Abstract
Objective This study aimed to identify laboratory indicators with significant implications for bone marrow invasion in gastric cancer patients and to evaluate their prognostic value. Methods A retrospective analysis of the clinical data of 320 gastric cancer patients who underwent either bone marrow cytological examination or bone marrow biopsy at our hospital between January 2013 and December 2023 was conducted. Among these patients, 31 patients with confirmed bone marrow invasion composed the study group, whereas 34 stage IV gastric cancer patients without bone marrow invasion composed the control group. Differences in demographic and laboratory data between the two groups were compared. Receiver operating characteristic curves were used to identify valuable indicators for predicting bone marrow invasion in patients with gastric cancer. Survival analysis was performed using the Kaplan‒Meier method and included the plotting of survival curves. Additionally, Cox proportional hazards regression analysis was performed to evaluate independent prognostic factors. Results Significantly different values (all P < 0.05) were observed for age, peripheral blood immature cells, Hb, PLT, SII, FIB, PT, FDP, D-Dimer, FDP/FIB, CEA, and CA72-4 between stage IV gastric cancer patients with and without bone marrow infiltration. The ROC analysis indicated that at a threshold value of 5.197 for FDP/FIB, the AUC was 0.958 (P < 0.01). Within the cohort of 65 stage IV gastric cancer patients, those with bone marrow invasion and high FDP/FIB ratios exhibited notably shorter median survival times than those without bone marrow invasion and with low FDP/FIB ratios (χ2 = 25.928, 20.128, P < 0.001). Multivariate analysis demonstrated that bone marrow invasion (HR = 4.148, P = 0.020) and the FDP/FIB ratio (HR = 1.026, P = 0.024) were independent risk factors influencing the prognosis and survival outcome of stage IV gastric cancer patients. Among the subset of 31 gastric cancer patients with bone marrow invasion, the median survival time for the high FDP/FIB group was 22 days, which was significantly shorter than the 60 days observed in the low FDP/FIB group (χ2 = 8.479, P = 0.004). Conclusion The FDP/FIB ratio can serve as an important indicator for the diagnosis and prognostic evaluation of bone marrow invasion in patients with gastric cancer.
Similar content being viewed by others
Introduction
The prevalence of gastric cancer, which is the most common malignant tumour of the digestive system globally and one of the main causes of cancer-related deaths, is significantly high1,2. Distant metastasis and local recurrence present substantial challenges in the treatment of patients with advanced gastric cancer, particularly those exhibiting bone marrow infiltration, which typically suggests rapid disease progression and a poor prognosis. Reports indicate that bone marrow infiltration occurs in various common nonhaematologic malignancies3,4,5,6,7, with gastric cancer being one of the primary tumours frequently associated with such involvement8. However, owing to the heterogeneous nature of tumour cells and the varying degrees of bone marrow involvement, the clinical manifestations of gastric cancer-related bone marrow infiltration are both complex and diverse, lacking specificity and contributing to a high misdiagnosis rate. Currently, there is a paucity of robust biomarkers for the early identification of bone marrow infiltration in clinical settings. While the median survival time for patients with advanced gastric cancer is typically less than one year9, the presence of bone marrow invasion significantly shortens the overall survival time10,11. Research suggests that active treatment of cancer patients with bone marrow invasion can prolong survival and enhance quality of life12,13,14,15. Thus, early identification of bone marrow invasion and prompt adjustment of treatment strategies hold paramount importance for the prognostication of gastric cancer patients.
Currently, primary indications for bone marrow evaluation in clinical settings include significant nontreatment-related blood cell depletion that is refractory to correction or evidence of multiple bone lesions on imaging. Patients with subtle clinical symptoms or inconspicuous imaging findings are at increased risk of being overlooked16,17. The timely identification of bone marrow infiltration poses a critical challenge for health care practitioners and laboratory professionals. Few documented cases and insufficient systematic investigations concerning bone marrow involvement in gastric cancer exist. This retrospective study delves into analysing the clinical and laboratory characteristics of gastric cancer patients with bone marrow invasion, conducting survival analysis, exploring laboratory biomarkers with predictive value for bone marrow infiltration, and determining their prognostic implications.
Results
Comparison of general data between gastric cancer patients with bone marrow invasion and those without invasion
Among the 31 patients with bone marrow invasion, 17 patients were aged ≤ 50 years (54.8%), whereas 14 patients were aged > 50 years (45.2%). Immature red cells were observed in 19 patients (61.3%), and immature granulocytes were observed in 16 patients (51.6%) via peripheral blood smears. These differences were statistically significant compared with those in the nonbone marrow invasion group (P < 0.05). However, there were no statistically significant differences in terms of gender, bone marrow hyperplasia, or bone marrow necrosis between these two groups (P > 0.05), as outlined in Table 1.
Bone marrow morphology and histopathological characteristics of patients with gastric cancer with bone marrow invasion
Figure 1A-C illustrates the characteristics of cancer cells in bone marrow smears from patients with gastric cancer with bone marrow invasion. Cancer cells typically exhibit a large and irregular morphology and tend to aggregate in clusters. The chromatin appears as coarse granules, the cytoplasm is rich and deep blue, and red granules are also observed. Vacuoles, multiple nuclei, and nuclear division may be present in some cells. Furthermore, in cases of bone marrow necrosis, certain nuclear cells may display signs of dissolution.
A total of eight gastric cancer patients with bone marrow invasion underwent bone marrow biopsy, as shown in Fig. 1D-F. Among them, cancer cells were diffusely dispersed in the trabecular bone interstitium in six patients, whereas they exhibited a focal distribution in two patients. In certain regions, cancer cells were organized in glandular formations, accompanied by a notable decrease in or absence of granulocytes, erythrocytes, and megakaryocytes. The reticulin staining results indicated varying degrees of bone marrow fibrosis in all eight patients, with five cases graded as 2–3 and three cases as grade 1. Immunohistochemical staining revealed strong positive results for metastatic cancer cells using CEA and broad-spectrum CK markers.
Comparison of laboratory test indicators between patients with and without bone marrow invasion in gastric cancer
Table 2 shows that the SII and Hb, PLT, and FIB levels were significantly lower in the gastric cancer bone marrow invasion group than in nonbone marrow invasion group, whereas the FDP, D-Dimer, CEA, and CA72-4 levels, PT, and FDP/FIB ratio were notably greater in the former group, all of which were significantly different (P < 0.05). There were no statistically significant differences in the WBC, NE, LY, ALB, or CA19-9 levels, NLR, PNI, APTT, TT, or FDP/D-Dimer between the two groups (P > 0.05).
Diagnostic efficiency of each indicator for bone marrow invasion in patients with gastric cancer
By utilizing the occurrence of bone marrow invasion as the decisive event, ROC analysis was conducted on key detection parameters within the 31 patients in the bone marrow invasion group and the 34 patients in the nonbone marrow invasion group. The findings are presented in Fig. 2; Table 3. Hb, PLT, PT, FIB, FDP, D-Dimer, the FDP/FIB ratio, and CA72-4 exhibited AUC values exceeding 0.7, indicating substantial diagnostic effectiveness in detecting bone marrow invasion in patients with gastric cancer. Notably, FDP, D-Dimer, and the FDP/FIB ratio demonstrated AUC values greater than 0.9, indicating elevated diagnostic efficacy in differentiating between invasive and noninvasive samples. In particular, the FDP/FIB ratio exhibited the most superior diagnostic efficacy, achieving an AUC of 0.958 at a threshold of 5.197. The sensitivity and specificity of this indicator were 90.30% and 97.10%, respectively (P < 0.01), with a positive predictive value (PPV) of 96.55% and a negative predictive value (NPV) of 91.67%. These findings further underscore the significant potential of the FDP/FIB ratio in diagnosing bone marrow invasion in patients with gastric cancer.
Influence of bone marrow invasion and the FDP/FIB ratio on the survival of patients with stage IV gastric cancer
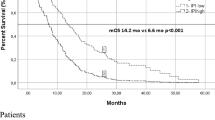
Among the 65 patients diagnosed with stage IV gastric cancer, 47 deaths were recorded, resulting in an overall survival rate of 27.69%. According to the X-tile program, the optimal cut-off value for fibrinogen degradation products (FDP) and fibrinogen (FIB) has been established at 18.913, thereby categorizing patients into low and high FDP/FIB groups. Kaplan–Meier analysis revealed that patients with bone marrow invasion and elevated FDP/FIB ratios had median survival times of 30 and 29 days, respectively, which were significantly lower than those without bone marrow invasion and those with lower FDP/FIB ratios, who survived for 212 and 155 days, respectively (χ2 = 25.928, 20.128, P < 0.001 for both), as illustrated in Fig. 3. Furthermore, patient age, Hb, PLT, PT, FIB, FDP, D-Dimer, CEA, and CA72-4 were correlated with patient survival time (χ2 = 6.730, 11.144, 7.347, 3.900, 8.736, 29.826, 27.601, 5.206, 4.662, P < 0.05 for all). A multivariate Cox proportional hazards regression analysis revealed that bone marrow invasion (HR = 4.148, P = 0.020) and elevated FDP/FIB ratios (HR = 1.026, P = 0.024) were independent risk factors that significantly influenced the prognosis and survival time of stage IV gastric cancer patients, as outlined in Table 4.
Influence of the FDP/FIB ratio on the survival outcomes of patients with bone marrow invasion in gastric cancer
Twenty-four of the 31 patients with gastric cancer and bone marrow invasion succumbed to the disease, yielding an overall survival rate of 22.58%. Using X-tile software, the optimum cut-off for FDP/FIB was found to be 30.688. The patients were subsequently divided into two groups based on their FDP/FIB ratio: a high group with 15 patients and a low group with 16 patients. The high FDP/FIB group presented a median survival time of 22 days, which was significantly shorter than the 60 days observed in the low FDP/FIB group (χ2 = 8.479, P = 0.004). This outcome underscores a significant correlation between FDP/FIB ratios and the survival time of individuals with bone marrow invasion in gastric cancer (Fig. 4).
Discussion
This study focused on patients with gastric cancer exhibiting bone marrow invasion, a distinct population that is uncommon among gastric cancer patients and has a significantly poor prognosis. The bone marrow serves as a significant site for tumour cells to metastasize to various target organs because of its loose tissue structure and unique sinusoidal vascular system, facilitating the concentration and retention of cancer cells. In some cases, tumours can metastasize to the bone marrow in early stages of development, occasionally resulting in the bone marrow being the sole site of occult metastasis18. The incidence of bone marrow invasion in patients with gastric cancer is relatively low19. A retrospective analysis conducted by Yakup et al.20on 896 gastric cancer patients revealed an incidence of 0.896% for bone marrow invasion. Our own study, which examined 3139 gastric cancer patients treated at our institution over an 11-year period, identified 31 instances of bone marrow invasion, leading to an incidence rate of 0.987%. Among the 320 cases subjected to bone marrow analysis, a detection rate of 9.69% was recorded, offering valuable clinical insights into the study of bone marrow invasion in patients with gastric cancer. Nonetheless, the invasive nature of bone marrow aspiration limits its widespread implementation among gastric cancer patients. Importantly, a negative result from a single bone marrow aspiration does not necessarily rule out bone marrow invasion, suggesting a likelihood of underestimation of the reported incidence rates. The presence of immature red blood cells and immature granulocytes in peripheral blood is an important clue in laboratory tests for bone marrow invasion21, possibly related to extramedullary haematopoiesis or tumour cell infiltration disrupting the blood‒bone marrow barrier. Data from our study demonstrated that 61.3% of gastric cancer patients with bone marrow invasion presented immature red blood cells, whereas 51.6% presented immature granulocytes in peripheral blood smears, which aligns with literature reports22.
Morphological examination of bone marrow cells and bone marrow biopsy are crucial for the clinical diagnosis of bone marrow invasion. In this study, gastric cancer cells were predominantly present in clusters, characterized by large irregular cell bodies, multinucleated giant cells, and structures resembling cell division. The phenomenon of tumour cell fusion is frequently observed due to hyaluronic acid depolymerization. The identification of these clustered cells in bone marrow smears, in conjunction with the patient’s medical history, facilitates a relatively straightforward diagnosis, while individual scattered tumour cells pose challenges in distinguishing certain malignant tumour cells within the haematopoietic system, necessitating cautious assessment. Among the 8 patients subjected to bone marrow biopsy, tumour cells exhibited diffuse distribution primarily, with some cases demonstrating focal or patchy patterns, alongside varying degrees of bone marrow fibrous tissue hyperplasia in all individuals. By avoiding sample dilution arising from bone marrow fibrosis, bone marrow biopsy preserves the structural integrity of the marrow tissue, and when combined with immunohistochemical staining, it enhances the identification of focal or scattered tumour cells, substantially improving the diagnostic accuracy23. Haematological changes often serve as the initial clinical indicators of bone marrow invasion, yet the current lack of specific markers results in insufficient vigilance among clinicians regarding bone marrow aspiration, leading to potential oversight or misdiagnosis of bone marrow invasion. Hence, there is an urgent need to investigate haematological indicators associated with bone marrow invasion.
Compared with patients in other cohorts, patients with bone marrow invasion presented significant reductions in haemoglobin and platelet levels and the SII, along with notable increases in the tumour markers CEA and CA72-4. These findings may be linked to multiple factors: (1) Infiltration of cancer cells can disrupt the bone marrow microenvironment, resulting in damage to stem cells and suppression of haematopoietic growth factor secretion by bone marrow stromal cells, resulting in haematopoietic dysfunction and decreased blood cell counts24,25. (2) Bone marrow mesenchymal stem cells and the chemokine CCL12 have the potential to promote the formation of tumour cells within the bone marrow microenvironment, contributing to tumour progression, proliferation, and metastasis26,27. (3) Stomach cancer cells directly induce the differentiation and activation of osteoclasts19,28, triggering the secretion of numerous growth factors that expedite the proliferation of stomach cancer cells, disrupt normal haematopoiesis, and result in elevated levels of tumour markers. Additionally, patients with bone marrow invasion displayed noticeable alterations in coagulation function.
Despite existing research investigating the roles of FDP and FIB in tumours29,30,31, studies assessing the FDP/FIB ratio as a diagnostic and prognostic marker in patients with gastric cancer involving bone marrow invasion remain largely exploratory. After bone marrow invasion, venous thrombosis and disseminated intravascular coagulation often occur32,33,34, with multiple underlying mechanisms: (1) Cancer cells infiltrating the bone marrow release various factors that readily enter the bloodstream, including coagulation and fibrinolytic enzymes that activate the coagulation and fibrinolytic systems, as well as cytokines that promote the activation of coagulation factors and induce the formation of neutrophil extracellular traps (NETs) to enhance coagulation35,36. (2) Bone marrow-infiltrating cancer cells engage in osteoclast activation, inducing tissue factor and Xa factor through the RANKL-dependent pathway to trigger the extrinsic coagulation pathway19. (3) An increase in the number of circulating tumour cells causes an increase in blood viscosity while also triggering the release of tissue factors, platelet activation, VWF production, and thrombosis induction37. The FDP/FIB ratio demonstrated the highest diagnostic efficacy in distinguishing between bone marrow invasion and nonbone marrow invasion, with a sensitivity, specificity, PPV, and NPV all exceeding 90%. This finding suggests that FDP/FIB ratios not only effectively identify patients with bone marrow invasion but also aid in excluding low-risk patients. FDP refers to fibrin degradation products, whereas FIB serves as the substrate in thrombin and fibrinolytic enzyme reactions. Elevated FDP/FIB ratios indicate a likely state of hyperfibrinolysis in patients; thus, a heightened FDP/FIB ratio strongly suggests the presence of bone marrow invasion.
Prognostic analysis demonstrated that in a cohort of 65 patients with stage IV gastric cancer, those with bone marrow invasion and elevated FDP/FIB ratios had median survival times of 30 and 29 days, respectively. These figures were notably lower than those of patients without bone marrow invasion and with lower FDP/FIB ratios, who had median survival times of 212 and 155 days, respectively, aligning closely with findings from prior studies8,11,38. Both single-factor and multifactor analyses identified bone marrow invasion and elevated FDP/FIB ratios as independent risk factors impacting the prognosis of stage IV gastric cancer patients. Notably, within the subgroup of 31 gastric cancer patients exhibiting bone marrow invasion, those with high FDP/FIB ratios experienced a median survival time of 22 days, which was significantly shorter than that of patients with lower FDP/FIB ratios (60 days). These findings highlight a strong association between elevated FDP/FIB ratios and survival outcomes in gastric cancer patients with bone marrow invasion.
In conclusion, our study systematically validated for the first time the diagnostic efficacy and prognostic value of the FDP/FIB ratio by comparing the clinical data and laboratory indicators of stage IV gastric cancer patients with and without bone marrow invasion. We confirmed that the FDP/FIB ratio can serve as an important indicator for the diagnosis and prognostic evaluation of bone marrow invasion in patients with gastric cancer. This finding not only introduces a new tool for clinical diagnosis but also opens new avenues for future research. Therefore, monitoring FDP/FIB ratios and promptly conducting bone marrow puncture examinations upon detecting abnormalities can lead to a clear diagnosis, allowing proactive treatment measures to improve patient prognosis. This study is retrospective and is subject to bias caused by the small sample size and single-centre design. Further research involving large samples and multiple centres is needed to validate the reliability and generalizability of the FDP/FIB ratio as a diagnostic and prognostic marker and to explore the interaction between bone marrow invasion and other relevant factors.
Materials and methods
Patients
This retrospective study analysed the data of 3139 patients who were diagnosed with gastric cancer at the Fourth Hospital of Hebei Medical University between January 2013 and December 2023. Among them, 320 patients underwent either bone marrow cytological examination or bone marrow biopsy, leading to the confirmation of bone marrow invasion in 31 patients. The incidence rate of bone marrow involvement was 0.987%, with an overall detection rate of 9.69%. The inclusion criteria were pathologically confirmed primary gastric cancer, evidence of bone marrow involvement via cytology or biopsy, and the availability of complete laboratory test results. The exclusion criteria were the presence of concomitant malignant tumours in other locations; a history of significant cardiac, cerebral, or renal impairments; and inadequate clinical or laboratory data. Additionally, 34 stage IV gastric cancer patients without bone marrow involvement served as the control group during the same period. All patients underwent a chemotherapy regimen based on platinum and fluorouracil. The diagnostic and staging standards for all patients were in accordance with the 8th edition of the International Union Against Cancer/American Joint Committee on Cancer (UICC/AJCC) TNM staging criteria for gastric cancer. All methods were performed in accordance with the relevant guidelines and regulations, and the study received approval from the Ethics Committee of the Fourth Hospital of Hebei Medical University (Approval No: 2021KS037). Informed consent was waived by the Medical Ethics Committee of the Fourth Hospital of Hebei Medical University since this was a retrospective study.
Bone marrow aspiration/biopsy
Bone marrow samples were obtained from either the anterior or posterior superior iliac spine. Thin bone marrow smears were subsequently stained with Wright‒Giemsa and examined under a microscope to assess cell morphology. Next, the bone marrow biopsy samples were fixed in neutral formalin, decalcified with formic acid, and embedded in paraffin to create 3 μm thick tissue sections. These sections were then stained with H&E for morphological analysis. The grading of reticular fibre staining in the bone marrow tissue sections was conducted using a four-grade scale. In addition, the bone marrow sections were deparaffinized and hydrated via the SP immunohistochemical technique. This involved blocking endogenous peroxidase activity with 3% H2O2 for 15 min, followed by a 20-minute blocking step with goat serum antibodies. The sections were subsequently incubated with a primary antibody against broad-spectrum CK (from Fuzhou Maixin Biotechnology Development Co., Ltd., China) at 37 °C for 1 h and then treated with biotinylated secondary antibodies and a streptavidin-HRP complex. The analysis of CK expression in the bone marrow tissue was based on the percentage of positively stained cells and the intensity of staining.
Laboratory tests
Patient data and routine laboratory test results were collected within a one-week period surrounding the time of bone marrow tissue collection. The parameters included gender, age, bone marrow proliferation status, presence of bone marrow necrosis, presence of nucleated red blood cells and immature granulocytes in peripheral blood, white blood cell count (WBC), neutrophil count (NE), lymphocyte count (LY), haemoglobin (Hb), platelet count (PLT), albumin (ALB), prothrombin time (PT), activated partial thromboplastin time (APTT), thrombin time (TT), fibrinogen (FIB), fibrinogen degradation products (FDP), D-Dimer (D-Dimer), carcinoembryonic antigen (CEA), carbohydrate antigen 19 − 9 (CA19-9), carbohydrate antigen 72 − 4 (CA72-4), neutrophil/lymphocyte ratio (NLR), systemic immune inflammation index (SII), prognostic nutritional index (PNI), FDP/FIB ratio, and FDP/D-Dimer ratio. The calculation formulas are as follows: NLR = neutrophil count/lymphocyte count; SII = neutrophil count × platelet count/lymphocyte count; PNI = albumin + 5 × lymphocyte count; FDP/FIB = fibrinogen degradation products/fibrinogen; FDP/D-Dimer = fibrinogen degradation products/D-Dimer.
Follow-up
Regular follow-up assessments were carried out via outpatient consultations, hospital monitoring, or phone interviews to ascertain the patients’ survival status. The follow-up period was concluded by January 2024 or upon patient death. In instances where there was no occurrence of an endpoint event or if the patient was lost to follow-up prematurely, the final recorded follow-up status and timestamp were treated as censored data. In this study, overall survival (OS) was defined as the duration between the confirmed date of bone marrow invasion and either the time of death or the most recent follow-up session.
Statistical analysis
We performed the statistical analysis using SPSS 25.0 and X-tile software, with the support of Prism 8.0 for graphical representation. Normality testing was conducted on all collected data. For normally distributed quantitative data, the mean values are reported as the means ± standard deviations (x ± s), and group comparisons were assessed using t tests. In the case of nonnormally distributed quantitative data, median values with interquartile ranges (M [P25, P75]) are presented, and group comparisons were carried out using the Mann‒Whitney U test. Categorical data are expressed as frequencies and percentages, and comparisons between groups were made using the chi-square test. Receiver operating characteristic (ROC) curves were used to assess the predictive value of various indicators for bone marrow invasion in patients with gastric cancer. The optimal cut-off values were determined using X-tile software, which also facilitated data grouping. Survival analysis was performed using the Kaplan‒Meier method, and the resulting curves were compared with the log-rank test. Additionally, independent prognostic factors were identified through Cox proportional hazards regression analysis. A significance level of P < 0.05 was considered statistically significant.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
SUNG, H. et al. Global Cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries [J]. CA Cancer J. Clin. 71(3), 209–249. https://doi.org/10.3322/caac.21660 (2021).
CAO, W. et al. Changing profiles of cancer burden worldwide and in China: a secondary analysis of the global cancer statistics 2020 [J]. Chin. Med. J. (Engl). 134(7), 783–791. https://doi.org/10.1097/CM9.0000000000001474 (2021).
CHANG W A et al. Differential expression profiles of the transcriptome in bone marrow-derived cells in lung cancer revealed by next generation sequencing and bioinformatics [J]. Oncol. Lett. 17(5), 4341–4350. https://doi.org/10.3892/ol.2019.10085 (2019).
TUSTUMI, F. et al. Prognostic value of bone marrow uptake using 18F-FDG PET/CT scans in solid neoplasms [J]. J. Imaging. 8(11). https://doi.org/10.3390/jimaging8110297 (2022).
YE, W. & HE, L. Case report: prompt response to Savolitinib in a case of advanced gastric Cancer with bone marrow invasion and MET abnormalities [J]. Front. Oncol. 12, 868654. https://doi.org/10.3389/fonc.2022.868654 (2022).
ASSI, R. & MUKHERJI, D. Metastatic colorectal cancer presenting with bone marrow metastasis: a case series and review of literature [J]. J. Gastrointest. Oncol. 7(2), 284–297. https://doi.org/10.3978/j.issn.2078-6891.2015.092 (2016).
WAKAMIYA, T. et al. Disseminated carcinomatosis of the bone marrow caused by prostate cancer diagnosed with only bone marrow biopsy [J]. IJU Case Rep. 4(5), 303–306. https://doi.org/10.1002/iju5.12332 (2021).
HUNG, Y. S. et al. Prognostic factors in adult patients with solid cancers and bone marrow metastases [J]. Asian Pac. J. Cancer Prev. 15(1), 61–67. https://doi.org/10.7314/apjcp.2014.15.1.61 (2014).
SMYTH E C, NILSSON, M. et al. Gastric cancer [J]. Lancet 396(10251), 635–648. https://doi.org/10.1016/S0140-6736(20)31288-5 (2020).
ZHOU, M. H. et al. Clinical outcome of 30 patients with bone marrow metastases [J]. J. Cancer Res. Ther. 14(Supplement), S512–S515. https://doi.org/10.4103/0973-1482.172717 (2018).
KWON J Y, YUN, J. et al. Clinical outcome of gastric cancer patients with bone marrow metastases [J]. Cancer Res. Treat. 43(4), 244–249. https://doi.org/10.4143/crt.2011.43.4.244 (2011).
PERES, T. et al. Metronomic cyclophosphamide for bone marrow carcinomatosis in metastatic castration-resistant prostate cancer [J]. J. Cancer Res. Clin. Oncol. 150(2), 84. https://doi.org/10.1007/s00432-023-05525-0 (2024).
OTSUKA, N. [A case of gastric Cancer with pulmonary carcinomatous lymphangitis and disseminated carcinomatosis of the bone marrow responding to S-1 plus cisplatin chemotherapy] [J]. Gan Kagaku Ryoho. 50(12), 1319–1321 (2023).
SENOO, S. et al. [HER2-Positive advanced gastric Cancer with disseminated intravascular coagulation and diffuse bone marrow carcinomatosis successfully treated with S-1/Trastuzumab Chemotherapy–A case report] [J]. Gan Kagaku Ryoho. 42(13), 2471–2475 (2015).
ETO, R. et al. [A case report of Cancer chemotherapy for disseminated carcinomatosis of the bone marrow associated with gastric Cancer accompanied by disseminated intravascular coagulation] [J]. Gan Kagaku Ryoho. 48(3), 367–369 (2021).
SHARMA, G. A. J. E. N. D. R. A. S. Cytomorphological evaluation of non-haematopoietic malignancies metastasizing to the bone marrow [J]. Am. J. Blood Res. 13(1), 1–11 (2023).
KIM H S et al. Clinical outcome of gastric cancer patients with bone marrow metastases [J]. Oncology 73(3–4), 192–197. https://doi.org/10.1159/000127386 (2007).
GIULIANO A E, HAWES, D. et al. Association of occult metastases in Sentinel lymph nodes and bone marrow with survival among women with early-stage invasive breast cancer [J]. JAMA 306(4), 385–393. https://doi.org/10.1001/jama.2011.1034 (2011).
IGUCHI H. Recent aspects for disseminated carcinomatosis of the bone marrow associated with gastric cancer: what has been done for the past, and what will be needed in future? [J]. World J. Gastroenterol. 21(43), 12249–12260. https://doi.org/10.3748/wjg.v21.i43.12249 (2015).
ERGUN Y. Gastric Cancer patients with bone marrow metastasis: A Single-Center experience and review of the literature [J]. Eurasian J. Med. Oncol. 1(3). https://doi.org/10.14744/ejmo.2017.65365 (2017).
MOHANTY S K, D. A. S. H. S. Bone marrow metastasis in solid tumors [J]. Indian J. Pathol. Microbiol. 46(4), 613–616 (2003).
YANG, H. et al. Clinical features and treatment of bone marrow metastasis [J]. Oncol. Lett. 26(2), 332. https://doi.org/10.3892/ol.2023.13918 (2023).
RANI, H. S. et al. Bone marrow metastasis of solid tumors: A study of 174 cases over 2 decades from a single institution in India [J]. Indian J. Hematol. Blood Transfus. 38(1), 8–14. https://doi.org/10.1007/s12288-021-01418-9 (2022).
GERBER-FERDER Y, COSGROVE, J. et al. Breast cancer remotely imposes a myeloid bias on Haematopoietic stem cells by reprogramming the bone marrow niche [J]. Nat. Cell. Biol. 25(12), 1736–1745. https://doi.org/10.1038/s41556-023-01291-w (2023).
RANA, N. A. et al. Laboratory evaluation and pathological features of bone marrow metastasis in Non-haematological malignancies [J]. J. Coll. Physicians Surg. Pak. 32(10), 1367–1369. https://doi.org/10.29271/jcpsp.2022.10.1367 (2022).
BERGFELD S A, DECLERCK Y, A. Bone marrow-derived mesenchymal stem cells and the tumor microenvironment [J]. Cancer Metastasis Rev. 29(2), 249–261. https://doi.org/10.1007/s10555-010-9222-7 (2010).
SHI, J. et al. CXCL12-CXCR4 contributes to the implication of bone marrow in cancer metastasis [J]. Future Oncol. 10(5), 749–759. https://doi.org/10.2217/fon.13.193 (2014).
LU, X. & WEI, M. U. E. VCAM-1 promotes osteolytic expansion of indolent bone micrometastasis of breast cancer by engaging alpha4beta1-positive osteoclast progenitors [J]. Cancer Cell. 20(6), 701–714. https://doi.org/10.1016/j.ccr.2011.11.002 (2011).
ZHANG, X. et al. Effectiveness of managing suspected metastasis using plasma D-Dimer testing in gastric cancer patients [J]. Am. J. Cancer Res. 12(3), 1169–1178 (2022).
SAKAI, M. & SOHDA, M. Fibrin/fibrinogen degradation products are associated with tumor stage and prognosis in patients undergoing resection of esophageal Cancer [J]. Anticancer Res. 41(9), 4523–4527. https://doi.org/10.21873/anticanres.15263 (2021).
WANG, X. et al. Clinical association between coagulation indicators and bone metastasis in patients with gastric cancer [J]. World J. Gastrointest. Oncol. 15(7), 1253–1261. https://doi.org/10.4251/wjgo.v15.i7.1253 (2023).
ZHAI, X. et al. Bone marrow metastasis from advanced gastric cancer complicated with disseminated intravascular coagulation: a highly aggressive but manageable disease subtype [J]. Cancer Commun. (Lond). 42(4), 350–354. https://doi.org/10.1002/cac2.12277 (2022).
SEKI, Y. & WAKAKI, K. Pathological findings in a case of bone marrow carcinosis due to gastric cancer complicated by disseminated intravascular coagulation and thrombotic microangiopathy [J]. Int. J. Hematol. 104(4), 506–511. https://doi.org/10.1007/s12185-016-2051-x (2016).
SUAREZ-REYES, G. et al. Thrombotic microangiopathy and disseminated intravascular coagulation in a patient with carcinomatosis of the bone marrow due to gastric adenocarcinoma: case report [J]. Rom J. Intern. Med. 61(3), 167–174. https://doi.org/10.2478/rjim-2023-0015 (2023).
MUNIR, H. et al. Stromal-driven and amyloid beta-dependent induction of neutrophil extracellular traps modulates tumor growth [J]. Nat. Commun. 12(1), 683. https://doi.org/10.1038/s41467-021-20982-2 (2021).
SUGIMOTO, T. et al. Repeated Social Defeat Exaggerates Fibrin-Rich Clot Formation by Enhancing Neutrophil Extracellular Trap Formation via Platelet-Neutrophil Interactions [J]. Cells, 10(12) doi:https://doi.org/10.3390/cells10123344. (2021).
DESIKAN S P, MCLAUGHLIN, N. et al. Recurrent Colon cancer: presentation with disseminated intravascular coagulation from disseminated carcinomatosis of the bone marrow [J]. J. Investig Med. High. Impact Case Rep. 9, 23247096211012224. https://doi.org/10.1177/23247096211012224 (2021).
KUCUKZEYBEK B B, CALLI A O, KUCUKZEYBEK, Y. et al. The prognostic significance of bone marrow metastases: evaluation of 58 cases [J]. Indian J. Pathol. Microbiol. 57(3), 396–399. https://doi.org/10.4103/0377-4929.138728 (2014).
Funding
This study was sponsored by grants from the Hebei Natural Science Foundation (H2024206074 and H2020206292) and the Medical Science Research Project of Hebei (20241554).
Author information
Authors and Affiliations
Contributions
X.J.G., J.Y.Z. and M.M. conceived and supervised the project. X.Y. and Y.H.N. contributed to the design of the study. X.X.Y., R.Y.Z., and W.X.C. contributed to the acquisition and analysis of the data. X.Y. and Y.H.N. wrote the main manuscript text. All authors reviewed and approved the submitted manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics Standard
The Medical Ethics Committee of the Fourth Hospital of Hebei Medical University approved this study. Informed consent was waived by the Medical Ethics Committee of the Fourth Hospital of Hebei Medical University since this was a retrospective study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yan, X., Niu, Y., Yang, X. et al. FDP/FIB ratio serves as a novel biomarker for diagnosing bone marrow invasion in gastric cancer and predicting patient prognosis\. Sci Rep 15, 9462 (2025). https://doi.org/10.1038/s41598-025-93056-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-93056-8