Abstract
Visualize-HD study aimed to examine prevalence of hyperkalemia (HK), associated practice patterns, and mortality in Chinese patients undergoing hemodialysis (HD). The study included patients aged ≥ 18 years and undergoing chronic HD for ≥ 3 months. Primary outcome was to examine the association between suspected risk factors and HK prevalence at the HD facility level. Secondary outcomes were to determine the HK prevalence, management pattern of serum potassium (sK), and risk factors associated with crude mortality. Overall, 50,983 patients undergoing HD from 231 HD centers were enrolled. HK prevalence (sK > 5.0 mmol/L) in patients undergoing HD was 40.84%. Proportion of patients sK > 5.5, > 6.0, > 6.5 mmol/L was 20.42%, 8.7%, and 3.21%, respectively. Three-year cumulative mortality of patients undergoing HD was 21.3%. Notably, 36.7% of deceased patients had HK as indicated by their final sK+ test results. Facilities in high HK prevalence group had a higher all-cause and cardiovascular mortalities compared with low HK prevalence group (20.7% vs. 21.9% and 11.5% vs. 13.5%; P < 0.05). A higher prevalence of hyperphosphatemia [hazard ratio (HR) 1.04 (95% confidence interval (CI): 1.01–1.07)] and more usage of potassium-binding drugs [HR 1.04 (95% CI: 1.00-1.07)] were positively associated with higher HK prevalence for facilities, whereas hypoalbuminemia prevalence and more elderly patients were reversely associated with higher HK prevalence for facilities. HK is prevalent in Chinese HD centers and is associated with risk factors. Chinese HD centers with a higher HK prevalence had higher mortality rates. Although, long-term sK control is important for improving survival in patients undergoing MHD, potassium-binding drugs are underused.
Clinical trial registration number: NCT05020717
Similar content being viewed by others
Introduction
Hemodialysis (HD) therapy is a life-saving and life-sustaining procedure that restores fluid balance1,2. According to the China National Hemodialysis and Peritoneal Dialysis Registry, 86.7% of patients requiring renal replacement therapy (RRT) received HD3. Globally, it is estimated that 2.5 million patients are receiving RRT and is projected to reach 5.4 million by 20304. However, the adjusted all-cause mortality rate was 6.5 to7.9 times higher for patients undergoing dialysis than that for the general population5. Hyperkalemia (HK), defined as elevated serum potassium (sK, > 5.0 or > 5.5mEq/L) levels because of the diminished renal function of excreting 90% of daily ingested K+, is a common life-threatening complication in patients undergoing HD that results in huge variations in serum potassium (sK) levels6,7. The clinical manifestations of HK include cardiac arrhythmias, nausea, muscle pain, paralysis, weakness, palpitations, paresthesia, kidney disease, renal tubular acidosis, or peripheral neuropathy8. A retrospective study found that the incidence of long dialysis interval (LIDI) HK was more than twice that of short dialysis interval (SIDI) HK, which poses a huge burden on the healthcare system9.
Previous studies have suggested that in spite of China having an even higher clinical and economic burden of HK, studies are commonly reported from the Western countries10. The Chinese population with end-stage renal disease (ESRD) is ever increasing with patients undergoing HD constituting a sizeable proportion of the population11. Although some observational studies in China have established the connection between HK and adverse outcomes, the exact association between them is ambiguous and uncertain9. Characterizing these associations may guide healthcare providers and nephrologists in dialysis settings9. Furthermore, owing to the differences in sK management patterns for patients undergoing HD, there is a necessity to standardize the sK management methods among different HD centers to improve long-term outcomes of patients undergoing HD in China. As HK and sK levels are correlated, it is crucial to achieve control of sK levels in patients undergoing MHD by identifying the risk factors of HK. Hence, the present study was undertaken to investigate the rate of the prevalence of HK, the risk factors associated with HK clinical burden, and crude mortality in Chinese patients undergoing HD as well as the current patterns of HD centers.
Results
Patient disposition and baseline characteristics
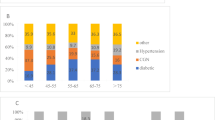
The study recruited 231 HD centers and 50,983 patients undergoing HD from 30 provinces, cities, and autonomous regions in China. The baseline demographic, clinical, and laboratory characteristics are summarized in Table 1. The distribution of included reach sites is presented in Fig. 1. The majority of the dialysis centers were affiliated tertiary hospitals (90.0%), and the median number of patient undergoing chronic dialysis was 118 per dialysis center. The median dialysis stations were 52, with 5 physicians and 25 nurses in each HD center. Most of the patients had treatment 3 times per week (82.8%). Male patients accounted for 58.9% of the total population. The age distribution of patients was given as follows: 18 to 44 years (18.7%), 45 to 64 years (46.5%), 65 to 74 years (23.0%), and ≥ 75 years (11.8%). The dialysis vintage distribution of < 1, 1 to 5, 5 to 10, and > 10 years was 14.0%, 48.2%, 27.1%, and 10.7%, respectively. The primary cause of ESRD was chronic glomerulonephritis (41.3%) followed by diabetic nephropathy (27.9%). Hypertension was the most common comorbidity reported in 70.7% of patients.
The proportion of patients with sK level > 5.5, > 6.0, > 6.5 mmol/L was 20.5%, 8.7%, and 3.2%, respectively. Facilities and patients were divided into low and high facility-level HK prevalence groups based on median prevalence of HK. The concentration of the most common dialysate potassium was 2.0 mmol/L (91.5%). Altogether, 56.2% of patients undergoing HD were accompanied by the usage of renin-angiotensin-aldosterone system inhibitors (RAASi). Further, 7.7% of patients received potassium-binding drugs.
Outcomes
Primary endpoint
Association between characteristics and high facility level of HK (> 5.0 mmol/L)
A negative association was observed with a higher prevalence of HK (> 5.0 mmol/L) and a higher percentage of patients undergoing dialysis more frequently (≥ 3 times/ week) [odds ratio (OR) 0.986 (95% confidence interval [CI]: 0.976–0.996)] with higher HK prevalence for facilities. A positive association was observed with a higher prevalence of HK (> 5.0 mmol/L) and a higher percentage of patients with albumin ≥ 40 (g/L) [OR 1.026 (95% CI: 1.009–1.044)] as well as with a higher percentage of patients with hemoglobin level ≥ 90 g/L [OR 1.032 (95% CI: 1.003–1.062), P < 0.05, Table 2].
Sensitivity study
Association between characteristics and high facility level of HK (> 5.5 mmol/L)
A positive association was observed between a higher prevalence of HK (> 5.5 mmol/L) and a higher proportion of male patients in an HD center [OR 1.042 (95% CI: 1.005–1.081), P < 0.05]. In addition, a higher prevalence of hyperphosphatemia (OR 1.04, 95% CI 1.01–1.07) was also associated with higher prevalence for facilities (P < 0.05, Table 3).
Secondary endpoints
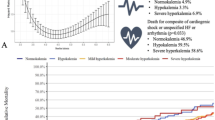
Association between facility level of HK and survival
A total of 10,861 patients died, of them 62.4% were males, and the average dialysis vintage of 51 months (Table 4). The 3-year cumulative mortality of patients undergoing HD was 21.3%. Compared with facilities in the low HK prevalence group, facilities in the high HK prevalence group had a higher all-cause and cardiovascular mortality (20.7% vs. 21.9% and 11.5% vs. 13.5%; P < 0.05, Table 5). The leading cause of death was cardiovascular disease (12.4% of total, and accounted for 58.2% of total death), followed by infection (12.9%). The average age of deceased patients was 66.5 years. The distribution of most recent sK ranges ([3.5, 5.0], [5.0, 5.5], [5.5, 6.0], [6.0, 6.5], [6.5, 7.0], and ~ 7.0 mmol/L) before death were 63.3%,16.6%, 10.0%, 5.4%, 2.3%, and 2.4%, respectively. After grouping the deaths of patients undergoing HD in each center during the last 3 years, we found that 36.7% of patients undergoing HD had HK as per the last sK test record before death, and HK or acute cardiovascular events accounted for 22% of deaths.
Methods
Study population and design
The Visualize-HD is a multicenter, observational, retrospective cohort study designed to understand the clinical burden of HK in China. The study procedure was executed in four different stages i.e., stage-1: site screening, stage-2: HD-centre enrolment, stage-3: data collection and stage-4: data analysis as described in our previously reported literature32. Briefly, this study planned to enroll 300 HD centers across China. HD centers willing to participate, having ≥ 100 patients undergoing MHD within 3 years before the study initiation, routine blood collection after LIDI, and death records were included in the study. Patients aged ≥ 18 years undergoing chronic HD for ≥ 3 months were deemed eligible for inclusion. The summary data on sK, characteristics of patients, and facility practice patterns were collected at the HD facility level, whereas death records were collected at the patient level. Since this was a retrospective study, the Peking University People’s Hospital review board waived the need for obtaining informed consent from the participants32.
The authors confirm that the study was conducted in accordance with the ethical standards of the relevant national and institutional committees on human experimentation and the Declaration of Helsinki. The study was approved by the ethics committee of Peking University People’s Hospital (ethical approval number: 2020PHB324-01). All participating sub-centers obtained approved from the ethics committee approval prior to initiation of the clinical trial. The trial is registered with ClinicalTrials.gov: NCT05020717.
Study groups
The prevalence of HK of each dialysis unit was determined by selected median cutoff of 39.2% and divided the dialysis centers into low and high groups.
Primary and secondary outcomes
The primary outcome was to examine the association between suspected risk factors and the prevalence of HK at HD facility level. Suspected risk factors included dialysis prescriptions, sK testing frequency, characteristics of patients, and related medication usage. Secondary outcome was to determine the prevalence of HK, sK management pattern, and risk factors associated with crude mortality. An assessment of risk factors associated with an sK levels of ≥ 6.0 and ≥ 6.5 mmol/L was the exploratory outcomes.
Statistical analyses
The full analysis set (FAS), defined as an analysis set closest to the intention-to-treat population, was used for all analyses. All eligible facilities were included, and an overall summary of data from each facility was generated. Continuous variables were summarized using descriptive statistics, whereas categorical variables were shown as frequencies and percentages. Multiple imputation method imputed the missing data.
Logistic regression model examined the association between suspected risk factors and the prevalence of HK at the facility level defined as the proportion of patients with sK level > 5.0mmol/L after LIDI. A probit regression was used to examine the relationship between suspected risk factors and the prevalence of HK at the facility level. The potential risk factors included key sK management factors (e.g., dialysis frequency, dialysate potassium concentration, and length of dialysis/session) and other factors (e.g., laboratory data, patients’ dialysis vintage, and other indices). For facility-level variables with m categories, there was m proportions at all categories for each facility. The categories of each risk factor were consolidated according to the clinical practice in the model to avoid over-parameterization. A variable selection procedure within multivariate analysis was processed using the backward algorithm within the regression model. A sensitivity analysis was conducted to change the sK cutoff to ≥ 5.5 mmol/L, using the same analysis method for the primary outcome. For secondary outcomes, the Poisson regression was used to explore the association of facility-level risk factors with crude mortality. The facility-level crude mortality was calculated as the ratio of the number of death records to the number of patients undergoing MHD during the past 3 years. Age and gender, the primary cause of ESRD and death, dialysis vintage on death, and the comorbidity condition were transformed into facility-level categorical variables. For exploratory outcomes, a similar method as mentioned above was used.
A 2-sided significance level of 0.05 (α = 0.05) was used for all analyses. All statistical analyses were performed using Microsoft Excel 2019 (Microsoft Corp., Redmond, WA, USA) and SAS 9.4 (SAS Institute Inc., Cary, NC, USA).
Discussion
HD facility is the primary healthcare provider for ESRD in China which prolongs life expectancy and improves a patient’s quality of life by intermittent potassium clearance12,13. To the best of our knowledge, the Visualize-HD study is the first and largest retrospective cohort study to investigate the prevalence of HK and the association between facility level of HK and clinical outcomes in patients undergoing HD using facility-level data. Our findings show that the prevalence of HK was high among patients undergoing dialysis. The 3-year cumulative all-cause and cardiovascular mortality rates among Chinese patients undergoing HD were 21.3% and 12.4%, respectively, with cardiovascular disease being the leading cause of death. It’s worth noting that 36.7% of deceased patients had HK based on their last sK+ tests. High facility levels of HK was found to be an independent risk factor for all-cause and cardiovascular mortalities. These results suggest that optimizing the management of sK levels and reducing HK could potentially improve the prognosis of patients undergoing HD.
Our study revealed that the overall dialysis pattern of Chinese patients undergoing HD tends to be standardized, regardless of the choice of dialysis frequency, dialysis duration, and dialysate concentration; nevertheless, the disease burden of HK is still heavy in Chinese patients undergoing HD. In addition, there exists a substantial difference between the modes of peritoneal dialysis and HD. Compared with the peritoneal dialysis which clears potassium ions all the time, HD is performed intermittently, thereby predisposing the patients to HK, severe HK, and heart rate abnormalities14. Patients undergoing dialysis have a rapid rebound in sK concentration within 1 h post dialysis, and the levels gradually increase until the next HD treatment15. In this regard, the French database showed that approximately 60% of patients undergoing HD had HK recurrence within 1 month16.
This study found that the overall incidence of HK in China is 40.9%, which is in line with the Precede-K study, that reported an incidence of 39.6%. Two different study types having similar incidence rates further confirm that the overall incidence of HK in China should be around 40% 17.
In terms of combination therapy, RAASi have a protective effect against dialysis risk in Chinese patients with hypertension undergoing HD in addition to their cardioprotective effects18. However, the overall use rate of oral potassium binders is still relatively low, which may be a breakthrough in further controlling the disease burden of HK in Chinese patients undergoing HD, especially in those with chronic kidney disease for whom diuretics are less effective, and dialysis is costly with inherent risks19.
With respect to risk factor analysis, hyperphosphatemia and hyperalbuminemia are the risk factors for HK, which are similar to those reported in the Dialysis Outcomes and Practice Patterns Study (DOPPS) China20. Both serum albumin and phosphorus are associated with an increased risk of HK, indicating that the dietary intake of patients with a good nutritional status should be optimized. When there is a risk of HK, a low-potassium diet should be combined to control the potassium intake in the diet. Besides, hyperphosphatemia also indicates the possibility of insufficient toxin clearance and insufficient dialysis adequacy. Hemoglobin and gender are important risk factors for HK. Although the difference in hemoglobin levels were similar for patients with normokalaemia and HK (108 g/L vs. 106 g/L) in this study, the rate of anemia remains high in other studies21,22. For the risk factor between different genders, the use of lower concentration of potassium in dialysate (< 2.5 mEq/L) in men was significantly higher than in women; however, the dialysis adequacy compliance rate was significantly lower in men when compared with women.
This study shows that dialysis should be conducted thrice a week for controlling blood potassium levels and avoiding potassium fluctuations, thereby preventing the occurrence of HK.
HK was associated with all-cause and cardiovascular mortalities on the facility level, which is in accordance with a previous study on the patient level, where HK posed an increased risk of cardiovascular and all-cause mortalities (including sudden cardiac death), hospitalization (including cardiovascular events), and emergency department visits9,23,24,25,26,27. When comparing patients undergoing HD with peak pre-dialysis, sK+ < 5.1 mEq/L in the global DOPPS28, the risk of all-cause mortality was 15% higher than that in those with sK+ level 5.1 to 5.5 mEq/L, 19% higher than that in those with sK+ level 5.6 to 6.0 mEq/L, and 33% higher than that in those with sK+ level > 6.0 mEq/L for 4 months. A similar trend was observed for the risks of all-cause hospitalization and the composite of cardiovascular death or hospitalization based on sK categories28. The risk of sudden cardiac arrest increased by 38% for each 1mEq/L increase in sK+ level > 5.1 mEq/L27. The DOPPS 5 study analyzed the blood potassium variability and prognosis of patients undergoing HD in 45 HD centers in China. The results showed that high facility-level potassium variability (> 0.8mmol/L) increased the risk of all-cause death in patients undergoing HD by 42%, and increased the risk of cardiovascular death in patients undergoing HD by 83%. A Japanese study also concluded that a significant increase in the blood potassium variability in patients undergoing HD increases the risk of all-cause death by 98%. Therefore, it is imperative to control sK on both dialysis and non-dialysis days. However, on dialysis days, HK can be controlled by HD treatments; oral potassium binders may be an accessible and effective alternative to reduce potassium management on non-dialysis days29.
An effective management of HK in patients undergoing HD during the interdialytic period, especially at LIDIs, is required. In China, studies on HK management in the HD setting are limited, and there is a dearth of updated clinical guidelines. The DIET-HD study concluded that relying solely on a low-potassium diet did not improve blood potassium levels and mortality risk in patients undergoing HD. No significant correlation was observed between increased dietary potassium intake and blood potassium levels or death in patients undergoing HD30. Similarly, the DIALIZE subgroup study also showed that regular dialysis and dietary control alone could not control the recurrence and fluctuation of HK in patients undergoing HD irrespective of the severity of HK at enrollment31.A recent consensus guideline provided recommendations on the use of potassium binders for the management of HK in the HD setting, along with dietary restrictions and the reduction of prescribed concomitant RAASi30,31,32.
Potassium binders, namely, sodium zirconium cyclosilicate (SZC), and patiromer, were recently approved for the treatment of chronic or recurrent HK34,35. Besides sodium polystyrene sulfonate (SPS) and calcium polystyrene sulfonate (CPS), SZC is currently the only available novel potassium binder for the management of HK in China36. Considering the fact that data are lacking on the efficacy and safety of SPS and CPS in the HD population, SZC may be a potential first treatment choice in Chinese population undergoing HD. For the management of HK in the HD setting, the DIALIZE study (NCT03303521) is the first randomized clinical trial to evaluate the efficacy of a novel potassium binder37. Among patients with three-times weekly HD and pre-dialysis HK treatment with SZC once daily on non-dialysis days resulted in a significantly higher proportion of patients who maintained sK level 4.0 to 5.0 mmol/L in at least three of four LIDIs, as compared with placebo, without the need for rescue therapy [41.2% vs. 1.0%; OR, 68.8 (95% CI: 10.9-2810.9); P < 0.001]37. A post hoc analysis showed that in a subgroup of patients with severe HK (sK+ ≥ 6.0mmol/L), SZC had an excellent blood potassium control rate compared with the control group [target sK+ranges of 4.0–5.0 mmol/L: 34.8% (SZC])vs 0% (placebo) and an extended range of 4.0-5.5 mmol/l: 67.4% (SZC) vs. 19.0% (placebo)]38. Furthermore, in comparison with placebo, treatment with SZC lowered the pre-dialysis and post-dialysis mean sK levels from baseline, which were maintained at a steady level throughout the treatment period of 8 weeks37. In contrast, sK fluctuations were observed in the control arm between the HD and LIDI cycles37. With lower sK+ levels, patients on treatment with SZC achieved a mean reduction of 0.74 mmol/L in their serum-dialysate potassium gradient and a shift toward lower-risk potassium gradient categories compared with those on placebo, without the need for any changes in the dialysate potassium concentration33. Furthermore, the DIALIZE subgroup analysis showed that SZC can effectively control potassium gradient in patients undergoing HD, and the long-term stability of blood potassium can help reduce the frequency of hospitalization and emergency visits33,39. These results will provide the specific treatment patterns for Chinese patients with ESRD in the HD setting.
A major strength of our study is that the Visualize Study is the largest HD cohort on HK with 231 HD centers and 50,983 patients. As this study extensively covers 30 provinces in China (except Tibet, Hong Kong, Macau, and Taiwan), it can better reflect the management model of country’s overall HD facilities and the disease burden of HK. This study generates the much-needed contemporary evidence to fill epidemiologic research gaps of HK and explore risk factors associated with HK disease burden in Chinese patients undergoing HD. An analysis of only facility-level data and not patientlevel data is the limiting factor of the study. This study has few limitations: (i) the present study only analyzed facility-level data but requires further analysis of patient level data for investigating on the detailed outcomes associated with HK in patients on HD. (ii) Further this study did not assess whether patients had followed any diet such as low-potassium diet.
In summary, the prevalence of HK in Chinese patients undergoing HD is high as more than one-third of the deceased patients who underwent HD had HK based on their last test results. Facilities with higher prevalence of HK tend to have higher all-cause and cardiovascular mortalities. Practice patterns and patient’s characteristics could affect HK prevalence. HK is an important component for the survival in patients undergoing HD, which needs to be valued and well managed, especially the non-dialysis days for the long-term management of potassium in patients undergoing HD with HK risk factors.
Data availability
The data underlying this article will be shared on reasonable request to the corresponding author.
References
Naseef, H. H. et al. Quality of Life of Palestinian patients on hemodialysis: cross-sectional observational study. Sci. World J. e4898202 (2023). (2023).
Steinwandel, U., Kheirkhah, H. & Davies, H. Residual renal function – How fast does the residual urine output function decline in the first year of Haemodialysis? – A scoping review. Front. Nephrol. 1, (2022).
Wang, H. et al. Cost-effectiveness analysis of Hemodialysis plus hemoperfusion versus Hemodialysis alone in adult patients with end-stage renal disease in China. Ann. Transl Med. 9, 1133 (2021).
Kitzler, T. M. & Chun, J. Understanding the current landscape of kidney disease in Canada to advance precision medicine guided personalized care. Can. J. Kidney Health Dis. 10, 20543581231154185 (2023).
Chandrashekar, A., Ramakrishnan, S. & Rangarajan, D. Survival analysis of patients on maintenance Hemodialysis. Indian J. Nephrol. 24, 206–213 (2014).
Palmer, F. B. Potassium binders for hyperkalemia in chronic kidney disease—diet, Renin-Angiotensin-Aldosterone system inhibitor therapy, and Hemodialysis. Mayo Clin. Proc. 95, 339–354 (2020).
Zacchia, M., Abategiovanni, M. L., Stratigis, S. & Capasso, G. Potassium: from physiology to clinical implications. Kidney Dis. (Basel). 2, 72–79 (2016).
Larivée, N. L., Michaud, J. B., More, K. M., Wilson, J. A. & Tennankore, K. K. Hyperkalemia: prevalence, predictors and emerging treatments. Cardiol. Ther. 12, 35–63 (2023).
Yusuf, A. A., Hu, Y., Singh, B., Menoyo, J. A. & Wetmore, J. B. Serum potassium levels and mortality in Hemodialysis patients: A retrospective cohort study. Am. J. Nephrol. 44, 179–186 (2016).
Zhang, J., He, X. & Wu, J. The impact of hyperkalemia on mortality and healthcare resource utilization among patients with chronic kidney disease: A matched cohort study in China. Front. Public. Health. 10, 855395 (2022).
Zhao, X. et al. Baseline data report of the China dialysis outcomes and practice patterns study (DOPPS). Sci. Rep. 11, 873 (2021).
Dhondup, T. & Qian, Q. Electrolyte and acid-base disorders in chronic kidney disease and end-stage kidney failure. Blood Purif. 43, 179–188 (2017).
Collier, S. & Davenport, A. Reducing the risk of infection in end-stage kidney failure patients treated by dialysis. Nephrol. Dial Transpl. 29, 2158–2161 (2014).
Huang, N. Y. et al. Current status of hyperkalemia in dialysis patients in China. Zhonghua Yi Xue Za Zhi. 101, 3466–3471 (2021).
Blumberg, A., Roser, H. W., Zehnder, C. & Müller-Brand, J. Plasma potassium in patients with terminal renal failure during and after haemodialysis; relationship with dialytic potassium removal and total body potassium. Nephrol. Dial Transpl. 12, 1629–1634 (1997).
Rossignol, P. et al. Hyperkalaemia prevalence, recurrence and management in chronic haemodialysis: a prospective multicentre French regional registry 2-year survey. Nephrol. Dial Transpl. 32, 2112–2118 (2017).
Ni, Z. et al. Hyperkalaemia prevalence and dialysis patterns in Chinese patients on haemodialysis: an interim analysis of a prospective cohort study (PRECEDE-K). BMC Nephrol. 24, 233 (2023).
Liu, B. et al. Utilization of antihypertensive drugs among chronic kidney disease patients: results from the Chinese cohort study of chronic kidney disease (C-STRIDE). J. Clin. Hypertens. (Greenwich). 22, 57–64 (2019).
Cañas, A. E. et al. A randomized study to compare oral potassium binders in the treatment of acute hyperkalemia. BMC Nephrol. 24, 89 (2023).
The prevalence and risk factors of hyperkalemia in. Chinese hemodialysis patients based on the China dialysis outcomes and practice patterns study. http://www.cjbp.org.cn/EN/abstract/abstract4351.shtml
Gheith, O. A. & Kamal, M. M. Risk factors of vascular access failure in patients on Hemodialysis. Iran. J. Kidney Dis. 2, 201–207 (2008).
Jeong, S. et al. Effects of patient age on patency of chronic Hemodialysis vascular access. BMC Nephrol. 20, 422 (2019).
Bem, D. et al. The effect of hyperkalemia and long inter-dialytic interval on morbidity and mortality in patients receiving hemodialysis: a systematic review. Ren. Fail. 43, 241–254 .
Karaboyas, A. et al. Dialysate potassium, serum potassium, mortality and arrhythmia events in hemodialysis: results from the Dialysis outcomes and practice patterns study. Am. J. Kidney Dis. 69, 266–277 (2017).
Brunelli, S. M., Mond, D., Oestreicher, C., Rakov, N., Spiegel, D. M. & V. & Serum potassium and short-term clinical outcomes among Hemodialysis patients: impact of the long interdialytic interval. Am. J. Kidney Dis. 70, 21–29 (2017).
Genovesi, S. et al. Sudden death and associated factors in a historical cohort of chronic haemodialysis patients. Nephrol. Dial Transpl. 24, 2529–2536 (2009).
Pun, P. H., Lehrich, R. W., Honeycutt, E. F., Herzog, C. A. & Middleton, J. P. Modifiable risk factors associated with sudden cardiac arrest within Hemodialysis clinics. Kidney Int. 79, 218–227 (2011).
Karaboyas, A. et al. Hyperkalemia excursions are associated with an increased risk of mortality and hospitalizations in Hemodialysis patients. Clin. Kidney J. 14, 1760–1769 (2020).
Yamaguchi, K. et al. Association between annual variability of potassium levels and prognosis in patients undergoing Hemodialysis. Clin. Exp. Nephrol. https://doi.org/10.1007/s10157-023-02368-4 (2023).
Bernier-Jean, A. et al. Dietary potassium intake and all-cause mortality in adults treated with Hemodialysis. Clin. J. Am. Soc. Nephrol. 16, 1851–1861 (2021).
Spinowitz, B. et al. Course of Hyperkalemia in patients on hemodialysis. International Journal of Nephrology e6304571 (2022). (2022).
Zhao, X. & Zuo, L. Multicentre, observational, retrospective cohort of hyperkalaemia burden at haemodialysis facility-level in China: the visualize-HD study protocol. BMJ Open. 13, e066394 (2023).
Fishbane, S. et al. Consensus-based recommendations for the management of hyperkalemia in the Hemodialysis setting. J. Ren. Nutr. 32, e1–e14 (2022).
Hoy, S. M. Sodium zirconium cyclosilicate: A review in hyperkalaemia. Drugs 78, 1605–1613 (2018).
Rossignol, P., David, L., Chan, C., Conrad, A. & Weir, M. R. Safety and tolerability of the potassium binder patiromer from a global pharmacovigilance database collected over 4 years compared with data from the clinical trial program. Drugs Real. World Outcomes. 8, 315–323 (2021).
Lokelma label update. approved in China for patients with hyperkalaemia on chronic haemodialysis. (2020). https://www.astrazeneca.com/media-centre/medical-releases/lokelma-label-update-approved-in-china-for-patients-with-hyperka.html
Fishbane, S. et al. A phase 3b, randomized, double-blind, Placebo-controlled study of sodium zirconium cyclosilicate for reducing the incidence of predialysis hyperkalemia. J. Am. Soc. Nephrol. 30, 1723–1733 (2019).
Ford, M. et al. Effectiveness of sodium zirconium cyclosilicate in Hemodialysis patients with severe hyperkalemia. Kidney Int. Rep. 6, 3074–3078 (2021).
Ni, Z. et al. DIALIZE China: A phase IIIb, randomized, Placebo-controlled study to reduce predialysis hyperkalemia with sodium zirconium cyclosilicate in Chinese patients. Clin. Ther. 45, 633–642 (2023).
Acknowledgements
The medical writing and editorial support for the preparation of this manuscript was provided by Kusuma Kumari. G, Ph.D, and Priyanka Bannikoppa, Ph.D, from of Indegene Ltd, India.
Funding
The Visualize-HD study was supported by AstraZeneca (Grant number: N/A). A grant from ZGC Nephrology & Blood Purification Innovation Alliance (Grant number: N/A) was obtained for this study. The funding source played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
X.Z., X.C., L.H., L.G., Z.P. and W.C. were involved in conception; methodology; data curation; formal analysis; visualization; resources; writing – original draft; writing – review and editing. X.Z., X.G., W.R., L.R., J.A., J.H., W.J., W.X. and Y.J. contributed to investigation; methodology; project administration; writing – original draft; writing – review and editing. Y.L., W.P., Z.R., L.Y., L.H., X.J. and C.M. were involved in conception; methodology and data curation. L.Y., C.Q., Y.Z., Z.Y. and L.H. contributed to project administration; software and supervision. H.W. and L.C. carried out funding acquisition. N.Z., G.L. and L.Z. were involved in writing – original draft; writing – review and editing. All authors have read and approved the final draft of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xinju, Z., Changying, X., Hong, L. et al. Prevalence, practice pattern, and mortality of hyperkalemia in Chinese patients undergoing hemodialysis in the visualize HD study. Sci Rep 15, 22405 (2025). https://doi.org/10.1038/s41598-025-92609-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92609-1