyer assessment of the upper extremity in chronic stroke. Arch. Phys. Med. Rehabil. 98, 456–462 (2017).
Zucchella, C. et al. Rehabilitation in oldest-old stroke patients: A comparison within over 65 population. Eur. J. Phys. Rehabil Med. 55, 148–155 (2019).
Bai, S., Liu, W. & Guan, Y. The visuospatial and sensorimotor functions of posterior parietal cortex in drawing tasks: A review. Front. Aging Neurosci. 13, 717002 (2021).
Biesbroek, J. M. et al. The anatomy of visuospatial construction revealed by lesion-symptom mapping. Neuropsychologia. 62, 68–76 (2014).
Duncan, J. & Owen, A. M. Common regions of the human frontal lobe recruited by diverse cognitive demands. Trends Neurosci. 23, 475–483 (2000).
Zhou, R. J. et al. Predicting gains with visuospatial training after stroke using an EEG measure of frontoparietal circuit function. Front. Neurol. 9, 597 (2018).
Huang, Q. et al. Immersive virtual reality-based rehabilitation for subacute stroke: a randomized controlled trial. J. Neurol. 271, 1256–1266 (2024).
Miyai, I. et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 25, 540–547 (2011).
Riga, A. et al. Evidence of motor skill learning in acute stroke patients without lesions to the thalamus and internal capsule. Stroke. 53, 2361–2368 (2022).
Taub, E. et al. A placebo-controlled trial of constraint-induced movement therapy for upper extremity after stroke. Stroke. 37, 1045–1049 (2006).
Kaneno, T. et al. Assessing the adjustability of grasping force using the iWakka in elderly individuals. J. Phys. Ther. Sci. 29, 2215–2219 (2017).
Yabuki, J., Akizuki, K., Yamamoto, R., Yamaguchi, K. & Ohashi, Y. Effectiveness of adjusted bandwidth knowledge of results in motor learning. Cogent Psychol. 9, 2131039 (2022).
Yamamoto, R., Akizuki, K., Yamaguchi, K., Yabuki, J. & Kaneno, T. A study on how concurrent visual feedback affects motor learning of adjustability of grasping force in younger and older adults. Sci. Rep. 12, 10755 (2022).
Wasaka, T. et al. Visuomotor tracking task for enhancing activity in motor areas of stroke patients. Brain Sci. 12, 1063 (2022).
Osterrieth, P. A. Le test de Copie D’une figure complexe; contribution à L’étude de La perception et de La mémoire. [Test of copying a complex figure; contribution to the study of perception and memory]. Arch. Psychol. 30, 206–356 (1944).
Chiulli, S. J., Haaland, K. Y., Larue, A. & Garry, P. J. Impact of age on drawing the Rey-Osterrieth figure. Clin. Neuropsychol. 9, 219–224 (1995).
Yamashita, H. Effects of the immediate recall trial on delayed recall performance in the Rey complex figure test in young and older adults. Appl. Neuropsychol. Adult. 22, 197–203 (2015).
Gosling, S. D., Rentfrow, P. J. & Swann, W. B. A very brief measure of the Big-Five personality domains. J. Res. Pers. 37, 504–528 (2003).
Santisteban, L. et al. Upper limb outcome measures used in stroke rehabilitation studies: A systematic literature review. PLOS ONE. 11, e0154792 (2016).
Loring, D. W., Martin, R. C., Meador, K. J. & Lee, G. P. Psychometric construction of the Rey-Osterrieth complex figure: methodological considerations and interrater reliability. Arch. Clin. Neuropsychol. 5, 1–14 (1990).
Chervinsky, A. B., Mitrushina, M. & Satz, P. Comparison of four methods of scoring the Rey-Osterrieth complex figure drawing test on four age groups of normal elderly. Brain Dysfunct. 5, 267–287 (1992).
Funding
This work was supported by JSPS KAKENHI Grant-in-Aid for Encouragement of Scientist Number JP22H04417 and Grant-in-Aid for Early-Career Scientists Number JP24K20476.
Author information
Authors and Affiliations
Contributions
Study Design: JY, TK, RY, KY, WN, and KA. Data collection: JY. Data analysis: JY. Data interpretation: JY, TK, RY, KY, WN, and KA. Manuscript writing: JY. Manuscript review: JY, TK, RY, KY, WN, and KA. All authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yabuki, J., Kaneno, T., Yamamoto, R. et al. Effects of visual terminal feedback on hand dexterity in relation to visuospatial ability in subacute stroke: a preliminary study. Sci Rep 15, 7368 (2025). https://doi.org/10.1038/s41598-025-91806-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-91806-2