Abstract
The capacity to forecast nonreassuring fetal heart (NFH) is essential for minimizing perinatal complications; therefore, this research aims to establish if a machine learning (ML) model can predict NFH. This was a retrospective analysis of information gathered from singleton cases over the gestational age of 28 weeks that sought vaginal delivery between January 2020 and January 2022. The information was acquired from the “Iranian Maternal and Neonatal Network.“A predictive model was built using four statistical ML models (decision tree classification, random forest classification, extreme gradient boost classification, and permutation feature classification with k-nearest neighbors). Because of the limited studies on the identification of NFH predictors, we decided to use the Chi-Square test to compare demographic, obstetric, maternal, and neonatal factors to identify NFH predictors. Then, all variables with p-values less than 0.05 were considered potential NFH predictors. The area under the receiver operating characteristic curve (AUROC), accuracy, precision, recall, and F1 score were measured to evaluate their diagnostic performance. The incidence of NFH in our study population was 9.2%. Based on our findings NFH was more common in cases of intrauterine growth restriction, late-term, post-term, and preterm births, preeclampsia, placenta abruption, primiparous, induced labor, male fetus, and lower in birth with the presence of doula support. Random forest classification (AUROC: 0.77), decision tree classification and extreme gradient boost classification (AUROC: 0.76), and permutation feature classification with K-nearest neighbors (AUROC: 0.77), all showed good performance in predicting NFH. The higher performance belonged to random forest classification with an accuracy of 0.77 and precision of 0.72. Although this study found that the classification tree models performed well in predicting NFH, more research is needed to make a better conclusion on the performance of ML models in predicting NFH.
Similar content being viewed by others
Introduction
The primary goal of antenatal testing is to detect fetal hypoxia before the fetus suffers long-term harm. Intrapartum fetal heart rate (FHR) monitoring is fundamental for assessing fetal well-being during labor1. Failing to recognize or address a concerning FHR can result in various health risks and devastating injuries such as hypoxia/anoxia, partial or complete brain damage, cerebral palsy, paralysis, nerve damage, and stillbirth2. Nonreassuring fetal heart (NFH) is not an adverse event in and of itself but rather a symptom of an underlying condition that causes temporary or permanent oxygen deprivation in the fetus, which can lead to fetal hypoxia and metabolic acidosis3. Because fetal oxygenation is dependent on maternal oxygenation and placental perfusion, changes in maternal oxygenation, uterine blood supply, placental transfer, or fetal gas transport may result in fetal hypoxia and unsatisfactory fetal status4. Conditions commonly reported to be associated with NFH include maternal comorbidities such as cardiovascular disease, anemia, diabetes, hypertension, infection, placental abruption, abnormal presentation of the fetus, intrauterine growth restriction and umbilical cord compression, among other obstetric, maternal or fetal conditions5. The ability to predict NFH is critical for reducing perinatal complications. Since the use of machine learning (ML) algorithms in establishing risk predictors in medicine has grown in popularity over the previous decade6,7,8, thus, this study seeks to determine whether a machine learning-based model can predict NFH. The advanced research on artificial intelligence (AI) in clinical medicine demonstrated noteworthy outcomes, inspiring us to utilize AI models more enthusiastically9,10,11.
Methods
This was a retrospective study of data collected from singleton cases above the gestational age of 28 weeks that attempted vaginal delivery between January 2020 and January 2022. Exclusion criteria included elective scheduled cesarean and fetal anomalies. The findings of this retrospective cohort study are based on birth records obtained from the “Iranian Maternal and Neonatal Network (IMaN Net),” a legitimate national system. IMaN Net is a comprehensive system for registering maternal and newborn information on the outcomes of each delivery, which is completed daily by midwives in all birth centers and hospitals throughout Iran in an integrated manner12. All patients’ personal information was deidentified and not disclosed.
The target population in this study was divided into the NFH group and the reassuring fetal heart (RFH) group. We used The International Federation of Gynecology and Obstetrics (FIGO) consensus guidelines on intrapartum fetal monitoring cardiotocography tracing classifications13 to define fetal status (Table 1).
Because of the limited studies on the identification of NFH predictors, we decided to use the Chi-Square test to compare all available demographic, obstetric, maternal, and neonatal factors of eligibale women to identify NFH predictors. Then, all variables with p-values less than 0.05 were considered potential NFH predictors.
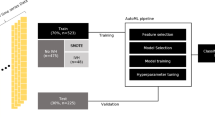
A predictive ML model was built using four statistical ML models, including decision tree classification, random forest classification, extreme gradient boost classification (XGBoost), and permutation feature classification with k-nearest neighbors (KNN). Classification trees were used because our dataset were split into classes that correspond to the response variable. In most circumstances, the answer was “Yes” or “No.” As a result, there were only two classes that were mutually exclusive. In cases of more than two classes in some circumstances, we just applied a modification of the classification tree technique.
We followed the Guidelines for Developing and Reporting Machine Learning Predictive Models in Biomedical Research: A Multidisciplinary View to report our findings. The programming language Python was chosen to create the machine learning model. Scikit-learn was used to implement the ML algorithm. Scikit-learn is a machine-learning library written in Python. It includes an extensive collection of cutting-edge machine-learning algorithms for both supervised (including the multi-output classification and regression algorithm) and unsupervised problems14.
Internal validation was carried out with the help of k-fold cross-validation. The cases were randomly assigned to either the “training set” (70%) or the “test set” (30%) using a random number generator. The original dataset kept the rate of NFH and RFH groups in the training and test sets constant. Using the training set, we arranged the parameters of the prediction models and evaluated their performance using the “test set.” The average performance was calculated by repeating these ten times.
Metrics, including area under the receiver operating characteristic curve (AUROC), accuracy, precision, recall, and F1 score were used to assess the predictive power of the models. The accuracy metric calculates how often a model is correctly predicted across the entire dataset. Precision measures how many of the model’s “positive” predictions were correct. Recall is a metric that evaluates the frequency at which a ML model accurately detects positive instances (true positives) among all the existing positive samples in the dataset. The F1 score, also known as the F-measure, is defined as the harmonic average of precision and recall in a classification model. Both metrics play an equal role in the score, guaranteeing that the F1 metric accurately reflects the reliability of a model. We used AUROC as the primary performance metric because it is a widely used index to describe the ML model’s ability to predict outcomes. The metrics were scaled from 0 to 1, with higher values indicating a better model15.
Patient characteristics were presented using frequencies (percentage). The chi-square test and Fisher’s exact test were used for categorical variables. All statistical analyses were done using SPSS (version 25.0, IBM Corp. Armonk, NY, United States) and Python software (Version 3.7.0). All statistical tests were two-tailed; p < 0.05 was considered statistically significant.
Results
661 (9.2%) of the 7166 eligible mothers experienced NFH. Table 2 shows the maternal demographic factors associated with antenatal fetal distress. NFH was found to be related to living residency. NFH was more common in mothers living in urban areas.
Table 3 shows the relationship between NFH and obstetrical factors. Primiparous mothers who had induced labour at less than 37 weeks or more than 40 weeks of gestational age or more had a higher rate of NFH. Mothers who had doula support during labor experienced less NFH.
Table 4 shows the relationship between maternal and neonatal clinical factors and NFH. Preeclampsia, placenta abruption. Intrauterine growth restriction, meconium amniotic fluid, and newborn sex were all associated with NFH.
In this study, we attempt to evaluate parameters and feature selection based on performance parameters using various ML algorithms. A plot ROC chart, as shown in Fig. 1, and calculate AUROC as a plot that allows the user to visualize the tradeoff between the classifier’s sensitivity. Decision tree classification (AUROC: 0.76), random forest classification (AUROC: 0.77), and XGBoost classification (AUROC: 0.76) had a higher performance than the permutation feature classification with KNN (AUROC: 0.71) as shown in Fig. 1.
Other performance parameters for each algorithm are shown in Table 5. Permutation feature classification with KNN had the lowest performance to predict NFH with an accuracy of 0.71 and precision of 0.66, while the higher performance belonged to random forest classification with an accuracy of 0.77 and precision of 0.72.
Figure 2 presents an analysis of the importance of variables in random forest classification. As the feature importance rank was identified, onset of labor, preeclampsia, placenta abruption, gestational age, parity, and intrauterine growth restriction were the top critical predictors of NFH.
Discussion
The incidence of NFH in our study population was 9.2%. Based on our findings NFH was more common in cases of intrauterine growth restriction, late-term, post-term, and preterm births, preeclampsia, placenta abruption, primiparous, induced labor, male fetus, and lower in birth with the presence of doula support .
Intrauteine growth restriction is one of the well-known cases of fetal distress. In fact, the same mechanisms that cause intrauterine growth restrictions by disrupting the placental blood supply can cause abnormal changes in the fetal heart rate during labor16.
There is not much information available regarding the relationship between gestational age and NFH. As we expected the rate of NFH in late-term and post-term pregnancies in our study population were higher. We also observed more rate of NFH in preterm births. However, based on our data, we cannot determine that the primary cause of fetal distress was the condition causing premature delivery or the administration of tocolytics to avoid premature delivery, which is one of our study’s limitations. As one study reported pregnant women who had tocolytic treatment more than one time during pregnancy were found to be at higher risk of NFH when compared to pregnant women without any tocolytic treatment17.
Based on our finding the NFH rate was more common in pregnant women diagnosed with preeclampsia. Poor utero-placental circulation in preeclamptic women retards fetal growth and causes NFH18.
The placenta provides the fetus with oxygen and nourishment while also excreting waste materials. Diffusion to and from the maternal circulatory system is crucial for the placenta’s life-sustaining capabilities19. When blood accumulates and separates the placenta from the maternal vascular network, these important placental activities are stopped, therefore in cases of placenta abruption the NFH is common.
Based on our analysis parity was among associated factors of NFH. As we observed NFH was more common in primiparous women. No explanation for this associtation has been reported yet. More resrech in this field might help to make a better conclusions.
Th onset of labor was another associated factors of NFH. Those with induced labor was more at risk of NFH. Synthetic oxytocin is the most often used method of inducing labor; nevertheless, the improper use of certain medicines, known as high-risk pharmaceuticals, can cause considerable damage to the patient. The link between oxytocin and hyperstimulation, NFH, and adverse neonatal consequences is known well20,21.
Based on our findings the rate of NFH was higher in male fetus than females. Some studies showed that male fetuses are at increased risk for fetal distress during labor, for low Apgar scores, and for perinatal death22,23. However we could not find any scientific reason to explane this issue.
Living residency were also associated with NFH. Those who lived in urban area with at higher risk of showing NFH compared to rural residents. We believe that sociodemographic factors should be more studied in different research to conclude the real association between them and health issues.
The new finding of our study was the presence of doula support during labor that was associated with lower risk of NFH. We expeculate that the presence of doula during labor prevent some conditions such as hyperstimualtion of uterous caused by uncontrolled use of oxytocin in cases of induced labor. There might be other explenations that need to be investigated.
This study was designed to assess the predictive ability of the maternal characteristics for NFH using ML models. Random forest classification (AUROC: 0.77), decision tree classification and extreme gradient boost classification (AUROC: 0.76), and permutation feature classification with K-nearest neighbors (AUROC: 0.77), all showed good performance in predicting NFH. Permutation feature classification with k-nearest neighbors had the lowest performance to predict NFH with an accuracy of 0.71 and precision of 0.66, while the higher performance belonged to random forest classification with an accuracy of 0.77 and precision of 0.72. With this account, it can be said that our study, like similar studies24,25,26,27, has succeeded in predicting cases of fetal distress using machine learning methods. Although a definitive conclusion to determine the effectiveness of this method requires more studies in the future.
The study of predicting NFH using the ML approach, which is the first to our knowledge, is a strength of the current research. The present study has attempted to simultaneously evaluate some predictors of NFH by using an appropriate sample size and statistical methods. Even though we used a large dataset with a lot of maternal and neonatal information, a significant variable, such as the use of tocolitic in preterm births, differen techniques used for induced labor (whether it was mechanical or medications), the maternal body mass index, was missing in the majority of the birth records, so we couldn’t use this factor in our selection features, which is a significant limitation of the study.
Conclusion
Identifying the risk factors of NFH can help clinicians guide patient counselling and anticipate the need for operative delivery or additional neonatal support at birth. ML approach adequately predicted NFH and allowed us to identify prediction variations based on specific case characteristics. The model revealed specific risk groups linked to NFH. Using ML approaches to predict NFH yielded promising results. As a result, this study might add to the current literature. More research is needed to make a better conclusion on the performance of ML models in predicting NFH.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- AI:
-
Artificial intelligence
- NFH:
-
Nonreassuring fetal heart
- RFH:
-
Reassuring fetal heart
- ML:
-
Machine learning
- XGBoost:
-
Extreme gradient boost
- KNN:
-
K-nearest neighbors
References
World Health Organization recommendations. Intrapartum Care for a Positive Childbirth Experience (World Health Organization, 2018).
Gravett, C. et al. Non-reassuring fetal status: Case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine 34 (49), 6084–6092. https://doi.org/10.1016/j.vaccine.2016.03.043 (2016).
Lewis, D., Downe, S. & FIGO Intrapartum Fetal Monitoring Expert Consensus Panel. FIGO consensus guidelines on intrapartum fetal monitoring: Intermittent auscultation. Int. J. Gynaecol. Obstet. 131 (1), 9–12. https://doi.org/10.1016/j.ijgo.2015.06.019 (2015).
Martin, C. B. Jr Normal fetal physiology and behavior, and adaptive responses with hypoxemia. Semin Perinatol. 32 (4), 239–242. https://doi.org/10.1053/j.semperi.2008.04.003 (2008).
Zuspan, F. P., Quilligan, E. J., Iams, J. D. & van Geijn, H. P. Predictors of intrapartum fetal distress: The role of electronic fetal monitoring. Report of the National Institute of child health and human development consensus development task force. Am. J. Obstet. Gynecol. 135 (3), 287–291. https://doi.org/10.1016/0002-9378(79)90691-4 (1979).
Banaei, M. et al. Utilizing machine learning to predict the risk factors of episiotomy in parturient women. AJOG Glob Rep. 5 (1), 100420. https://doi.org/10.1016/j.xagr.2024.100420 (2024).
Darsareh, F. et al. Application of machine learning to identify risk factors of birth asphyxia. BMC Pregnancy Childbirth. 23 (1), 156. https://doi.org/10.1186/s12884-023-05486-9 (2023).
Taeidi, E., Ranjbar, A., Montazeri, F., Mehrnoush, V. & Darsareh, F. Machine learning-based approach to predict intrauterine growth restriction. Cureus 15 (7), e41448. https://doi.org/10.7759/cureus.41448 (2023).
Tan, Y., Peng, Y., Guo, L., Liu, D. & Luo, Y. Cost-effectiveness analysis of AI-based image quality control for perinatal ultrasound screening. BMC Med. Educ. 24 (1), 1437. https://doi.org/10.1186/s12909-024-06477-w (2024).
Peng, Y. et al. Automatic measurement of fetal anterior neck lower jaw angle in nuchal translucency scans. Sci. Rep. 14 (1), 5351. https://doi.org/10.1038/s41598-024-55974-x (2024).
Mehrnoush, V., Darsareh, F., Shabana, W. & Shahrour, W. Prediction of renal Cancer recurrence using artificial intelligence: A systematic review. Canc Therapy Oncol. Int. J. 28 (2), 556233. https://doi.org/10.19080/CTOIJ.2025.28.556233 (2025).
Shekari, M. et al. The incidence and risk factors of meconium amniotic fluid in Singleton pregnancies: An experience of a tertiary hospital in Iran. BMC Pregnancy Childbirth. 22 (1), 930. https://doi.org/10.1186/s12884-022-05285-8 (2022).
Ayres-de-Campos, D., Arulkumaran, S., FIGO Intrapartum Fetal Monitoring Expert Consensus Panel(1). Corrigendum to "FIGO consensus guidelines on intrapartum fetal monitoring: Introduction" [Int J Gynecol Obstet 131(2015) 3-4]. Int. J. Gynaecol. bstet. 133 (2):254. https://doi.org/10.1016/j.ijgo.2016.03.001 (2016).
Pedregosa, F. et al. Scikit-learn: Machine learning in Python. J. Mach. Learn. Res. 12, 2825–2830. https://doi.org/10.1145/2786984.2786995 (2011).
Yen, S. J. & Lee, Y. S. Under-sampling approaches for improving prediction of the minority class in an imbalanced dataset. in Proceedings of the. International Conference on Intelligent Computing; ICIC ‘06; August 16–19, Kunming, China. 2006. 731–40. (2016).
Arabin, B., Becker, R., Mohnhaupt, A., Entezami, M. & Weitzel, H. K. Prediction of fetal distress and poor outcome in intrauterine growth restriction—A comparison of fetal heart rate monitoring combined with stress tests and doppler ultrasound. Fetal Diagn. Ther. 8 (4), 234–240. https://doi.org/10.1159/000263833 (1993).
Wang, I. T., Tsai, M. T., Erickson, S. R. & Wu, C. H. Tocolysis and the risk of nonreassuring fetal status among pregnant women in labor: Findings from a population-based retrospective cohort study. Med. (Baltim). 98 (50), e18190. https://doi.org/10.1097/MD.0000000000018190 (2019).
Yang, J. M. & Wang, K. G. Relationship between acute fetal distress and maternal-placental-fetal circulations in severe preeclampsia. Acta Obstet. Gynecol. Scand. 74 (6), 419–424. https://doi.org/10.3109/00016349509024402 (1995).
Downes, K. L., Grantz, K. L., Shenassa, E. D. & Maternal Labor, delivery, and perinatal outcomes associated with placental abruption: A systematic review. Am. J. Perinatol. 34 (10), 935–957. https://doi.org/10.1055/s-0037-1599149 (2017).
Alan, S., Akça, E., Şenoğlu, A., Gozuyesil, E. & Surucu, S. G. The use of Oxytocin by healthcare professionals during labor. Yonago Acta Med. 63 (3), 214–222. https://doi.org/10.33160/yam.2020.08.012 (2020).
Wu, S. W., Dian, H., Zhang, W. Y. & Labor Onset Oxytocin use, and epidural anesthesia for vaginal birth after Cesarean section and associated effects on maternal and neonatal outcomes in a tertiary hospital in China: A retrospective study. Chin. Med. J. (Engl). 131 (8), 933–938. https://doi.org/10.4103/0366-6999.229897 (2018).
Bekedam, D. J., Engelsbel, S., Mol, B. W., Buitendijk, S. E. & van der Pal-de Bruin, K. M. Male predominance in fetal distress during labor. Am. J. Obstet. Gynecol. 187 (6), 1605–1607. https://doi.org/10.1067/mob.2002.127379 (2002).
Lau, T. K., Chung, K. H., Haines, C. J. & Chang, A. M. Fetal sex as a risk factor for fetal distress leading to abdominal delivery. Aust. N Z. J. Obstet. Gynaecol. 36 (2), 146–149. https://doi.org/10.1111/j.1479-828x.1996.tb03271.x (1996).
Yohai, D. et al. Does gender of the fetus have any relation with fetal heart monitoring during the first and second stage of labor? J. Matern. Fetal Neonatal. Med. 30 (2), 150–154. https://doi.org/10.3109/14767058.2016.1168802 (2017).
Boujarzadeh, B. et al. Machine learning approach to predict postpartum haemorrhage: A systematic review protocol. BMJ Open. 13 (1), e067661. https://doi.org/10.1136/bmjopen-2022-067661 (2023).
Ranjbar, A. et al. Machine learning-based approach for predicting low birth weight. BMC Pregnancy Childbirth. 23 (1), 803. https://doi.org/10.1186/s12884-023-06128-w (2023).
Ranjbar, A. et al. Machine learning models for predicting preeclampsia: A systematic review. BMC Pregnancy Childbirth. 24 (1), 6. https://doi.org/10.1186/s12884-023-06220-1 (2024).
Acknowledgements
All of the authors acknowledged Hormozgan University of Medical Sciences.
Funding
This study received financial support from Hormozgan University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
F.D. and N.R. wrote the proposal. F.M. and V.M. contributed significantly to data collection. The findings were analyzed and interpreted by M.V. F.D., the primary contributor to the manuscript’s commenting and editing. N.R. assessed the manuscript’s scientific content critically. The final manuscript for submission was read and approved by all authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
This research adhered to the Declaration of Helsinki and was conducted following the approval of the ethics committee. The study was approved by the Ethics and Research Committee of Hormozgan University of Medical Sciences (IR.HUMS.REC.1403.127). The files of every patient who gave informed consent for the use of their data in research were examined. For individuals below eighteen years old, consent was obtained from their guardians. Statistical analysis was conducted while maintaining patient anonymity in accordance with ethics committee guidelines.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Roozbeh, N., Montazeri, F., Farashah, M.V. et al. Proposing a machine learning-based model for predicting nonreassuring fetal heart. Sci Rep 15, 7812 (2025). https://doi.org/10.1038/s41598-025-92810-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-92810-2
Keywords
This article is cited by
-
Developing a prognostic model for predicting preterm birth using a machine learning algorithm
BMC Pregnancy and Childbirth (2025)
-
Application of machine learning in identifying risk factors for low APGAR scores
BMC Pregnancy and Childbirth (2025)
-
Developing and validating a risk prediction model for caesarean delivery in Northwest Amhara comprehensive specialized hospitals
BMC Pregnancy and Childbirth (2025)