Abstract
Intravenous thrombolysis is the preferred treatment for acute ischemic stroke (AIS). In China, obtaining written informed consent from patients or their surrogates is mandatory before administering thrombolysis, often leading to delays in treatment. This study aims to explore the relationship between the decision-making characteristics and psychological states of surrogates during thrombolysis for AIS patients. A total of 383 AIS patients and their surrogate decision-makers were recruited from the Emergency Department of the First Affiliated Hospital of Zhengzhou University between September 2021 and December 2023. Comprehensive sociodemographic and disease-related data were collected for both patients and surrogates. Surrogate decision-makers were assessed using the State-Trait Anxiety Inventory (STAI), Control Preference Scale(CPS), Wake Forest Physician Trust Scale (WFPTS), and Perceived Social Support Scale (PSS). Data were analyzed using SPSS 26.0 software. The average score of state anxiety of surrogates was 49.47 ± 9.04, indicating a relatively high level of anxiety. Specifically, the average state anxiety score of the surrogate decision-makers has already reached a moderate level, indicating significant anxiety. Additionally, 18.2% (70/383) of surrogates took more than 15 minutes to decide. There was a significant positive correlation between state anxiety scores and decision duration (r = 0.189, p < 0.001). Factors influencing surrogate anxiety included sociodemographic factors, psychological factors, patient-related factors, and decision-making process characteristics (all p < 0.05). In conclusion, the anxiety is influenced by various factors related to the decision-making process. Medical staff should address these emotional factors to reduce decision time, enhance decision quality, and expedite informed consent, thereby minimizing treatment delays.
Similar content being viewed by others
Introduction
Acute ischemic stroke (AIS) is one of the leading causes of death and long-term disability worldwide1. According to the latest statistical data, the incidence rate of stroke in China is approximately 219 cases per 100,000 people annually, with an increasing trend year by year2. Globally, stroke is a major cause of long-term disability and mortality, including in Western countries and many other regions worldwide3. Stroke not only causes severe physical and cognitive impairments to patients but also imposes a heavy economic burden on families and society4. Patients often require long-term medical care and rehabilitation, placing significant economic and psychological pressure on their family members. Additionally, the substantial consumption of medical resources poses challenges to the public health system5. Intravenous thrombolysis is one of the preferred treatments for AIS, offering significant clinical benefits. It can dissolve blood clots and restore blood flow to the brain tissue within a short period, thereby reducing the damage to the ischemic area and lowering the rates of disability and mortality6. However, thrombolysis also carries certain risks, such as a relatively higher incidence of complications like intracranial hemorrhage. Despite these risks4, the benefits of thrombolysis outweigh its potential drawbacks, making it a crucial therapeutic option for improving the prognosis of patients with AIS.
Medical staff must discuss thrombolysis informed consent with patients and families in clinical practice. Physicians need to explain its necessity, including benefits and risks, to ensure understanding and voluntary acceptance5. In many Western countries, verbal consent suffices for thrombolysis, as it’s a standard treatment7. However, in China, written informed consent is still required due to differences in medical environment and legal system8, which required patients and families to understand the treatment before thrombolysis starts. The therapeutic window for AIS thrombolysis is typically 4.5 h, imposing significant decision-making pressure9. Patients and families need to quickly understand and decide whether to accept the treatment10. This time pressure often leads to anxiety, prolonging the decision-making process and potentially delaying thrombolysis.
State anxiety is a common emotional experience characterized by physiological arousal and subjective perceptions of tension, fear, and dread. State anxiety is closely related to the specific situation faced by the individual. In the context of AIS thrombolysis decision-making, patients and their families face a variety of stressors, including time constraints, complex information, and potential risks, which can easily trigger state anxiety11, interfering with their decision-making ability and leading to prolonged decision-making time12. Therefore, understanding the causes of state anxiety and its impact on decision-making is important for improving clinical communication and enhancing treatment outcomes13.
Method
Design and sample
This is an observational study from an advanced stroke center in China. The aim of this study was to investigate the relationship between state anxiety and decision-making duration of surrogate decision-makers in patients with acute ischemic stroke. A diverse group of patients was recruited from the emergency department between September 2021 and December 2023. Patients who met the diagnostic criteria of the 2018 Chinese Guidelines for the Diagnosis and Treatment of Acute Ischemic Stroke and the indications for alteplase thrombolytic therapy were included in the study14.Inclusion criteria: (1) patients met the sign for thrombolysis and signed written informed consent for thrombolysis by proxy. (2) be able to understand and express the Chinese language. Exclusion criteria: (1) patients or surrogate decision-makers unable to cooperate with the interview for various reasons. Or those who do not agree to participate in the interview.
Measurement
General information questionnaire
The general information questionnaire was designed by the researchers based on the objectives of this study. It recorded the patients’ gender, age, occupation, education level, economic status, type of medical insurance, medical history, pre-onset health status, type of complications, and stroke score. Additionally, the surrogate decision-makers’ gender, age, education level, occupation, economic status, relationship with patients, whether they lived with the patient, the number of people involved in the decision, and whether the patient is involved in the decision were also assessed. The above details were obtained through questionnaires, medical records, or from the decision-makers.
State anxiety
The state/trait inventory (STAI) was compiled by Charles Spielberger in 1977 and revised in 198315. This scale is a tool to assess the anxiety level of decision-makers in the decision-making process. In this study, we employed the state anxiety subscale of the questionnaire consisting of 20 assessment items to evaluate the emotional experience of fear, tension, anxiety, and neuroticism among surrogate decision-makers during the decision-making process. A four-level scoring method was applied to measure the degree of results on a scale of 1-4 (1 is not at all, and 4 is very obvious); the higher the score, the higher the level of anxiety. The levels of anxiety are categorized as follows: low anxiety tendency (20-39 points), moderate anxiety tendency (40-59 points), and high anxiety tendency (60-80 points).Cronbach’s α coefficient of this scale was 0.893 in this study.
The control preference scale
The Control Preference Scale(CPS) was is originally devised by Professor Degner16 in 1992 and subsequently refined by Xu17 to evaluate the level of willingness displayed by surrogate decision-makers in participating in thrombolytic therapy decisions. It is usually scored using a Likert scale, with each entry ranging from 1 to 5, representing a different level of agreement from “completely disagree” to “completely agree”. The Cronbach’s α coefficient was 0.86.
Wake forest physician trust scale (Chinese version)
The Wake Forest Physician Trust Scale was initially formulated by Hall et al. in 2002 and then refined by Dong and Bao18 in 2012 to assess patients’ trust in physicians during communication for informed consent. The scale consisted of two dimensions, each consisting of 10 items, It is scored on a scale of 1-5, with 5 indicating significant trust in the physician. In this study, the Cronbach’s α coefficient of the scale was 0.904.
Perceived social support
The Perceived social support scale was used to assess an individual’s self-understanding and perceived level of social support, including support from family, friends, and others19. The scale contains 12 items; the highest score is 7 points: 1 is strongly disagree, and 7 is strong agreement. The higher scores represent that the individuals perceived the higher level of support. The Cronbach’s α coefficient of this scale is 0.875.
Decision time
The decision time was defined as the time spent from the beginning of the informed consent conversation to the decision-maker signing the informed consent.
Sample size
To ensure robust statistical analysis and meaningful results, we calculated the required sample size using G*Power software. Based on a moderate effect size (Cohen’s r = 0.30) for the correlation between state anxiety scores and decision-making duration, with a significance level (α) of 0.05 and statistical power (1 - β) of 0.80, the minimum sample size was determined to be 383 participants. Considering potential dropouts and the practical constraints of recruiting participants from the emergency department of a large comprehensive hospital, we aimed to enroll at least 383 AIS patients and their surrogate decision-makers. Ultimately, we successfully recruited 383 pairs of AIS patients and their surrogate decision-makers from September 2021 to December 2023, which provided sufficient power to detect meaningful associations and analyze influencing factors comprehensively.
Data collection
Before data collection, the researchers trained the nurses responsible for thrombolysis, instructed them about using electronic and paper questionnaires, and informed them about the details to be noted. After the surrogate decision-makers signed the informed consent letter for thrombolysis, the nurse introduced the purpose and content of the study and obtained informed consent to fill in the electronic or paper questionnaire. Then, the on-site audit assessed for any missing items or obvious errors for re-verification. The investigators visited the patient’s bed or accessed the electronic medical record within 48 h of admission to collect patient data (such as financial burden and occupation) and disease-related data. Finally, the paper questionnaire data were entered by two individuals independently for accuracy.
Data analysis
Data were analyzed using SPSS 26.0 (IBM, Armonk, New York, USA), and normality tests were conducted for the measurement data. Data conforming to a normal distribution were represented as X ± SD, while non-normally distributed data were presented as M(Q1, Q3). The enumeration data were presented as case (%). Pearson’s correlation analysis or Spearman’s correlation analysis was used to assess the association of variables and state anxiety scores. Variance inflation factor (VIF) was used to assess the collinearity between variables. If VIF ≤ 10, the regression model was constructed using multiple linear regression analysis, and for VIF > 10, ridge regression analysis was used to establish a multi-factor regression model. p < 0.05 was considered statistically significant.
Informed consent statement
The study was conducted according to the guidelines of the Declaration of Helsinki. All the participants were previously informed of the detail of the research and signed the informed consent documents. No one outside the study group could view the subjects’ personal information.
Ethics approval and consent to participate
This study has the approval of the Ethics Review Committee of Life Sciences in the First Affiliated Hospital of Zhengzhou University (2020-KS-459), and informed consent was obtained before all questionnaires were collected.
Results
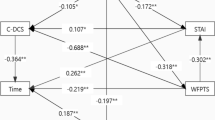
383 AIS patients and their surrogate decision-makers were recruited in this study. The mean age of the surrogate decision-maker was 60.7 ± 13.0, and no correlation was established with the state anxiety scale score of the surrogate decision-makers (r =-0.040, p = 0.460). In addition to the respondents, 1(0,2) participants were involved in the decision-making process, and no correlation was established with the STAI score of the surrogate decision-maker (r = 0.096, p = 0.077).Conversely, the state anxiety score of the surrogate decision-makers showed a negative correlation with “whether they are the main sources of income for the patient” (r =-0.222, p < 0.001),and “trust in the doctor” (r =-0.231, p < 0.001), while it showed a positive correlation with “whether they pay for this treatment” (r = 0.206, p = 0.041) (Table 1).
The mean age of the patients was 41.6 ± 10.1 years and was not associated with the surrogate decision-maker State Anxiety Scale score (r = 0.062, p = 0.250). The median of the patient’s NIHSS score was 4(3,5).The state anxiety score of the surrogate decision-maker avowed a negative correlation with “patient’s occupation” (r =-0.140, p = 0.009) and “patient’s income before onset” (r =-0.126, p = 0.020), while a positive correlation with “patient’s NIHSS score” (r = 0.184, p = 0.001), and “patient’s economic burden” (r = 1.131, p = 0.015) (Table 2) .
The surrogate decision-maker STAI scores were (49.47 ± 9.04) points. The decision time was (12.62 ± 3.24) min, and 18.2% (70/383) took longer than 15 minutes. Thus, a positive correlation was established between the rating of the State Anxiety scale and decision duration (r = 0.189, p < 0.001).
The original values of the independent variables were substituted for continuous variables for analysis, and the assignment of the categorical variables was shown in Table 3. The collinearity diagnostics revealed multicollinearity among the included independent variables in the study. Thus, ridge regression was used to improve the stability of the regression model in this study. The ridge trace analysis revealed that when the value of K was 0.57, the model presented a stable state. Therefore, K = 0.57 was selected as the corresponding ridge parameter of the regression model.
Ridge regression analysis identified several factors influencing the state anxiety levels of surrogate decision-makers, including trust in doctors, relationship with the patient, age of the surrogate decision-maker, their role, financial responsibility for the patient’s daily life, payment of treatment costs, perceived social support, patient’s age, type of medical insurance, number of relapses, NIHSS score, and patient participation in the decision-making process (all p < 0.05). These results are summarized in Table 4.
Discussion
Acute ischemic stroke (AIS) is a common acute cerebrovascular disease treated with thrombolytic therapy. The state of anxiety experienced by decision-makers can influence both the decision-making process and the duration required to make decisions regarding thrombolytic therapy, according to this study. State anxiety is a common emotional experience in people’s daily lives, accompanied by physiological arousal and subjective perception, including emotional experiences such as tension, fear, and dread. In this study, the state anxiety scale score of the agent decision-maker was 49.47 ± 9.04, which belonged to a high level of anxiety compared with other studies. This elevated anxiety level may be attributed to the strict time constraints that decision-makers face when collecting critical information within a short time. This situation complicates the decision-makers’ ability to balance the risks of intracerebral hemorrhage against the potential benefits of patient improvement, resulting in limited cognitive processing capacity. This reduced cognitive ability, in turn, diminishes the decision-makers’ capacity to acquire and process information efficiently. Consequently, their perception of decision-related information becomes insufficient, leading to uncertainty in decision-making. All the above phenomena increased anxiety outcomes20,21. Therefore, exploring the factors influencing state anxiety among surrogate decision-makers for AIS thrombolysis is essential to provide a reference for formulating decision-making assistance programs.
The current results indicate that the relationship between the decision-maker and the patient significantly influences the decision-maker’s anxiety levels. Specifically, when the decision-maker is the patient’s child, their anxiety level tends to be lower. This may be attributed to children’s younger age, higher education, and superior cognitive abilities, which facilitate a better understanding of disease and treatment information and, consequently, As a result, they are able to more quickly and comprehensively obtain relevant information, which helps them make decisions rationally rather than being overwhelmed by the anxiety associated with decision-making difficulties. Conversely, the anxiety level is higher when the decision-maker is the patient’s spouse. This elevated anxiety may stem from the closer emotional bond between spouses, leading to increased concern about the patient’s prognosis and the risk of complications, such as bleeding. Additionally, the age of the patient also impacts the decision-maker’s anxiety level. When the patient is older, the decision-maker’s anxiety tends to be lower. This may be because decision-makers have lower expectations for treatment outcomes and are mentally prepared for adverse medical outcomes, consistent with findings by Iverson et al.22 Furthermore, our study found no significant correlation between the decision-maker’s age or gender and their anxiety levels, but a clear correlation was observed between the decision-maker’s education level and anxiety levels23.Moreover, Our results also indicated that the patient’s medical insurance type affects the decision-maker’s state anxiety level. The patient’s provincial medical or commercial insurance reduces the decision-maker’s state anxiety20, as they cover a higher proportion of medical expenses, reducing the patient’s out-of-pocket proportion, which does not cause a significant economic burden. And decision-makers will not delay decision-making when considering whether to accept thrombolytic therapy due to economic factors. Moreover, patients with higher NIHSS scores and multiple recurrences were associated with higher anxiety levels among decision-makers. This may be related to the increased risk of hemorrhagic transformation in such cases24.
The results of this study showed that a high level of social support is associated with low anxiety levels25. This association may be explained by the fact that decision-makers who perceive stronger social support are likely to feel more confident and emotionally reassured. This emotional support can enhance their ability to process complex medical information and make decisions more efficiently, thereby reducing the anxiety associated with decision-making. Additionally, social support may provide practical assistance, such as helping to gather and interpret medical information, which further facilitates the decision-making process. The study also found that trust in doctors shows a negative correlation with the anxiety level of decision-makers. Therefore, healthcare professionals can employ appropriate communication techniques to stabilize decision-makers’ emotions while conducting informed consent conversations for thrombolysis. Additionally, leveraging the intelligent decision-making advantages of big data can provide convincing information to decision-makers26, making it easier to establish trust and reduce anxiety levels. The results of this study further revealed that the patients’ participation in decision-making reduces the anxiety level of decision-makers. This might be because when patients can effectively communicate their preferences to decision-makers, the psychological burden on decision-makers in balancing patient wishes was reduced, further reducing anxiety levels. This conclusion aligns with the findings of Wu and Li26.
Taken together, the results also indicated that the anxiety level of decision-makers is positively associated with decision-making duration. This might be because the state of high anxiety tends to make decision-makers avoid risks under time pressure26, and they cannot make decisions in a timely manner, resulting in longer decision duration. Another study has shown that anxiety reduced the decision-making ability of decision-makers27, weakened their ability to allocate cognitive resources, thus restricting cognitive processing28. Furthermore, decision-makers may worry that patients will experience severe complications after treatment, which was contrary to the doctor’s recommended treatment plan, further aggravating their anxiety. All the above factors could prolong the duration of decision-making. Therefore, it is crucial to shorten patient admission, examination, and testing time to improve the process29. Also, it is pivotal to understand and meet decision-makers’ needs in the decision-making process from a psychological perspective.
The theoretical and practice implication
This study offers significant theoretical and practical implications by elucidating the relationship between the state anxiety of surrogate decision-makers and the duration of decision-making regarding thrombolysis for AIS patients. Theoretically, it advances our understanding of how psychological factors influence medical decision-making, particularly in emergency settings, and provides empirical evidence to refine theoretical models related to decision-making under stress and uncertainty. It also highlights the role of various influencing factors, such as trust in physicians, social support, and sociodemographic characteristics, which can be further integrated into theoretical frameworks in nursing and medical research. Practically, the findings have important implications for clinical practice. By identifying the high level of state anxiety in surrogate decision-makers and its impact on decision-making time, healthcare providers can tailor their communication strategies to address these emotional factors. These approaches might help reduce the anxiety level of decision-makers, shorten the time required for informed consent, and ultimately minimize treatment delays, leading to improved patient outcomes in the management of acute ischemic stroke. Additionally, the findings suggest that healthcare institutions can consider implementing decision-making aids or support programs to assist surrogate decision-makers in coping with the stress and anxiety associated with making critical treatment decisions.
Conclusion
This study highlights the significant anxiety experienced by surrogate decision-makers of AIS patients during thrombolytic decision-making. It underscores the influence of various factors such as trust in physicians, social support, and sociodemographic characteristics on this anxiety level. Given the close relationship between state anxiety and decision-making time, effective communication strategies and decision-making aids should be employed during informed consent discussions. These approaches can enhance decision-makers’ trust in doctors, reduce anxiety, and expedite the decision-making process.
Limitations
This study comprehensively examined the relationship between state anxiety and decision-making duration in surrogate decision-makers for AIS patients, utilizing well-established scales and a sample size of 383 participants. However, it has limitations, including being conducted in a single hospital in Zhengzhou, Henan Province, which may limit generalizability, and relying primarily on self-evaluation questionnaires, which could introduce response bias. Future research should involve multi-center studies across different regions and hospital types, larger sample sizes, and mixed-methods approaches to enhance the robustness and generalizability of the findings.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Martin, S. S. et al. 2024 Heart Disease and Stroke Statistics:A Report of US and Global Data From the American Heart Association[J] Circulation, 149(8)e347–e913. https://doi.org/10.1161/cir.0000000000001209. (2024).
Wang, L. D. & author group of China Stroke Center Report. Summary of China Stroke Center Report 2022[J].Chinese Journal of Cerebrovascular Diseases,2024,21(8):565–576. (2022). https://doi.org/10.3969/j.issn.1672-5921.2024.08.009
Powers, W. J. et al. :2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke:A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association[J] Stroke, 50(12)e344–e418. DOI:https://doi.org/10.1161/str.0000000000000211. (2019).
Virani, S. S. et al. Heart disease and stroke Statistics-2020 update:a report from the American. Heart Association[J] Circulation. 141 (9), e139–e596. https://doi.org/10.1161/cir.0000000000000757 (2020).
Thomalla, G. et al. Effect of informed consent on patient characteristics in a stroke thrombolysis trial[J].Neurology,2017,89(13),1400–1407 .https://doi.org/10.1212/wnl.0000000000004414
Xu, L. Dong Y,Dong q.research progress and prospect of Teneplase in the treatment of acute ischemic stroke[J]. Chin. J. Stroke. 20 (01), 20–25 (2025). From Cnki.
Majersik, J. J. Morgenstern LB.Informed consent in acute ischemic stroke:It’s on us[J].Neurology,2018,90(5),203–204 .https://doi.org/10.1212/wnl.0000000000004903
Xu, H. et al. Changes in Informed Consent Policy and Treatment Delays in Stroke Thrombolysis[J].J Stroke Cerebrovasc Dis,30(3),105551. (2021). https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.105551
Zhu, Y. et al. Factors Associated with Pre-Hospital Delay and Intravenous Thrombolysis in China[J].J Stroke Cerebrovasc Dis,29(8),104897. (2020). https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.104897
Iverson, E. et al. Factors affecting stress experienced by surrogate decision makers for critically ill patients:implications for nursing practice[J].Intensive Crit Care Nurs,30(2),77–85.DOI:10.1016/j.iccn.2013.08.008.From NLM. (2014).
Hieu, T. H. et al. Therapeutic efficacy and safety of chamomile for state anxiety,generalized anxiety disorder,insomnia,and sleep quality:a systematic review and meta-analysis of randomized trials and quasi-randomized trials[J]. Phytother Res. 33 (6), 1604–1615. https://doi.org/10.1002/ptr.6349 (2019).
Cui, M. J. et al. Meta-integration of qualitative studies on life support decision experience of proxy decision-makers in critically ill patients[J]. J. Nurs. 39 (23), 87–92. https://doi.org/10.3870/j.issn.1001-4152.2024.23.087 (2024).
Tian, Y. Y. D. I. N. G. et al. Neural mechanisms of anxiety,risk decision making and their relationship[J].Applied Psychology,2019,25(2):169–178 .https://doi.org/10.3969/j.issn.1006-6020.2019.02.008
Zhong, D. & Zhang ST,Wu, B. Interpretation of Chinese guidelines for diagnosis and treatment of acute ischemic stroke 2018[J]. Chin. J. Mod. Neurol. Dis. 19 (11), 897–901. https://doi.org/10.3969/j.issn.1672-6731.2019.11.015 (2019).
Azmeh, S. M. et al. State-Trait anxiety Inventory(STAI)[J].Springer new York, (2011). https://doi.org/10.1007/978-1-4419-9893-4_90
Degner, L. F., Sloan, J. A. & Venkatesh, P. The control preferences Scale[J]. Can. J. Nurs. Res. 29 (3), 21–43 (1997).
Xu, X. L. Preparation and reliability and validity evaluation of the satisfaction scale of patients’participation in medical decision making[D]. Hunan:Central South. Univ. https://doi.org/10.7666/d.y1718142 (2010).
Dong, E. H. & Bao, Y. Reliability and validity of the Chinese revised version of wake forest physician trust Scale[J]. Chin. J. Mental Health. 26 (3), 171–175. https://doi.org/10.3969/j.issn.1000-6729.2012.03.003 (2012).
Zimet, G. D. et al. The multidimensional scale of perceived social support[J]. J. Pers. Assess. 52 (1), 30–41. https://doi.org/10.1207/s15327752jpa5201_2 (1988).
Auerbach,Stephen, M. Trait-state anxiety and adjustment of surgery[J]. J. Consult Clin. Psych. 40 (2), 264–271. https://doi.org/10.1037/h0034538 (1973).
Chen The influence of attributive style and time pressure on information processing in decision making[J]. Psychol. Sci. 32 (6), 1445–1447. https://doi.org/10.1360/972009-782 (2009).
Iverson, E. et al. Factors affecting stress experienced by surrogate decision makers for critically ill patients:implications for nursing practice[J]. Intensive Crit. Care Nurs. 30 (2), 77–85. https://doi.org/10.1016/j.iccn.2013.08.008 (2014).
Tian, Y. Y. et al. Neural mechanisms of anxiety and risky decision making[J]. Chin. J. Appl. Psychol. 25 (2), 169–178 (2019).
Aloiau, A. et al. Impact of end-of-life planning on surrogate decision-maker anxiety in the US[J]. Int. J. Palliat. Nurs. 26 (2), 75–82. https://doi.org/10.12968/ijpn.2020.26.2.75 (2020).
Nundy, S. Montgomery T,Wachter RM.Promoting trust between patients and physicians in the era of artificial intelligence[J].Jama,2019,322(6),497–498 .https://doi.org/10.1001/jama.2018.20563
Wu, W. X. Li yz.application of preoperative shared decision-making in patients with breast cancer surgery[J]. J. Harbin Med. Univ. 56 (2), 128–132 (2022).
Soshi, T. et al. Pre-specified anxiety predicts future decision-making performances under different temporally constrained conditions[J]. Front. Psychol. 10 https://doi.org/10.3389/fpsyg.2019.01544 (2019).
Hindmarch, T. Hotopf M,Owen gs.depression and decision-making capacity for treatment or research:a systematic review[J]. Bmc Med. Ethics. 14 https://doi.org/10.1186/1472-6939-14-54 (2013).
Wang, Y. B. et al. The pre-hospital and in-hospital delay time in patients of the acute cerebralvascular disease in Beijing[J]. Chin. J. Nerv. Ment Dis. 35 (1), 22–25 (2009).
Acknowledgements
In addition to the authors, we would like to acknowledge the following individuals and organizations for their valuable contributions to this study: The surrogate decision-makers and patients who participated in the study: We deeply appreciate their willingness to share their experiences and insights, which were crucial for the completion of this research.The nursing staff of the Emergency Department of the First Affiliated Hospital of Zhengzhou University: Their assistance with data collection and patient care was instrumental in the successful execution of the study.The Ethics Committee of the First Affiliated Hospital of Zhengzhou University: We thank them for their guidance and approval throughout the research process.
Funding
The study was supported by Nursing research special fund of Zhengzhou University (HLKY20230001) and The National Health Commission’s Center for Science and Technology Development of Medical and Health 2023 Research Project on “Stroke Prevention and Treatment Technology“ (WKZX2023CZ0402), and the Henan Provincial Science and Technology Department science and Technology Attack Project (242102310221).
Author information
Authors and Affiliations
Contributions
YL G (Corresponding Author) was responsible for research design, data collection, and manuscript revision. CX Y contributed to research design, data collection and analysis, and wrote the manuscript. KK M participated in research design and prepared the figures for the manuscript. WF F and RK G participated in data collection and analysis, and assisted in writing the manuscript. YP L and LN G participated in research design, and assisted in data collection and analysis. All authors reviewed and approved the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, C., Ma, K., Guo, L. et al. The relationship between state anxiety of surrogate decision-makers and decision-making duration in acute ischemic stroke thrombolysis. Sci Rep 15, 13363 (2025). https://doi.org/10.1038/s41598-025-95937-4
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95937-4