Abstract
Intestinal and soil-transmitted helminth (STH) infections are significant public health concerns in Somalia and are driven by poor sanitation, contaminated water, and inadequate hygiene practices. This study was undertaken to assess the prevalence and intensity of intestinal and soil-transmitted helminth infections among school-aged children in the Deyniile and Kahda internally displaced persons camps. A well-structured questionnaire was used to collect sociodemographic, behavioral and environmental data from the respondents, while fresh stool samples were collected to detect helminths via the cellophane-based Kato–Katz technique. Bivariate and multivariate logistic regression analyses were used to measure the strength of the associations. The overall prevalence of intestinal and soil-transmitted helminth infection was 72.5% (232/320). A mixed effects logistic regression analysis revealed that fathers with secondary school education (P = 0.039; AOR = 0.148; 95% CI 0.024–0.904) and children living in Kahda (P = 0.033; AOR = 0.519; 95% CI 0.283–0.950) had a significantly lower risk of helminths infection. The prevalence of helminths in both vamps was high. Dirty fingernails (P = 0.462; AOR = 0.72; 95% CI 0.30–1.73), eating unwashed fruits (P = 0.654; AOR = 0.86; 95% CI 0.45–1.66) and walking barefoot (P = 0.803; AOR = 1.13; 95% CI 0.43–2.96) were all not associated with increased risk of infection, including sanitary condition at home (P = 0.054; AOR = 2.99; 95% CI 0.98–9.17).
Similar content being viewed by others
Introduction
Intestinal helminthiasis and soil-transmitted helminthiasis are among the most common neglected tropical diseases (NTDs) in Africa, especially among impoverished populations1,2.
Soil-transmitted helminths (STHs) are a group of parasitic worms that pose a significant public health challenge, particularly in tropical and subtropical regions where sanitation and hygiene conditions are poor3. The main species of STH include Ascaris lumbricoides (roundworm), Trichuris trichiura (whipworm), and hookworms (Ancylostoma duodenale, Ancylostoma ceylanicum, and Necator americanus). These parasites are transmitted through contaminated soil, often because of improper disposal of human feces and inadequate sanitation practices4. The public health burden of STH infections is enormous, with millions of people affected globally, particularly in resource-limited settings.
Hymenolepis nana on the other hand is the cestode associated with human hymenolepiasis, and infection usually follows fecal‒oral transmission after the ingestion of food or water contaminated with infective eggs from the feces of humans and rodents5,6. Infection is most common among the pediatric population, especially those living in resource-poor countries and settings with poor sanitation and hygiene7. The disease is one of the most prevalent cestodes globally, infecting over 75 million people in 78 countries6.
Morbidities attributable to these parasites primarily result from chronic infections, which can lead to significant health issues such as malnutrition, anemia, impaired growth, and cognitive deficits in children3,4,7. In most cases, infection is asymptomatic; however, heavy infections may cause gastrointestinal signs characterized by abdominal cramps, diarrhea, nausea, and vomiting8. Recent World Health Organization (WHO) estimates indicate that STH affects more than 1.5 billion people, accounting for approximately 24% of the world’s population, with the majority living in low-income countries9. Hookworms, for example, attach to the intestinal wall and consume blood, leading to iron deficiency anemia10. The resulting chronic blood loss can result in fatigue, weakness, dizziness, and impaired cognitive function11,12. In severe cases, especially in children and pregnant women, anemia can lead to serious health consequences, such as developmental delays and complications during pregnancy12. Furthermore, STHs, especially Ascaris lumbricoides and Trichuris trichiura, compete for nutrients in the host’s intestines, thereby impairing the ability of the host body to absorb essential vitamins and minerals. This often leads to malnutrition, especially in children, resulting in stunted growth and poor physical development13,14,15. Although direct mortality from STH infections is relatively low, severe cases can result in life-threatening complications, such as bowel obstruction due to Ascaris infection or severe anemia from hookworms9,15. Indirect mortality may also occur through the exacerbation of other conditions, such as malnutrition or infection-related complications.
In Somalia, approximately 5 to 6 million people live in areas that are highly endemic for intestinal and soil-transmitted helminths16. The World Health Organization, in collaboration with the Somalia Ministry of Health and Human Services, undertook a mapping exercise between 2016 and 2017 to determine the prevalence of neglected tropical diseases, and the outcome of this exercise revealed unexpectedly high cases of intestinal schistosomiasis and hookworms16. A survey conducted by Ilardi et al. revealed that 85% of the population of two Somali communities harbor soil and intestinal helminth infections, with Trichuris trichiura accounting for 59% of the infections17. Although there is a dearth of national data regarding the status of this important neglected tropical disease, several small institution-based surveys have demonstrated a high disease prevalence. This includes a prevalence of intestinal parasitic infections of 35% and 30.6% for single and multiple infections, respectively, among children in pastoralist and agro-pastoralist communities in the Adadle woreda of the Somali Regional State of Ethiopia18. Similarly, a 6-year retrospective survey of intestinal parasites among patients attending tertiary hospitals in Somalia revealed that 7% of 37,398 patients tested for parasitic intestinal infections were positive for at least one species of intestinal parasite, with Giardia duodenalis, Entamoeba histolytica, Trichuris trichiura, Hymenolepis nana, and Ascaris lumbricoides being the most common19.
To overcome morbidities from intestinal and soil-transmitted helminths, the Federal Government of Somalia, with support from the World Health Organization (WHO), has conducted mass drug administration campaigns since 2017. Over an 18-day period of the mass campaign, essential medicines, such as praziquantel and metronidazole, were administered to approximately 3 million vulnerable school-aged children between the ages of 5 and 14 years, as well as to adults in 39 districts of the country. These interventions were part of the global effort to eradicate this important public health challenge in line with Sustainable Development Goals. Although these interventions were able to temporarily reduce the prevalence and intensity of soil and intestinal helminth infections, the disease has persisted, as demonstrated by a recently published 5-year retrospective survey, which revealed an overall prevalence of 11.9% (6,766/56,824), with Giardia lamblia having the highest prevalence 60.84% (4,116/6,766), followed by Entamoeba histolytica 33.07% (2,238/6,766) and Ascaris lumbricoides 3.18% (215/6,766)20. This finding suggests the need for sustained surveillance and stringent monitoring and evaluation of the situation in the country.
Therefore, this study was undertaken to estimate the prevalence of intestinal and soil-transmitted helminth infections, the intensity of the infections and the behavioral and environmental risk factors among children living in IDP settlements in Mogadishu, Somalia. This is because children in internally displaced persons (IDPs) are particularly vulnerable to helminth infections due to several compounding factors, including poor hygiene and sanitation, overcrowding, and limited access to basic healthcare services. The findings of this cross-sectional study will be useful for decision-makers and humanitarian actors in allocating resources and providing targeted interventions to reduce the direct and indirect impacts of these infections as well as improve the overall public health outcomes in Somalia.
Methods
Ethical approval and consent to participate
The study was approved by the ethical committee of the SIMAD University Institutional Review Board (Ref: 2023/SU-IRB/FMHS/P034). Ethical considerations were addressed by providing free drugs against intestinal protozoa to participants who were positive. Written informed consent was obtained from the parents or guardians of the selected study children. All methods in the study were performed in accordance with the relevant guidelines and regulations.
Study setting
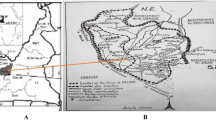
This study was conducted in the Deyniile and Kahda districts in Mogadishu Somalia. Deyniile and Kahda are two districts that house the largest population of IDPs in Somalia. Recent IDP site verification identified 1,979 IDP sites, with the majority (1115) located in Deyniile and 864 in Kahda. The two camps host 230,473 households with a total of 1,247,669 individuals21 (Fig. 1).
Verified IDP sites in Deyniile and Kahda based on CCCM Cluster, Somalia-Nov. 2023 Report21.
Study design and sample size
A cross-sectional study was undertaken by recruiting children aged 17 years and younger whose parents or guardians were residents of the Deyniile and Kahda IDP camps. The minimum sample size to achieve the aim of this study was computed via the single population proportion formula on the basis of a reported prevalence of 29.7% STH among children (P) and a 5% margin of error (e).
Therefore, the minimum sample size was found to be 320.
Sampling technique and method of data collection
One hundred and sixty (160) children from each of the IDP camps were selected via a systematic random sampling technique, where after the first house with children was conveniently chosen, every tenth household with at least one child was selected if the head of household consented. Children aged 17 years and younger during the data collection period were included in the study, while those with a history of recent deworming were excluded from the study.
The participants’ households were visited by trained data collectors to administer the questionnaire. A validated structured questionnaire developed after extensive literature review and review by expert researchers was uploaded to Google Forms and used to collect data through face‒to-face interviews with mothers/caretakers of the selected children. The data collected include data on environmental factors, such as domestic water sources and storage containers; waste disposal; the hygiene conditions of the households and their surroundings; and the type of toilet facility as well as animal ownership. Similarly, the questionnaire also addressed participants’ household demographic risk factors.
Laboratory stool examination
Following demonstrations to the children’s mothers or caregivers on how to aseptically collect stool without extraneous contaminants such as soil or urine, a sterile plastic screw-capped stool container labeled with the corresponding identification number of the questionnaire details was given to the parents for stool specimens. The collected stool sample was transported in an ice box immediately after collection to the Microbiology Laboratory, Faculty of Medicine and Health Sciences, SIMAD University Mogadishu, Somalia, for diagnosis. All diarrheic samples and samples contaminated with urine, water, or sand was discarded. In accordance with the recommended Kato–Katz technique by the WHO, a single thick stool smear was prepared according to the manufacturer’s instructions22. The prepared cellophane thick stool smear was kept at room temperature within 30 min under bright light to allow for sample clearing before examination under a bright-field microscope. The volume of stool filled into the template before smearing was 41.7 mg. The number of helminth eggs present in the prepared glass slide was counted and recorded, while the intensity of infection was computed by multiplying the number of eggs found in the fecal smear by a factor of 24 to obtain the number of eggs per gram of feces. This count was used for classifying the infection into either light, moderate or heavy infections (Table 3).
Data analysis
The questionnaire data were retrieved from the Google Form in the form of an Excel spreadsheet, coded and entered into SPSS v27 for analysis. All categorical variables were analyzed via descriptive statistics as frequencies and percentages. Univariable and multivariable logistic regression were used to assess the associations between infection and sociodemographic and behavioral risk factors, while a P value of less than 0.05, indicates statistical significance.
The data were statistically analyzed using bivariate and multivariate logistic regression to obtain the crude odds ratios and adjusted odds ratios. All variables from socio-demographic characteristics of participants and the behavioural and environmental risk factors in the bivariate analysis were fitted into the multivariate logistic regression model to identify independent predictors of intestinal and STH infection among the participants23.
COR was obtained by considering only the outcome (Intestinal and STH infection) and one exposure variable (independent variable) at a time, COR = (Odds of outcome in exposed group)/(Odds of outcome in unexposed group) and COR does not control for confounder. Whereas adjusted Odds ratios on the other hand was calculated using multivariate logistic regression analysis, which allows for the simultaneous control of multiple confounders by adding all the independent variables (exposures) into the equation.
Results
A total of 320 participants from 320 households, comprising of 161 children from Deynile and 159 children from Kahda IDP camps were involved in the study. The descriptive analysis of the results revealed that the majority of the participants 55% (177/320) were girls. The evaluation of age revealed that 61% (195/320) were under 5 years, 34% (109/320) were between the ages of 6–10 years, and 5% (16/320) were between 11 and 15 years. The detailed social and demographic characteristics of the participants and their households are shown in Table 1.
With respect to the environmental and behavioral risk factors, the results revealed that 16% (52/320) of the households kept animals, 46% (148/320) had poor sanitary conditions around their homes, and 92% (294/320) practiced open defecation. Similarly, 65.6% (110/320) of the children washed their hands after defecation, whereas 82.5% (264/320) washed their hands before and after eating. Most of the children 315/320 (98.4%) had no history of deworming, and 26.9% (86/320) had dirty fingernails (Table 2).
Prevalence and intensity of intestinal and soil-transmitted helminth infection
Among the 320 children enrolled in the study, 72.5% (232/320) were infected with one or more STHs or intestinal helminths. With respect to single infection, 74 (31.9%), 54 (23.3%), 1 (0.4%), and 21 (9.1%) of the children had T. trichiura, A. lumbricoides, hookworm, and H. nana infection alone. The prevalence rates of A. lumbricoides, T. trichiura, H. nana and hookworm infestations were 44.7%, 15.9%, 6.6%, and 1.9%, respectively (Table 3). The prevalence of each species of parasite and the intensity of infection among the infected children are presented in Table 3.
The intensity among the STH and intestinal helminth infections varies across the various parasites (Ascariasis, Hookworm and Trichuriasis intensity distributions). The median helminth intensity is as follows: 192 eggs per grams for Ascariasis, 24 eggs per grams for Hookworm, 192 eggs per grams for Hymenolepiasis, and 240 eggs per grams for Trichuriasis.
The results of the Kruskal‒Walli’s analysis, with a Chi-Square value 10.8, degree of freedom 3 and P value of 0.03, indicate statistically significant differences between the helminths infection Furthermore, statistically significant differences were detected between the ascariasis and the hookworm, with p values 0.00932, and between the hookworm and hymenolepis and the hookworm and trichuriasis (Fig. 2).
In the two IDP camps involved in this study, the intensity of infection was generally light for all the helminths surveyed, except for T. trichiura, which had 3.5% moderate infection, indicating an infection with 1000 to 9999 eggs per gram (EPG) of feces. The prevalence of helminth infection also varied per IDP camp, with the highest prevalence observed in Deyniile 78.3% (126/161), whereas that in Kahda was 66.7% (106/159) (Table 4).
Associations between sociodemographic factors and the risk of helminth infection
Bivariate and multivariate mixed effects logistic regression analyses of sociodemographic factors influencing helminth infection among children in Deyniile and Kahda IDP camps, Mogadishu, Somalia, revealed that fathers with secondary level education (P = 0.039; AOR = 0.148; 95% CI 0.024–0.904) and children living in Kahda (P = 0.033; AOR = 0.519; 95% CI 0.283–0.950) had significantly lower risk of helminth infections. Residents of a household with more than five members (AOR = 1.252; 95% CI 0.726–2.160), female gender (AOR = 0.84; 95% CI 0.49–1.410), and family income (AOR = 1.300; 95% CI 0.566–2.987) (Table 4) were all found not to be associated with increased or decreased risk of helminths infection.
Potential behavioral and environmental risk factors for intestinal and soil-transmitted helminth infection in children
The results of the logistic regression analysis are shown in Table 5. Children without dirty fingernails (P = 0.462; AOR = 0.72; 95% CI 0.30–1.73) and not eating unwashed fruits (P = 0.654; AOR = 0.86; 95% CI 0.45–1.66) and not wearing footwears (P = 0.803; AOR = 1.13; 95% CI 0.43–2.96) were found to not be significant risk factors for helminths infection. On the other hand, despite having poor sanitary conditions both within and outside their homes (P = 0.054; AOR = 2.99; 95% CI 0.98–9.17) showing potential association (p < 0.05), this was also found to not constitute a significant risk for helminths infection. Furthermore, all the remaining independent variables were found not be statistically significant contributors of intestinal and STH infection in this current study.
Discussion
In this study, the prevalence of intestinal and soil-transmitted helminth infection and helminth intensity as well as sociodemographic, environmental and behavioral risk factors among children living at the two major internally displaced people in Mogadishu, Somalia, were assessed. The prevalence of any intestinal or STH infection was found to be 72.53%, and only T. trichiura was found to have moderate infection among all children (3.5%).
Although recent data on the prevalence of helminth infection are scarce, our study revealed that intestinal- and soil-transmitted helminth infections persist among children in the Deyniile and Kahda IDP settlements in Mogadishu, Somalia. This result is lower than the 85% prevalence of intestinal helminths reported by Ilardi et al.17. This finding may suggest a slight improvement as a result of helminth prevention interventions as well as better water resources and sanitation infrastructure and practices in the area. However, this finding is considerably higher than the 11.9% reported in a 4-year retrospective survey among patients assessed at the laboratory of a tertiary hospital in Somalia20. This disparity is likely because only 5.3% of the participants studied in the 4-year retrospective study were children (0–15 years) in comparison with the present study. Many studies have shown that children have higher prevalence of helminths infection due to poor hygiene practices, immature immune systems, and frequent exposure to contaminated environment24,25,26,27.
The prevalence of any of the intestinal or STH infections in the Mogadishu Deyniile and Kahda IDP camps was light, with only T. trichiura showing a moderate intensity infection among 3.1% of the children. This may not be unconnected with the ongoing efforts aimed at reducing the prevalence of neglected tropical diseases in Somalia championed by the WHO in collaboration with the Somalia Ministry of Health. One such intervention is the mass drug (praziquantel and metronidazole) administration campaign to eradicate schistosomiasis and soil-transmitted helminth infections that was launched in 2017 through 2022, which targeted approximately 2.48 million school-aged children (aged between 5 and 14 years) and adults in 39 districts of Somalia28. These interventions will help reduce the reservoir of infection and interrupt disease spread. In addition to offering medicines to control and eradicate helminth infections, the stakeholders also embark on intense public awareness of these diseases, especially among the most vulnerable groups, including internally displaced persons28.
The prevalence of STH infection in this study was similar to the 75.6% reported among primary school children in Uttar Pradesh, India, whereas it was lower than the 89.6% reported in a survey of intestinal parasitism among school children in an internally displaced person camp in Benin city, Nigeria25,29. Important to highlight that the high prevalence in the Nigerian study could be because it included 8 different intestinal parasites while the current study investigated only four STHs and intestinal parasites. The disagreements in the prevalence of helminth infections in these studies could be attributed to the high helminth prevalence in Somalia due to poor sanitation, inadequate access to clean water, overcrowded living conditions in IDP camps, and limited health services. These factors are driven by the protracted conflicts, droughts and famine that have affected the country in recent years30,31. The ensuing humanitarian crisis facilitated the transmission of intestinal and soil-transmitted helminths, compounded by poverty, insufficient public health infrastructure, and a lack of awareness of hygiene and preventive measures17,28,32. On the other hand, the higher prevalence in Benin city was attributed to the presence of resistant cysts in the camp, which are able to withstand harsh environmental conditions in addition to poor personal and environmental hygiene, host genetic variability and geographical factors33,34.
In the present study, A. lumbricoides was the predominant STH species detected (44.7%), followed by T. trichiura (22.9%) and hookworms (1.9%), whereas the prevalence of the intestinal helminth H. nana was 6.6%. This finding is similar to studies in China, Ethiopia and India but differs from results in Benin city, Nigeria, and Northwestern Ethiopia where Entamoeba histolytica (64.3%), and Giardia duodenalis (57.0%), and hookworms were predominant respectively29,35,36,37. The findings in this study are also slightly dissimilar from recent reports in Somalia, where Giardia lamblia was found to have the highest prevalence (60.84%) in a five-year period, followed by Entamoeba histolytica (33.07%) and Ascaris lumbricoides (3.18%)2036,38. The fact that 58.1% of the children in our study reported wearing shoes while playing outside may have contributed to the reduced number of hookworm infections observed. Interestingly, some of the children in our study were found to harbor Hymenolepis nana infections, while no infection with Strongyloides stercoralis was detected, probably due to the limitations of the Kato–Katz technique38,39.
The high prevalence of helminth infection recorded in this study may be due to the lack of sustained mass drug administration (MDA) for helminths, especially among vulnerable displaced populations at the greatest risk. Approximately 30.1% of the children with one or more helminth infections were found to have dirty fingernails. Dirty fingernails can harbor soil, fecal matter, and helminth eggs, which act as a significant pathway for soil-transmitted helminth (STH) infections40,41. This finding is consistent with a study that assessed fingernail contamination with soil-transmitted helminths in schoolchildren in Ethiopia, where 24.3% of the children had A. lumbricoides, T. trichiura, and hookworm41. However, the intensity of the infections was generally light, with only 3.5% showing moderate-intensity infection. The fact that children often put their hands in their mouths or eat without washing their hands facilitates the ingestion of infective eggs or larvae, perpetuating the transmission cycle. This risk is heightened in settings such as IDP settlements with poor hygiene, inadequate sanitation, and limited access to clean water.
Our study also assessed the associations of potential risk factors with the prevalence of intestinal and STH infections. Some of the sociodemographic variables evaluated were parents’ education and occupation, family income, home of residence, and duration of stay in the camp. For all the sociodemographic variables studied, no associations were found except for fathers’ education and place of residence. This finding is similar to studies in Eastern Ethiopia and Indonesia38,42. However, in terms of place of residence, the number of infected children was greater in Deyniile (n = 126) than in Kahda (n = 106) IDP camps. Deyniile and Kahda are the largest IDP camps in Somalia, housing 273,181 families43. Unfortunately, the water, hygiene and sanitation conditions of IDP camps are poor, with low access to portable drinking water and rampant open defecation44. One possible explanation of the prevalence disparity is the fact that Deynile has higher number of verified IDPs (Deynile-1, 115 vs. Kahda-864), households (Deynile-123, 642 vs. Kahda-106, 831), and individuals (Deynile-653, 057 vs. Kahda-594, 612) according to recent estimations21. Overcrowding in IDP camps leads to competition for scarce resources, increases helminth infections due to poor sanitation, inadequate clean water, close contact, and increased environmental contamination among other things45,46. With respect to the significant association between fathers’ education and helminth infection, studies have shown that a father’s education level is one of several factors that can be associated with the prevalence of helminths in children, particularly as it affects the knowledge and awareness of helminth parasites47,48. This finding is consistent with the findings of Ayele et al. and Andargie et al. in Ethiopia, who reported that children whose fathers are illiterate are at greater risk of infection with helminths than are those whose fathers are literate24,48.
When we analyzed the associations between helminth infection and other environmental and behavioral risk factors, we found that most of the variables were not statistically significant after adjusting the odds ratio, except for the unsanitary condition of one’s home which showed potential association, but even this does not seem to significantly increase the risk of intestinal and soil-transmitted helminth infection. While, the p-value indicate possible association, the wide confidence interval implies variability and potential imprecision in the estimate possibly due to the relatively small sample size. Although studies in Malaysia and Honduras indicate that open defecation can increase the risk of helminth infection twofold, in this study, no association was found49,50. Additionally, from multivariate analysis, we did not find an association between the source of drinking water, storage of water, history of deworming or keeping livestock and the risk of intestinal and STH infection. This finding is consistent with studies conducted in Malaysia and Indonesia38,50.
Strengths and limitations
The cross-sectional study design used in this study is not able to generate evidence of a causal relationship and cannot account for seasonal variations in helminth transmission, which may lead to under- or overestimation of prevalence. Second, the sensitivity of the Kato‒Katz technique decreases with low-intensity infections, potentially underestimating its prevalence. It is also ineffective in detecting Strongyloides stercoralis and other helminths that are not shedding eggs. Hence, using more sensitive assays like molecular techniques (conventional and quantitative polymerase chain reaction) is recommended for better diagnosis and differentiation of helminths species including strongyloides. Finally, the relatively small sample size used to generate evidence on the infection status of children in this study due the high-security risk may have resulted in the lack of statistically significant association between the exposure and outcome variables analyzed.
Conclusion
The prevalence of intestinal and soil-transmitted helminth infections among children residing in internally displaced persons camps in Mogadishu Somalia remained high in both Deyniile and Kahda IDPs, although the intensity was light. This implies that despite the success of mass drug administration campaigns in reducing the prevalence of helminth infection, considerable sustained efforts are still needed on strengthening health systems, enhanced national and regional surveillance as well as addressing environmental and social determinants in order to achieve the morbidity elimination target. Therefore, continued mass drug administration, awareness creation and monitoring of the deworming process should be undertaken to accelerate the elimination of these important public health problems in the country.
Data availability
All data generated or analysed during this study are included in this published article.
Abbreviations
- IDP:
-
Internally displaced persons
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- IRB:
-
Institutional research ethics review board
- MDA:
-
Mass drug administration
- OR:
-
Odds ratio
- STH:
-
Soil-transmitted helminthiasis
- WHO:
-
World Health Organization
- NTD:
-
Neglected tropical diseases
- SPSS:
-
Statistical package for social sciences
- EPG:
-
Eggs per gram
References
Hotez, P. J. et al. Helminth infections: The great neglected tropical diseases. J. Clin. Invest. 118, 1311–1321 (2008).
Peter, J. & Hotez The neglected tropical diseases and the neglected infections of poverty: Overview of their common features, global disease burden and distribution, new control tools, and prospects for disease elimination. In The Causes and Impacts of Neglected Tropical and Zoonotic Diseases: Opportunities for Integrated Intervention Strategies. (ed. Institute of Medicine (US) Forum on Microbial Threats) (National Academies Press (US); Washington (DC), 2011).
Lebu, S. et al. Soil-transmitted helminths: A critical review of the impact of co-infections and implications for control and elimination. PLoS Negl. Trop. Dis. 17, e0011496 (2023).
Peter, J. et al. Helminth infections: Soil-transmitted helminth infections and schistosomiasis. in Disease Control Priorities in Developing Countries. (Oxford University Press, 2006).
Coello Peralta, R. D. et al. Hymenolepiasis caused by Hymenolepis Nana in humans and natural infection in rodents in a marginal urban sector of Guayaquil, Ecuador. Am. J. Case Rep. 24, (2023).
Al-Mekhlafi, H. M. The neglected cestode infection: Epidemiology of Hymenolepis Nana infection among children in rural Yemen. Helminthologia 57, 293–305 (2020).
Thompson, R. C. A. Neglected zoonotic helminths: Hymenolepis Nana, Echinococcus Canadensis and Ancylostoma ceylanicum. Clin. Microbiol. Infect. 21, 426–432 (2015).
Cabada, M. M. et al. Hymenolepis Nana impact among children in the highlands of Cusco, Peru: An emerging neglected parasite infection. Am. Soc. Trop. Med. Hygiene. 95, 1031–1036 (2016).
WHO. Soil-transmitted helminth infections. (2023). https://www.who.int/news-room/fact-sheets/detail/soil-transmitted-helminth-infections
Misikir, S. W., Wobie, M., Tariku, M. K. & Bante, S. A. Prevalence of hookworm infection and associated factors among pregnant women attending antenatal care at governmental health centers in DEMBECHA district, North West Ethiopia, 2017. BMC Pregnancy Childbirth. 20, 457 (2020).
Ness, T. E. et al. Maternal hookworm infection and its effects on maternal health: A systematic review and meta-analysis. Am. J. Trop. Med. Hyg. 103, 1958–1968 (2020).
Apili, F. et al. Hookworm infection among pregnant women at first antenatal visit in Lira, Uganda: A cross-sectional study. Int. J. Reprod. Med. 2020 1–8 (2020).
Adrizain, R. et al. Factors influencing stunted growth in children: A study in Bandung regency focusing on a deworming program. Parasite Epidemiol. Control. 26, e00361 (2024).
Martin, S. et al. Factors associated with early childhood stunted growth in a 2012–2015 birth cohort monitored in the rural Msambweni area of coastal Kenya: A cross-sectional study. BMC Pediatr. 20, 208 (2020).
Else, K. J. et al. Whipworm and roundworm infections. Nat. Rev. Dis. Primers. 6, 44 (2020).
WHO. Ending the neglect: eliminating worm infections as a public health problem in Somalia. (2022). https://www.emro.who.int/somalia/news/ending-the-neglect-eliminating-worm-infections-as-a-public-health-problem-in-somalia.html
Ilardi, I. et al. The prevalence and intensity of intestinal parasites in two Somalian communities. Trans. R Soc. Trop. Med. Hyg. 81, 336–338 (1987).
Lanker, K. C. et al. Prevalence and associated risk factors of intestinal parasitic infections among children in pastoralist and agro-pastoralist communities in the adadle woreda of the Somali regional state of Ethiopia. PLoS Negl. Trop. Dis. 17, e0011448 (2023).
Eker, H. H. et al. Prevalence of intestinal parasites among patients attending A tertiary referral hospital in Mogadishu, Somalia: A 6-year retrospective study. Hamidiye Med. J. 5, 1–6 (2024).
Doğan, S., Mohamud, S. M., Mohamud, R. Y. H., Orey, A., Orhan, Z. & A. M. & Distribution of the intestinal parasites according to species and gender in patients presented to the microbiology laboratory in a tertiary hospital, in Somalia between January 2018 and October 2022. Infect. Drug Resist. 16, 7007–7014 (2023).
CCCM Cluster & UNHCR & Somalia Verified IDP sites in Mogadishu Daynille and Mogadishu Khada - November (2023). https://reliefweb.int/report/somalia/somalia-verified-idp-sites-mogadishu-daynille-and-mogadishu-khada-november-2023 (2024).
Bosch, F. et al. Diagnosis of soil-transmitted helminths using the Kato-Katz technique: What is the influence of stirring, storage time and storage temperature on stool sample egg counts? PLoS Negl. Trop. Dis. 15, e0009032 (2021).
Bursac, Z., Gauss, C. H., Williams, D. K. & Hosmer, D. W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 3, 17 (2008).
Ayele, A., Tegegne, Y., Derso, A., Eshetu, T. & Zeleke, A. J. Prevalence and associated factors of intestinal helminths among kindergarten children in Gondar town, Northwest Ethiopia. Pediatr. Health Med. Ther. 12, 35–41 (2021).
Ganguly, S. et al. High prevalence of soil-transmitted helminth infections among primary school children, Uttar Pradesh, India, 2015. Infect. Dis. Poverty. 6, 139 (2017).
Júlio, C. et al. Prevalence and risk factors for Giardia duodenalis infection among children: A case study in Portugal. Parasit. Vectors. 5, 22 (2012).
Peltola, H., Kataja, M., Mohamed, O. N. & Kyrönseppö, H. Intestinal parasitism of children and mothers in rural Somalia. Pediatr. Infect. Dis. J. 7, 488–491 (1988).
WHO-EMRO. WHO Somalia: Health Emergency Programme Update, November 2022 - Somalia | ReliefWeb. (2022). https://reliefweb.int/report/somalia/who-somalia-health-emergency-programme-update-november-2022
Evbuomwan, I. O. et al. Survey of intestinal parasitism among schoolchildren in internally displaced persons camp, Benin City, Nigeria. Sci. Afr. 17, e01373 (2022).
Maxwell, D., Majid, N., Adan, G., Abdirahman, K. & Kim, J. J. Facing famine: Somali experiences in the famine of 2011. Food Policy. 65, 63 (2016).
Seal, A. & Bailey, R. The 2011 famine in Somalia: Lessons learnt from a failed response? Confl. Health. 7, 1–5 (2013).
Warsame, A., Frison, S. & Checchi, F. Drought, armed conflict and population mortality in Somalia, 2014–2018: A statistical analysis. PLOS Global Public. Health. 3, e0001136 (2023).
Halpenny, C. M. et al. Household and individual factors that influence soil transmitted helminth reinfection dynamics in preschool children from rural indigenous Panamá. PLoS Negl. Trop. Dis. 7, e2070 (2013).
Mohammed, K., Abdullah, M. R., Omar, J., Eugene, I. I., Ismail, A. & I. & Intestinal parasitic infection and assessment of risk factors in North-Western, Nigeria: A community based study. Int. J. Pharma Med. Biol. Sci. https://doi.org/10.18178/ijpmbs.4.2.141-145 (2015).
Gizaw, Z., Addisu, A. & Gebrehiwot, M. Socioeconomic predictors of intestinal parasitic infections among under-five children in rural Dembiya, Northwest Ethiopia: A community-based cross-sectional study. Environ. Health Insights 13, (2019).
Zerdo, Z. et al. Prevalence, intensity and endemicity of intestinal schistosomiasis and soil-transmitted helminthiasis and its associated factors among school-aged children in Southern Ethiopia. Sci. Rep. 12, 4586 (2022).
Wang, X. et al. Soil-transmitted helminth infections and correlated risk factors in preschool and school-aged children in rural Southwest China. PLoS One. 7, e45939 (2012).
Pasaribu, A. P., Alam, A., Sembiring, K., Pasaribu, S. & Setiabudi, D. Prevalence and risk factors of soil-transmitted helminthiasis among school children living in an agricultural area of North Sumatera, Indonesia. BMC Public. Health. 19, 1066 (2019).
Knopp, S. et al. Diagnosis of soil-transmitted helminths in the era of preventive chemotherapy: Effect of multiple stool sampling and use of different diagnostic techniques. PLoS Negl. Trop. Dis. 2, e331 (2008).
Mengist, A., Aschale, Y. & Reta, A. Bacterial and parasitic assessment from fingernails in Debre Markos, Northwest Ethiopia. Can. J. Infect. Dis. Med. Microbiol. 2018, 1–7 (2018).
Tadege, B. et al. Assessment of the nail contamination with soil-transmitted helminths in schoolchildren in Jimma town, Ethiopia. PLoS One. 17, e0268792 (2022).
Tefera, E., Mohammed, J. & Mitiku, H. Intestinal helminthic infections among elementary students of babile town, Eastern Ethiopia. Pan Afr. Med. J. 20, (2015).
CCCM Cluster. CCCM Cluster Somalia Dashboard as of October 2022. (2022).
Somali Community Concern (SCC). RAPID Needs ASSESSEMENT REPORT, Kahda, Mogadishu, Somalia. (2022).
Saed, A. H., Abdulle, M. O. & Isack, I. A. Evaluation of the availability of safe water and sanitation facilities in IDP camps Kahda district in Mogadishu Somalia. Afr. J. Health Med. Sci. 06, 17–21 (2021).
BRCiS, C. P. e4c. BRCiS & Caafimaad Plus: Nutrition and Mortality Monitoring in IDP Populations: Report on Round 5 - March 2023 (Report issued: 31/03/2023). The United Nations Office for the Coordination of Humanitarian Affairs OCHA (2023).
Forson, A. O., Arthur, I. & Ayeh-Kumi, P. F. The role of family size, employment and education of parents in the prevalence of intestinal parasitic infections in school children in Accra. PLoS One. 13, e0192303 (2018).
Andargie, Y., Alelign, A. & Tekeste, Z. Prevalence and associated risk factors of soil-transmitted helminth infections among schoolchildren in Mekan Eyesus town, Northwestern Ethiopia. Parasite Epidemiol. Control. 27, e00379 (2024).
Ziegelbauer, K. et al. Effect of sanitation on soil-transmitted helminth infection: Systematic review and meta-analysis. PLoS Med. 9, e1001162 (2012).
Ngui, R. et al. Patterns and risk factors of soil-transmitted helminthiasis among Orang Asli subgroups in Peninsular Malaysia. Am. Soc. Trop. Med. Hygiene. 93, 361–370 (2015).
Funding
None.
Author information
Authors and Affiliations
Contributions
B.G., N.I.D., A.O.S., A.A.H., and I.A.M.A performed the research including sample collection and laboratory analysis. Y.U., J.H.M., and M.H.A analyzed the data. B.G., H.A.A., J.H., and F.A.H.O designed the study. B.G wrote the first draft of the paper. M.A.M., and M.M.A revised the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Garba, B., Asowe, H.A., Dirie, N.I. et al. Prevalence and intensity of intestinal and soil-transmitted helminths infection among children in internally displaced camps in Mogadishu Somalia. Sci Rep 15, 12697 (2025). https://doi.org/10.1038/s41598-025-93364-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-93364-z